Abstract
Objective
To investigate postnatal neural conduction in the auditory brainstem in neonatal bronchopulmonary dysplasia (BPD) survivors.
Methods
Thirty-two very preterm BPD survivors were studied at 57–58 weeks of postconceptional age. Brainstem auditory-evoked response was studied using maximum length sequence. Wave latencies and intervals were analyzed in detail. The controls were 37 normal term infants and 35 very preterm non-BPD infants.
Results
Compared with normal term controls, BPD survivors showed significantly shortened I–III interval but significantly prolonged III–V interval and greater III–V/I–III interval ratio. Compared with very preterm non-BPD controls, BPD survivors showed a significant shortening in waves III latency and I–III interval, moderate prolonged III–V interval, and significantly greater III–V/I–III interval ratio. These differences were generally similar at all click rates used. The slopes of latency- and interval-click rate functions in BPD survivors did not differ significantly from the two control groups.
Conclusions
Brainstem neural conduction in BPD survivors differed from normal term and age-matched non-BPD infants; neural maturation is accelerated in caudal brainstem regions but delayed in rostral regions. Neonatal BPD survivors are associated with differential maturation in neural conduction at caudal and rostral brainstem regions, which may constitute an important risk for postnatal neurodevelopment in BPD survivors.
Impact
-
We found that brainstem neural conduction at PCA 57–58 weeks in neonatal BPD survivors differs from normal term and age-matched non-BPD infants.
-
No major differences were found between normal term and very preterm non-BPD infants in brainstem auditory conduction.
-
Neural conduction in BPD survivors is accelerated in caudal brainstem regions but delayed in rostral regions.
-
Neonatal BPD survivors are associated with differential maturation in neural conduction at caudal and rostral brainstem regions.
-
The abnormality may constitute an important risk for postnatal neurodevelopment in BPD survivors.
Similar content being viewed by others
Introduction
Infants born very preterm are often associated with various perinatal complications or problems. Improved perinatal care and survival of very preterm infants have led to an increased number of infants with neonatal bronchopulmonary dysplasia (BPD).1,2,3 As severe respiratory morbidity and mortality, neonatal BPD has been recognized to be a very high risk for neurological impairment and developmental deficits in infants born very preterm.4,5,6,7,8,9 Cortical auditory processing seems to be influenced by clinical conditions, mainly BPD, complicating very or extremely preterm birth.10 Cerebral magnetic resonance imaging studies found that neonatal BPD was significantly associated with delayed brain maturation, and a significant predictor of delayed brain maturation.11 At term equivalent age neonatal BPD is a prominent perinatal risk factor for delayed brain maturation in very preterm infants. Whether such maturational delay extends to postnatal age is subject to further investigation.
It was not until recently that neural conduction in the brainstem in BPD neonates was found to be significantly abnormal at term age.12 Using the maximum length sequence brainstem auditory-evoked response (MLS BAER), we studied functional integrity of the brainstem auditory pathway in very preterm infants. In an early multivariate analysis of risk factors for MLS BAER abnormalities in very preterm infants, we found that BPD was a potential major risk for the abnormalities (unpublished data). We then carried out a specific MLS BAER study in very preterm BPD infants at 40 weeks of postconceptional age (PCA), i.e., shortly after neonatal BPD was diagnosed at PCA 36 weeks.12 These infants were found to have major abnormalities in the MLS BAER variables that mainly reflect brainstem neural conduction, suggesting a significant delay or impairment in neural conduction of the auditory brainstem, mainly at more central or rostral brainstem regions. Clearly, at term equivalent age neonatal BPD and associated perinatal conditions exert a detrimental effect on neural conduction of the immature brainstem. A preliminary study of auditory function shortly after term in BPD infants showed minor auditory abnormalities in conventional BAER, i.e., the BAER recorded and analyzed with conventional averaging technique.13
So far, little is known about postnatal changes in the major abnormalities in brainstem neural conduction in BPD infants found at term age by Wilkinson et al.12 The understanding is important for postnatal management of BPD survivors to improve their outcome. It is plausible that the detrimental effect of neonatal BPD and associated perinatal conditions on neural conduction of the auditory brainstem continues beyond the full term age in BPD survivors. We hypothesize that the major neurological impairment, i.e., significantly delayed neural conduction in the brainstem, found at term age in BPD infants would improve or change with increasing age but there would still be some longer-term abnormalities unresolved.
