Abstract
Aim
To assess whether patients born with an abdominal wall defect (AWD) have impaired cardiorespiratory performance capacity, motor skills, core stability or quality of life in a long-term follow up.
Methods
Patients diagnosed with AWD between 2002 and 2013 were invited to participate in the study, which included clinical examination, spirometry, cardiopulmonary exercise performance testing, assessment of motor activity, ultrasound, electromyography of the abdominal wall and assessment of the Gastrointestinal Quality of Life Index (GIQLI). The results were compared to a healthy control group matched for age, sex, BMI, and physical activity levels.
Results
In total, 18 AWD patients (mean age 12.6 ± 3.5 years) were included and there were no significant differences in anthopometric data compared to the control group (n = 18). AWD patients had a significantly lower GIQLI score (AWD mean 137.2 ± 6.8 vs. control mean 141.4 ± 4.9; p = 0.038) and were affected by decreased motor abilities with significantly higher Dordel-Koch-Test values (AWD median 3.54/IQR 1 vs. control median 2.8/IQR 1; p = 0.005).
Conclusion
Follow-up examinations of AWD patients revealed decreased motor abilities and GIQLI scores while cardiopulmonary function was not different compared to healthy controls. The clinical impact of these findings remains to be elucidated.
Impact
-
Clinical examination, assessment of the gastrointestinal quality of life, sport medical testing, electromyography and abdominal wall ultrasound were performed in patients with congenital abdominal wall defect and compared to an age and sex matched healthy control group.
-
Results of spirometry and spiroergometry, ultrasound or electromyography did not significantly differ between the groups.
-
Significantly decreased locomotor function and gastrointestinal quality of life were found in patients with abdominal wall defect. However, the clinical impact of these findings remains to be elucidated.
Similar content being viewed by others
Introduction
Gastroschisis (GS) and omphalocele (OC) represent the two most common congenital abdominal wall defects (AWDs) occurring with an incidence of 4.5 of 10,000 live births and 0.6–4.8 of 10,000 live births, respectively. As opposed to other congenital malformations, a rising incidence of GS has been shown in the recent years.1,2,3,4
GS is usually a solitary anomaly and the outcome is related to the underlying integrity of the prolapsed bowel loops. In contrary, OC is frequently associated with other malformations such as chromosomal or cardiac defects or syndromes like pentalogy of Cantrell and Beckwith Wiedemann syndrome.5 Both forms of AWDs necessitate early postnatal surgical intervention, mostly in one or two stages, as well as support at a neonatal or surgical intensive care unit. Mortality is lower in GS patients than in these born with OC mostly due to associated anomalies.6
The literature concerning long-term outcome and quality of life (QOL) of patients suffering from AWDs is scarce. Some publications have reported long-term complications like redo surgical procedures because of fascial gaps or umbilical and incisional hernias.7,8 Furthermore, stool irregularities, abdominal pain and several hospital admissions due to ileus or sub-ileus have been described.7 Additionally, half of the patients are unsatisfied with the cosmetic result.9,10,11 Other studies, however, have revealed that children born with an AWD have the same QOL compared with the healthy population.11
Recent studies have revealed a decreased cardiopulmonary performance capacity (CPC) in patients born with congenital malformations such as anorectal malformations or esophageal atresia.12,13 However, only one report describes the cardiopulmonary outcome in patients with large AWDs (GS > 4 cm, OC > 6 cm) including 18 participants. The authors reported that patients operated on for AWD at birth exhibit a normal cardiorespiratory function.14
The trunk musculature including the transversus abdominis, internal and external oblique and rectus abdominis muscles are important for core and especially for spine stability.15 However, the abdominal musculature of AWD patients compared to a healthy control group has not been studied yet.
Therefore, it was the aim of this single-center observational long-term outcome case-control pilot study to assess whether patients born with AWDs have a decreased CPC, impaired motor skills and QOL compared to healthy controls.
Patients and methods
All patients born between 2002 and 2013 (aged between 6 and 18 years) diagnosed with an AWD and treated at our Department were invited to participate in a prospective study consisting of clinical examination, spirometry, cardiopulmonary exercise performance testing (CPET), assessment of the motor activity, ultrasound and electromyography of the abdominal wall, stance and gait analyses and questionnaires for gastrointestinal QOL. All measurements were performed in one day. Patients with hemodynamic relevant cardiac disease or mental disorders were excluded.
According to the literature, we classified GS as complicated if patients suffered from concomitant intestinal atresia, volvulus, necrosis or perforation.16,17,18 Giant OC was defined as a defect larger than 5 cm.19,20
The results were compared to a healthy age-, sex-, BMI- and physical activity level-matched control group recruited from friends and family of the Department´s employees.
