Abstract
Background
To investigate association of prenatal risk factors and neonatal outcomes of preterm infants with pulmonary hypertension (PH).
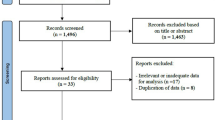
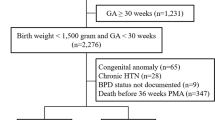
Methods
A prospective cohort study of very-low-birth-weight infants born at 22–29 weeks’ gestation who received PH-specific treatment during hospitalization. Infants were classified using a two-step cluster analysis based on gestational age (GA), small-for-gestational-age (SGA), exposure to antenatal corticosteroids (ACS), histologic chorioamnionitis (HCA), and oligohydramnios.
Results
Among 910 infants, six clusters were identified: cluster A (HCA, n = 240), cluster B (oligohydramnios, n = 79), cluster C (SGA, n = 74), cluster D (no-ACS, n = 109), cluster E (no dominant parameter, n = 287), and cluster F (HCA and oligohydroamnios, n = 121). Cluster A was used as a reference group for comparisons among clusters. Compared to cluster A, cluster C (aHR: 1.63 [95% CI: 1.17–2.26]) had higher risk of overall in-hospital mortality. Clusters B (aHR: 1.52 [95% CI: 1.09–2.11]), D (aHR: 1.71 [95% CI: 1.28–2.30]), and F (aHR: 1.51 [95% CI: 1.12–2.03]) had higher risks of receiving PH-specific treatment within the first week of birth compared to cluster A.
Conclusion
These findings may provide a better understanding of prenatal risk factors contributing to the development of PH.
Impact
-
Pulmonary hypertension (PH), presenting as hypoxic respiratory failure, has complex etiologies in preterm infants.
-
Although multifactorial risks for the development of PH in preterm infants are known, few studies have classified infants with similar etiologies for PH.
-
Each cluster has distinct patterns of prenatal condition and neonatal outcome.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The Korean Neonatal Network (KNN) Publication Ethics Policy adheres to the following research data management and access guidelines. All information about patients and participating NICUs are confidential. They might be used by individuals for approved research purposes. If an individual or institution that is not affiliated with KNN wants to use the data, it must make an official request to the KNN publication-Ethics Committee and obtain approval from the network.
References
Mirza, H., Mandell, E. W., Kinsella, J. P., McNamara, P. J. & Abman, S. H. Pulmonary vascular phenotypes of prematurity: the path to precision medicine. J. Pediatr. 259, 113444 (2023).
Arjaans, S. et al. Clinical significance of early pulmonary hypertension in preterm infants. J. Pediatr. 251, 74–81.e3 (2022).
Kim, H. H. et al. Early pulmonary hypertension is a risk factor for bronchopulmonary dysplasia-associated late pulmonary hypertension in extremely preterm infants. Sci. Rep. 11, 11206 (2021).
Mirza, H. et al. Natural history of postnatal cardiopulmonary adaptation in infants born extremely preterm and risk for death or bronchopulmonary dysplasia. J. Pediatr. 198, 187–193.e181 (2018).
Nakanishi, H., Suenaga, H., Uchiyama, A. & Kusuda, S. Persistent pulmonary hypertension of the newborn in extremely preterm infants: a Japanese cohort study. Arch. Dis. Child Fetal Neonatal Ed. 103, F554–F561 (2018).
Al-Ghanem, G. et al. Bronchopulmonary dysplasia and pulmonary hypertension: a meta-analysis. J. Perinatol. 37, 414–419 (2017).
Arjaans, S. et al. Identification of gaps in the current knowledge on pulmonary hypertension in extremely preterm infants: a systematic review and meta-analysis. Paediatr. Perinat. Epidemiol. 32, 258–267 (2018).
Ruoss, J. L., Rios, D. R. & Levy, P. T. Updates on management for acute and chronic phenotypes of neonatal pulmonary hypertension. Clin. Perinatol. 47, 593–615 (2020).
Goss, K. Long-term pulmonary vascular consequences of perinatal insults. J. Physiol. 597, 1175–1184 (2019).
Seth, S. A., Soraisham, A. S. & Harabor, A. Risk factors and outcomes of early pulmonary hypertension in preterm infants. J. Matern. Fetal Neonatal Med. 31, 3147–3152 (2018).
Check, J. et al. Fetal growth restriction and pulmonary hypertension in premature infants with bronchopulmonary dysplasia. J. Perinatol. 33, 553–557 (2013).
Kim, D.-H. et al. Risk factors for pulmonary artery hypertension in preterm infants with moderate or severe bronchopulmonary dysplasia. Neonatology 101, 40–46 (2011).