To address this issue, we studied brainstem neural conduction at PCA 57–58 weeks in very preterm BPD survivors using MLS BAER, which improves the detection of brainstem auditory abnormality.14,15 Detailed analysis was focused on MLS BAER wave latencies and, in particular, interpeak intervals to assess postnatal neural conduction of the auditory brainstem. The MLS BAER data in the BPD survivors were compared with those in normal term infants to detect any abnormalities in BPD survivors, and with those in age-matched very preterm infants who did not suffer neonatal BPD (non-BPD) to assess any postnatal effect of very preterm birth. The findings should enhance our understanding of functional maturation of the auditory brainstem in BPD survivors and postnatal effect of neonatal BPD on brainstem neural conduction, proving valuable information for postnatal management of very preterm infants who survive BPD.
Methods
Study population
Three groups of infants were recruited at a mean PCA of 57–58 weeks, equivalent to four months of corrected age (i.e., adjusted for prematurity), from the Children’s Hospital of Fudan University: very preterm BPD (study) group, normal term (control) group, and very preterm non-BPD (control) group. Prior to the study, approved by the Children’s Hospital Ethics Committee, informed parental consent was obtained for each infant. Those infants who had major perinatal complications or problems (except BPD in the study group) that could affect the functional integrity of the brainstem auditory pathway were excluded to minimize any possible confounding effect on the results.15,16 The major conditions or problems included severe perinatal hypoxia-ischemia, grades III and IV intraventricular hemorrhage, periventricular leukomalacia, hyperbilirubinemia, necrotizing enterocolitis, congenital malformation or chromosomal anomalies, congenital or perinatal infection of the central nervous system, and syndromes, family history of hearing loss. Any infants who had a monaural BAER threshold great than 20 dB normal hearing level (nHL) were also excluded to minimize the effect of any peripheral hearing problems on the MLS BAER.
The BPD (study) group was comprised of 32 very preterm survivors of neonatal BPD. The diagnostic criteria for neonatal BPD, while they were hospitalized, were the same as previously described.12 These included a requirement for supplementary oxygen or ventilatory support beyond 36 weeks of PCA to maintain PaO2 > 50 mmHg, clinical signs of chronic lung respiratory disease, and radiographic evidence of BPD (persistent strands of density in both lungs). Their gestation ranged between 24 and 30 weeks (25.9 ± 1.7 weeks), and birth weight between 615 and 1350 g (828 ± 191 g).
The normal term control group was comprised of 37 healthy term infants without any major perinatal conditions. Their gestational age ranged between 37 and 41 weeks (39.2 ± 1.2 weeks) and birth weight between 2560 and 4528 g (3442 ± 501 g). The non-BPD group was comprised of 35 very preterm infants who did not suffer from neonatal BPD. Their gestation ranged between 24 and 30 weeks (26.4 ± 1.5 weeks), which did not differ significantly from the BPD group, and birth weight was between 625 and 1490 g (1127 ± 235 g), which was greater than in the BPD group (P < 0.01).
Recording and analysis of MLS BAER
The recording was carried out at a mean PCA of 57–58 weeks: PCA 57.4 ± 5.3 weeks for the BPD group, 57.7 ± 4.9 weeks for the normal term group, and 57.6 ± 5.1 weeks for the non-BPD group. These PCAs did not differ significantly between any of the three groups of infants. The procedures for recording MLS BAER were basically the same as previously reported.12 Briefly, the left ear was tested in all infants for consistency and saving recording time. This also allowed ensuring that estimates of population statistics were not biased by the ear difference in BAER waveforms and measurements of various wave components. Three surface disk electrodes (positive, negative, and ground) were placed, respectively, at the middle forehead, left (ipsilateral) earlobe, and right (contralateral) earlobe. Rarefaction clicks of 100 µs at 60 dB nHL were delivered through an earphone to the left ear. Two runs of MLS BAER for each recording condition were recorded for reproducibility. Evoked brainstem responses to 1500 trains of clicks were preamplified, and bandpassed between 100 and 3000 Hz.12 The recording and analyzing of MLS BAER were carried out on a Nicolet Biomedical portable evoked potential system.
