Abstract
Background
Type 1 diabetes mellitus (T1DM) affects the development of cognitive function in children, which may be due to deficits in brain structures or functions. It is unclear whether children with T1DM experience alterations in the gray matter (GM) structure at the initial stages of the disease. This study investigated GM structure alterations in children with newly diagnosed T1DM.
Methods
Based on 3D T1-weighted MR images, we investigated the gray matter volume (GMV) of 35 newly diagnosed T1DM children and 35 age- and sex-matched healthy controls using voxel-based morphometry. The brain regions with significant differences in GMV between the newly diagnosed T1DM children and the controls were extracted and the correlation with clinical data was assessed.
Results
Compared with the control group, children with newly diagnosed T1DM had a lower GMV in the right inferior and middle temporal gyri, right lingual gyrus, and left superior frontal gyrus. In T1DM subjects, the GMV of the right middle temporal gyrus was positively correlated with IQ but was negatively correlated with HbA1c.
Conclusions
Our findings provide compelling evidence that GM abnormalities occur during early disease stages in T1DM children, which may be a potential neurobiological mechanism underlying cognitive deficits.
Impact
-
Using an efficient method to analyze gray matter changes in T1DM is very important.
-
The anterior, posterior, and temporal brain regions are susceptible to T1DM in children.
-
Recent glucose variability may affect regional gray matter volume in children with newly diagnosed T1DM.
-
Structural changes were documented in the gray matter of the brain even at the early stages of the disease in children with T1DM.
Similar content being viewed by others
Introduction
It is well-established that type 1 diabetes mellitus (T1DM) usually develops during childhood or adolescence, and results in metabolic and vascular disturbances, with devastating effects on many organs, including nephrological, cardiac, and ophthalmological complications.1,2 T1DM is also known to affect the central nervous system, increasing the risks of seizures, diabetic encephalopathy, and cognitive disorders.
An increasing body of evidence suggests that T1DM affects the development of cognitive function and induces cognition impairments in children.3,4,5 Children with T1DM have lower overall intelligence quotient (IQ) scores than normal controls, especially in early-onset T1DM children.4 Moreover, T1DM children often exhibit alterations in processing speed, executive functions, and learning and memory.1,6,7,8 Notwithstanding that significant inroads have been achieved in recent years, the mechanism of cognition impairment caused by T1DM remains unclear. It has been suggested that these cognitive impairments are due to brain structural or functional deficits.
T1DM is well-recognized to result in alterations in brain structures. Over the years, studies based on voxel-based morphometry (VBM) have mainly focused on adult patients and reported a reduced gray matter volume (GMV) in several brain regions involved in the pathophysiology of T1DM-related cognitive decline. Specifically, reduced GMV was found in brain regions responsible for memory, attention, information processing, and psychomotor speed.9,10,11 Reduced GMV has also been reported in the thalamus, occipital and frontal regions, and in the parahippocampal regions.12,13,14 Lower GMV was associated with poor control of blood glucose, severe hypoglycemia, and long duration and early onset of T1DM.12,13,15
To the best of our knowledge, few studies have hitherto investigated GMV changes in children and adolescents with T1DM. Interestingly, existing studies have shown structural changes in the brain as early as childhood in patients with T1DM.16,17,18 One study showed a reduced GMV in the left temporal area in T1DM children aged from 4 to 10 years, which was associated with severe hypoglycemia.19 Another study showed the GMV was decreased in the bilateral occipital-temporal and cerebellar areas, but was increased in the left insula, frontal and temporal areas in young children with early-onset T1DM, associated with hyperglycemia.18 In addition, it has been shown that T1DM affects brain structure development. In this regard, longitudinal studies revealed that gray matter (GM) growth was decreased throughout the cortex and cerebellum in T1DM children.20
Given that the disease duration for T1DM children in previous brain structural studies was more than 2 years, there is a lack of studies on newly diagnosed T1DM children. It remains unclear whether there are alterations in GM structure at the initial stages of T1DM. Hence, we aimed to examine GM alterations in newly diagnosed T1DM children relative to control subjects on 3D T1-weighted images (T1WI) using VBM procedures and determine the nature of GMV alterations. Our study may provide novel insights into early structural brain alterations associated with the development of T1DM.
