Abstract
Background
The infectious burden in hereditary spherocytosis (HS) children before splenectomy has rarely been reported and the risk of severe postsplenectomy infection is controversial.
Methods
We conducted a retrospective study of pediatric patients with HS to evaluate the risk of infection presplenectomy and postsplenectomy. The primary outcome was any bacterial, Mycoplasma, or fungal infection that required hospitalization. The secondary outcomes were sepsis and septic shock. Appendectomized children were matched on age at surgery and enrolled as controls.
Results
In all, 232 patients were included. Before splenectomy, the primary outcome was identified in 51 (22.0%) patients, and the secondary outcome was identified in 1 (0.4%) patient. After splenectomy, the primary and secondary outcomes were detected in 8 (4.1%) and 1 (0.5%) patients, respectively. The risk of infection was higher presplenectomy than postsplenectomy (OR, 6.6; 95% CI, 3.0–14.2). HS patients had a higher risk of infection than the controls before surgery (OR, 3.7; 95% CI, 2.3–5.9) but not after surgery (OR, 1.4; 95% CI, 0.6–3.6).
Conclusions
HS patients who require splenectomy later in life had a high incidence of hospitalization for infections. In contrast, postsplenectomy risk of hospitalization involving infection or severe infection was low.
Impact
-
Patients with hereditary spherocytosis who require splenectomy later in life have a high risk of hospital admission for infections, especially those with severe hereditary spherocytosis. With vaccines or postoperative antibiotics, splenectomy does not increase the risk of infection or severe infections.
-
Splenectomy may reduce the risk of hospitalization for infections by alleviating the complications of hereditary spherocytosis.
-
With vaccines, prophylaxis, or advanced antibiotics, the benefits of splenectomy in children with hereditary spherocytosis and a heavy disease burden may outweigh the risks.
Similar content being viewed by others
Introduction
Hereditary spherocytosis (HS) is one of the most common causes of inherited chronic hemolysis among people worldwide.1,2,3 HS is a group of disorders in which intrinsic erythrocyte membrane protein defects lead to spherical erythrocytes with reduced deformability and shortened lifespans.1,4,5 The destruction of these abnormal erythrocytes leads to anemia, jaundice, and cholelithiasis, often necessitating splenectomy early in life.6,7
Removal of the spleen effectively abates erythrocyte damage and, thus, anemia. However, immune impairment secondary to splenectomy increases susceptibility to bacterial infections. The increased risk of overwhelming postsplenectomy infection (OPSI) has been recognized since the 1900s. The crude rate of OPSI among splenectomized patients is 3–4%, with a mortality rate of 50% among infected individuals.8,9,10,11 A population-based cohort study reported that the incidence of hospital contact for patients with any infection was 10.2% within 90 days of splenectomy, a much higher rate than that of OPSI.12 However, these results were limited by a short follow-up length and confounded by splenectomy indications and comorbid conditions. A recent study among splenectomized patients with nonmalignant hematologic disorders showed a very low incidence of OPSI over a median of 14 years of follow-up.13
Despite comprehensive studies on postsplenectomy complications, common infections, such as lower respiratory infections and diarrheal diseases, are rarely reported, especially in the pediatric population. Common infections account for two of the three leading causes of global mortality in young children14 and are the most frequent causes of pediatric attendance at health services in low- and middle-income countries, with 2–12% of cases progressing to severe episodes.15 Assessing the incidence of infectious burden before and after splenectomy in patients with HS will facilitate a more comprehensive weighing of the pros and cons of splenectomy. Therefore, the primary aim of this study was to investigate the presplenectomy and postsplenectomy incidence of any infectious disease requiring hospitalization.
Methods
This was a two-center retrospective cohort study. The study was approved by the relevant Institutional Review Board and conducted according to the guidelines in the Helsinki Declaration and its later amendments. Informed consent was waived due to the retrospective nature of the study.