Data analysis
Figure 1 shows sample MLS BAER traces, recorded at 91/s clicks, in a normal term baby, and schematic measurement of wave latencies and interpeak intervals. These were conducted by two independent evaluators without knowing the clinical data. The measurements of each MLS BAER variable from two replicated recordings were averaged for statistical analysis using an SPSS package (version 22, Chicago, IL). The one-sample Kolmogorov–Smirnov test showed that all wave latencies and interpeak intervals in MLS BAER followed a normal distribution. Thus, mean and standard deviation of each MLS BAER variable at each repetition rate of click stimuli were compared between different groups using the analysis of variance (ANOVA). Statistical significance was set as two-tailed value of P < 0.05. Regression analysis was performed to assess the relationship between MLS BAER variables and the repetition rate of clicks. The slope (or regression coefficient) was calculated for each MLS BAER wave latency- or interval-rate function, and then compared between any two of the BPD, normal term, and non-BPD groups using a Student t-test for any significant differences.
Results
The BAER threshold in the BPD group (10.8 ± 5.9 dB nHL) did not differ significantly from that in the non-BPD group (11.2 ± 5.4 dB nHL). However, the threshold in the two groups of very preterm infants was significantly higher than in the normal term group (8.5 ± 4.5 dB nHL) (P < 0.05 and 0.05). The difference in BAER threshold affects MLS BAER wave latencies between groups, but does not exert any significant effect on MLS BAER interpeak intervals between groups because the intervals are minimally affected by variation in the threshold.15 There were small differences among the three groups of infants in the hearing levels (i.e., the dB above the threshold of each individual infant); 50.7 ± 8.1 dB nHL in the BPD group, 51.5 ± 4.9 dB nHL in the normal term group, and 50.2 ± 6.3 dB nHL in the non-BPD group, which did not differ significantly between any of the three groups.
Comparison of MLS BAER variables between different click rates
All MLS BAER wave latencies and interpeak intervals were recorded and analyzed at 91, 227, 455, and 910/s clicks. Post Hoc multiple comparisons were performed using Least-significant difference to identify any differences between the 4 different click rates for each of the latencies and intervals. In the BPD group, all latencies and interpeak intervals differed significantly between different click rates (all P < 0.001). This was also true for the non-BPD and normal term groups.
Comparison among the three groups of infants
At the click rate of 91/s, the latencies of MLS BAER waves I, III, and V, the I–III and III–V intervals, and the III–V/I–III interval ratio all differed significantly among the BPD, normal term, and non-BPD groups of infants (P < 0.05–0.001). At 227/s clicks, the latencies of waves I, III, and V, the I–III interval, and the III–V/I–III interval ratio differed significantly among the three groups (P < 0.05–0.001). At 455/s clicks, the results of comparison among these groups were the same as at 91/s clicks. At 910/s clicks, the results of comparison among these groups were the same as at 227/s clicks. Taken together, the latencies of waves I, III, and V, the I–III interval, and the III–V/I–III interval ratio differed significantly at all click rates among the BPD, normal term, and non-BPD groups.
Comparison of BPD group with normal term group
At 91/s clicks, MLS BAER wave I latency in the BPD group is longer than in the term group, which is related to a higher BAER threshold in the BPD group (P < 0.05) (Table 1). There were slight differences between the two groups of infants in the latencies of wave III and V and the I–V interval, but none differed significantly. The I–III interval in the BPD group was significantly shorter than in the term group (P < 0.01), whereas the III–V interval was significantly longer than in the term group (P < 0.01) (Table 2). The III–V/I–III interval ratio was significantly greater than in the term group (P < 0.001) (Table 2).
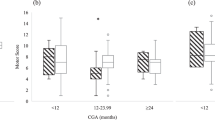
At the higher rates of 227/s, 455/s, and 910/s clicks, the results of comparison between the BPD and term groups were generally similar to those at 91/s clicks, with only small variations. Wave I latency in the BPD group is longer than in the term group at all these click rates (all P < 0.05) (Table 1), but the latencies of waves III and V did not differ significantly between the two groups at any click rates. There were no significant differences between the two groups in the I–V interval at any click rates. However, the BPD group showed a significant shortening in the I–III interval (all P < 0.01–0.001), a moderate to significant prolongation in the III–V interval (P < 0.05–0.001), and a significant increase in the III–V/I–III interval ratio (all P < 0.001) (Table 2). These distinct differences between the BPD and normal term groups can be clearly visualized in Figs. 2–4, which graphically depict the major differences between different groups of infants in the I–III and III–V intervals and III–V/I–III interval ratio, respectively.
