Abstract
Background
To investigate the feasibility of a freehand transperineal (TP) systematic prostate biopsy protocol under local anaesthesia (LA) and the value of different sectors in diagnosing prostate cancer (PCa).
Methods
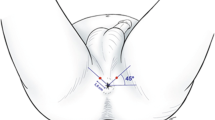
A total of 611 consecutive freehand TP biopsies under LA in 2 hospitals were prospectively evaluated. Cancer detection rate in each of the four different sectors (anterior, mid, posterior, basal) was recorded to evaluate the value of each sector. Procedure tolerability was assessed by pain score and complications were documented.
Results
Systematic biopsies were performed in 556 out of 611 men with a median of 20 (IQR 12–24) biopsy cores taken. The median PSA was 9.9 (Inter-quartile range[IQR] 6.4–16.2) ng/mL, and 89.0% were first biopsies. All PCa and ISUP grade group (GG) ≥ 2 PCa (HGPCa) were diagnosed in 41.4% (230/556) and 28.2% (157/556) biopsies respectively. 77.0% HGPCa was diagnosed in ≥2 sectors. Single-sector HGPCa was predominantly found in anterior or posterior sector. Omitting base sector would have missed 1.5% (1/65) HGPCa out of the 219 cases with ≥24-core biopsies performed. Further omission of mid sector would have missed 3.1% (2/65) HGPCa and 7.4% (7/94) ISUP GG1 PCa (in which 3/7 involved 2 sectors). LA TP biopsy was well tolerated and the mean pain scores of the different steps of the procedure were between 1.9–3.1 (out of 10). Post-biopsy fever occurred in 0.3% of patients (2/611) and no sepsis was reported. The risk of urinary retention in men with ≥20 cores in ≥60 ml prostate was 7.8% (14/179), compared with 1.7% (7/423) in other groups (p < 0.001).
Conclusions
TP sectoral prostate biopsy under LA was well tolerated with minimal sepsis risk. Basal sector biopsies had minimal additional value to HGPCa detection and its omission can be considered.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Rawla P. Epidemiology of Prostate Cancer. World J Oncol. 2019;10:63–89.
Loeb S, Vellekoop A, Ahmed HU, Catto J, Emberton M, Nam R, et al. Systematic review of complications of prostate biopsy. Eur Urol. 2013;64:876–92.
Xiang J, Yan H, Li J, Wang X, Chen H, Zheng X. Transperineal versus transrectal prostate biopsy in the diagnosis of prostate cancer: a systematic review and meta-analysis. World J Surg Oncol. 2019;17:31.
Eldred-Evans D, Kasivisvanathan V, Khan F, Hemelrijck MV, Polson A, Acher P, et al. The use of transperineal sector biopsy as a first-line biopsy strategy: a multi-institutional analysis of clinical outcomes and complications. Urol J. 2016;13:2849–55.
Kuru TH, Wadhwa K, Chang RT, Echeverria LM, Roethke M, Polson A, et al. Definitions of terms, processes and a minimum dataset for transperineal prostate biopsies: a standardization approach of the Ginsburg Study Group for Enhanced Prostate Diagnostics. BJU Int. 2013;112:568–77.
Kum F, Elhage O, Maliyil J, Wong K, Faure Walker N, Kulkarni M, et al. Initial outcomes of local anaesthetic freehand transperineal prostate biopsies in the outpatient setting. BJU Int. 2020;125:244–52.
Lo KL, Chui KL, Leung CH, Ma SF, Lim K, Ng T, et al. Outcomes of transperineal and transrectal ultrasound-guided prostate biopsy. Hong Kong Med J. 2019;25:209–15.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:801–10.
Epstein JI, Egevad L, Amin MB, Delahunt B, Srigley JR, Humphrey PA, et al. The 2014 International Society of Urological Pathology (ISUP) consensus conference on gleason grading of prostatic carcinoma: definition of grading patterns and proposal for a new grading system. Am J Surg Pathol. 2016;40:244–52.
Altok M, Kim B, Patel BB, Shih YT, Ward JF, McRae SE, et al. Cost and efficacy comparison of five prostate biopsy modalities: a platform for integrating cost into novel-platform comparative research. Prostate Cancer Prostatic Dis. 2018;21:524–32.
Patel V, Merrick GS, Allen ZA, Andreini H, Taubenslag W, Singh S, et al. The incidence of transition zone prostate cancer diagnosed by transperineal template-guided mapping biopsy: implications for treatment planning. Urology. 2011;77:1148–52.
