Abstract
Background
Pediatric resuscitation guidelines recommend continuous chest compression with asynchronized ventilation (CCaV) during cardiopulmonary resuscitation. We recently described that providing a constant high distending pressure, or sustained inflation (SI) while performing continuous chest compressions (CC = CC + SI) reduces time to return of spontaneous circulation (ROSC) in neonatal and pediatric piglets with asphyxia-induced cardiac arrest.
Methods
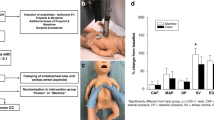
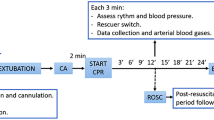
To determine if CC + SI compared to CCaV will improve frequency of achieving ROSC and reduce time to ROSC in asphyxiated pediatric piglets. Twenty-eight pediatric piglets (21–24 days old) were anesthetized and asphyxiated by clamping the endotracheal tube. Piglets were randomized to CC + SI or CCaV for resuscitation (n = 14/group). Heart rate, arterial blood pressure, carotid blood flow, cerebral oxygenation, and respiratory parameters were continuously recorded throughout the experiment.
Results
The mean(SD) duration of resuscitation was significantly reduced with CC + SI compared to CCaV with 208(190) vs. 388(258)s, p = 0.045, respectively. The number of piglets achieving ROSC with CC + SI and CCaV were 12/14 vs. 6/14, p = 0.046. Minute ventilation, end-tidal carbon dioxide, ventilation rate, and positive end expiratory pressures were also significantly improved with CC + SI.
Conclusions
CC + SI improves duration of resuscitation and increases number of piglets achieving ROSC secondary to improved minute ventilation.
Impact
-
Chest compressions superimposed with sustained inflation resulted in shorter duration of resuscitation
-
Chest compressions superimposed with sustained inflation resulted in higher number of piglets achieving return of spontaneous circulation
-
Further animal studies are needed to examine chest compressions superimposed with sustained inflation
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during the current study are available from the corresponding author on reasonable request.
References
Topjian, A. A. et al. Part 4: Pediatric basic and advanced life support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 142, https://doi.org/10.1161/CIR.0000000000000901 (2020).
Soar, J. et al. 2019 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations: Summary from the Basic Life Support; Advanced Life Support; Pediatric Life Support; Neonatal Life Support; Education, Implementation, and Teams; and First Aid Task Forces. Circulation 140, https://doi.org/10.1161/CIR.0000000000000734 (2019)
Kitamura, T. et al. Conventional and chest-compression-only cardiopulmonary resuscitation by bystanders for children who have out-of-hospital cardiac arrests: a prospective, nationwide, population-based cohort study. Lancet 375, 8 (2010).
Sutton, R. M. et al. Ventilation rates and pediatric in-hospital cardiac arrest survival outcomes*. Crit. Care Med. 47, 1627–1636 (2019).
Schmölzer G. M. et al. Sustained inflation during chest compression: a new technique of pediatric cardiopulmonary resuscitation that improves recovery and survival in a pediatric porcine model. J. Am. Heart Assoc. 10, https://doi.org/10.1161/JAHA.120.019136 (2021).
Schmölzer, G. M. et al. Cardiopulmonary resuscitation with chest compressions during sustained inflations: a new technique of neonatal resuscitation that improves recovery and survival in a neonatal porcine model. Circulation 128, 2495–2503 (2013).
Schmölzer, G. M. Chest compressions during sustained inflation during cardiopulmonary resuscitation in newborn infants translating evidence from animal studies to the bedside. JACC Basic Transl. Sci. 4, 116–121 (2019).
Li, E. S. et al. Chest compressions during sustained inflations improve recovery when compared to a 3:1 compression:ventilation ratio during cardiopulmonary resuscitation in a neonatal Porcine Model of Asphyxia. Neonatology 112, 337–346 (2017).