Taglauer, E., Abman, S. H. & Keller, R. L. Recent advances in antenatal factors predisposing to bronchopulmonary dysplasia. Semin. Perinatol. 42, 413–424 (2018).
Abman, S. H. Pulmonary hypertension: the hidden danger for newborns. Neonatology 118, 211–217 (2021).
Polglase, G. R. et al. Intrauterine inflammation causes pulmonary hypertension and cardiovascular sequelae in preterm lambs. J. Appl. Physiol. 108, 1757–1765 (2010).
Williams, O., Hutchings, G., Hubinont, C., Debauche, C. & Greenough, A. Pulmonary effects of prolonged oligohydramnios following mid-trimester rupture of the membranes–antenatal and postnatal management. Neonatology 101, 83–90 (2012).
Mohseni-Bod, H. & Bohn, D. Pulmonary hypertension in congenital diaphragmatic hernia. Semin. Pediatr. Surg. 16, 126–133 (2007).
Barros, F. C. et al. The distribution of clinical phenotypes of preterm birth syndrome: implications for prevention. JAMA Pediatr. 169, 220–229 (2015).
Maron, B. A. & Abman, S. H. Translational advances in the field of pulmonary hypertension. Focusing on developmental origins and disease inception for the prevention of pulmonary hypertension. Am. J. Respir. Crit. Care Med. 195, 292–301 (2017).
Barrington, K. J., Finer, N. & Pennaforte, T. Inhaled nitric oxide for respiratory failure in preterm infants. Cochrane Database Syst. Rev. 1, Cd000509 (2017).
Villar, J. et al. Association between preterm-birth phenotypes and differential morbidity, growth, and neurodevelopment at age 2 years: results from the INTERBIO-21st newborn study. JAMA Pediatr. 175, 483–493 (2021).
Chang, Y. S., Park, H.-Y. & Park, W. S. The Korean neonatal network: an overview. J. Korean Med. Sci. 30, S3–S11 (2015).
Singh, Y. & Lakshminrusimha, S. Pathophysiology and management of persistent pulmonary hypertension of the newborn. Clin. Perinatol. 48, 595–618 (2021).
Bacher, J, Wenzig, K & Vogler, M. SPSS TwoStep Cluster—a First Evaluation. (Department of Sociology, Social Science Institute, Friedrich-Alexander-University: Erlangen-Nuremberg, Germany, 2004) 1–30.
Kent, P., Jensen, R. K. & Kongsted, A. A comparison of three clustering methods for finding subgroups in MRI, SMS or clinical data: SPSS TwoStep cluster analysis, latent gold and snob. BMC Med. Res. Methodol. 14, 113 (2014).
Rohan, J. M. et al. Identification of self-management patterns in pediatric type 1 diabetes using cluster analysis. Pediatr. Diabetes 12, 611–618 (2011).
Huang, R. C. et al. Importance of cardiometabolic risk factors in the association between nonalcoholic fatty liver disease and arterial stiffness in adolescents. Hepatology 58, 1306–1314 (2013).
Kaufman L. & Rousseeuw P. J. Finding Groups in Data: An Introduction to Cluster Analysis (John Wiley & Sons, 2005).
Finken, M. J. J. et al. Children born small for gestational age: differential diagnosis, molecular genetic evaluation, and implications. Endocr. Rev. 39, 851–894 (2018).
Goldenberg, R. L., Hauth, J. C. & Andrews, W. W. Intrauterine infection and preterm delivery. N. Engl. J. Med. 342, 1500–1507 (2000).
Mourani, P. M. et al. Early pulmonary vascular disease in preterm infants at risk for bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. 191, 87–95 (2015).
Mehler, K. et al. An echocardiographic screening program helps to identify pulmonary hypertension in extremely low birthweight infants with and without bronchopulmonary dysplasia: a single-center experience. Neonatology 113, 81–88 (2018).
Sallmon, H. et al. Extremely premature infants born at 23–25 weeks gestation are at substantial risk for pulmonary hypertension. J. Perinatol. 42, 781–787 (2022).
Kramer, B. W. et al. Decreased expression of angiogenic factors in placentas with chorioamnionitis after preterm birth. Pediatr. Res. 58, 607–612 (2005).
Miller, J. D., Benjamin, J. T., Kelly, D. R., Frank, D. B. & Prince, L. S. Chorioamnionitis stimulates angiogenesis in saccular stage fetal lungs via CC chemokines. Am. J. Physiol. Lung Cell Mol. Physiol. 298, L637–L645 (2010).
Yum, S. K. et al. Impact of histologic chorioamnionitis on pulmonary hypertension and respiratory outcomes in preterm infants. Pulm. Circ. 8, 2045894018760166 (2018).