Methods
Subjects
This study was approved by our institution’s ethics committee. Written informed consent was obtained from parents and children aged 12 years and older. Children newly diagnosed with T1DM were consecutively recruited from the Department of Pediatric Endocrinology from April 2016 until January 2018. T1DM was diagnosed according to the following criteria: history of polydipsia and/or polyuria, blood glucose level (BGL) above 200 mg/dL, glycated hemoglobin A1C (HbA1c) above 6.5%, low insulin (fasting insulin level <5 μIU/mL) and C-peptide level (peak C-peptide <0.2 pmol/mL), and insulin dependency.21,22,23 The inclusion criteria for the T1DM group were as follows: (1) patients first diagnosed with T1DM within the past 30 days; (2) aged from 6 to 16 years; (3) complete clinical, imaging, and IQ data available. The inclusion criteria for the control group were children and adolescents with normal fasting glucose (<110 mg/dL), normal HbA1c (<6%), and complete clinical, imaging, and IQ data. The exclusion criteria for both groups were vascular disease, heart or kidney disease, neurologic diseases such as seizure disorders, (history of) intracranial neoplasms or infection, traumatic brain injury, psychiatric disorders, left- or mixed-handed, and MRI contraindications (metal implants or claustrophobia). In addition, controls were matched to cases on age and sex.
Intelligence assessments
All subjects were assessed for general intellectual ability using the Chinese Wechsler Intelligence Scale for Children or the Wechsler Intelligence Scale for Children IV. For stability and reliability of our findings, all assessments were performed by personnel who have been systematically trained and qualified for the above-mentioned scales. The evaluation was completed on the day of the MRI scan. Since the subtests of these two scales are different, only the total IQ was used to assess cognitive function.
MRI protocol
The children underwent structural brain MRI scans using a 3.0-Tesla magnetic resonance system (GE, Waukesha, WI). The 3D T1-BRAVO sequence was used to obtain a high-resolution T1WI. The parameters were set as follows: repetition time 7.2 msec, echo time 3.4 msec, number of excitations 1, flip angle 12°, matrix 256 × 256, field of view 240 × 240 mm2, Locs per Slab 188, slice thickness 1 mm, and voxel size 1.0 × 1.0 × 1.0 mm. All T1DM children underwent MR scans after their condition became stable, determined by the pediatric endocrinologists. For T1DM children with diabetic ketoacidosis (DKA), MR scans were performed at least 3 days after the resolution of DKA.
Image processing and analysis
Analysis of structural data was performed on FSL 4.1 software (the Analysis Group, FMRIB, Oxford) by using FSL-VBM.24,25 Brain extracting tool was used to carry out brain extraction on the structural images. FSL Automated Segmentation Tool 4 (FAST4) was used to carry out tissue-specific segmentation.26,27 The GM partial volume images were then aligned to the MNI standard space (MNI152) followed by nonlinear registration.28,29 The resulting images were averaged to generate a study-specific GM template (including all subjects).30 Then, all GM images were nonlinearly registered to the standard space template generated above, with intensity modulation being used to adjust for local contractions or expansions coming from the nonlinear components of the spatial transformation. The normalized images were then smoothed with an isotropic Gaussian kernel (sigma = 3 mm, full width at half maximum = 9.4 mm). Finally, a series of 3D matrices were output.30 The three indices in each matrix represented the spatial x, y, and z coordinates in the reference space, and each value was proportional to the GMV.30
FMRIB Software (the Analysis Group, Oxford) was used to generate design matrix and contrast files. Based on the general linear model (age, sex, and total intracranial volume as covariates), voxel-wise t-tests were performed to investigate intergroup differences in GMV. Permutation-based non-parametric testing (5000 permutations) was used to conduct statistical inference.31 Threshold-free cluster enhancement with family-wise error correction was used for statistical thresholding and multiple comparisons correction (P < 0.05).32
Statistical analysis
Data normality was tested by the Shapiro–Wilk test. The results are reported as mean ± standard deviation. Demographic and clinical data were analyzed on SPSS 19.0 (SPSS, Inc., Chicago, IL) using an independent-samples t-test. The sex comparison was performed using χ2 test. To investigate the relationship between GMV and clinical variables, we extracted the mean GMV value of regions with significant intergroup differences. Then partial correlation analysis was carried out between the mean GMV of each ROI and each clinical variable. The correlations were corrected for age, sex, and total intracranial volume. Bonferroni corrections were used for multiple comparisons. A P value <0.05 was statistically significant.
