Abstract
Background
The functional acute kidney injury (AKI) diagnostic tests serum creatinine (SCr) and urine output are imprecise and make management challenging. Combining tubular injury biomarkers with functional markers reveal AKI phenotypes that may facilitate personalized care. However, when and in whom to obtain injury biomarkers remains unclear.
Methods
This was a prospective, observational study of patients admitted to a pediatric intensive care unit (PICU). Using the Renal Angina Index (RAI), subjects were screened for the presence (RAI+) or absence (RAI−) of renal angina 12 h post-admission and assigned an AKI phenotype using urinary NGAL (NGAL+: ≥150 ng/ml) and SCr (SCr+: ≥KDIGO Stage 1). Outcomes for each AKI phenotype were assessed and compared by RAI status.
Results
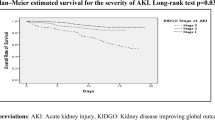
In all, 200/247 (81%) subjects were RAI+. RAI+ subjects who were NGAL+ had higher risk of Day 3 AKI, renal replacement therapy use, and mortality and fewer ventilator- and PICU-free days, compared to NGAL−, irrespective of Day 0 SCr. Similar findings were not demonstrated in RAI− subjects, though NGAL+/SCr+ was associated with fewer ventilator- and PICU-free days compared to NGAL−/SCr+.
Conclusions
NGAL- and SCr-based AKI phenotypes provide improved prognostic information in children with renal angina (RAI+) and/or with SCr elevation. These populations may be appropriate for targeted biomarker testing.
Impact
-
New consensus recommendations encourage the integration of kidney tubular injury biomarkers such as urinary NGAL with serum creatinine for diagnosis and staging of acute kidney injury; however, no structured testing framework exists guiding when to test and in whom.
-
Urinary NGAL- and serum creatinine-based acute kidney injury phenotypes increase diagnostic precision in critically ill children experiencing renal angina (RAI+) or serum creatinine-defined acute kidney injury.
-
These data provide preliminary evidence for a proposed framework for directed urinary NGAL assessment in the pediatric intensive care unit.
Similar content being viewed by others
Introduction
Acute kidney injury (AKI) occurs commonly in critically ill children and is associated with poor outcomes, including mortality, increased resource utilization, and reduced health-related quality of life after admission.1,2,3,4 Unfortunately, management of patients with AKI is challenging, as effective disease-modifying therapies have yet to be identified.5 In order to advance the care of AKI, a more precise and timelier framework for detection and characterization of ongoing injury in affected patients is required.
The use of kidney tubular injury biomarkers such as neutrophil gelatinase-associated lipocalin (NGAL) may help improve timeliness and precision of AKI diagnosis. NGAL is a 25 kDa protein released by the injured distal nephron, and concentrations are typically low in the urine and rise quickly in response to tubular injury.6 Expert consensus has called for the integration of NGAL and other injury biomarkers with serum creatinine (SCr) (i.e., a marker of excretory function or glomerular filtration rate (GFR)) to refine the AKI diagnosis,7,8,9 and several groups have operationalized this concept with promising results.10,11,12 Notably, the use of urinary NGAL in concert with SCr to derive different AKI phenotypes (Fig. 1) helps distinguish between patients with transient/functional (i.e., injury biomarker negative) and persistent, damage-associated (i.e., injury biomarker positive) SCr elevation and identifies a previously unrecognized subset of patients with ongoing tubular injury who do not yet have SCr elevation (i.e., subclinical AKI).7,10,12,13,14 The increasing evidence supporting the added prognostic value of injury biomarkers to SCr data for AKI diagnosis has resulted in experts recommending their inclusion in AKI staging definitions.9
Successful translation of these injury biomarkers to clinical practice will require pragmatic and evidence-based guidance on their use. We have previously demonstrated that directed use of injury biomarkers in those at risk for severe AKI is feasible and improves precision of the AKI diagnosis,15,16 using the validated risk stratification tool the Renal Angina Index (RAI). Calculated 12 h after pediatric intensive care unit (PICU) admission, the RAI incorporates AKI risk and injury criteria (Supplementary Fig. 1), with a score of ≥8 identifying children with renal angina at high risk for severe AKI 72 h later (RAI+).17,18 An assessment of the SCr and injury biomarker based AKI phenotypes (Fig. 1) exclusively in this high-risk subset of RAI+ patients (i.e., those who may be most appropriate for injury biomarker testing) has not yet been performed.