Li, E. S. et al. Return of spontaneous circulation is not affected by different chest compression rates superimposed with sustained inflations during cardiopulmonary resuscitation in newborn piglets. PLoS ONE 11, e0157249 (2016).
Mustofa, J. et al. Effects of different durations of sustained inflation during cardiopulmonary resuscitation on return of spontaneous circulation and hemodynamic recovery in severely asphyxiated piglets. Resuscitation 129, 82–89 (2018).
Schmölzer, G. M., O. Reilly, M., Fray, C., van Os, S. & Cheung, P. Y. Chest compression during sustained inflation versus 3:1 chest compression:ventilation ratio during neonatal cardiopulmonary resuscitation: a randomised feasibility trial. Arch. Dis. Child Fetal Neonatal Ed. 103, F455–F460 (2018).
Xanthos, T. et al. Baseline hemodynamics in anesthetized landrace–large white swine: reference values for research in cardiac arrest and cardiopulmonary resuscitation models. J. Am. Assoc. Lab. Anim. Sci. 46, 5 (2007).
Kilkenny C., Browne W., Cuthill I., Emerson M., & Aktman D. Improving bioscience research reporting: The ARRIVE Guidelines for Reporting Animal Research. PLOS Biol. 8, e1000412 (2010)
van Os, S. et al. Exhaled carbon dioxide can be used to guide respiratory support in the delivery room. Acta Paediatr. 103, 796–806 (2014).
Baik, N. et al. Reference ranges for cerebral tissue oxygen saturation index in term neonates during immediate neonatal transition after birth. Neonatology 108, 283–286 (2015).
Wollborn, J. et al. Standardized model of porcine resuscitation using a custom-made resuscitation board results in optimal hemodynamic management. Am. J. Emerg. Med. 36, 1738–1744 (2018).
Okubo, M., Chan, H. K., Callaway, C. W., Mann, N. C. & Wang, H. E. Characteristics of paediatric out-of-hospital cardiac arrest in the United States. Resuscitation 153, 227–233 (2020).
Jayaram, N., McNally, B., Tang, F. & Chan, P. S. Survival after out‐of‐hospital cardiac arrest in children. J. Am. Heart Assoc. 4, e002122 (2015).
Sutton, R. M. et al. Effect of physiologic point-of-care cardiopulmonary resuscitation training on survival with favorable neurologic outcome in cardiac arrest in pediatric icus: a randomized clinical trial. JAMA 327, 934 (2022).
Manrique, G. et al. Comparison between synchronized and non-synchronized ventilation and between guided and non-guided chest compressions during resuscitation in a pediatric animal model after asphyxial cardiac arrest. PLoS ONE 14, e0219660 (2019).
Sutton, R. M. et al. Hemodynamic-directed cardiopulmonary resuscitation during in-hospital cardiac arrest. Resuscitation 85, 983–986 (2014).
Lautz, A. J. et al. Hemodynamic-directed cardiopulmonary resuscitation improves neurologic outcomes and mitochondrial function in the heart and brain. Crit. Care Med. 47, e241–e249 (2019).
O’Brien, C. E. et al. Use of an end-tidal carbon dioxide-guided algorithm during cardiopulmonary resuscitation improves short-term survival in paediatric swine. Resusc. Plus 8, 100174 (2021).
Morgan, R. W. et al. A hemodynamic-directed approach to pediatric cardiopulmonary resuscitation (HD-CPR) improves survival. Resuscitation 111, 41–47 (2017).
Kern, K. B., Ewy, G. A., Voorhees, W. D., Babbs, C. F. & Tacker, W. A. Myocardial perfusion pressure: A predictor of 24-hour survival during prolonged cardiac arrest in dogs. Resuscitation 16, 241–250 (1988).
Halperin, H. R. et al. Determinants of blood flow to vital organs during cardiopulmonary resuscitation in dogs. Circulation 73, 539–550 (1986).