This study was performed according to the declaration of Helsinki. All patients and controls and/or their legal guardians gave informed written consent. This study was approved by the institutional review board (EK 32–231 ex 19/20). All measurements were performed between May 2020 and June 2021.
Anthropometric data
Body height (BH) and weight (BW) were measured and the body mass index (BMI) calculated. Segmental multi-frequency impedance spectroscopy (CombynTM ECG, Academic Technologies at the Institute of Cardiovascular Medicine GmbH, Graz, Austria) was used to measure appendicular muscle mass and total body fat (TBF) as previously described in the literature.21 Cardiac arrhythmias were excluded with a 12-lead resting electrocardiography (ECG) and non-invasive blood pressure (NIBP) measurement at rest was performed.
Participants were asked to rate their physical activity levels according to four groups (“daily”, “several times a week”, “once per week” or “once per month”).
Spirometry
Lung function was measured by small spirometry (Oxycon Pro® Carl Reiner GmbH, Vienna, Austria) at rest and following exercise. Maximum vital capacity (VCmax) and the forced expiratory volume in 1 s (FEV 1) were assessed.
VCmax was expressed as observed and corrected according to the expected maximum vital capacity over age and sex. The Tiffeneau index was calculated as FEV 1/VCmax. A restrictive ventilation disorder was defined as a predominantly decreased VCmax and an obstructive ventilation disorder as a decreased Tiffeneau index.22
Cardiopulmonary exercise performance testing (CPET)
CPET with a bicycle ergometer (Excalibur Sport®, Lode B.V., Groningen, The Netherlands) and the spirometer in an upright position was used to measure cardiopulmonary exercise performance. A stepwise load increase protocol, specified for sex and age, was used as published before.23 The spiroergometry was continued to subjective exhaustion or until the participants were unable to maintain the required pedaling speed (cadence) of more than 60 revolutions per minute (rpm). A three minutes “cool down” of slow pedaling (60 rpm) with the same workload as at the beginning of the test followed the exercise phase.
Twelve-lead ECG (Cardinal HealthTM electrocardiography, Dublin, Ireland) measured Heartrate (HR) and finger pulse oximeter (Habel Medizintechnik®, Vienna, Austria) assessed oxygen saturation continuously during the whole exercise.
At the end of each step and after the cool down lactate levels were determined by earlobe sampling of 20 µl blood per measurement to heparinized capillaries before the test (enzymatically amperometric measurement with a Biosen C_line® (EKF Diagnostics for life, Cardiff, UK)).
Respiratory parameters including the oxygen uptake (VO2), the oxygen pulse (O2/HR), the respiratory equivalent for oxygen (EQO2), the breathing reserve (BR) and the respiratory exchange ratio (RER) were assessed.23
Relative performance capacity was calculated from the achieved maximal wattage in relation to age and sex-specific standard values.24 The peak oxygen uptake (peak VO2) was defined as the average VO2 over the last 30 seconds prior to subjective exhaustion and was expressed in ml/kg/min. A RER > 1.10 was used as criterion to determine that the peak VO2 reflects a peak physiological workload.25
Assessment of motor abilities
The Dordel-Koch-Test (DKT) was used to assess motor abilities (flexibility, coordinative and conditional skills).26 The tests consists of seven established and validated items: lateral jumping, sit and reach, sit-ups, long stand jump, one-legged stand, push-ups and 6-min-run and allows a quick and differentiated evaluation of motor performance among all basic motor skills.26 In the present study, the endurance was tested with a spiroergometry instead of a 6-min-run. The indicated grades 1 to 6 correspond to a school grading system with lower values indicating better performance.26
Electromyography (EMG) of the abdominal wall & gait and stance analysis
Eight sensors as shown in Supplementary Fig. 1 were fixed to the abdominal wall (Ultium® Wireless Surface EMG, Velamed GmbH with Ultium® EMG Sensor, Velamed GmbH and Noraxon MR 3.14, Cologne, Germany). Afterwards, patients had to perform eight exercises to measure activity of the M. rectus abdominis (RA), M. obliquus externus (OE)/internus (OI) and M. transversus abdominis (TA). Exercises are shown in Supplementary Fig. 2. The EMG amplitude of each muscle and exercise was normalized to the amplitude observed in isometric maximum voluntary contraction (MVC) for each muscle. The neural activity was expressed as percentage of the MVC for each muscle.27
A floor-based foot pressure measurement device (Zebris (F64x240x3), Velamed GmbH, Noraxon MR 3.14, Cologne, Germany) was used for gait and stance analyses in order to measure core stability. For stance analyses, the trajectory of the center of pressure (COP) was assessed while ordinary relaxed stand and Matthias’ Arm-Raising Test on the plate. Gait analyses were performed by walking over the plate for 3 min. Exercises are shown in Supplementary Fig. 3. The whole examination was filmed for later analyses (Logitech HD Pro Webcam C920, Logitech Europe S.A., Lausanne, Switzerland).