Kim, S. Y. et al. Neonatal morbidities associated with histologic chorioamnionitis defined based on the site and extent of inflammation in very low birth weight infants. J. Korean Med. Sci. 30, 1476–1482 (2015).
Villamor-Martinez, E. et al. Association of chorioamnionitis with bronchopulmonary dysplasia among preterm infants: a systematic review, meta-analysis, and metaregression. JAMA Netw. Open 2, e1914611–e1914611 (2019).
Wu, C.-S., Chen, C.-M. & Chou, H.-C. Pulmonary hypoplasia induced by oligohydramnios: findings from animal models and a population-based study. Pediatr. Neonatol. 58, 3–7 (2017).
Kim, Y. J., Shin, S. H., Park, H. W., Kim, E. K. & Kim, H. S. Risk factors of early pulmonary hypertension and its clinical outcomes in preterm infants: a systematic review and meta-analysis. Sci. Rep. 12, 14186 (2022).
Daayana, S., Baker, P. & Crocker, I. An image analysis technique for the investigation of variations in placental morphology in pregnancies complicated by preeclampsia with and without intrauterine growth restriction. J. Soc. Gynecol. Investig. 11, 545–552 (2004).
Gumina, D. L., Black, C. P., Balasubramaniam, V., Winn, V. D. & Baker, C. D. Umbilical cord blood circulating progenitor cells and endothelial colony-forming cells are decreased in preeclampsia. Reprod. Sci. 24, 1088–1096 (2017).
Di Fiore, J. M. et al. Patterns of oxygenation, mortality, and growth status in the surfactant positive pressure and oxygen trial cohort. J. Pediatr. 186, 49–56.e41 (2017).
Walsh, M. C. et al. Association of oxygen target and growth status with increased mortality in small for gestational age infants: further analysis of the surfactant, positive pressure and pulse oximetry randomized trial. JAMA Pediatr. 170, 292–294 (2016).
Boghossian, N. S., Geraci, M., Edwards, E. M. & Horbar, J. D. Morbidity and mortality in small for gestational age infants at 22 to 29 weeks’ gestation. Pediatrics 141, e20172533 (2018).
Breinig, S. et al. Pulmonary hypertension among preterm infants born at 22 through 32 weeks gestation in France: prevalence, survival, morbidity and management in the EPIPAGE-2 cohort study. Early Hum. Dev. 184, 105837 (2023).
Ryu, Young, H., Oh, S., Sohn, J. & Lee, J. The associations between antenatal corticosteroids and in-hospital outcomes of preterm singleton appropriate for gestational age neonates according to the presence of maternal histologic chorioamnionitis. Neonatology 116, 369–375 (2019).
Bird, A. D., Choo, Y. L., Hooper, S. B., McDougall, A. R. & Cole, T. J. Mesenchymal glucocorticoid receptor regulates the development of multiple cell layers of the mouse lung. Am. J. Respir. Cell Mol. Biol. 50, 419–428 (2014).
Bridges, J. P. et al. Glucocorticoid regulates mesenchymal cell differentiation required for perinatal lung morphogenesis and function. Am. J. Physiol. Lung Cell. Mol. Physiol. 319, L239–l255 (2020).
Konduri, G. G., Bakhutashvili, I., Eis, A. & Afolayan, A. Antenatal betamethasone improves postnatal transition in late preterm lambs with persistent pulmonary hypertension of the newborn. Pediatr. Res. 73, 621–629 (2013).
El-Saie, A. et al. Bronchopulmonary dysplasia—associated pulmonary hypertension: an updated review. Semin. Perinatol. 47, 151817 (2023).
Acknowledgements
This research was supported by a research grant (2022-ER0603-00#) funded by Korea National Institute of Health.
Funding
This research was supported by Soonchunhyang University Research Fund (grant number 2022-1214) to cover publication costs. The funder had no role in (1) the design, (2) the collection, analysis, and interpretation of data, (3) the writing of the report, or (4) the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
S.P.B. and S.S.K. conceptualized and designed the research. S.P.B. and S.P. collected and analyzed the data. S.P.B. and J.Y. wrote the manuscript. H.L. assisted with study design and reviewed the manuscript. S.S.K. and W.H.H. reviewed and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent to participate
Participation of infants in the registration of data in the KNN was approved by the Institutional Review Board (IRB) of each participating center. Written informed consent was obtained from parents of each participant in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bae, S.P., Kim, S.S., Yun, J. et al. Neonatal outcomes of preterm infants with pulmonary hypertension: clustering based on prenatal risk factors. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03232-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-024-03232-1