Results
Demographic and clinical comparisons
There were no significant differences in age, sex, or IQ between the T1DM and control groups (P > 0.05, Table 1). HbA1c and BGL at imaging in the T1DM group were higher than in the control group (P < 0.05). For the T1DM group, the time interval from diagnosis to imaging was 4.7 days (Table 1).
Group differences in GMV
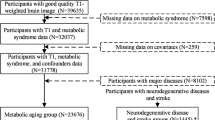
Compared with the control group, children with newly diagnosed T1DM had a lower GMV in the right inferior temporal gyrus (ITG), right middle temporal gyrus (MTG), right lingual gyrus (LG), and left superior frontal gyrus (SFG) (Table 2 and Fig. 1). There were no brain regions with increased GMV in these children.
Images showing the smaller GMV of the right inferior gyrus (a), right middle temporal gyrus (b), right lingual gyrus (c), and left superior frontal gyrus (d) in the T1DM group compared with the CON group. Crosshairs indicate the location of the peak voxels of the significant regions. The color bar indicates 1 – P values. GMV gray matter volume, T1DM type 1 diabetes mellitus, CON control.
Correlation between GMV and clinical variables
In T1DM subjects, there was a significant negative correlation between HbA1c and GMV in the right MTG (Table 3 and Fig. 2). However, a significant positive correlation was found between full-scale IQ and the GMV of the right MTG (Table 3 and Fig. 2). No significant correlations were identified between HbA1c, BGL at imaging or full-scale IQ and reduced GMV in the right ITG, right LG, and left SFG. For the normal controls, no significant correlations were found between GMV and HbA1c, BGL at imaging, and full-scale IQ in the right MTG, right ITG, right LG, and left SFG.
Discussion
In this VBM-based study, we found GMV decreases in the right ITG, right MTG, right LG, and left SFG in newly diagnosed T1DM children compared with healthy controls. Interestingly, significant correlations were found between GMV and HbA1c and full-scale IQ in the right MTG in the newly diagnosed T1DM children. These structural alterations indicate that brain tissue integrity is affected by T1DM even at the beginning of the disease.
Few studies have investigated GM structure alterations in T1DM children. A previous study reported that relative to the controls, T1DM children with a mean age of 12.6 ± 2.7 years displayed no significant GMV alteration.19 In contrast, young T1DM children with a mean age of 7.0 ± 1.7 years showed GMV alterations in several brain regions, such as the left frontal and occipital lobes, bilateral temporal lobe and cerebellum, and left insula region.18 It should be borne in mind that in these studies, the children had T1DM for more than 2 years. Herein, we found a reduced GMV in the right ITG, right MTG, right LG, and left SFG in children with newly diagnosed T1DM with a mean age of 10.00 ± 2.45 years. The above studies suggest that the GM structure of younger children is more susceptible to T1DM than older children. Our findings were inconsistent with those reported by Marzelli et al., which may stem from the heterogeneity in the age of onset, disease duration, and hyperglycemic exposure.18 Our results also suggest that brain structure is altered at the beginning of T1DM, especially the GMV of the anterior, posterior, and temporal regions. A previous study showed neurocognitive changes in children within days of T1DM diagnosis, especially in psychomotor speed, visuomotor integration, and phonemic fluency.33 These findings support Ryan et al.’s hypothesis that the peri-onset period may be a period of significant structural and cognitive vulnerability.34
The neural basis of GMV alterations in diabetes remains unclear, but hyperglycemia is widely thought to be a crucial mediator. Hyperglycemia causes oxidative stress and the production of toxic glucose metabolites, which represents the mechanism for increased neuronal apoptosis.2,35 A recent study demonstrated that defective cell volume regulation due to increased oxidative stress might lead to neuronal loss.36 Intriguingly, hyperglycemia leads to an increase in the polyol pathway activity and a decrease in the production of insulin-like growth factors and nerve growth factors, which account for reduced dendritic arborization and inhibited neuron growth.37,38 It was also shown that hyperglycemia induces the remodeling (such as retraction and simplification) of apical dendrites of neurons, resulting in relatively smaller cortical neurons.39 The above alterations induced by hyperglycemia may contribute to decreased GMV in children with newly diagnosed T1DM.
