Abstract
Background
Overnutrition in early life increases the risk of obesity and metabolic diseases. We investigated the effects and the window period of a curcumin (CUR) diet on postnatal overfed rats.
Methods
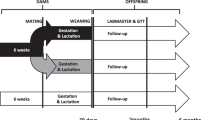
Male rats aged 3 days were randomly divided into normal litters (NL, 10 pups/litter) and small litters (SL, 3 pups/litter). After weaning (Week 3, W3), NL rats were fed a normal diet (NL) and SL rats were fed a normal diet (SL) or 2% CUR diet from weaning (W3) (SL-CURW13), beginning of puberty (W6) (SL-CURW16), or end of puberty (W8) (SL-CURW18) for 10 weeks.
Results
Body weight, glucose intolerance and hyperlipidemia in the SL rats were higher than in the NL rats, especially after puberty. After the CUR intervention, SL-CURW13 and SL-CURW16 rats showed lower body weight gain, adipose tissue weight and mRNA level of C/EBPα in SAT, along with higher mRNA levels of β-catenin. There was no difference between SL and SL-CURW18 rats. Glucose tolerance, serum lipids and hepatic lipids recovered to normal in the SL-CURW13 rats, but only partially in the SL-CURW16 and SL-CURW18 rats.
Conclusion
Prepuberty is a window period for CUR intervention to improve programmed outcomes in postnatal overfed rats.
Impact
-
Overnutrition during the first 1000 days of life has persistent negative effects on metabolism. Strategies should be taken to prevent overnutrition in early life to reduce the risk of obesity and metabolic disease in later life.
-
A small-litter rat model was utilized to simulate early-life overnutrition in humans. We investigated the different effects and critical period for curcumin intervention on postnatal overfed rats.
-
Dietary curcumin intervention before puberty could effectively transform nutritional programming to reduce obesity and metabolic disorders caused by early-life overnutrition, and an earlier intervention might predict a better outcome.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
Data included in this manuscript are available upon request by contacting the corresponding author.
References
Pan, X. F., Wang, L. & Pan, A. Epidemiology and Determinants of Obesity in China. Lancet Diabetes Endocrinol. 9, 373–392 (2021).
Jaacks, L. M. et al. The Obesity Transition: Stages of the Global Epidemic. Lancet Diabetes Endocrinol. 7, 231–240 (2019).
Di Cesare, M. et al. The Epidemiological Burden of Obesity in Childhood: A Worldwide Epidemic Requiring Urgent Action. BMC Med. 17, 212 (2019).
Mameli, C., Mazzantini, S. & Zuccotti, G. V. Nutrition in the First 1000 Days: The Origin of Childhood Obesity. Int. J. Environ. Res. Public Health 13, 838 (2016).
Agosti, M., Tandoi, F., Morlacchi, L. & Bossi, A. Nutritional and Metabolic Programming during the First Thousand Days of Life. Pediatr. Med. Chir. 39, 157 (2017).
Draijer, L., Benninga, M. & Koot, B. Pediatric NAFLD: An Overview and Recent Developments in Diagnostics and Treatment. Expert Rev. Gastroenterol. Hepatol. 13, 447–461 (2019).
La Colla, A., Cámara, C. A., Campisano, S. & Chisari, A. N. Mitochondrial Dysfunction and Epigenetics Underlying the Link between Early-Life Nutrition and Non-Alcoholic Fatty Liver Disease. Nutr. Res. Rev. 362, 1–33 (2022).
Langley-Evans, S. C. Nutrition in Early Life and the Programming of Adult Disease: A Review. J. Hum. Nutr. Diet. 28, 1–14 (2015).
Xavier, J. L. P. et al. Litter Size Reduction Induces Metabolic and Histological Adjustments in Dams throughout Lactation with Early Effects on Offspring. Acad. Bras. Cienc. 91, e20170971 (2019).
Parra-Vargas, M., Ramon-Krauel, M., Lerin, C. & Jimenez-Chillaron, J. C. Size Does Matter: Litter Size Strongly Determines Adult Metabolism in Rodents. Cell Metab. 32, 334–340 (2020).