Thus, we aimed to assess the incidence and differential outcomes of the four different NGAL- and SCr-based AKI phenotypes in RAI+ patients, and we hypothesized that elevation in urinary NGAL would be associated with poor outcomes irrespective of SCr. Secondarily, when data were available to do so, we also sought to examine the incidence and outcomes of these AKI phenotypes in a cohort of RAI− (RAI < 8) patients. We hypothesized a priori that the distribution of the AKI phenotypes would differ in RAI− compared to RAI+ patients but that elevation in urinary NGAL would continue to be associated with poor outcomes.
Methods
Study design and subjects
We performed a single-center, prospective, observational cohort study of children and young adults aged 1 month–25 years who were admitted to a quaternary PICU for at least 48 h from 2017 through 2020. This study was approved by the Cincinnati Children’s Hospital Medical Center (CCHMC) Institutional Review Board with a waiver of informed consent. The following criteria were required for study inclusion: (1) an available RAI score calculated appropriately at 12-h post-PICU admission, (2) an available urine NGAL and SCr measured within 24 h of RAI calculation, and (3) available PICU Day 3 SCr data. Patients were excluded if they had chronic kidney disease, were requiring renal replacement therapy (RRT) at the time of PICU admission, or if they were admitted post-operatively following a kidney transplant. To facilitate enrollment, we leveraged an ongoing study at CCHMC (TAKING FOCUS 2, NCT03541785) that operationalizes automated RAI calculation by the electronic medical record (EMR), with a reflex order for urine NGAL released if the patient “rules in” for renal angina (RAI ≥ 8, RAI+).19 Patients were screened for enrollment by N.L.S. in one of the two ways: (1) via e-mail notification when a patient was RAI+ (i.e., already undergoing NGAL assessment automatically), and (2) via EMR query of patients admitted to the PICU with an RAI < 8 (RAI−) who had a urine NGAL sent within 48 h for clinical use based on provider discretion. A flow diagram outlining patient screening and enrollment is outlined in Fig. 2. Once enrolled, clinical and laboratory data were collected daily during PICU admission for up to 7 days; mortality, duration of mechanical ventilation, and duration of PICU stay were tracked for 28 days after enrollment.
In all, 741 consecutive patients meeting inclusion criteria were reviewed from April 2017 to December 2020. A total of 553 fulfilled criteria for renal angina (RAI+) and thus had reflex urinary NGAL samples automatically collected. The remaining 188 did not have renal angina (RAI−) and were included because a urinary NGAL was ordered as part of clinical care by the medical team. After exclusion criteria were applied, a total of 247 patients (200 RAI+, 47 RAI−) remained for inclusion in the analyses.
Definitions and measurements
The RAI was calculated for each patient by the EMR using clinical and demographic data from the first 12 h of PICU admission (Supplementary Fig. 1).17,18 Based on previous literature, children with an RAI of ≥8 were deemed high risk for severe AKI 3 days later and termed RAI+; those with an RAI <8 were termed RAI−.17,18
Subjects were classified as one of the four individual AKI phenotypes based on SCr and urine NGAL concentrations: NGAL−/SCr− (no AKI), NGAL+/SCr− (subclinical AKI), NGAL−/SCr+ (functional AKI), or NGAL+/SCr+ (damage-associated AKI) (Fig. 1)12,20,21 on the day of PICU admission (Day 0). If more than one SCr value was available on Day 0, the value closest to the RAI calculation at 12 h post-admission was utilized. Patients were classified as SCr+ if they had Kidney Diseases Improving Global Outcomes (KDIGO) stage 1 AKI or higher by SCr (≥1.5× baseline)22; they were termed NGAL+ if they had a urine NGAL concentration ≥150 ng/ml.12,16 Baseline SCr was identified using the lowest SCr value in the 3 months leading up to PICU admission. For subjects without documented baseline SCr values (n = 90), estimated values were calculated using their using their body surface area (m2) and an estimated GFR of 120 ml/min per 1.73 m2, as previously validated in the pediatric literature.1,23
The primary analyses focused on examining the association between Day 0 AKI phenotype and outcomes in both RAI+ and RAI− patients. Our primary outcome of interest was Day 3 severe AKI, which was defined as KDIGO stage 2 AKI or higher by SCr criteria only (≥2× baseline).22 Secondary outcomes of interest included the development of >10% cumulative fluid balance (FB) at Day 3, need for RRT in the first 7 days, ventilator-free and PICU-free days (at Day 28 following PICU admission), and PICU mortality. Cumulative FB percent was calculated using the previously published formula: %FB = [(Total Fluid In (L) − Total Fluid Out (L))/Admission Weight (kg)] × 100%.24
Data analysis
Given the lack of data regarding the incidence and outcomes for the different NGAL- and SCr-based AKI phenotypes in RAI+ children, it was determined a priori that 200 RAI+ patients would be included in this pilot study, consistent with a previously published sample size.12 Similarly, it was determined a priori that we would enroll all RAI− patients meeting criteria for comparison during the study period (2017–2020), recognizing that the number of patients in this group would likely be lower. After inclusion and exclusion criteria were applied, a total of 247 (200 RAI+ and 47 RAI−) patients were included in the final cohort.