Patients
Patients were identified from two institutional databases, a national center for children’s health (site A: Beijing Children’s Hospital) and a regional medical center (site B: Qilu Hospital of Shandong University), by a systematic, computerized search. Consecutive patients who had an HS diagnosis between December 1, 2007 and December 1, 2021 were eligible candidates. The inclusion criteria were as follows: (1) open or laparoscopic splenectomy and (2) less than 18 years of age. Patients were excluded if they met the following criteria: (1) diseases causing immune dysfunction, such as immunodeficiency or malignancy; (2) diseases prone to infection, such as pulmonary or bronchial malformation, congenital heart disease, or urinary tract malformations; and (3) partial splenectomy.
The diagnosis of HS was established based on family history, presence of nonimmune hemolytic anemia, and assessment of spherocyte morphology. Data on patient demographics, clinical and laboratory metrics, age at surgery, primary indication for splenectomy, and history of any infections requiring hospitalization were extracted using a predetermined table. The severity of disease was classified according to the British Committee for Standards in Haematology guidelines.16
Comparison groups
To compare the effects of HS on preoperative and postoperative infection and to minimize the potential effects of abdominal surgery on the postoperative risk of infection, a comparison group was established. Patients who underwent appendectomy for acute appendicitis were identified through the electronic medical database to match these splenectomy patients (2:1 sample) on the age at surgery. The diagnosis of appendicitis was established based on postoperative pathology. Patients who had postoperative intra-abdominal infections related to appendicitis or any chronic complications as identified by two senior surgeons (Y.C. and Y.Li.) were excluded.
Definitions of outcome variables and follow-up
The primary outcome was any bacterial, Mycoplasma, or fungal infection that required hospitalization. The secondary outcome was severe infection, which included sepsis and septic shock.17 For cases of concurrent infections, the index infections were counted. Consecutive infections were defined as two infections with an intermediate complete remission.
All outcomes of interest identified through inpatient electronic medical records (EMRs) or outpatient EMRs were recorded. The duration of follow-up was defined as the time interval between splenectomy and the date of the patient’s last clinical encounter.
Statistical analysis
Statistical analysis was performed using SPSS 24.0 (IBM Corp., Armonk, NY) and GraphPad Prism 9.3.0 (GraphPad Software, San Diego, CA). Continuous variables are presented as the median and interquartile range (IQR), and comparisons were made using the Mann–Whitney U-test. Categorical variables are expressed as numbers and percentages and compared using the chi-square test or Fisher’s exact test, as appropriate. Kaplan–Meier plots were generated to investigate the cumulative incidence of hospitalization involving infectious disease. Intergroup comparisons were made using the log-rank test. To estimate preoperative risk of infection, we observed the patients from 1 month of age until hospitalization involving an outcome of interest, splenectomy or appendectomy, whichever occurred first. For postoperative risk estimation, we observed the patients from the date of surgery until hospitalization involving an outcome of interest or February 1, 2022, whichever came first. A two-tailed P value of <0.05 was considered statistically significant.
Results
A total of 238 patients were identified with a diagnosis of HS and a history of splenectomy; of these, 232 patients were included in the study. The matched controls included 464 patients with acute appendicitis and a history of appendectomy. The median age at splenectomy was 6.8 years (IQR, 5.2–10.4). The median preoperative hemoglobin level was 87 g/L. The median preoperative weight-for-age percentile was 25.8. The distributions of sex, age at splenectomy, clinical severity of HS, primary indication for splenectomy, and manner of splenectomy were comparable between patients with postoperative follow-up (n = 194) and those lost to follow-up (n = 38). The detailed characteristics are shown in Table 1. Patients from the two sites had comparable characteristics except for the manner of surgery (Supplementary Table).
For most of the study period, patients were recommended to take postoperative prophylactic antibiotics for 3–5 years after splenectomy. Most patients (71%) could easily access oral antibiotics, mainly cephalosporins and amoxicillin. Vaccinations were not routinely recommended until 2015. Twenty-six (13.4%) patients received preoperative or postoperative vaccinations.