Zhou, N., Du, S., Dai, Y., Yang, F. & Li, X. ω3pufas Improve Hepatic Steatosis in Postnatal Overfed Rats and HepG2 Cells by Inhibiting Acetyl-COA Carboxylase. Food Sci. Nutr. 9, 5153–5165 (2021).
Zhu, X. et al. Dietary Curcumin Supplementation Promotes Browning and Energy Expenditure in Postnatal Overfed Rats. Nutr. Metab. 18, 97 (2021).
Du, S. et al. Curcumin Alleviates Hepatic Steatosis by Improving Mitochondrial Function in Postnatal Overfed Rats and Fatty L02 Cells through the SIRT3 Pathway. Food Funct. 13, 2155–2171 (2022).
Patel, S. S. et al. Cellular and Molecular Mechanisms of Curcumin in Prevention and Treatment of Disease. Crit. Rev. Food Sci. Nutr. 60, 887–939 (2020).
Jabczyk, M., Nowak, J., Hudzik, B. & Zubelewicz-Szkodzińska, B. Curcumin in Metabolic Health and Disease. Nutrients 13, 4440 (2021).
Abd El-Hameed, N. M., Abd El-Aleem, S. A., Khattab, M. A., Ali, A. H. & Mohammed, H. H. Curcumin Activation of Nuclear Factor E2-Related Factor 2 Gene (Nrf2): Prophylactic and Therapeutic Effect in Nonalcoholic Steatohepatitis (NASH). Life Sci. 285, 119983 (2021).
Hassan, M. H. et al. Antitoxic Effects of Curcumin against Obesity-Induced Multi-Organs’ Biochemical and Histopathological Abnormalities in an Animal Model. Evid. Based Complement Altern. Med. 2022, 9707278 (2022).
Chen, Y. et al. Curcumin Prevents Obesity by Targeting TRAF4-Induced Ubiquitylation in M(6) A-Dependent Manner. EMBO Rep. 22, e52146 (2021).
Hellmann, P. H. et al. The Effect of Curcumin on Hepatic Fat Content in Individuals with Obesity. Diabetes Obes. Metab. 24, 2192–2202 (2022).
Vors, C. et al. Supplementation with Resveratrol and Curcumin Does Not Affect the Inflammatory Response to a High-Fat Meal in Older Adults with Abdominal Obesity: A Randomized, Placebo-Controlled Crossover Trial. J. Nutr. 148, 379–388 (2018).
Rahmani, S. et al. Treatment of Non-Alcoholic Fatty Liver Disease with Curcumin: A Randomized Placebo-Controlled Trial. Phytother. Res. 30, 1540–1548 (2016).
Norris, S. A. et al. Nutrition in Adolescent Growth and Development. Lancet 399, 172–184 (2022).
Brown, T. et al. Interventions for Preventing Obesity in Children. Cochrane Database Syst. Rev. 7, Cd001871 (2019).
Mintjens, S. et al. Cardiorespiratory Fitness in Childhood and Adolescence Affects Future Cardiovascular Risk Factors: A Systematic Review of Longitudinal Studies. Sports Med. 48, 2577–2605 (2018).
Lee, J. H. et al. Heat-Killed Enterococcus Faecalis Prevents Adipogenesis and High Fat Diet-Induced Obesity by Inhibition of Lipid Accumulation through Inhibiting C/EBP-α and PPAR-γ in the Insulin Signaling Pathway. Nutrients 14, 1308 (2022).
Luo, J., Yu, Z., Tovar, J., Nilsson, A. & Xu, B. Critical Review on Anti-Obesity Effects of Phytochemicals through Wnt/β-Catenin Signaling Pathway. Pharm. Res. 184, 106461 (2022).
Schneider, M. Adolescence as a Vulnerable Period to Alter Rodent Behavior. Cell Tissue Res. 354, 99–106 (2013).
Bolton, M. M. et al. Postnatal Alterations in GABAB Receptor Tone Produce Sensorimotor Gating Deficits and Protein Level Differences in Adulthood. Int J. Dev. Neurosci. 41, 17–27 (2015).