Data were described using medians, interquartile ranges, frequencies, and percentages. Comparisons between groups were performed using Wilcoxon rank sum, Chi-square, or Fisher exact test, as appropriate. For categorical outcomes, relative risk calculations were performed for inter-group comparison. Chi-square testing was performed to assess for a difference in the distribution of AKI phenotypes between RAI+ and RAI− patients. For RAI+ patients, we also sought to assess the additive value of NGAL measurement for outcome prediction. To do this, we used logistic regression to assess the independent impact of NGAL elevation on the development of Day 3 severe AKI, need for RRT in the first 7 days, and mortality, after adjusting for potential confounders and/or covariates identified on bivariate analysis. Potential confounders and/or covariates considered included patient age, severity of illness by Pediatric Risk of Mortality Score III (PRISM III),25,26 number of comorbidities documented for the patient, number of nephrotoxic medications received on Day 0 (see Supplemental Methods), and Day 0 AKI Stage by KDIGO SCr criteria. Variables with an alpha level <0.15 on bivariate analysis were included in the multivariable logistic regression model for each outcome. All statistical analyses were performed using Sigmaplot 14.5 (Systat Software Inc., San Jose, CA).
Results
Baseline characteristics
The study cohort consisted of 247 patients, 200 (81%) of whom were RAI+ (Fig. 2). Forty-seven (19%) were RAI− and thus were eligible for inclusion since they had an NGAL result obtained as part of clinical care by the ICU providers. Table 1 outlines basic clinical, demographic, and outcome data for RAI+ vs. RAI− patients. RAI+ patients had higher PRISM III scores, higher risk of any and severe AKI on Day 3, as well as higher risk of requiring mechanical ventilation when compared to RAI− patients. There were no other differences in outcomes between the RAI+ and RAI− patients.
AKI phenotype assessment in patients fulfilling renal angina criteria (RAI+)
Day 0 NGAL and SCr values classified the unique AKI phenotypes for RAI+ patients: NGAL−/SCr− (n = 54, 27%), NGAL+/SCr− (n = 11, 5.5%), NGAL−/SCr+ (n = 44, 22%), and NGAL+/SCr+ (n = 91, 45.5%). There were no baseline demographic or clinical differences between NGAL+/SCr− and NGAL−/SCr− patients on Day 0 (Table 2). However, NGAL+/SCr− patients had increased risk of >10% cumulative fluid balance at Day 3 (relative risk (RR) 2.9, 95% confidence interval (C.I.) 1.5–5.6, p = 0.011) and 10 fewer ventilator-free days (p = 0.011) compared to NGAL−/SCr− patients.
Similarly, Table 3 depicts demographic, clinical, and outcome data for Day 0 SCr+ patients by NGAL status. NGAL+/SCr+ patients had higher PRISM III scores compared to NGAL−/SCr+ patients. NGAL+/SCr+ patients had increased risk for any AKI (RR 1.9, 95% C.I. 1.4–2.6, p < 0.001) and severe AKI (RR 2.5, 95% C.I. 1.5–4.1, p < 0.001) at Day 3, RRT use (RR 5.8, 95% C.I. 1.4–23.5, p = 0.005), fewer ventilator-free days (p = 0.004) and PICU-free days (p < 0.001), compared to NGAL−/SCr+ patients.