Ultrasound of the abdominal wall
Ultrasound of the abdominal wall (GE Healthcare Vivid S5 Ultrasound Machine/GE Healthcare 12L-RS probe, Solingen, Germany) was performed to assess the thickness of the four muscles (RA/OE/OI/TA). A protocol was established as shown in Fig. 1. First, the distance between the xiphoid and the symphysis was halved (C), divided in thirds (B1/B2) and marked with a skin marker. Then, the medioclavicular and anterior axillar lines were marked. The rectus abdominis muscle was measured at its thickest point in the sagittal axis in B1, B2 and C. At the crossing I-VI the OE, OI and TA were measured in the sagittal axis. All tests were performed by the same examiner (CF).
Quality of life and cosmetic satisfaction
The Gastrointestinal Quality of Life Index (GIQLI) was assessed in all participants. This index is a tool to assess the QOL, specifically for patients with gastrointestinal disorders. In total, the questionnaire consists of 36 items answered by the patient. The questions can be separated in five dimensions: core symptoms, physical items, psychological items, social items and disease- specific items. Each question is scored from 0–4 (Likert Scale) whereas 4 is the most favorable outcome. The scoring system ranges from 0 to 144 with higher scores describing a better QoL.28
Moreover, patients had to rate their stool consistency according to the Bristol Stool scale, a validated tool that has been used in children before.29
All patients were asked if they suffer from backpain and/or gastroesophageal reflux. If yes, the patients were asked to quantify their occurrence (“never”, “once per month”, “once per week” or “daily”).
The POSAS (Patient and Observer Scar Assessment Scale) as a well validated tool to assess the quality of the scar and cosmetic satisfaction was used in this study.30, 31 Patients (PSAS) and the Observer (OSAS) had to assess the scar on the abdominal wall. The scoring system ranges from 6–60 with lower scores describing a better cosmetic result. In addition, both had to give an overall opinion of the scar (1–10). Lower scores mean higher quality or satisfaction with the scar.
A clinical examination of the abdomen was performed to identify length, width and position of the scar. It was checked if an umbilicus, hypertrophic scar, scar hardening, additional scars and visible stichtes were present. All examinations were performed by the same person (CF).
Statistical analysis
Data were entered in an Excel 2016® spreadsheet. For statistical analysis SPSS Statistics 27© (IBM Corp. Released 2020. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp) was used. Data were tested for normal distribution applying the Kolmogorow-Smirnow test. In case of normal distribution, data are depicted as mean and standard deviation and a two-sided, unpaired t test was used for statistical group comparison between AWD patients and controls. If no normal distribution was found, data are displayed as median and interquartile range (IQR) and group comparisons were performed with Mann–Whitney-U tests. Pearson tests were used to analyze correlations between metric parameters and Spearman tests for correlation analysis between ordinal and metric data. The Fishers exact test was used for group comparison in case of categorical data. Statistical significance was defined as p < 0.05.
Results
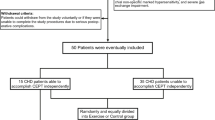
Out of 43 eligible patients treated with an AWD in the respective period, we were able to contact 30 patients and 18 agreed to participate in the study. A detailed CONSORT diagram of the included and excluded patients is provided in Fig. 2.
AWD group
The mean age of the patients (7 males, 11 females) was 12.6 ± 3.5 years (range: 7–18). Table 1 shows the different types of AWD (GS: n = 12, OC: n = 6) and their treatment.
One patient (8%) with GS had a congenital colonic atresia as an associated malformation and was classified as complicated GS in comparison to eleven (92%) uncomplicated GS cases. Two OC cases (33%) were defined as a giant OC and four as small OC (67%). In one small OC, an ileum atresia had been treated. The detailed associated malformations are listed in Table 1.
In fourteen patients (77.8%) primary closure within the first 24 h could be achieved. Two children were born with an intestinal atresia necessitating creation of a stoma and primary closure of the AWD. In one case it was necessary to perform a delayed closure using a spring-loaded silo and in one case secondary closure was performed with a patch following primary application of a silo (Table 1).
Overall, the mean number of procedures affecting the abdominal wall was 2.2 ± 1.4. The maximum number was five surgical procedures in one patient. There was no significant difference in the number of surgeries between OC and GS patients (OC mean 2.8 ± 2 vs GS mean 1.9 ± 0.9; p = 0.334; unpaired two-sided t test).