Koletzko, B. et al. Nutrition During Pregnancy, Lactation and Early Childhood and Its Implications for Maternal and Long-Term Child Health: The Early Nutrition Project Recommendations. Ann. Nutr. Metab. 74, 93–106 (2019).
Fall, C. H. D. & Kumaran, K. Metabolic Programming in Early Life in Humans. Philos. Trans. R. Soc. Lond. B Biol. Sci. 374, 20180123 (2019).
Haschke, F., Binder, C., Huber-Dangl, M. & Haiden, N. Early-Life Nutrition, Growth Trajectories, and Long-Term Outcome. Nestle Nutr. Inst. Workshop Ser. 90, 107–120 (2019).
Kerkhof, G. F. & Hokken-Koelega, A. C. Rate of Neonatal Weight Gain and Effects on Adult Metabolic Health. Nat. Rev. Endocrinol. 8, 689–692 (2012).
Tock, L. et al. Nonalcoholic Fatty Liver Disease Decrease in Obese Adolescents after Multidisciplinary Therapy. Eur. J. Gastroenterol. Hepatol. 18, 1241–1245 (2006).
Grønbæk, H. et al. Effect of a 10-Week Weight Loss Camp on Fatty Liver Disease and Insulin Sensitivity in Obese Danish Children. J. Pediatr. Gastroenterol. Nutr. 54, 223–228 (2012).
de Piano, A. et al. Metabolic and Nutritional Profile of Obese Adolescents with Nonalcoholic Fatty Liver Disease. J. Pediatr. Gastroenterol. Nutr. 44, 446–452 (2007).
Nowak, K. L. et al. Curcumin Therapy to Treat Vascular Dysfunction in Children and Young Adults with Autosomal Dominant Polycystic Kidney Disease: Design and Baseline Characteristics of Participants. Contemp. Clin. Trials Commun. 19, 100635 (2020).
Lewanda, A. F., Gallegos, M. F. & Summar, M. Patterns of Dietary Supplement Use in Children with Down Syndrome. J. Pediatr. 201, 100–105.e130 (2018).
Hanai, H. et al. Curcumin Maintenance Therapy for Ulcerative Colitis: Randomized, Multicenter, Double-Blind, Placebo-Controlled Trial. Clin. Gastroenterol. Hepatol. 4, 1502–1506 (2006).
Heidari, Z., Daei, M., Boozari, M., Jamialahmadi, T. & Sahebkar, A. Curcumin Supplementation in Pediatric Patients: A Systematic Review of Current Clinical Evidence. Phytother. Res. 36, 1442–1458 (2022).
Saadati, S. et al. The Effects of Curcumin Supplementation on Liver Enzymes, Lipid Profile, Glucose Homeostasis, and Hepatic Steatosis and Fibrosis in Patients with Non-Alcoholic Fatty Liver Disease. Eur. J. Clin. Nutr. 73, 441–449 (2019).
Hodaei, H., Adibian, M., Nikpayam, O., Hedayati, M. & Sohrab, G. The Effect of Curcumin Supplementation on Anthropometric Indices, Insulin Resistance and Oxidative Stress in Patients with Type 2 Diabetes: A Randomized, Double-Blind Clinical Trial. Diabetol. Metab. Syndr. 11, 41 (2019).
Sahebkar, A. et al. Curcuminoids Modulate Pro-Oxidant-Antioxidant Balance but Not the Immune Response to Heat Shock Protein 27 and Oxidized LDL in Obese Individuals. Phytother. Res. 27, 1883–1888 (2013).
Saraf-Bank, S., Ahmadi, A., Paknahad, Z., Maracy, M. & Nourian, M. Effects of Curcumin on Cardiovascular Risk Factors in Obese and Overweight Adolescent Girls: A Randomized Clinical Trial. Sao Paulo Med. J. 137, 414–422 (2019).
Yan, H. et al. Ajuba Functions as a Co-Activator of C/EBPβ to Induce Expression of PPARγ and C/EBPα During Adipogenesis. Mol. Cell Endocrinol. 539, 111485 (2022).
