Abstract
Introduction and objectives
GnRH agonists and GnRH antagonists are two of the mainstays of hormonal therapy (HT) for prostate cancer (PCa). These drugs are at increased risk of cardiovascular (CV) adverse events (AEs). Aim of our study was to compare real-life data on AEs associated with GnRH agonists and GnRH antagonists based on Eudra-Vigilance (EV) and Food and Drug Administration (FDA) reported AEs.
Materials and methods
EV and FDA databases were queried and the number of CV adverse events (AEs) for degarelix, buserelin, goserelin, leuprorelin, triptorelin until September 2021 were recorded. Specific CV AEs were recorded and data were analyzed per age and severity. pooled relative risk (PRR) was used to compare data between drugs.
Results
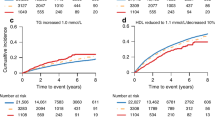
CV events were reported in 315/5128 (6%) for Degarelix, in 55/628 for Buserelin (9%), in 843/12,145 (7%) for Goserelin, in 3395/71,160 (5%) for Leuprorelin and in 214/4969 (5%) for Triptorelin. In terms of specific CV disorders, Degarelix presented lower risk of hypertension (PRR 0.60 (95% CI 0.37–0.98), p = 0.04), of myocardial infarction (PRR 0.05 (95% CI 0.01–0.39), p < 0.01) and thrombosis (PRR 0.14 (0.02–1.07), p = 0.06) when compared to GnRH agonists. Overall, younger patients (<65 years) presented a very low risk of CV AEs. Side effects were classified as serious in 90–96% of the cases. Fatal AEs were 5–20% over the CV AEs and 0.2–1% over the total AEs.
Conclusions
Real-life data are consistent with registry studies regarding side effects related to HT. Real-life data suggest GnRH agonists are associated with higher CV AEs when compared to GnRH antagonists. Clinicians should consider these data when prescribing HT especially in patients with CV comorbidities.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
Data were obtained by EudraVigilance and Food and Drug Administration Database freely accessible according by European Medicines Agency policies on website https://www.ema.europa.eu/en/human-regulatory/research-development/pharmacovigilance/eudravigilance.
References
Perrone V, Esposti LD, Giacomini E, Veronesi C, Blini V, Oderda M. Cardiovascular risk profile in prostate cancer patients treated with GnRH agonists versus antagonists: an Italian real-world analysis. Ther Clin Risk Manag. 2020;16:393–401.
Rosario DJ, Davey P, Green J, Greene D, Turner B, Payne H, et al. The role of gonadotrophin-releasing hormone antagonists in the treatment of patients with advanced hormone-dependent prostate cancer in the UK. World J Urol. 2016;34:1601–9.
Abufaraj M, Iwata T, Kimura S, Haddad A, Al-Ani H, Abusubaih L, et al. Differential impact of gonadotropin-releasing hormone antagonist versus agonist on clinical safety and oncologic outcomes on patients with metastatic prostate cancer: a meta-analysis of randomized controlled trials. Eur Urol. 2021;79:44–53.
Cindolo L, Natoli C, De Nunzio C, De Tursi M, Valeriani M, Giacinti S, et al. Abiraterone acetate for treatment of metastatic castration-resistant prostate cancer in chemotherapy-naive patients: an Italian analysis of patients’ satisfaction. Clin Genitourin Cancer. 2017;15:520–5.
Tema G, Lombardo R, Voglino O, Sica A, Baldassarri V, Nacchia A, et al. Adverse events related to radium-223 treatment: ‘real-life’ data from the Eudra-Vigilance database. Minerva Urol Nephrol. 2021;73:342–8.
Cindolo L, Natoli C, De Nunzio C, De Tursi M, Valeriani M, Giacinti S, et al. Safety and efficacy of abiraterone acetate in chemotherapy-naive patients with metastatic castration-resistant prostate cancer: an Italian multicenter real life study. BMC Cancer. 2017;17. https://doi.org/10.1186/s12885-017-3755-x.
Tenny S, Hoffman MR. Relative risk. StatPearls. 2022. https://pubmed.ncbi.nlm.nih.gov/28613574/.
De Nunzio C, Lombardo R, Tema G, Voglino O, Sica A, Baldassarri V, et al. Adverse events related to abiraterone and enzalutamide treatment: analysis of the EudraVigilance database and meta-analysis of registrational phase III studies. Prostate Cancer Prostatic Dis. 2020;23:199–206.