Impact of NGAL positivity on outcomes in patients fulfilling renal angina criteria (RAI+)
NGAL+ patients had higher PRISM III scores, were more likely to have sepsis, and had more baseline comorbidities (Supplementary Table 1). NGAL+ patients were also more likely to have AKI at Day 3, require RRT, suffer 28-day mortality, and have fewer ventilator-free and PICU-free days (Supplementary Table 1). The association of Day 0 NGAL+ on outcomes for RAI+ patients is outlined in Table 4. After adjustment for significant covariates identified on bivariate analyses for each outcome, NGAL+ status conferred an incremental risk of severe Day 3 AKI (adjusted odds ratio (OR) 3.8, 95% C.I. 1.6–8.7, p = 0.002) and need for RRT (adjusted OR 4.8, 95% C.I. 1.3–17.8, p = 0.019) and was the strongest independent predictor of both outcomes in RAI+ patients. Although NGAL+ status was associated with increased mortality on bivariate analysis, this association was not retained on multivariate regression; PRISM III score and the presence of Day 3 severe AKI (adjusted OR 14.9, 95% C.I. 2.4–95, p = 0.004) were the only retained associated variables with mortality in this cohort.
AKI phenotype assessment in patients without renal angina (RAI−)
Day 0 NGAL and SCr values were also used to classify the unique AKI phenotypes for the 47 RAI− patients. The distribution of these phenotypes differed from the RAI+ cohort (p < 0.001): NGAL−/SCr− (n = 17, 36%), NGAL+/SCr− (n = 12, 26%), NGAL−/SCr+ (n = 11, 23%), and NGAL+/SCr+ (n = 7, 15%). Basic demographic, clinical and outcome data for Day 0 SCr− and Day 0 SCr+ patients by NGAL status are shown in Supplementary Tables 2 and 3, respectively. There was no association between being NGAL+ and poor outcomes in RAI− patients who were SCr− on Day 0 (Supplementary Table 3). Conversely, Day 0 SCr+ patients who were NGAL+ had 7 fewer ventilator-free days (p = 0.048) and 8 fewer PICU-free days (p = 0.021) compared to those who were NGAL− (Supplementary Table 3).
Discussion
We demonstrate that concomitant use of urinary NGAL and SCr to derive unique AKI phenotypes refines AKI diagnosis, particularly in patients who are RAI+ and/or SCr+. Specifically, a urinary NGAL concentration ≥150 ng/ml identifies a subset of RAI+ patients most likely to develop severe AKI at Day 3, irrespective of SCr concentration on admission. Conversely, urinary NGAL measurement in a small subset of RAI− patients does not provide the same prognostic value, except in those with SCr-defined AKI. These data add to the growing body of evidence outlining the clinical utility of urinary NGAL measurement10,11,12,15 and continue to demonstrate the importance of having a framework for identifying high-risk patients in whom thoughtful, targeted biomarker measurement is appropriate and likely to be useful.
Early assessment of individual patient risk for severe, persistent AKI is important given its association with poor outcomes and continued reliance on kidney protection strategies and supportive care as the mainstays of therapy.1,2,3,4 While previous work has demonstrated the early prognostic value of AKI phenotypes,11,12 those studies were performed in all-comers to the ICU, providing no guidance regarding which patients are appropriate for early biomarker measurement. We attempted to address this knowledge gap by utilizing the RAI17,18,27 to assess the potential impact of pre-test probability for severe AKI on the predictive performance of the individual AKI phenotypes. In this cohort, the associations between AKI phenotypes indicative of tubular injury (i.e., damage-associated AKI and subclinical AKI) and poor outcomes were indeed stronger in patients who were RAI+; furthermore, the absence of tubular injury was associated with lower rates of persistent AKI at Day 3, need for RRT, and other poor outcomes, even in the presence of SCr elevation. While the RAI− group was comprised of only 47 patients, similar associations were not observed, except in those with SCr elevation. Taken together, we suggest that RAI+ and/or isolated SCr+ patients are most likely to benefit from tubular injury biomarker assessment to help identify their specific AKI phenotype and improve risk prediction for Day 3 AKI and associated poor outcomes.