In eight patients postoperative complications, necessitating operative procedures within the first twelve years of life, were detected. In three of these patients (37.5%) post-operative complications occurred in the first year of life: one patient suffered from midgut volvulus and an ileus due to adhesions, another one from an ileus due to adhesions and in one case a patch infection after two months was recorded.
Furthermore, in three other cases an umbilical hernia was detected and repaired (at an age of 1, 1 and 2 years, respectively). One case of a midgut volvulus and ileus due to adhesions at the age of six years and one more patient with an ileus due to adhesions at the age of twelve was reported.
Control group
The mean age of the age-, sex- and BMI-matched healthy control group (7 males, 11 females) was 12.3 ± 3.3 years (range: 7–17 years). There was no statistically significant difference regarding patient age between AWD and control groups (p = 0.798; unpaired two-sided t test).
Anthropometric data and laboratory results
Height, weight, BMI, body fat percentage and muscle mass were not statistically significant different between the study and the control group (Table 2). Likewise, no significant differences in physical activity levels could be found.
Spirometry
Neither VCmax nor Tiffeneau index was significantly different between the control group and AWD patients (Table 2). Likewise, comparisons of spirometry values revealed no significant differences between patients with GS and OC. Detailed data is shown in Supplementary Table 1.
Two patients in the AWD group showed a restrictive ventilation disorder. These two were born with giant OC and lung hypoplasia (ID 18) and additional lung dysplasia in one case (ID 14). In the control group, four probands showed an obstructive and one a restrictive ventilation disorder.
Cardiopulmonary exercise performance
RER Value (AWD mean 1.16 ± 0.08 vs. controls mean 1.14 ± 0.11) did not differ significantly between the two groups (p = 0.600; unpaired t test,).
Spiroergometry was not significantly different regarding relative performance capacity, peak VO2, O2/HR, EQO2 and BR (Table 2).
Comparing patients with GS and OC no statistically significant differences in spiroergometry were seen. Detailed data is shown in Supplementary Table 1.
There was no significant difference of the relative performance capacity between the group of uncomplicated and complicated GS as well as between small and giant OC (data not shown).
Assessment of motor abilities
The Dordel-Koch Test (DKT) revealed significantly decreased values in the AWD group (p = 0.005; unpaired two-sided t test). In detail, AWD patients had significantly lower values concerning lateral jumping and sit-ups (Table 3). However, no statistically significant differences between patients with GS and OC were found (Supplementary Table 1).There was no significant correlation between DKT and BMI (r = 0.213, p = 0.213; Spearman test), muscle mass (r = 0.241, p = 0.183; Spearman test), total body fat percentage (r = 0.171, p = 0.318; Spearman test) or relative performance capacity (r = −0.001, p = 0.994; Spearman test). However, we found a statistically significant negative correlation between DKT and physical activity level (r = −0.379, p = 0.022; Spearman test). There was no significant difference of the DKT results comparing uncomplicated and complicated GS as well as small and giant OC (data not shown).
Gait and stance analyses and electromyography (EMG) of the abdominal wall
Except for cadence and stride time there were no statistically significant differences in stance and gait analyses between the AWD and the control group (Table 4).
The EMG amplitude of each muscle (RA, OI, OE, TA) and exercise showed no significant differences between the AWD and control group as well as between GS and OC patients (data not shown).
There was no statistical difference in duration (seconds) of performing the exercise “plank” (AWD mean 20.7 ± 14.7 vs. controls mean 21.3 ± 10.5; p = 0.981; unpaired t test,) and “lift and hold legs” (AWD median 14/ IQR 16 vs. controls median 10.5/ IQR 9; p = 0.126; Mann–Whitney-U Test). Exercises are shown in detail in Supplementary Fig. 2. Four patients of the AWD group were not able to perform the exercise “plank”. Two controls and one patient with AWD were not able to perform the exercise “lift and hold legs”.
Ultrasound of the abdominal wall
Thickness of the abdominal wall muscles (RA/OE/OI/TA) showed no statistical difference between AWD and control patients (Table 5). Likewise, GS and OC patients did not have significant differences. Details are shown in Supplementary Table 2. There was also no statistical difference between measurements on the right and the left side of the abdomen. Detailed values are presented in Supplementary Table 3.
Evaluation of cosmetic satisfaction and quality of life
GIQLl was significantly different between the AWD and control group (AWD mean 137.2 ± 6.8 vs. controls mean 141.4 ± 4.9, p = 0.038; unpaired two-sided t-test) but not between GS and OC (GS mean 137.5 ± 7.7 vs. OC mean 136.5 ± 5.2, p = 0.749; unpaired two-sided t test). However, there were no significant differences in GIQLI between the group of uncomplicated and complicated GS as well as between small and giant OCs (data not shown). There was no significant correlation between the number of surgeries and GIQLI (r = 0.154, p = 0.542; Spearman test).