The association between T1DM and cognitive impairment has been widely reported in the literature. However, little is known about neural deficits, which may lead to cognitive impairment. A recent study that investigated the association between structural deficits and functional outcomes in adult T1DM patients found that whole-brain volume and structural defects of the temporal lobe were associated with IQ, information processing, and attention impairments. However, the association between cognition and structural deficits in T1DM children remains unclear. There is vast literature available suggesting that cognitive impairments in IQ, language, visual perception, and memory are present in T1DM children.3,40 The ITG and the MTG are located on the lateral surface of the temporal cortex and are involved in the language process, visual perception, and semantic memory.41,42,43,44,45 The LG is a structure in the visual cortex with vision-related functions.46 In contrast, the SFG accounts for one-third of the human brain’s frontal lobe and is reported to be involved in working memory.47 In the present study, we found a reduced GMV in brain regions responsible for IQ, language, visual perception, and memory. A positive relationship was also found between the GMV of the right MTG and IQ in T1DM children, which suggested that a smaller GMV in the right MTG was associated with a worse IQ. We speculate that the reduction of GMV in these brain regions provides a neural basis for cognitive decline in children with T1DM, which warrants further study.
A negative relationship was found between GMV of the right MTG and HbA1c in newly diagnosed T1DM children, suggesting that the right MTG may be particularly vulnerable to T1DM because altered GMV in this brain region is not only associated with diabetes but also with an elevated level of HbA1c. It is widely acknowledged that HbA1c is an indicator of BGLs for the past 2–3 months. Our results indicated that recent changes in glucose levels could affect the GMV of the right MTG in newly diagnosed T1DM children, and the reduction of GMV in the right MTG may result from recent hyperglycemic injury.
There are limitations to the present study. First, the sample size is small, which can cause large variability in results. Multicenter studies with larger sample sizes are required to reduce the variability of heterogeneity of our findings. Second, the intelligence scale used in this study is relatively basic and cannot determine specific cognitive alterations such as language processing, visual perception, and learning and memory. Third, due to the limited number of cases with DKA, we did not evaluate the impact of DKA on GM and cognition. Fourth, given that all T1DM children received insulin treatment, the potential confounding effect of insulin cannot be ruled out. Fifth, due to the lack of prior imaging, this study could not determine whether these changes are truly due to hyperglycemia or due to underlying genetic or metabolic pathways. Lastly, this study could not determine the effect of altered GMV on cognition because of the cross-sectional design. A subsequent longitudinal study is warranted to observe changes in GMV over time and its role in brain function.
Conclusion
We found that GMV was reduced in the right ITG, right MTG, right LG, and left SFG in newly diagnosed T1DM children compared with the controls. In T1DM subjects, the GMV of the right MTG was positively correlated with IQ but was negatively correlated with HbA1c. Our study revealed that GM structural alterations occurred at the beginning of the disease, which may contribute to the cognitive decline in children with T1DM.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Litmanovitch, E., Geva, R. & Rachmiel, M. Short and long term neuro-behavioral alterations in type 1 diabetes mellitus pediatric population. World J. Diabetes 6, 259–270 (2015).
Hamed, S. A. Brain injury with diabetes mellitus: evidence, mechanisms and treatment implications. Expert Rev. Clin. Pharm. 10, 409–428 (2017).
Gaudieri, P. A., Chen, R., Greer, T. F. & Holmes, C. S. Cognitive function in children with type 1 diabetes: a meta-analysis. Diabetes Care. 31, 1892–1897 (2008).
Cato, M. A. et al. Cognitive functioning in young children with type 1 diabetes. J. Int. Neuropsychol. Soc. 20, 238–247 (2014).
Kirchhoff, B. A., Jundt, D. K., Doty, T. & Hershey, T. A longitudinal investigation of cognitive function in children and adolescents with type 1 diabetes mellitus. Pediatr. Diabetes 18, 443–449 (2017).
Biessels, G. J., Deary, I. J. & Ryan, C. M. Cognition and diabetes: a lifespan perspective. Lancet Neurol. 7, 184–190 (2008).