Preoperative hospitalization involving infection
Before splenectomy, primary outcomes were detected in 51 (22.0%) patients, with 62 hospitalizations. Of these children, 20 children (39.2%) had infections before 3 years of age, and 35 (68.6%) had infections before 5 years of age. The remaining 16 had infections between 5 and 14 years old. The most frequently detected infection was pneumonia (71.0%). The categories of all infections requiring hospitalization are detailed in Table 2.
Secondary outcomes were detected in one patient. A child with severe HS had bacterial pneumonia in combination with sepsis at the age of 3.5 years. Blood cultures were positive for Streptococcus pneumoniae.
The overall incidence of presplenectomy hospitalization involving infection was 34.6 cases per 1000 person-years, and the incidence for hospitalization involving pneumonia was 24.5 cases per 1000 person-years. The overall incidence of severe infection was 0.6 cases per 1000 person-years. The cumulative incidence of hospitalization for infections is illustrated in Fig. 1. Of the 106 patients with severe HS, 30 (28.3%) had at least 1 hospitalization involving infection. Of the remaining 126 patients with moderate or mild HS, 21 (16.7%) had at least 1 hospitalization involving infection. Patients with severe HS had a significantly higher risk of infection than those with moderate or mild HS (hazard ratio, 2.34; 95% confidence interval [CI], 1.33–4.12). This comparison is also illustrated in Fig. 1. Of the 14 patients with mild HS, 1 had at least 1 hospitalization involving infection.
This figure shows the overall incidence of presplenectomy hospitalization involving infection (black line) and the subgroup comparison between patients with severe HS (red line) and patients with moderate or mild HS (blue line). Patients with severe HS had a significantly higher risk of infection than those with moderate or mild HS (HR, 2.34; 95% CI, 1.33–4.12).
Patients from the two sites had a comparable risk of infections (Table 3).
Postoperative hospitalization involving infection
After splenectomy, 194 patients were followed for a median of 5.5 (IQR, 3.2–8.5) years, for a total follow-up of 1136 patient-years. Hemolysis and anemia were alleviated in all patients, and the mean difference in weight-for-age percentile increased by 22.62 (95% CI, 17.51–27.73) points after splenectomy.
Primary outcomes were detected in 8 (4.1%) patients, with 10 hospitalizations. These 8 patients were not vaccinated, and 7 of them had severe HS before splenectomy, with the remaining patient having moderate HS. Patients with severe HS had a higher risk of hospitalization for infection than those with mild or moderate HS (OR, 8.9; 95% CI, 1.1–73.6). Of the 10 hospitalizations involving infections, 6 (60%) took place during the first 3 years after splenectomy, and the remaining 4 (40%) occurred 3–5 years after splenectomy. The categories of infections requiring hospitalization are detailed in Table 2.
Secondary outcomes occurred in 1 patient (0.5%). This child underwent splenectomy for severe anemia and frequent transfusions (more than once per month) at the age of 10 months. A complete response was observed with a postoperative hemoglobin value of 116 g/L. This child was transferred to our institution 7 weeks later for an intermittent fever lasting 7 days and was diagnosed with sepsis (infection of unknown origin). Consecutive blood cultures were negative for bacterial or fungal pathogens. Two weeks later, this patient died from multiple organ dysfunction syndrome.
The overall incidence of hospitalization involving any infection was 8.8 cases per 1000 person-years, and the incidence for hospitalization involving pneumonia was 6.2 cases per 1000 person-years. The incidence of severe postsplenectomy infection was 0.9 cases per 1000 person-years. The cumulative incidence of hospitalization for any infection is illustrated in Fig. 2.
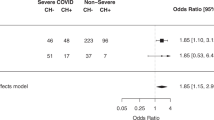
Preoperative and postoperative comparisons
The incidence of presplenectomy hospitalization involving infection was significantly higher than that of postsplenectomy hospitalization involving infection (P < 0.001), with an odds ratio (OR) of 6.6 (95% CI, 3.0–14.2). However, the incidence of presplenectomy hospitalization involving severe infection was not significantly different from that of postsplenectomy hospitalization involving severe infection (P = 1.00).