Berg, R. A. et al. Adverse hemodynamic effects of interrupting chest compressions for rescue breathing during cardiopulmonary resuscitation for ventricular fibrillation cardiac arrest. Circulation 104, 2465–2470 (2001).
Ewy, G. A. et al. Improved neurological outcome with continuous chest compressions compared with 30:2 compressions-to-ventilations cardiopulmonary resuscitation in a realistic swine model of out-of-hospital cardiac arrest. Circulation 116, 2525–2530 (2007).
Pearson, J. W. Influence of peripheral vascular tone on cardiac resuscitation. Anesth. Analg. 44, 746 (1965).
Berg, R. A. et al. Association between diastolic blood pressure during pediatric in-hospital cardiopulmonary resuscitation and survival. Circulation 137, 1784–1795 (2018).
Rudikoff, M. T., Freund P., & Weisfeldt M. L. Mechanisms of blood flow during cardiopulmonary resuscitation. Circulation 61, 8 (1980).
Chandra, N., Rudikoff, M. & Weisfeldt, M. L. Simultaneous chest compression and ventilation at high airway pressure during cardiopulmonary resuscitation. Lancet 26, 175–178 (1980).
Berkowitz, I. D. et al. Blood flow during cardiopulmonary resuscitation with simultaneous compression and ventilation in infant pigs. Pediatr. Res. 26, 558–559 (1989).
Aufderheide, T. P. et al. Hyperventilation-induced hypotension during cardiopulmonary resuscitation. Circulation 109, 1960–1965 (2004).
de Caen, A. R. et al. Part 12: pediatric advanced life support: 2015 American Heart Association Guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 132, S525–S542 (2015).
McInnes, A. D. et al. The first quantitative report of ventilation rate during in-hospital resuscitation of older children and adolescents. Resuscitation 82, 1025–1029 (2011).
Li, E. S., Cheung, P. Y., O’Reilly, M. & Schmölzer, G. M. Change in tidal volume during cardiopulmonary resuscitation in newborn piglets. Arch. Dis. Child Fetal Neonatal Ed. 100, F530–F533 (2015).
Shim, G. H. et al. Effects of sustained inflation pressure during neonatal cardiopulmonary resuscitation of asphyxiated piglets. PLoS ONE 15, e0228693 (2020).
Berg, R. A. et al. End-tidal carbon dioxide during pediatric in-hospital cardiopulmonary resuscitation. Resuscitation 133, 173–179 (2018).
Hamrick, J. T. et al. End-tidal CO2–guided chest compression delivery improves survival in a neonatal asphyxial cardiac arrest model*. Pediatr. Crit. Care Med. 18, e575–e584 (2017).
Nicoll, J. et al. Effect of cardiac output changes on exhaled carbon dioxide in newborn piglets. Resuscitation 84, 1439–1442 (2013).
Funding
We would like to thank the public for donating money to our funding agencies: This research has been facilitated by the Women and Children’s Health Research Institute through the generous support of the Stollery Children’s Hospital Foundation.
Author information
Authors and Affiliations
Contributions
Conception and design: G.M.S., P.Y.C., M.O.R., T.F.L. Collection and assembly of data: G.M.S., P.Y.C., M.O.R., T.F.L., C.M.D.M. Analysis and interpretation of the data: G.M.S., P.Y.C., M.O.R., T.F.L., C.M.D.M. Drafting of the article: G.M.S., P.Y.C., M.O.R., T.F.L., C.M.D.M. Critical revision of the article for important intellectual content: G.M.S., P.Y.C., M.O.R., T.F.L., C.M.D.M. Final approval of the article: G.M.S., P.Y.C., M.O.R., T.F.L., C.M.D.M.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Morin, C.M.D., Cheung, PY., Lee, TF. et al. Chest compressions superimposed with sustained inflations during cardiopulmonary resuscitation in asphyxiated pediatric piglets. Pediatr Res 95, 988–995 (2024). https://doi.org/10.1038/s41390-023-02563-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02563-9