Lopes RD, Higano CS, Slovin SF, Nelson AJ, Bigelow R, Sørensen PS, et al. Cardiovascular safety of degarelix versus leuprolide in patients with prostate cancer: the primary results of the PRONOUNCE randomized trial. Circulation. 2021;144:1295–307.
Davey P, Kirby MG. Cardiovascular risk profiles of GnRH agonists and antagonists: real-world analysis from UK general practice. World J Urol. 2021;39:307–15.
Zareba P, Duivenvoorden W, Leong DP, Pinthus JH. Androgen deprivation therapy and cardiovascular disease: what is the linking mechanism? Ther Adv Urol. 2016;8:118–29.
Lester JF, Mason MD. Cardiovascular effects of hormone therapy for prostate cancer. Drug Health Patient Saf. 2015;7:129–38.
De Nunzio C, Lombardo R, Tema G, Alkhatatbeh H, Gandaglia G, Briganti A, et al. External validation of Chun, PCPT, ERSPC, Kawakami, and Karakiewicz nomograms in the prediction of prostate cancer: a single center cohort-study. Urol Oncol Semin Orig Investig. 2018;36:364.e1–7.
Brassetti A, Lombardo R, Emiliozzi P, Cardi A, Antonio DV, Antonio I, et al. Prostate-specific antigen density is a good predictor of upstaging and upgrading, according to the new grading system: the keys we are seeking may be already in our pocket. Urology. 2017. https://doi.org/10.1016/j.urology.2017.07.071.
De Nunzio C, Lombardo R, Nacchia A, Tema G, Tubaro A. Repeat prostate-specific antigen (PSA) test before prostate biopsy: a 20% decrease in PSA values is associated with a reduced risk of cancer and particularly of high-grade cancer. BJU Int. 2018;122:83–8.
De Nunzio C, Tema G, Trucchi A, Cicione A, Sica A, Lombardo R, et al. Smoking reduces PSA accuracy for detection of prostate cancer: results from an Italian cross-sectional study. Minerva Urol Nefrol. 2019. https://doi.org/10.23736/S0393-2249.19.03360-5.
Zhao J, Zhu S, Sun L, Meng F, Zhao L, Zhao Y, et al. Androgen deprivation therapy for prostate cancer is associated with cardiovascular morbidity and mortality: a meta-analysis of population-based observational studies. PLoS ONE. 2014;9. https://doi.org/10.1371/JOURNAL.PONE.0107516.
Bosco C, Bosnyak Z, Malmberg A, Adolfsson J, Keating NL, Van Hemelrijck M. Quantifying observational evidence for risk of fatal and nonfatal cardiovascular disease following androgen deprivation therapy for prostate cancer: a meta-analysis. Eur Urol. 2015;68:386–96.
Yu-Hsuan Joni S, Jian-Hua H, Chun-Kai C, Chao-Yuan H. Cardiovascular risk of gonadotropin-releasing hormone antagonist versus agonist in men with prostate cancer: an observational study in Taiwan. Prostate Cancer Prostatic Dis. 2022. https://doi.org/10.1038/S41391-022-00555-0.
Kim J-S, Taaffe DR, Galvão DA, Clay TD, Redfern AD, Hart NH, et al. Acute effect of high-intensity interval aerobic exercise on serum myokine levels and resulting tumour-suppressive effect in trained patients with advanced prostate cancer. Prostate Cancer Prostatic Dis. 2022. https://doi.org/10.1038/s41391-022-00624-4.
Kim JS, Taaffe DR, Galvão DA, Hart NH, Gray E, Ryan CJ, et al. Exercise in advanced prostate cancer elevates myokine levels and suppresses in-vitro cell growth. Prostate Cancer Prostatic Dis. 2022;25:86–92.
Harrison MR, Davis PG, Khouri MG, Bartlett DB, Gupta RT, Armstrong AJ, et al. A randomized controlled trial comparing changes in fitness with or without supervised exercise in patients initiated on enzalutamide and androgen deprivation therapy for non-metastatic castration-sensitive prostate cancer (EXTEND). Prostate Cancer Prostatic Dis. 2022;25:58–64.
Hanson ED, Alzer M, Carver J, Stopforth CK, Lucas AR, Whang YE, et al. Feasibility of home-based exercise training in men with metastatic castration-resistant prostate cancer. Prostate Cancer Prostatic Dis. 2022. https://doi.org/10.1038/s41391-022-00523-8.
