Abstract
Background
Some studies have reported an inverse association between type 2 diabetes mellitus (T2DM) and prostate cancer (PCa), but results on this issue are still inconsistent. In this study, we evaluate whether this heterogeneity might be related to differences in this relationship by tumour or by individual genetic susceptibility to PCa.
Methods
We studied 1047 incident PCa cases and 1379 randomly selected controls, recruited in 7 Spanish provinces for the population-based MCC-Spain case-control. Tumour were classified by aggressiveness according to the International Society of Urological Pathology (ISUP), and we constructed a PCa polygenic risk score (PRS) as proxy for genetic susceptibility. The epidemiological questionnaire collected detailed self-reported data on T2DM diagnosis and treatment. The association between T2DM status and PCa was studied by fitting mixed logistic regression models, and, for its association by aggressiveness of PCa, with multinomial logistic regression models. To evaluate the possible modulator role of PRS in this relationship, we included the corresponding interaction term in the model, and repeated the analysis stratified by PRS tertiles.
Results
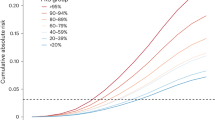
Globally, our results showed an inverse association between T2DM and overall PCa limited to grade 1 tumours (ORISUP = 1: 0.72; 95% CI: 0.53–0.98), which could be compatible with a detection bias. However, PCa risk also varied with duration of diabetes treatment -inversely to metformin and positively with insulin-, without differences by aggressiveness. When we considered genetic susceptibility, T2DM was more strongly associated with lower PCa risk in those with lower PRS (ORtertile 1: 0.31; 95% CI: 0.11–0.87), independently of ISUP grade.
Conclusions
Our findings reinforce the need to include aggressiveness and susceptibility of PCa, and T2DM treatments in the study of the relationship between both diseases.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Piñeros M, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144:1941–53.
Plym A, Penney KL, Kalia S, Kraft P, Conti DV, Haiman C et al. Evaluation of a multiethnic polygenic risk score model for prostate cancer. J Natl Cancer Inst. 2021. https://doi.org/10.1093/jnci/djab058. [Online ahead of print].
Dahut WL, Couvillon A, Pinto PA, Turkbey B, Karzai F. Natural history and imaging in men with high genetic risk for developing prostate cancer. Can J Urol. 2019;26:7–8.
Mucci LA, Hjelmborg JB, Harris JR, Czene K, Havelick DJ, Scheike T, et al. Familial risk and heritability of cancer among twins in nordic countries. JAMA. 2016;315:68–76.
Saunders EJ, Kote-Jarai Z, Eeles RA. Identification of germline genetic variants that increase prostate cancer risk and influence development of aggressive disease. Cancers. 2021;13:760.
World Cancer Research Fund International/American Institute for Cancer Research Continuous Update Project Report. Diet, Nutrition, Physical Activity, and Prostate Cancer. 2014.www.wcrf.org/sites/default/files/Prostate-Cancer-2014-Report.pdf.
Pilleron S, Sarfati D, Janssen-Heijnen M, Vignat J, Ferlay J, Bray F, et al. Global cancer incidence in older adults, 2012 and 2035: A population-based study. Int J Cancer. 2019;144:49–58.
Loeb S, Bjurlin MA, Nicholson J, Tammela TL, Penson DF, Carter HB, et al. Overdiagnosis and overtreatment of prostate cancer. Eur Urol. 2014;65:1046–55.
Fenton JJ, Weyrich MS, Durbin S, Liu Y, Bang H, Melnikow J. Prostate-specific antigen-based screening for prostate cancer: evidence report and systematic review for the US preventive services task force. JAMA. 2018;319:1914–31.
Sacerdote C, Ricceri F. Epidemiological dimensions of the association between type 2 diabetes and cancer: A review of observational studies. Diabetes Res Clin Pr. 2018;143:369–77.
Bansal D, Bhansali A, Kapil G, Undela K, Tiwari P. Type 2 diabetes and risk of prostate cancer: a meta-analysis of observational studies. Prostate Cancer Prostatic Dis. 2013;16:151–8. S1
Tsilidis KK, Allen NE, Appleby PN, Rohrmann S, Nöthlings U, Arriola L, et al. Diabetes mellitus and risk of prostate cancer in the European prospective investigation into cancer and nutrition. Int J Cancer. 2015;136:372–81.
Häggström C, Van Hemelrijck M, Zethelius B, Robinson D, Grundmark B, Holmberg L, et al. Prospective study of Type 2 diabetes mellitus, anti-diabetic drugs and risk of prostate cancer. Int J Cancer. 2017;140:611–7.
Xu H, Jiang H, Ding G, Zhang H, Zhang L, Mao S, et al. Diabetes mellitus and prostate cancer risk of different grade or stage: a systematic review and meta-analysis. Diabetes Res Clin Pr. 2013;99:241–9.