While in the AWD group six patients suffered from back pain (n = 5 several times a month and n = 1 several times a week), four patients of the control groups reported back pain (n = 2 several times a month and n = 2 several times a week). These differences were not significantly different (p = 0.354; Fisher´s Exact test).
The rate of gastroesophageal reflux was not significantly different between AWD patients (n = 1 several times a month and n = 1 daily) and controls (n = 1 several times a month) (p = 0.500; Fisher´s Exact test).
16 patients (94%) indicated a normal stool frequency as “every other day to twice a day” and one (6%) “more often” in the AWD group. 13 patients (76%) of control group rated their stool frequency as “every other day to twice a day” and four (24%) as “more often”. In both groups most participants classified their stool consistency as Bristol Stool Scale (BSS) type 3 or 4 (AWD: type 2 n = 1 (6%), type 3 n = 5 (27%), type 4 n = 11 (61%), type 6 n = 1 (6%) and controls: type 3 n = 12 (67%), type 4 n = 6 (33%)). There was no significant difference between AWD group and controls concerning stool frequency or consistency.
In nine cases (n = 6 GS; n = 3 OC) the umbilicus was the only visible scar following abdominal wall closure. Seven patients (n = 4 GS; n = 3 OC) had a horizontal and one a vertical main scar. Six patients had additional scars on their abdominal wall (n = 3 GS; n = 3 OC) and in twelve cases stiches were visible as scars (n = 10 GS; n = 2 OC).
Cosmetic satisfaction was good, as patients rated their overall opinion with 3.9 ± 2.8 and the observer overall opinion was 2.7 ± 1.4. The PSAS Score was 16.7 ± 8.6 and the OSAS was 13.5 ± 5.7.
The GS group had a significantly wider scar than the OC group (GS mean 21.8 ± 9.21 mm; OC mean 11.5 ± 8.2 mm; p = 0.034; unpaired two-sided t test). However, neither the length of the scar nor the cosmetic satisfaction (PSAS, OSAS) was significantly different between the two groups. Detailed data is shown in Table 6.
OSAS showed significant correlation with the length of the scar (r = 0.685, p = 0.002; Spearmen test), otherwise neither OSAS nor PSAS showed significant correlation with number of surgeries or the appearance of the scar (Table 6).
No statistically significant differences of GIQLI, cosmetic satisfaction, back pain, reflux, stool frequency or BSS could be found between GS and OC (data not shown).
Discussion
The main findings of our pilot study were that patients born with AWDs had significantly decreased scores concerning motor abilities and gastrointestinal quality of life. Additionally, we present data of lung function, exercise performance, electromyography, stance and gait analyses, ultrasound of the abdominal wall as well as cosmetic satisfaction of 18 AWD patients at a mean follow-up of 13 years and compare the obtained values to a healthy matched control group.
GS is defined as complicated in the presence of concomitant intestinal atresia, volvulus, necrosis or perforation.16,17,18 The definition of giant omphalocele is more diverse and ranges from inability to achieve primary closure, different amount of liver in the sac (>50–75%) or size of the defect (>5 cm).19,20 For our study, we have defined a giant OC as a size of the defect greater or equal to 5 cm. Nevertheless, we did not find any differences in our outcome parameters between uncomplicated and complicated GS or small and giant OCs. However, these findings have to be interpreted with caution due to the limited number of patients included in the respective subgroups.
Spirometry did not reveal any significant long-term pulmonary impairment of AWD patients suggesting that the abdominal wall malformation per se does not necessarily influence the cardiopulmonary function. Only two patients had a restrictive ventilation disorder and these children were born with a giant OC associated with lung hypoplasia (compare Table 1, Patient ID 14 and 18). This finding is in line with previous studies showing that patients with giant OCs may suffer from long term respiratory difficulties.32
Cardiopulmonary performance capacity plays an important role in health and well-being.33 Therefore, cardiopulmonary exercise performance testing should be part of the long-term examinations of children with congenital malformations. While a reduced relative performance capacity has already been found for esophageal atresia and anorectal malformation patients,12,13 the cardiopulmonary performance has only been described once for patients with AWDs.14 Zaccara and coworkers examined 18 patients with large AWDs (GS > 4 cm, OC > 6 cm) who have completed a stress test consisting of running on a treadmill with a stepwise increase in workload until exhaustion. The authors measured time of exercise (TE) and maximal oxygen consumption (VO2max) during the whole exercise as well as heart rate and blood pressure at baseline (HR and BP) and the end of the exercise (HRmax and BPmax). AWD patients reached HRmax after a significantly shorter TE and VO2max was significantly lower compared to a healthy pediatric population. The authors, however, suggested that their findings may result from being unfit instead of the illness per se and concluded that further investigations are necessary. Our results did not show any differences in the studied parameters of cardiopulmonary exercise performance testing comparing AWD patients to healthy controls.