The incidence of presplenectomy hospitalization involving infection was also significantly higher than that of postsplenectomy hospitalization involving infection for patients with severe HS (OR, 4.6; 95% CI, 1.9–11.1) and patients with moderate or mild HS (OR, 20.8; 95% CI, 2.7–157.5).
Comparisons with the control group
Before appendectomy, primary outcomes were detected in 33 of the 464 patients in the control group, with 35 hospitalizations. None of the 464 subjects in the control group had a severe infection. The overall incidence of hospitalization involving any infection was 9.6 per 1000 person-years.
After appendectomy, 373 patients were followed for a median of 5.9 (IQR, 5.3–6.7) years, generating a total follow-up of 2373 patient-years. Severe infection occurred in a 1.3-year-old child (0.3%) with pneumonia and sepsis 2 months after appendectomy. Overall, 11 (2.9%) patients were hospitalized for any infection after appendectomy, generating an incidence of hospitalization involving infection of 4.6 cases per 1000 person-years.
The incidence of preoperative hospitalization involving infection was significantly higher for HS patients than for the controls (OR, 3.7; 95% CI, 2.3–5.9; P < 0.001). The incidence of preoperative hospitalization involving severe infection was not significantly different between the two groups (P = 0.33). The incidence of hospitalization involving any infection in splenectomized HS patients was not significantly different from that in appendectomized children (OR, 1.4; 95% CI, 0.6–3.6; P = 0.46), nor was the incidence of hospitalization involving severe infection significantly different (OR, 1.9; 95% CI, 0.1–31.0; P = 1.00). These comparisons are detailed in Table 2.
Discussion
The risk of hospitalization involving infection was higher for HS patients who required splenectomy later in life than that for matched controls, particularly among patients with severe HS. After splenectomy, the risks of hospitalization involving infection or severe infection in HS patients were not significantly different from those in appendectomized patients. During the follow-up (a total of 1136 patient-years), severe infection or death was found in 1 HS patient (0.5%) who underwent splenectomy at 10 months. No typical OPSI was identified.
To our knowledge, this is the first study to evaluate the infectious burden of HS before splenectomy in the pediatric population. Surprisingly, HS patients who required splenectomy later in life were at high risk of hospitalization involving infection (22.0%). It is possible that the infections are related to anemia or other complications of the destruction of abnormal erythrocytes, because the risk of infection was higher among severe HS patients than among patients with moderate or mild HS. Previous studies have verified the association of anemia and an increased risk of infectious disease.18,19
Notably, 68.6% of preoperative infections occurred before the age of 5 years. Possible explanations for this finding include the following: (1) severe HS patients tend to undergo splenectomy around the age of 5 years, which leads to a decreased proportion of patients with severe HS among patients older than 5 years old; and (2) risk of infection decreases with age.15 To minimize the influence of age, we enrolled children with appendicitis as controls, matched on the age at surgery with HS patients. HS patients had a 3.7-fold higher risk of preoperative hospitalization involving infection than the controls. In the absence of sufficient evidence,20,21 we have no reason to believe that acute appendicitis is associated with previous hospitalization involving infections. However, current evidence is insufficient to include children who develop appendicitis later in life in the general pediatric population.
Severe postsplenectomy infections have been studied for a very long time. Eraklis et al.9 found that the incidence of death from infection was 5.4% among splenectomized patients and 1.4% among splenectomized patients with HS. Pedersen et al.22 reported a severe infection rate of 5.5% and mortality of 1.6% in patients with HS. However, a recent study reported a much lower incidence of postsplenectomy severe infection (0%). This study included 49 patients with HS, notably, all were vaccinated.23 In the current study, the risks of severe postsplenectomy infection and death were also relatively low (both 0.5%), which is consistent with the results of the study by Luoto et al.23. Despite the lower rate of vaccination (13.4%) in the present study, most of the included patients could easily access antibiotics (within hours after the onset of symptoms of infection). No typical OPSI was found in the current study. Another recent study that included 41 vaccinated HS patients also did not identify any typical cases of OPSI during a long-term follow-up.13
After splenectomy, the risk of hospitalization for infection among HS patients was reduced, which differs, to some extent, from existing knowledge. The high risk of preoperative infections may be associated with young ages,24 anemia,25 hemolysis,26 or malnutrition.27,28 These factors are associated with an increased risk of infections and are common in unsplenectomized HS children, especially those with severe HS. The synergistic or aggravated effects of multiple risk factors may increase the risk of infection even further. The alleviation of these factors after splenectomy may be the main cause of the decrease in risk of infection. Postoperative infections may be related to an impaired immune system.29 Although the risk factors for preoperative and postoperative infections may differ, longitudinal comparisons can help doctors evaluate the role of splenectomy and select the most appropriate time point for splenectomy.