Chen M, Luo Y, Yang S, Xu L, Li N, Li H, et al. Association of diabetes mellitus with prostate cancer grade and prostate-specific antigen in Chinese biopsy population. Diabetes Res Clin Pr. 2018;141:80–87.
Dankner R, Boffetta P, Keinan-Boker L, Balicer RD, Berlin A, Olmer L, et al. Diabetes, prostate cancer screening and risk of low- and high-grade prostate cancer: an 11 year historical population follow-up study of more than 1 million men. Diabetologia. 2016;59:1683–91.
Miller EA, Pinsky PF, Pierre-Victor D. The relationship between diabetes, prostate-specific antigen screening tests, and prostate cancer. Cancer Causes Control. 2018;29:907–14.
Feng X, Song M, Preston MA, Ma W, Hu Y, Pernar CH, et al. The association of diabetes with risk of prostate cancer defined by clinical and molecular features. Br J Cancer. 2020;123:657–65.
Lin E, Garmo H, Van Hemelrijck M, Adolfsson J, Stattin P, Zethelius B, et al. Association of type 2 diabetes mellitus and antidiabetic medication with risk of prostate cancer: a population-based case-control study. BMC Cancer. 2020;20:551.
Ballotari P, Vicentini M, Manicardi V, Gallo M, Chiatamone Ranieri S, Greci M, et al. Diabetes and risk of cancer incidence: results from a population-based cohort study in northern Italy. BMC Cancer. 2017;17:703.
Lind M, Fahlén M, Eliasson B, Odén A. The relationship between the exposure time of insulin glargine and risk of breast and prostate cancer: an observational study of the time-dependent effects of antidiabetic treatments in patients with diabetes. Prim Care Diabetes. 2012;6:53–59.
Zaidi S, Gandhi J, Joshi G, Smith NL, Khan SA. The anticancer potential of metformin on prostate cancer. Prostate Cancer Prostatic Dis. 2019;22:351–61.
Kincius M, Patasius A, Linkeviciute-Ulinskiene D, Zabuliene L, Smailyte G. Reduced risk of prostate cancer in a cohort of Lithuanian diabetes mellitus patients. Aging Male. 2020;23:1333–8.
Castaño-Vinyals G, Aragonés N, Pérez-Gómez B, Martín V, Llorca J, Moreno V, et al. Population-based multicase-control study in common tumors in Spain (MCC-Spain): rationale and study design. Gac Sanit. 2015;29:308–15.
World Health Organization. Anatomical Therapeutic Chemical (ATC) Classification. Accessed 8 January 2021. https://www.who.int/tools/atc-ddd-toolkit/atc-classification.
Egevad L, Delahunt B, Srigley JR, Samaratunga H. International Society of Urological Pathology (ISUP) grading of prostate cancer - An ISUP consensus on contemporary grading. APMIS. 2016;124:433–5.
Gómez-Acebo I, Dierssen-Sotos T, Fernandez-Navarro P, Palazuelos C, Moreno V, Aragonés N, et al. Risk model for prostate cancer using environmental and genetic factors in the Spanish multi-case-control (MCC) study. Sci Rep. 2017;7:8994.
Rastmanesh R, Hejazi J, Marotta F, Hara N. Type 2 diabetes: a protective factor for prostate cancer? An overview of proposed mechanisms. Clin Genitourin Cancer. 2014;12:143–8.
Elabbady A, Hashad MM, Kotb AF, Ghanem AE. Studying the effect of type 2 diabetes mellitus on prostate-related parameters: a prospective single institutional study. Prostate Int. 2016;4:156–9.
Pashayan N, Pharoah PD, Schleutker J, Talala K, Tammela TL, Määttänen L, et al. Reducing overdiagnosis by polygenic risk-stratified screening: findings from the Finnish section of the ERSPC. Br J Cancer. 2015;113:1086–93.
Sipeky C, Talala KM, Tammela TLJ, Taari K, Auvinen A, Schleutker J. Prostate cancer risk prediction using a polygenic risk score. Sci Rep. 2020;10:17075.
Xiang YZ, Jiang SB, Zhao J, Xiong H, Cui ZL, Li GB, et al. Racial disparities in the association between diabetes mellitus-associated polymorphic locus rs4430796 of the HNF1β gene and prostate cancer: a systematic review and meta-analysis. Genet Mol Res. 2014;13:6582–92.
Machiela MJ, Lindström S, Allen NE, Haiman CA, Albanes D, Barricarte A, et al. Association of type 2 diabetes susceptibility variants with advanced prostate cancer risk in the Breast and Prostate Cancer Cohort Consortium. Am J Epidemiol. 2012;176:1121–9.
Pierce BL, Ahsan H. Genetic susceptibility to type 2 diabetes is associated with reduced prostate cancer risk. Hum Hered. 2010;69:193–201.