Ussing A, Mikkelsen MLK, Villumsen BR, Wejlgaard J, Bistrup PE, Birkefoss K, et al. Supervised exercise therapy compared with no exercise therapy to reverse debilitating effects of androgen deprivation therapy in patients with prostate cancer: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis. 2022;25:491–506.
Cornford P, van den Bergh RCN, Briers E, Van den Broeck T, Cumberbatch MG, De Santis M, et al. EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer. Part II-2020 update: treatment of relapsing and metastatic prostate cancer. Eur Urol. 2021;79:263–82.
Algotar AM, Hsu CH, Chow HH, Dougherty ST, Babiker HM, Marrero DG, et al. Comprehensive lifestyle improvement program for prostate cancer (CLIPP) is associated with improvement in weight and components of metabolic syndrome in men exposed to androgen deprivation therapy for prostate cancer. Prostate Cancer Prostatic Dis. 2021;24:903–9.
Galvão DA, Newton RU, Chambers SK, Spry N, Joseph D, Gardiner RA, et al. Psychological distress in men with prostate cancer undertaking androgen deprivation therapy: modifying effects of exercise from a year-long randomized controlled trial. Prostate Cancer Prostatic Dis. 2021;24:758–66.
Galvão DA, Chambers SK. Exercise medicine in men with prostate cancer: breaking barriers to increase participation. Prostate Cancer Prostatic Dis. 2021;24:942–3.
Schumacher O, Galvão DA, Taaffe DR, Chee R, Spry N, Newton RU. Exercise modulation of tumour perfusion and hypoxia to improve radiotherapy response in prostate cancer. Prostate Cancer Prostatic Dis. 2021;24. https://doi.org/10.1038/s41391-020-0245-z.
De Nunzio C, Pastore AL, Lombardo R, Simone G, Leonardo C, Mastroianni R, et al. The new Epstein gleason score classification significantly reduces upgrading in prostate cancer patients. Eur J Surg Oncol. 2018. https://doi.org/10.1016/j.ejso.2017.12.003.
Zhang Y, Ouyang P, Post WS, Dalal D, Vaidya D, Blasco-Colmenares E, et al. Sex-steroid hormones and electrocardiographic QT-interval duration: findings from the third National Health and Nutrition Examination Survey and the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2011;174:403–11.
Boland J, Choi W, Lee M, Lin J. Cardiovascular toxicity of androgen deprivation therapy. Curr Cardiol Rep. 2021;23. https://doi.org/10.1007/S11886-021-01561-9.
De Nunzio C, Truscelli G, Presicce F, Bellangino M, Gacci M, Gaudio C, et al. Moderate-to-high cardiovascular risk is associated with increased lower urinary tract storage symptoms in patients with benign prostatic enlargement. Minerva Urol Nefrol. 2018;70:340–6.
De Nunzio C, Presicce F, Lombardo R, Cancrini F, Petta S, Trucchi A, et al. Physical activity as a risk factor for prostate cancer diagnosis: a prospective biopsy cohort analysis. BJU Int. 2015;17:29–35.
de Nunzio C, Tema G, Lombardo R, Cicione A, Dell’oglio P, Tubaro A. The role of metabolic syndrome in high grade prostate cancer: development of a clinical nomogram. Minerva Urol Nefrol. 2020;72:729–36.
Wekesa A, Harrison M, Watson RW. Physical activity and its mechanistic effects on prostate cancer. Prostate Cancer Prostatic Dis. 2015;18:197–207.
Author information
Authors and Affiliations
Contributions
AC: data collection, project development. AN: manuscript writing, data analysis. AG: data collection. CG: data collection. AF: data collection. MCG: manuscript writing. GT: data collection. RL: data collection. AT: project development. CDN: project development, manuscript writing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Ethical approval was waived by the local Ethics Committee of University La Sapienza of Rome in view of the retrospective nature of the study and all the procedures being performed were part of the routine care.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cicione, A., Nacchia, A., Guercio, A. et al. Cardiovascular adverse events-related to GnRH agonists and GnRH antagonists: analysis of real-life data from Eudra-Vigilance and Food and Drug Administration databases entries. Prostate Cancer Prostatic Dis 26, 765–771 (2023). https://doi.org/10.1038/s41391-022-00640-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-022-00640-4