The Dordel-Koch-Test has been used in the literature before to assess the locomotor function in patients with congenital anomalies such as anorectal malformations.12 The AWD cohort had significantly higher values revealing worse locomotor function compared to the control group (compare Table 3). Especially the exercises “sit up” and “lateral jumping” which are related to core muscle activity revealed significantly worse scores. This might be related to a functional disability of the abdominal wall muscles. Nevertheless, the clinical relevance and impact of the numerical differences in real life remain unclear. The questions whether or not AWD patients may benefit from long-term follow-up combined with targeted physical therapy has to be answered in future studies.
Neither gait and stance analyses nor electromyography of the abdominal wall muscles have been performed in AWD patients before. Gait analysis is used for children with cerebral palsy and surface electromyography plays an important role for instance when diagnosing neuromuscular, urodynamic or laryngeal disorders.34,35,36,37,38 However, we could not find any significant differences suggesting that there are no long-term sequelae in muscle activation and innervation of abdominal wall muscles in AWD patients. Additionally, the sonographic thickness measurement of the abdominal wall revealed no significant difference between the AWD and control group confirming the hypothesis that the structure of the abdominal wall muscles develops normally in people born with an AWD. These two findings could be communicated to parents of affected patients in order to dispel concerns about long-term outcome regarding the muscular abdominal wall. A potential functional disability of the abdominal wall muscles as suggested by the differences in parts of the DKT has to be clarified in future studies.
QoL consists of social and physical well-being and might be affected by gastrointestinal disorders in patients born with an AWD. Previous studies have already assessed the quality of life of AWD patients using the pediatric quality of life inventory (PedQoL) and in one of these studies differences in young adults have been found.11,39,40 It has also been described that 25% of patients with AWD suffer from chronic abdominal complaints maybe due to intraabdominal adhesions.40 To the best of our knowledge, our study is first one to apply the GIQLI for patients with AWDs. In the AWD group, we found a statistically significant lower score of GIQLI. Therefore, gastrointestinal disorders may affect patients following AWD repair through child- and adulthood in daily life. These findings and their real-life impact, however, have to be re-examined in studies with a larger group of patients. Nevertheless, we did not find any significant differences between the AWD group and controls concerning stool frequency or consistency.
Cosmetic satisfaction is of pivotal importance for patients who have undergone AWD repair and additional abdominal surgery due to complications. Especially, the dissatisfaction because of an abnormal/lacking umbilicus is a major issue; almost half of AWD patients experience psychological stress if they do not have an umbilicus.5,41 In our population, however, more than two thirds of the patients (71%) rated the overall quality and appearance of their scar as quite good (PSAS overall opinion: 3.9 ± 2.8) and we found no significant correlation between an absent umbilicus and cosmetic satisfaction. However, cosmetic satisfaction may change over time and might be a concern with growing age. Umbilicus reconstruction is often performed at a higher age.5,41,42,43
A limitation of our study is the relatively small sample size of 18 patients. Additionally, 5 out of 18 children were not able to complete CPET due to their height and in 4 out of 18 it was not possible to detect muscle mass due to technical reasons and low weight of the patients. However, in orphan pediatric diseases it is difficult to obtain large sample sizes and therefore possible statistically significant difference may be missed due to the small sample size. An additional limitation is that AWDs are heterogenous diseases and therefore our findings observed in a relatively small number of patients with heterogenous diseases are confounded by a certain lack of power. Moreover, even though the values for DKT and GIQLI were statistically significantly different between AWD patients and controls, the impact of these difference for real life remains unclear. Strengths of this study, however, are a mean long-term follow-up of 13 years ranging from 7 to 18 years and the inclusion of an age-, sex-, BMI- and physical activity matched control group.
In conclusion, we present the feasibility of an extensive long-term follow-up examinations of AWD patients. We found decreased motor abilities and GIQLI scores while cardiopulmonary function was not different compared to healthy controls. However, due to the limited number of patients in our pilot study, larger ideally multicentric studies are mandatory in order to confirm our results.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Jones, A. M. et al. Increasing prevalence of gastroschisis-−14 States, 1995-2012. MMWR Morb. Mortal. Wkly. Rep. 65, 23–26 (2016).