Frayling TM, Colhoun H, Florez JC. A genetic link between type 2 diabetes and prostate cancer. Diabetologia. 2008;51:1757–60.
Cuyàs E, Verdura S, Llorach‐Pares L, Fernández‐Arroyo S, Luciano‐Mateo F, Cabré N, et al. Metformin directly targets the H3K27me3 demethylase KDM6A/UTX. Aging Cell. 2018;17:e12772.
Wang Y, Liu X, Yan P, Tang J, Chen T, Sun Y, et al. Effect of metformin on the risk of prostate cancer in patients with type 2 diabetes by considering different confounding factors: a meta-analysis of observational studies. Eur J Cancer Prev. 2020;29:42–52.
Ghiasi B, Sarokhani D, Najafi F, Motedayen M, Dehkordi AH. The relationship between prostate cancer and metformin consumption: a systematic review and meta-analysis study. Curr Pharm Des. 2019;25:1021–9.
He K, Hu H, Ye S, Wang H, Cui R, Yi L. The effect of metformin therapy on incidence and prognosis in prostate cancer: A systematic review and meta-analysis. Sci Rep. 2019;9:2218.
Chien S-W, Kuo D-Y, Liao J-M, Wang PS, Yu C-H. Growth modulation of diabetic factors and antidiabetic drugs on prostate cancer cell lines. Chin J Physiol. 2016;59:109–18.
Chen Y, Chen Q, Wang Z, Zhou J. Insulin therapy and risk of prostate cancer: a systematic review and meta-analysis of observational studies. PLoS ONE. 2013;8:e81594.
Colmers IN, Bowker SL, Tjosvold LA, Johnson JA. Insulin use and cancer risk in patients with type 2 diabetes: a systematic review and meta-analysis of observational studies. Diabetes Metab. 2012;38:485–506.
Cambra K, Galbete A, Forga L, Lecea O, Ariz MJ, Moreno-Iribas C, et al. Sex and age differences in the achievement of control targets in patients with type 2 diabetes: results from a population-based study in a South European region. BMC Fam Pract. 2016;17:144.
Basterra-Gortari FJ, Bes-Rastrollo M, Ruiz-Canela M, Gea A, Martinez-Gonzalez MÁ. Prevalencia de obesidad y diabetes en adultos españoles, 1987-2012. Med Clínica. 2017;148:250–6.
International Diabetes Federation. IDF Diabetes Atlas. 9th edn. International Diabetes Federation: Brussels, Belgium, 2019. https://www.diabetesatlas.org.
Acknowledgements
The authors thank Ingrid de Ruiter, MBChB, PhD, for English language support in the preparation of this manuscript. We thank all subjects who participated in the study and all MCC-Spain collaborators.
Data and material availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Funding
The study was partially funded by the “Acción transversal del cancer”, approved by the Spanish Ministry council on 11 October 2007, by the Instituto de Salud Carlos III-FEDER-a way to build Europe-(PI08/1770, PI08/0533, PI08/1359, pi09/00773, PI09/01286, PI 09/01903, PI09/02078, PI09/01662, PI11/01403, PI11/01889-FEDER, PI11/00226, PI11/01810, PI11/02213, PI12/00488, PI12/00265, PI12/01270, PI12/00715, PI12/00150, PI14/01219, PI14/0613), by the Fundación Marqués de Valdecilla (api 10/09), by the Junta de Castilla y León (le22a10-2), by the Consejería de Salud of the Junta de Andalucía (2009-s0143), by the Conselleria de Sanitat of the Generalitat Valenciana (ap_061/10), by the Recercaixa (2010acup 00310), by the regional government of the Basque country, by the Consejería de Sanidad de la Región de Murcia, by the European Commission Grants Food-ct-2006-036224-hiwate, by the Spanish Association Against Cancer (AECC) scientific foundation, by the Catalan Government DURSI grant 2014SGR647, by the Fundación Caja de Ahorros de Asturias and by the University of Oviedo.
Author information
Authors and Affiliations
Contributions
BP-G, MK, MP and JJJ-M conceptualisation and design of the study; RB-R and EG-E formal analysis of data; NFLB, RO-R, MV-E, GF-T, PF-N, LC, VL and IG-A, data curation; BP-G, GC-V, JL, JA and JJJ-M funding acquisition; GC-V, NA, MK and MP project administration; RB-R, EG-E, BP-G and JJJ-M first draft of this paper. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Barrios-Rodríguez, R., García-Esquinas, E., Pérez-Gómez, B. et al. Prostate cancer genetic propensity risk score may modify the association between this tumour and type 2 diabetes mellitus (MCC-Spain study). Prostate Cancer Prostatic Dis 25, 694–699 (2022). https://doi.org/10.1038/s41391-021-00446-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-021-00446-w