Hannonen, R. et al. Academic skills in children with early-onset type 1 diabetes: the effects of diabetes-related risk factors. Dev. Med. Child Neurol. 54, 457–463 (2012).
Tonoli, C. et al. Type 1 diabetes-associated cognitive decline: a meta-analysis and update of the current literature. J. Diabetes 6, 499–513 (2014).
Ferguson, S. C. et al. Influence of an early-onset age of type 1 diabetes on cerebral structure and cognitive function. Diabetes Care 28, 1431–1437 (2005).
Moulton, C. D., Costafreda, S. G., Horton, P., Ismail, K. & Fu, C. H. Meta-analyses of structural regional cerebral effects in type 1 and type 2 diabetes. Brain Imaging Behav. 9, 651–662 (2015).
Nunley, K. A. et al. Regional gray matter volumes as related to psychomotor slowing in adults with type 1 diabetes. Psychosom. Med. 79, 533–540 (2017).
Wessels, A. M. et al. Voxel-based morphometry demonstrates reduced grey matter density on brain MRI in patients with diabetic retinopathy. Diabetologia 49, 2474–2480 (2006).
Northam, E. A. et al. Central nervous system function in youth with type 1 diabetes 12 years after disease onset. Diabetes Care 32, 445–450 (2009).
Hughes, T. M. et al. Frontal gray matter atrophy in middle aged adults with type 1 diabetes is independent of cardiovascular risk factors and diabetes complications. J. Diabetes Complications 27, 558–564 (2013).
Franc, D. T. et al. High connectivity between reduced cortical thickness and disrupted white matter tracts in long-standing type 1 diabetes. Diabetes 60, 315–319 (2011).
Arbelaez, A. M., Semenkovich, K. & Hershey, T. Glycemic extremes in youth with T1DM: the structural and functional integrity of the developing brain. Pediatr. Diabetes 14, 541–553 (2013).
Antenor-Dorsey, J. A. et al. White matter microstructural integrity in youth with type 1 diabetes. Diabetes 62, 581–589 (2013).
Marzelli, M. J. et al. Neuroanatomical correlates of dysglycemia in young children with type 1 diabetes. Diabetes 63, 343–353 (2014).
Perantie, D. C. et al. Regional brain volume differences associated with hyperglycemia and severe hypoglycemia in youth with type 1 diabetes. Diabetes Care 30, 2331–2337 (2007).
Mazaika, P. K. et al. Variations in brain volume and growth in young children with type 1 diabetes. Diabetes 65, 476–485 (2016).
Alberti, K. G. & Zimmet, P. Z. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a who consultation. Diabet. Med. 15, 539–553 (1998).
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 36(Suppl 1), S67–S74 (2013).
Orban, T. et al. Co-stimulation modulation with abatacept in patients with recent-onset type 1 diabetes: a randomised, double-blind, placebo-controlled trial. Lancet 378, 412–419 (2011).
Ashburner, J. & Friston, K. J. Voxel-based morphometry-the methods. Neuroimage 11, 805–821 (2000).
Smith, S. M. et al. Advances in functional and structural MR image analysis and implementation as FSL. Neuroimage 23(Suppl 1), S208–S219 (2004).
Smith, S. M. Fast robust automated brain extraction. Hum. Brain Mapp. 17, 143–155 (2002).
Zhang, Y., Brady, M. & Smith, S. Segmentation of brain MR images through a hidden Markov random field model and the expectation-maximization algorithm. IEEE Trans. Med. Imaging 20, 45–57 (2001).
Jenkinson, M. & Smith, S. A global optimisation method for robust affine registration of brain images. Med. Image Anal. 5, 143–156 (2001).
Jenkinson, M., Bannister, P., Brady, M. & Smith, S. Improved optimization for the robust and accurate linear registration and motion correction of brain images. Neuroimage 17, 825–841 (2002).
Comley, R. A. et al. A comparison of gray matter density in restless legs syndrome patients and matched controls using voxel-based morphometry. J. Neuroimaging 22, 28–32 (2012).
Winkler, A. M., Ridgway, G. R., Webster, M. A., Smith, S. M. & Nichols, T. E. Permutation inference for the general linear model. Neuroimage 92, 381–397 (2014).