Loane, M., Dolk, H., Bradbury, I. & Group, E. W. Increasing prevalence of gastroschisis in Europe 1980–2002: A phenomenon restricted to younger mothers? Paediatr. Perinat. Epidemiol. 21, 363–369 (2007).
Springett, A. et al. Birth prevalence and survival of exomphalos in England and Wales: 2005 to 2011. Birth Defects Res. A Clin. Mol. Teratol. 100, 721–725 (2014).
Stallings, E. B. et al. Population-based birth defects data in the United States, 2012-2016: A focus on abdominal wall defects. Birth Defects Res. 111, 1436–1447 (2019).
Gamba, P. & Midrio, P. Abdominal wall defects: Prenatal diagnosis, newborn management, and long-term outcomes. Semin. Pediatr. Surg. 23, 283–290 (2014).
Corey, K. M. et al. Frequency of anomalies and hospital outcomes in infants with gastroschisis and omphalocele. Early Hum. Dev. 90, 421–424 (2014).
Arnold, H. E. et al. Short-term and family-reported long-term outcomes of simple versus complicated gastroschisis. J. Surg. Res. 224, 79–88 (2018).
Tullie, L. G. et al. Umbilical hernia following gastroschisis closure: A common event? Pediatr. Surg. Int. 32, 811–814 (2016).
Kaiser, M. M., Kahl, F., von Schwabe, C. & Halsband, H. [Omphalocele and gastroschisis. outcome–complications–follow-up–quality of life]. Chirurg 71, 1256–1262 (2000).
Harris, E. L. et al. The long term physical consequences of gastroschisis. J. Pediatr. Surg. 49, 1466–1470 (2014).
Snoep, M. C. et al. Gastro-intestinal function and quality of life are favorable in adolescent and adult gastroschisis patients. Early Hum. Dev. 141, 104936 (2020).
Arneitz, C. et al. Cardiorespiratory performance and locomotor function of patients with anorectal malformations. Sci. Rep. 11, 18919 (2021).
Arneitz, C. et al. Cardiorespiratory performance capacity and airway microbiome in patients following primary repair of esophageal atresia. Pediatr. Res. 90, 66–73 (2021).
Zaccara, A. et al. Cardiopulmonary performances in young children and adolescents born with large abdominal wall defects. J. Pediatr. Surg. 38, 478–481 (2003). discussion 478-481.
Barr, K. P., Griggs, M. & Cadby, T. Lumbar stabilization: core concepts and current literature, part 1. Am. J. Phys. Med. Rehabil. 84, 473–480 (2005).
Bergholz, R., Boettcher, M., Reinshagen, K. & Wenke, K. Complex gastroschisis is a different entity to simple gastroschisis affecting morbidity and mortality-a systematic review and meta-analysis. J. Pediatr. Surg. 49, 1527–1532 (2014).
Arnold, M. A. et al. Risk stratification of 4344 patients with gastroschisis into simple and complex categories. J. Pediatr. Surg. 42, 1520–1525 (2007).
Laje, P. et al. Complex gastroschisis: Clinical spectrum and neonatal outcomes at a referral center. J. Pediatr. Surg. 53, 1904–1907 (2018).
Baerg, J. E. & Munoz, A. N. Long term complications and outcomes in omphalocele. Semin Pediatr. Surg. 28, 118–121 (2019).
Nolan, H. R., Wagner, M. L., Jenkins, T. & Lim, F. Y. Outcomes in the giant omphalocele population: A single center comprehensive experience. J. Pediatr. Surg. 55, 1866–1871 (2020).
Skrabal, F. et al. The Combyn ECG: adding haemodynamic and fluid leads for the ECG. Part II: prediction of total body water (TBW), extracellular fluid (ECF), ECF overload, fat mass (FM) and “dry” appendicular muscle mass (AppMM). Med. Eng. Phys. 44, 44–52 (2017).
Jat, K. R. Spirometry in children. Prim. Care Respir. J. 22, 221–229 (2013).
Windhaber, J. et al. Bicycle spiroergometry: comparison of standardized examination protocols for adolescents: is it necessary to define own standard values for each protocol? Eur. J. Appl Physiol. 121, 1783–1794 (2021).
Fletcher, G. F. et al. Exercise standards for testing and training: A Scientific Statement from the American Heart Association. Circulation 128, 873–934 (2013).
Mezzani, A., Corra, U., Bosimini, E., Giordano, A. & Giannuzzi, P. Contribution of peak respiratory exchange ratio to peak Vo2 prognostic reliability in patients with chronic heart failure and severely reduced exercise capacity. Am. Heart J. 145, 1102–1107 (2003).