Vyas L, Acher P, Kinsella J, Challacombe B, Chang RT, Sturch P, et al. Indications, results and safety profile of transperineal sector biopsies (TPSB) of the prostate: a single centre experience of 634 cases. BJU Int. 2014;114:32–7.
Smith JB, Popert R, Nuttall MC. Transperineal sector prostate biopsies: a local anesthetic outpatient technique. Urology. 2014;83:1344–9.
Yao MH, Zou LL, Wu R. Transperineal ultrasound-guided 12-core prostate biopsy: an extended approach to diagnose transition zone prostate tumors. PLoS ONE. 2014;9:e89171.
Guo G, Xu Y, Zhang X. TRUS-guided transperineal prostate 12+X core biopsy with template for the diagnosis of prostate cancer. Oncol Lett. 2017;13:4863–7.
Mai Z, Yan W, Zhou Y, Zhou Z, Chen J, Xiao Y, et al. Transperineal template-guided prostate biopsy: 10 years of experience. BJU Int. 2016;117:424–9.
Merrick GS, Irvin S, Fiano R, Anderson R, Butler WM, Adamovich E. Pathology and quality of life outcomes following office-based transperineal prostate biopsy. Urology. 2016;94:24–8.
Meyer AR, Joice GA, Schwen ZR, Partin AW, Allaf ME, Gorin MA. Initial experience performing in-office ultrasound-guided transperineal prostate biopsy under local anesthesia using the precisionpoint transperineal access system. Urology. 2018;115:8–13.
Ristau BT, Allaway M, Cendo D, Hart J, Riley J, Parousis V, et al. Free-hand transperineal prostate biopsy provides acceptable cancer detection and minimizes risk of infection: evolving experience with a 10-sector template. Urol Oncol. 2018;36:528.e15–.e20.
Thurtle D, Starling L, Leonard K, Stone T, Gnanapragasam VJ. Improving the safety and tolerability of local anaesthetic outpatient transperineal prostate biopsies: a pilot study of the CAMbridge PROstate Biopsy (CAMPROBE) method. J Clin Urol. 2018;11:192–99.
Stefanova V, Buckley R, Flax S, Spevack L, Hajek D, Tunis A, et al. Transperineal Prostate Biopsies Using Local Anesthesia: experience with 1,287 Patients. Prostate Cancer Detection Rate, Complications and Patient Tolerability. J Urol. 2019;201:1121–6.
Neale A, Stroman L, Kum F, Jabarkhyl D, Di Benedetto A, Mehan N, et al. Targeted and systematic cognitive freehand-guided transperineal biopsy: is there still a role for systematic biopsy? BJU Int. 2020;126:280–5.
Marra G, Zhuang J, Beltrami M, Calleris G, Zhao X, Marquis A, et al. Transperineal freehand multiparametric MRI fusion targeted biopsies under local anaesthesia for prostate cancer diagnosis: a multicentre prospective study of 1014 cases.. BJU Int. 2020. https://doi.org/10.1111/bju.15121. [Online ahead of print].
Chen R, Sjoberg DD, Huang Y, Xie LP, Zhou L, He D, et al. Prostate Specific Antigen and Prostate Cancer in Chinese Men Undergoing Initial Prostate Biopsies Compared with Western Cohorts. J Urol. 2017;197:90–6.
Kasivisvanathan V, Rannikko AS, Borghi M, Panebianco V, Mynderse LA, Vaarala MH, et al. MRI-Targeted or Standard Biopsy for Prostate-Cancer Diagnosis. N Engl J Med. 2018;378:1767–77.
Ahdoot M, Wilbur AR, Reese SE, Lebastchi AH, Mehralivand S, Gomella PT, et al. MRI-Targeted, Systematic, and Combined Biopsy for Prostate Cancer Diagnosis. N Engl J Med. 2020;382:917–28.
Drost FH, Osses DF, Nieboer D, Steyerberg EW, Bangma CH, Roobol MJ, et al. Prostate MRI, with or without MRI-targeted biopsy, and systematic biopsy for detecting prostate cancer. Cochrane Database Syst Rev. 2019:4;CD012663.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Chiu, P.KF., Lo, KL., Teoh, J.YC. et al. Sectoral cancer detection and tolerability of freehand transperineal prostate biopsy under local anaesthesia. Prostate Cancer Prostatic Dis 24, 431–438 (2021). https://doi.org/10.1038/s41391-020-00293-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-020-00293-1
This article is cited by
-
Antimicrobial prophylaxis: To do or not to do? This is the question
Prostate Cancer and Prostatic Diseases (2024)