Once identified, these AKI phenotypes may help inform care at the bedside. In this cohort, patients who were RAI+ had a 39% incidence of severe AKI at Day 3 of PICU stay, reflecting more than a twofold risk increase compared to RAI− patients. Identifying the specific biomarker-based AKI phenotype in these RAI+ patients may allow for this risk profile to be further refined. For instance, RAI+ patients identified as NGAL-/SCr− can be assigned the lowest-risk category, with the focus being delivery of standard care without unnecessary, low-value interventions given their low risk for progression to severe AKI. Similarly, patients identified as NGAL−/SCr+ could also be stratified into a lower-risk echelon, with a focus on avoidance of unnecessary interventions in response to SCr-defined AKI, as these patients are likely to recover with appropriate maintenance of euvolemia and adequate renal perfusion.28,29 In contrast, the highest-risk patients can be identified as NGAL+/SCr+, as these patients had higher rates of Day 3 AKI, RRT use, and increased resource utilization, compared to other AKI phenotypes. These patients are important to identify to facilitate early and aggressive kidney protection strategies that may improve outcomes,30,31,32 to appropriately allocate the use of high-risk and costly therapies such as RRT, and to inform enrollment of high-risk patients into clinical trials aimed at identifying effective AKI disease-modifying therapies. Although the numbers were small, the risk profile of RAI− patients who were NGAL+/SCr+ was similar, with 57% having Day 3 severe AKI and 29% requiring RRT. These data suggest that a similar approach to management is likely warranted in these patients, despite being deemed low risk by the RAI.
Of note, our data suggest that biomarker screening to identify patients with subclinical AKI (NGAL+/SCr−) may only be clinically useful in those with renal angina fulfillment (RAI+). While there are now substantial data to support the existence and importance of subclinical AKI,11,12,14,21,33 the exact incidence is unknown, and the questions of when to test kidney injury biomarkers and in whom are particularly important, but remain unanswered. While the number of RAI+ patients with subclinical AKI was less than expected (only 5.5% of RAI+ cohort), trends toward higher rates of AKI and worse outcomes were seen in these patients compared to their biomarker negative counterparts. Conversely, although 26% of the RAI− cohort (n = 12) were identified as having subclinical AKI— an incidence more consistent with previous reports12— this designation did not appear to be associated with any AKI-related outcomes. As noted above, while these data suggest using a framework for biomarker testing to identify this phenotype only in RAI+ patients, further study is warranted given the limited sample size.
This study helps provide some preliminary guidance on the specific patient populations in whom tubular injury biomarkers are useful to obtain, an important piece of information given the continued advocacy for their use in clinical practice.9 However, our data has limitations. Given the nature of the study, providers were not blinded to either the RAI or NGAL data, and thus, their values could have informed clinical care and subsequent AKI rates. Additionally, despite a long enrollment period, the number of RAI− patients with NGAL data was comparatively low, and thus conclusions about this specific subset of patients are difficult to draw as the study is likely underpowered in this regard. Finally, as this was an observational study of a new clinical practice in our PICU (i.e., automated RAI screening followed by NGAL assessment if patients were RAI+), there were some initial challenges with fidelity of this intervention that resulted in high drop-out rate related to delayed NGAL data specifically (Fig. 2). Though this improved throughout the study period, we recognize that this could bias our results, as we failed to capture all RAI+ patients in this study. We suggest that future work aims to address these limitations in larger study populations.
Conclusion
In summary, injury biomarker and SCr-based AKI phenotypes provide important prognostic information on ICU admission about an individual patient’s risk for ongoing AKI and associated poor outcomes. The added predictive benefit of this biomarker information appears to be most pronounced in patients with renal angina fulfillment or SCr-defined AKI, thus suggesting that targeted biomarker testing in these specific patient populations is warranted. This work could provide a preliminary framework to help operationalize tubular injury biomarkers into clinical practice.
Data availability
The dataset generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Kaddourah, A., Basu, R. K., Bagshaw, S. M., Goldstein, S. L. & AWARE Investigators. Epidemiology of acute kidney injury in critically ill children and young adults. N. Engl. J. Med. 376, 11–20 (2017).