Jouck, S., Koch, B., Graf, C., Predel, H. G. & Dordel, S. Dordel-Koch-Test (Dkt) – Zur Erfassung Der Motorischen Basisfunktionen Im Kindes- Und Jugendalter; Erste Ergebnisse Der Normierung. Aktuelle Ernährungsmedizin 31, P27 (2006).
Ng, J. K., Kippers, V., Parnianpour, M. & Richardson, C. A. Emg activity normalization for trunk muscles in subjects with and without back pain. Med. Sci. Sports Exerc 34, 1082–1086 (2002).
Eypasch, E. et al. Gastrointestinal quality of life index: development, validation and application of a new instrument. Br. J. Surg. 82, 216–222 (1995).
Lewis, S. J. & Heaton, K. W. Stool form scale as a useful guide to intestinal transit time. Scand. J. Gastroenterol. 32, 920–924 (1997).
Van de Kar, A. L. et al. Reliable and feasible evaluation of linear scars by the patient and observer scar assessment scale. Plast. Reconstr. Surg. 116, 514–522 (2005).
Draaijers, L. J. et al. The patient and observer scar assessment scale: A reliable and feasible tool for scar evaluation. Plast. Reconstr. Surg. 113, 1960–1965 (2004). discussion 1966-1967.
Duggan, E. & Puligandla, P. S. Respiratory disorders in patients with omphalocele. Semin Pediatr. Surg. 28, 115–117 (2019).
Ortega, F. B., Ruiz, J. R., Castillo, M. J. & Sjostrom, M. Physical fitness in childhood and adolescence: A powerful marker of health. Int J. Obes. (Lond.) 32, 1–11 (2008).
Armand, S., Decoulon, G. & Bonnefoy-Mazure, A. Gait analysis in children with cerebral palsy. EFORT Open Rev. 1, 448–460 (2016).
Aragon-Ramos, P., Garcia-Lopez, I., Santiago, S., Martinez, A. & Gavilan, J. Laryngeal electromyography, a useful tool in difficult cases of pediatric laryngeal mobility disorders. Int J. Pediatr. Otorhinolaryngol. 161, 111264 (2022).
Higashihara, M. et al. Quantitative analysis of surface electromyography for pediatric neuromuscular disorders. Muscle Nerve 58, 824–827 (2018).
Maizels, M. & Firlit, C. F. Pediatric urodynamics: A clinical comparison of surface versus needle pelvic floor/external sphincter electromyography. J. Urol. 122, 518–522 (1979).
Irumudomon, O. T. & Ghosh, P. S. Electromyography in infants: Experience from a pediatric neuromuscular center. Acta Neurol. Belg. 122, 1195–1200 (2022).
Hijkoop, A. et al. Gastroschisis at school age: What do parents report? Eur. J. Pediatr. 178, 1405–1412 (2019).
van Eijck, F. C., Wijnen, R. M. & van Goor, H. The incidence and morbidity of adhesions after treatment of neonates with gastroschisis and omphalocele: A 30-year review. J. Pediatr. Surg. 43, 479–483 (2008).
Bongini, M., Tanini, S., Messineo, A., Facchini, F. & Ghionzoli, M. Umbilical reconstruction in children: A simplified operative technique. Aesthetic Plast. Surg. 39, 414–417 (2015).
Gardani, M. et al. Umbilical reconstruction: Different techniques, a single aim. Acta Biomed. 90, 504–509 (2019).
Lee, Y., Lee, S. H. & Woo, K. V. Umbilical reconstruction using a modified inverted C-V Flap With Conjoint Flaps. J. Plast. Surg. Hand Surg. 47, 334–336 (2013).
Funding
Parts of the project were funded by the Doctoral School “Bone, Muscle and Joint” of the Medical University of Graz.
Author information
Authors and Affiliations
Contributions
The authors confirm contribution to the paper as follows: C.F., MD: study conception and design, data collection. draft manuscript preparation. J.W., MD: study conception and design, data collection, draft manuscript preparation. P.G., MD, PhD: draft manuscript preparation. C.C., MD: study conception and design, draft manuscript preparation. S.T., Prof: study conception and design, draft manuscript preparation. B.M., MD: draft manuscript preparation. V.W., MD draft manuscript preparation. G.S., Prof: study conception and design, draft manuscript preparation: H.T., Prof.: study conception and design, draft manuscript preparation: All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Approved by the institutional review board (EK 31–338 ex 18/19).
Consent statement
Informed written consent was obtained from all patients and controls and/or their legal guardians.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Flucher, C., Windhaber, J., Gasparella, P. et al. Long-term motor activity, cardiopulmonary performance and quality of life in abdominal wall defect patients. Pediatr Res 95, 1101–1109 (2024). https://doi.org/10.1038/s41390-023-02900-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02900-y