The incidence of hospitalization involving severe infection did not significantly differ preoperative and postsplenectomy. The low incidence of severe infections and the relatively insufficient sample size of the present may have influenced the results. However, the current risk of severe postsplenectomy infection is lower than that reported decades ago12,30 and consistent with the results of recent studies.13,23
Most of the hospitalizations involving infections (60%) occurred within 3 years after splenectomy, and all (100%) occurred within 5 years. These results are consistent with those of previous studies.9,10,30
The incidence of hospitalization for infection or severe infection was not higher in splenectomized patients than in appendectomized patients. These results differ from those of a previous study, which found that the risk of hospital contact involving infection in splenectomized patients differed from that in appendectomized patients (controls).12 In the previous study, the risk of hospital contact involving infection among splenectomized patients was higher than that among controls (adjusted hazard ratio, 2.4). However, these results were confounded by splenectomy indications, and the proportion of patients with hereditary hemolytic anemia was limited (3.7%).
Unfortunately, the current study failed to enroll a general pediatric population for additional comparison. A population-based study from Hong Kong identified 2.3–6.3 hospitalizations per 1000 person-years for community-acquired pneumonia among the 0–19-year-old population.31 The risk of hospitalization involving pneumonia in the current study was 24.5 cases before splenectomy and 6.2 cases after splenectomy per 1000 person-years. The postsplenectomy result is slightly higher than that in the Hong Kong general pediatric population. Another study assessed postappendectomy infections (including sepsis/organ failure, pneumonia, and urinary tract infection) in patients with cerebral palsy and patients without cerebral palsy; postappendectomy infections were detected in <5% of patients without cerebral palsy.32 In our study, the postappendectomy infection rate was 2.9%.
Guidelines and studies recommended that splenectomy should ideally be performed after the age of 5 or 6 years when indicated.7,9,16,33,34,35 However, the rationale is mainly based on studies from the twentieth century, and these conclusions are confounded by the indications for splenectomy. Studies have reported that splenectomized HS patients have a low risk of severe infection or OPSI, particularly in the twenty-first century, when vaccination and prophylaxis are widely recommended before splenectomy.9,10,13,23,30,35 In addition, most studies have not included the general population as a control; thus, the relative risk of severe postsplenectomy infection in HS patients, particularly the risk after excluding the influence of age on susceptibility to infection, has not been fully elucidated. Therefore, the recommended age of splenectomy for HS patients merits further investigation, especially when vaccination, prophylaxis, and advanced antibiotics are widely available. Early splenectomy may help reduce the infectious burden in HS patients by alleviating potential risk factors for infection.
Our study has significant limitations. First, the subjects included were HS patients who underwent splenectomy. HS patients who do not require splenectomy in childhood tend to have mild or moderate HS. Although 54.3% of the included subjects had mild or moderate HS, the results are thus not representative of the risk of hospitalization for infection in the whole HS population. Second, individuals from the general pediatric population were not included in an additional control group. Thus, it remains unclear whether there is a difference in the risk of hospitalization for infection between splenectomized HS patients and the general population. Third, most of the included patients could easily access antibiotics, which may affect the generalizability of our findings. Fourth, the included children were characterized by low serum hemoglobin levels (median, 87 g/L) and low weight-for-age percentiles (median, 25.8), which may be less common in countries with well-developed healthcare systems. Fifth, this study includes the inherent methodological pitfalls of retrospective research. We were unable to determine why, after splenectomy, patients with severe HS had a higher risk of hospitalization involving infection than patients with mild or moderate HS. We were unable to explore whether pediatricians have lower admission criteria for these anemic patients presenting with bacterial infections of the lower respiratory tract or other sites.