Jetton, J. G. et al. Incidence and outcomes of neonatal acute kidney injury (AWAKEN): a multicentre, multinational, observational cohort study. Lancet Child Adolesc. Health 1, 184–194 (2017).
Starr, M. C. et al. Severe acute kidney injury is associated with increased risk of death and new morbidity after pediatric septic shock. Pediatr. Crit. Care Med. 21, e686 (2020).
Stanski, N. L. et al. Severe acute kidney injury is independently associated with mortality in children with septic shock. Intensive Care Med. 46, 1050–1051 (2020).
Devarajan, P. The current state of the art in acute kidney injury. Front. Pediatr. 8, 70 (2020).
Singer, E. et al. Neutrophil gelatinase-associated lipocalin: pathophysiology and clinical applications. Acta Physiol. 207, 663–672 (2013).
McCullough, P. A. et al. Implementation of novel biomarkers in the diagnosis, prognosis, and management of acute kidney injury: executive summary from the tenth consensus conference of the Acute Dialysis Quality Initiative (ADQI). Contrib. Nephrol. 182, 5–12 (2013).
Chawla, L. S. et al. Acute kidney disease and renal recovery: consensus report of the Acute Disease Quality Initiative (ADQI) 16 Workgroup. Nat. Rev. Nephrol. 13, 241 (2017).
Ostermann, M. et al. Recommendations on acute kidney injury biomarkers from the Acute Disease Quality Initiative Consensus Conference: A Consensus Statement. JAMA Netw. Open 3, e2019209 (2020).
Basu, R. K. et al. Combining functional and tubular damage biomarkers improves diagnostic precision for acute kidney injury after cardiac surgery. J. Am. Coll. Cardiol. 64, 2753–2762 (2014).
Haase, M. et al. The outcome of neutrophil gelatinase-associated lipocalin-positive subclinical acute kidney injury: a multicenter pooled analysis of prospective studies. J. Am. Coll. Cardiol. 57, 1752–1761 (2011).
Stanski, N., Menon, S., Goldstein, S. L. & Basu, R. K. Integration of urinary neutrophil gelatinase-associated lipocalin with serum creatinine delineates acute kidney injury phenotypes in critically ill children. J. Crit. Care 53, 1–7 (2019).
Murray, P. T. et al. Current use of biomarkers in acute kidney injury: report and summary of recommendations from the 10th Acute Dialysis Quality Initiative Consensus Conference. Kidney Int. 85, 513–521 (2014).
Ronco, C., Kellum, J. A. & Haase, M. Subclinical AKI is still AKI. Crit. Care 16, 313 (2012).
Menon, S. et al. Urinary biomarker incorporation into the renal angina index early in intensive care unit admission optimizes acute kidney injury prediction in critically ill children: a prospective cohort study. Nephrol. Dial. Transplant. 31, 586–594 (2016).
Basu, R. K. et al. Incorporation of biomarkers with the renal angina index for prediction of severe AKI in critically ill children. Clin. J. Am. Soc. Nephrol. 9, 654–662 (2014).
Basu, R. K. et al. Derivation and validation of the renal angina index to improve the prediction of acute kidney injury in critically ill children. Kidney Int. 85, 659–667 (2014).
Basu, R. K., Kaddourah, A. & Goldstein, S. L. & AWARE Study Investigators. Assessment of a renal angina index for prediction of severe acute kidney injury in critically ill children: a multicentre, multinational, prospective observational study. Lancet Child Adolesc. Health 2, 112–120 (2018).
Children’s Hospital Medical Center, Cincinnati. Use of NGAL to optimize fluid dosing, CRRT initiation and discontinuation in critically ill children with acute kidney injury. https://clinicaltrials.gov/ct2/show/NCT03541785 (2021).
De Oliveira, B. D. et al. Molecular nephrology: types of acute tubular injury. Nat. Rev. Nephrol. 15, 599–612 (2019).
Moledina, D. G. & Parikh, C. R. Phenotyping of acute kidney injury: beyond serum creatinine. Semin. Nephrol. 38, 3–11 (2018).
Kellum, J. A. et al. Kidney Disease: Improving Global Outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int. Suppl. 2, 1–138 (2012).