Smith, S. M. & Nichols, T. E. Threshold-free cluster enhancement: addressing problems of smoothing, threshold dependence and localisation in cluster inference. Neuroimage 44, 83–98 (2009).
Schwartz, D. D., Axelrad, M. E. & Anderson, B. J. Neurocognitive functioning in children and adolescents at the time of type 1 diabetes diagnosis: associations with glycemic control 1 year after diagnosis. Diabetes Care 37, 2475–2482 (2014).
Ryan, C. M. Searching for the origin of brain dysfunction in diabetic children: going back to the beginning. Pediatr. Diabetes 9, 527–530 (2008).
Malone, J. I. et al. Hyperglycemia not hypoglycemia alters neuronal dendrites and impairs spatial memory. Pediatr. Diabetes 9, 531–539 (2008).
Hansen, S. H. The role of taurine in diabetes and the development of diabetic complications. Diabetes Metab. Res. Rev. 17, 330–346 (2001).
Suzuki, T., Sekido, H., Kato, N., Nakayama, Y. & Yabe-Nishimura, C. Neurotrophin-3-induced production of nerve growth factor is suppressed in Schwann cells exposed to high glucose: involvement of the polyol pathway. J. Neurochem. 91, 1430–1438 (2004).
Bondy, C. A. & Cheng, C. M. Signaling by insulin-like growth factor 1 in brain. Eur. J. Pharm. 490, 25–31 (2004).
McEwen, B. S., Magarinos, A. M. & Reagan, L. P. Studies of hormone action in the hippocampal formation: possible relevance to depression and diabetes. J. Psychosom. Res. 53, 883–890 (2002).
Semenkovich, K. et al. Clinical presentation and memory function in youth with type 1 diabetes. Pediatr. Diabetes 17, 492–499 (2016).
Onitsuka, T. et al. Middle and inferior temporal gyrus gray matter volume abnormalities in chronic schizophrenia: an MRI study. Am. J. Psychiatry 161, 1603–1611 (2004).
Chao, L. L., Haxby, J. V. & Martin, A. Attribute-based neural substrates in temporal cortex for perceiving and knowing about objects. Nat. Neurosci. 2, 913–919 (1999).
Tranel, D., Damasio, H. & Damasio, A. R. A neural basis for the retrieval of conceptual knowledge. Neuropsychologia 35, 1319–1327 (1997).
Cabeza, R. & Nyberg, L. Imaging cognition II: an empirical review of 275 PET and FMRI studies. J. Cogn. Neurosci. 12, 1–47 (2000).
Herath, P., Kinomura, S. & Roland, P. E. Visual recognition: evidence for two distinctive mechanisms from a PET study. Hum. Brain Mapp. 12, 110–119 (2001).
Mechelli, A., Humphreys, G. W., Mayall, K., Olson, A. & Price, C. J. Differential effects of word length and visual contrast in the fusiform and lingual gyri during reading. Proc. Biol. Sci. 267, 1909–1913 (2000).
du Boisgueheneuc, F. et al. Functions of the left superior frontal gyrus in humans: a lesion study. Brain 129, 3315–3328 (2006).
Acknowledgements
We thank Home for Researchers editorial team (www.home-forresearchers.com) for the language editing service.
Funding
This work was supported by the grants from Zhejiang Provincial Natural Science Foundation (LY18H070003 and LY19H180003), National Natural Science Foundation of China (81400863, 82071902, and 82100952), and Health Department of Zhejiang province (2018KY522).
Author information
Authors and Affiliations
Contributions
Each author has met the Pediatric Research authorship requirements. K.L., X.L., X.Y., and Z.Y. had substantial contributions to the conception and design, acquisition of data, analysis, and interpretation of data. K.L. drafted the article. H.S., J.S., S.C., X.H., and Y.Z. had substantial contributions to the acquisition of data and analysis of data. X.Y. and Z.Y. revised the article. All authors are in agreement with the content of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The current study was approved by the Research Ethics Committee of The Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University.
Consent for publication
Informed consent was obtained from the parents of the children and, when appropriate, assent was acquired from the children themselves.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, K., Su, H., Song, J. et al. Altered gray matter volume in children with newly diagnosed type 1 diabetes mellitus. Pediatr Res 93, 1342–1347 (2023). https://doi.org/10.1038/s41390-022-02227-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02227-0