Our study’s main strength is the relatively large number of pediatric patients with HS enrolled from national and regional medical centers.
Conclusions
HS patients who require splenectomy later in life had a high incidence of hospitalization for infection. Patients with severe HS were more likely to be admitted for infections. The postsplenectomy risk of hospitalization involving infection was low, and the risk of severe infection or OPSI was minimal. The alleviation of preoperative risk factors for infection after splenectomy may be the main cause of the decrease in the risk of infection. Future studies are warranted to investigate whether the recommended timing of splenectomy should be shifted earlier in patients with HS who receive vaccines, prophylaxis, or advanced antibiotics to reduce the disease burden.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Perrotta, S., Gallagher, P. G. & Mohandas, N. Hereditary spherocytosis. Lancet 372, 1411–1426 (2008).
Tse, W. T. & Lux, S. E. Red blood cell membrane disorders. Br. J. Haematol. 104, 2–13 (1999).
Yawata, Y. et al. Characteristic features of the genotype and phenotype of hereditary spherocytosis in the Japanese population. Int J. Hematol. 71, 118–135 (2000).
Delaunay, J. The molecular basis of hereditary red cell membrane disorders. Blood Rev. 21, 1–20 (2007).
Mohandas, N. & Chasis, J. A. Red blood cell deformability, membrane material properties and shape: regulation by transmembrane, skeletal and cytosolic proteins and lipids. Semin. Hematol. 30, 171–192 (1993).
Baird, R. N., Macpherson, A. I. & Richmond, J. Red-blood-cell survival after splenectomy in congenital spherocytosis. Lancet 2, 1060–1061 (1971).
Iolascon, A. et al. Recommendations regarding splenectomy in hereditary hemolytic anemias. Haematologica 102, 1304–1313 (2017).
KING, H. & SHUMACKER, H. J. Splenic studies. I. Susceptibility to infection after splenectomy performed in infancy. Ann. Surg. 136, 239–242 (1952).
Eraklis, A. J., Kevy, S. V., Diamond, L. K. & Gross, R. E. Hazard of overwhelming infection after splenectomy in childhood. N. Engl. J. Med. 276, 1225–1229 (1967).
Bisharat, N., Omari, H., Lavi, I. & Raz, R. Risk of infection and death among post-splenectomy patients. J. Infect. 43, 182–186 (2001).
Cullingford, G. L., Watkins, D. N., Watts, A. D. & Mallon, D. F. Severe late postsplenectomy infection. Br. J. Surg. 78, 716–721 (1991).
Thomsen, R. W. et al. Risk for hospital contact with infection in patients with splenectomy: a population-based cohort study. Ann. Intern. Med. 151, 546–555 (2009).
Yacobovich, J. et al. Splenectomy in childhood for non-malignant haematologic disorders - long-term follow-up shows minimal adverse effects. Br. J. Haematol. 190, 909–915 (2020).
Collaborators, G. U. M. Global, regional, and national progress towards Sustainable Development Goal 3.2 for neonatal and child health: all-cause and cause-specific mortality findings from the Global Burden of Disease Study 2019. Lancet 398, 870–905 (2021).
Walker, C. et al. Global burden of childhood pneumonia and diarrhoea. Lancet 381, 1405–1416 (2013).
Bolton-Maggs, P. H., Langer, J. C., Iolascon, A., Tittensor, P. & King, M. J. Guidelines for the diagnosis and management of hereditary spherocytosis–2011 update. Br. J. Haematol. 156, 37–49 (2012).
Singer, M. et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 315, 801–810 (2016).
Harris, A. M. et al. Air pollution and anemia as risk factors for pneumonia in Ecuadorian children: a retrospective cohort analysis. Environ. Health 10, 93 (2011).