Zappitelli, M. et al. Ascertainment and epidemiology of acute kidney injury varies with definition interpretation. Clin. J. Am. Soc. Nephrol. 3, 948–954 (2008).
Goldstein, S. L. et al. Outcome in children receiving continuous venovenous hemofiltration. Pediatrics 107, 1309–1312 (2001).
Pollack, M. M., Patel, K. M. & Ruttimann, U. E. PRISM III: an updated Pediatric Risk of Mortality score. Crit. Care Med. 24, 743–752 (1996).
CPCCRN. PRISM III calculator. https://www.cpccrn.org/calculators/prismiiicalculator/ (2022).
Stanski, N. L. et al. Recalibration of the renal angina index for pediatric septic shock. Kidney Int. Rep. https://doi.org/10.1016/j.ekir.2021.04.022 (2021).
Varnell, C. D., Goldstein, S. L., Devarajan, P. & Basu, R. K. Impact of near real-time urine neutrophil gelatinase–associated lipocalin assessment on clinical practice. Kidney Int. Rep. 2, 1243–1249 (2017).
De Oliveira, B. D. et al. Molecular nephrology: types of acute tubular injury. Nat. Rev. Nephrol. 15, 599–612 (2019).
Göcze, I. et al. Biomarker-guided intervention to prevent acute kidney injury after major surgery: the prospective randomized BigpAK study. Ann. Surg. 267, 1013–1020 (2018).
Meersch, M. et al. Prevention of cardiac surgery-associated AKI by implementing the KDIGO guidelines in high risk patients identified by biomarkers: the PrevAKI randomized controlled trial. Intensive Care Med. 43, 1551–1561 (2017).
Schanz, M. et al. Urinary [TIMP-2]·[IGFBP7]-guided randomized controlled intervention trial to prevent acute kidney injury in the emergency department. Nephrol. Dial. Transplant. https://doi.org/10.1093/ndt/gfy186 (2018).
Fang, F. et al. Subclinical acute kidney injury is associated with adverse outcomes in critically ill neonates and children. Crit. Care 22, 256 (2018).
Acknowledgements
The authors would like to thank Lin Fei, PhD, for statistical assistance during the design and analysis of this study, and the Center for Acute Care Nephrology research staff for their work on the TAKING FOCUS 2 study.
Funding
R.S.C., K.K., and S.L.G. receive support from the National Institute of Diabetes and Digestive and Kidney (NIDDK) Diseases grant (P50 DK 096418-06). N.L.S. receives support from the National Center for Advancing Translational Sciences of the National Institutes of Health (institutional CT2 grant, 2UL1TR001425-05A1).
Author information
Authors and Affiliations
Contributions
N.L.S. conceptualized and designed the project, acquired the data, analyzed and interpreted the data, drafted and revised and manuscript for important intellectual content, and approved the final version to be published. K.K. acquired the data, drafted and revised and manuscript for important intellectual content, and approved the final version to be published. R.S.C. conceptualized and designed the project, drafted and revised and manuscript for important intellectual content, and approved the final version to be published. S.L.G. conceptualized and designed the project, analyzed and interpreted the data, drafted and revised and manuscript for important intellectual content, and approved the final version to be published.
Corresponding author
Ethics declarations
Competing interests
S.L.G. receives consulting fees from BioPorto Diagnostics, Inc. and Cincinnati Children’s Hospital Medical Center and receives grant funding from BioPorto Diagnostics, Inc. separate from this project. BioPorto, Inc. had no input into the conduct of this study.
Ethics approval and consent to participate
This study was conducted with a waiver of informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stanski, N.L., Krallman, K.A., Chima, R.S. et al. A risk-stratified assessment of biomarker-based acute kidney injury phenotypes in children. Pediatr Res 93, 1354–1360 (2023). https://doi.org/10.1038/s41390-022-02233-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02233-2
This article is cited by
-
Daily serum phosphate increase as early and reliable indicator of kidney injury in children with leukemia and lymphoma developing tumor lysis syndrome
Pediatric Nephrology (2023)
-
Epidemiology of acute kidney injury in children: a report from the 26th Acute Disease Quality Initiative (ADQI) consensus conference
Pediatric Nephrology (2023)