Liu, M., Qin, J., Cong, J. & Yang, Y. Chlorogenic Acids Inhibit Adipogenesis: Implications of Wnt/β-Catenin Signaling Pathway. Int J. Endocrinol. 2021, 2215274 (2021).
Chen, N. & Wang, J. Wnt/β-Catenin Signaling and Obesity. Front. Physiol. 9, 792 (2018).
Harvey, I. et al. Glucocorticoid-Induced Metabolic Disturbances Are Exacerbated in Obese Male Mice. Endocrinology 159, 2275–2287 (2018).
Hou, M. et al. Neonatal Overfeeding Induced by Small Litter Rearing Causes Altered Glucocorticoid Metabolism in Rats. PLoS One 6, e25726 (2011).
Yan, C. et al. Curcumin Regulates Endogenous and Exogenous Metabolism via Nrf2-FXR-LXR Pathway in NAFLD Mice. Biomed. Pharmacother. 105, 274–281 (2018).
Saadati, S. et al. Curcumin and Inflammation in Non-Alcoholic Fatty Liver Disease: A Randomized, Placebo Controlled Clinical Trial. BMC Gastroenterol. 19, 133 (2019).
Teixeira, D., Martins, C., Oliveira, G. & Soares, R. Metabolically Healthy Obesity in a Paediatric Obesity Clinic. J. Pediatr. Endocrinol. Metab. 35, 1147–1153 (2022).
Mathis, B. J., Tanaka, K. & Hiramatsu, Y. Factors of Obesity and Metabolically Healthy Obesity in Asia. Medicine 58, 1271 (2022).
Smith, G. I., Mittendorfer, B. & Klein, S. Metabolically Healthy Obesity: Facts and Fantasies. J. Clin. Invest 129, 3978–3989 (2019).
Li, S. et al. Curcumin Alleviates High-Fat Diet-Induced Hepatic Steatosis and Obesity in Association with Modulation of Gut Microbiota in Mice. Food Res. Int. 143, 110270 (2021).
Kindblom, J. M. et al. BMI Change during Puberty and the Risk of Heart Failure. J. Intern. Med. 283, 558–567 (2018).
Ohlsson, C., Bygdell, M., Nethander, M., Rosengren, A. & Kindblom, J. M. BMI Change During Puberty Is an Important Determinant of Adult Type 2 Diabetes Risk in Men. J. Clin. Endocrinol. Metab. 104, 1823–1832 (2019).
Suzuki, A. et al. Association between Puberty and Features of Nonalcoholic Fatty Liver Disease. Clin. Gastroenterol. Hepatol. 10, 786–794 (2012).
Jones, J. G. Hepatic Glucose and Lipid Metabolism. Diabetologia 59, 1098–1103 (2016).
Reinehr, T., Kleber, M., Lass, N. & Toschke, A. M. Body Mass Index Patterns over 5 Y in Obese Children Motivated to Participate in a 1-Y Lifestyle Intervention: Age as a Predictor of Long-Term Success. Am. J. Clin. Nutr. 91, 1165–1171 (2010).
Sangouni, A. A., Taghdir, M., Mirahmadi, J., Sepandi, M. & Parastouei, K. Effects of Curcumin and/or Coenzyme Q10 Supplementation on Metabolic Control in Subjects with Metabolic Syndrome: A Randomized Clinical Trial. Nutr. J. 21, 62 (2022).
Funding
This study was supported by the National Natural Science Foundation of China (81773421) and the Innovation Team of Jiangsu Health (CXTDA2017035).
Author information
Authors and Affiliations
Contributions
Xiaonan Li designed the study. Susu Du, Nan Zhou and Wen Zheng performed the experiments. Susu Du analyzed the data and wrote the original draft. Xiaolei Zhu, Ru Ling and Wei Zhou reviewed the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
All animal studies were approved by the University Committee on Use and Care of Animals and were overseen by the Unit for Laboratory Animal Medicine of Nanjing Medical University (ID: 1904056-1).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Du, S., Zhou, N., Zheng, W. et al. Prepuberty is a window period for curcumin to prevent obesity in postnatal overfed rats. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03154-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-024-03154-y