Kao, J. et al. Early childhood anemia in a birth cohort in coastal Kenya: links to infection and nutrition. Am. J. Trop. Med. Hyg. 101, 242–252 (2019).
Addiss, D. G., Shaffer, N., Fowler, B. S. & Tauxe, R. V. The epidemiology of appendicitis and appendectomy in the United States. Am. J. Epidemiol. 132, 910–925 (1990).
Dursun, I., Kiziltan, M. Y., Bozkaya, D., Aygun, A. & Gucuyener, K. Pneumococcal pneumonia preceding appendicitis in a child. Eur. J. Pediatr. 163, 500 (2004).
Pedersen, F. K. Postsplenectomy infections in Danish children splenectomized 1969-1978. Acta Paediatr. Scand. 72, 589–595 (1983).
Luoto, T. T., Pakarinen, M. P. & Koivusalo, A. Long-term outcomes after pediatric splenectomy. Surgery 159, 1583–1590 (2016).
Jain, S. et al. Community-acquired pneumonia requiring hospitalization among U.S. children. N. Engl. J. Med. 372, 835–845 (2015).
Levy, A. et al. Anemia as a risk factor for infectious diseases in infants and toddlers: results from a prospective study. Eur. J. Epidemiol. 20, 277–284 (2005).
Martins, R. et al. Heme drives hemolysis-induced susceptibility to infection via disruption of phagocyte functions. Nat. Immunol. 17, 1361–1372 (2016).
Ibrahim, M. K., Zambruni, M., Melby, C. L. & Melby, P. C. Impact of childhood malnutrition on host defense and infection. Clin. Microbiol. Rev. 30, 919–971 (2017).
Bhutta, Z. A. et al. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet 382, 452–477 (2013).
Rubin, L. G. & Schaffner, W. Clinical practice. Care of the asplenic patient. N. Engl. J. Med. 371, 349–356 (2014).
Kyaw, M. H. et al. Evaluation of severe infection and survival after splenectomy. Am. J. Med. 119, 271–276 (2006).
Yu, Q. et al. The impact of childhood pneumococcal conjugate vaccine immunisation on all-cause pneumonia admissions in Hong Kong: a 14-year population-based interrupted time series analysis. Vaccine 39, 2628–2635 (2021).
Dhiman, N. et al. Increased complications after appendectomy in patients with cerebral palsy: are special needs patients at risk for disparities in outcomes? Surgery 154, 479–485 (2013).
Holdsworth, R. J., Irving, A. D. & Cuschieri, A. Postsplenectomy sepsis and its mortality rate: actual versus perceived risks. Br. J. Surg. 78, 1031–1038 (1991).
Jugenburg, M., Haddock, G., Freedman, M. H., Ford-Jones, L. & Ein, S. H. The morbidity and mortality of pediatric splenectomy: does prophylaxis make a difference? J. Pediatr. Surg. 34, 1064–1067 (1999).
Ein, S. H. et al. The morbidity and mortality of splenectomy in childhood. Ann. Surg. 185, 307–310 (1977).
Acknowledgements
We thank the patients, nurses, and administrators for their participation in the study. The authors would also like to acknowledge all doctors in our department for their contributions in the treatment of patients with hereditary spherocytosis.
Funding
This research was supported by the Natural Science Foundation of Shandong Province (grant No. ZR2020GSF118021). The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Y. Liu designed the study, performed the research, analyzed the data, and wrote the paper. S.J. performed the research and edited the paper. R.X., C.D., and W.P. contributed to data interpretation and reviewed and provided their comments on this manuscript. Y. Li and Y.C. designed the study, edited the paper, and approved the final version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Informed consent was waived by the institutional review boards due to the retrospective nature of the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, Y., Jin, S., Xu, R. et al. Hereditary spherocytosis before and after splenectomy and risk of hospitalization for infection. Pediatr Res 93, 1336–1341 (2023). https://doi.org/10.1038/s41390-022-02229-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02229-y