Comparison of BPD group with non-BPD group
At 91/s clicks, MLS BAER wave I latency was similar in the two very preterm groups of infants. However, the latencies for waves III and V were both significantly shorter in the BPD group than in the non-BPD group (P < 0.05 and 0.05) (Table 1). Although the I–V interval did not differ significantly between the BPD and non-BPD groups, the I–III interval in the BPD group was significantly shorter than in the non-BPD group (P < 0.01), whereas the III–V was longer than in the non-BPD group (P < 0.05) (Table 2). The BPD group also showed a significantly greater III–V/I–III interval ratio (P < 0.001) (Table 2).
At the higher click rates of 227–910/s, there were some differences between the two very preterm groups. Wave I latency in the BPD group did not differ significantly from that in the non-BPD group at any click rates. Wave III latency was significantly shorter than in non-BPD group at all 227/s, 455/s, and particularly 910/s clicks (P < 0.05–0.01) (Table 1). Wave V latency tended to be shorter than in the non-BPD group, which differ significantly at 227/s clicks (P < 0.05) (Table 1). The I–V interval did not show any significant differences between the two groups at any click rates, although it tended to be shorter in the BPD group than in the non-BPD group. At all 227–910/s clicks, the I–III interval in the BPD group was significantly shorter than in the non-BPD group (all P < 0.01), whereas the III–V interval was longer than in the non-BPD group (all P < 0.05) (Table 2). Similar to at 91/s clicks, the III–V/I–III interval ratio in the BPD group was significantly greater than in the non-BPD group at all higher click rates (all P < 0.01–0.001) (Table 2). These differences in MLS BAER interval variables between the two very preterm groups can be clearly visualized in Figs. 2–4.
Comparison of non-BPD group with normal term group
At 91/s clicks, the latencies of waves I, III, and V in the very preterm non-BPD group were all significantly longer than in the normal term group (all P < 0.01) (Table 1). This is related to the higher BAER threshold in the non-BPD group than in the term group. However, no significant differences were found between the two groups in any of the I–V, I–III, and III–V intervals. The III–V/I–III interval ratio was almost the same in the two groups.
At the higher click rates of 227–910/s, the latencies of waves I, III, and V in the non-BPD group were also all significantly longer than in the term group (P < 0.01–0.001) (Table 1). Although there were small differences between the two groups in the I–V, I–III, and III–V intervals, none of the differences reached statistical significance at any click rates. There was also no significant difference between the two groups in the III–V/I–III interval ratio at any click rates. As depicted graphically in Figs. 2–4, no distinct differences can be seen between the non-BPD and normal term groups in any of the I–III and III–V intervals and III–V/I–III interval ratio.
Comparison of the slopes of MLS BAER variable-rate functions between different groups
Linear regression analysis was carried out between 91 and 455/s, instead of between 91 and 910/s, to more accurately examine the linear relationship of MLS BAER variables with the repetition rate of clicks.14,17 As presented in Table 3, the slopes of the latency-rate functions for waves I, III, and V in the BPD group were slightly different from those in the normal term and non-BPD groups, which did not differ significantly between any groups of infants. The slopes of the interval-rate functions for I–V, I–III, III–V, and III–V/I–III were also slightly different from those in the two control groups, without any statistical significance.
Discussion
Abnormal brainstem neural conduction in BPD survivors
The first MLS BAER study in very preterm infants with neonatal BPD revealed that at PCA 40 weeks BPD infants had major abnormalities in the MLS BAER variables that reflect neural conduction and are related to myelination and synaptic function in the auditory brainstem.12 The main abnormalities included a significant prolongation in wave V latency and the I–V and particularly III–V intervals. There was also a significant increase in the III–V/I–III interval ratio. These MLS BAER abnormalities indicate impaired or delayed neural conduction in the auditory brainstem, reflecting poor myelination and neural asynchrony, mainly in more central or rostral regions of the brainstem.12,15 This is in general agreement with previous findings that neonatal BPD had significant brain damage,18,19,20 and that at term age very preterm BPD infants were significantly associated with brain maturational delay.11
In the present study, the BPD survivors at PCA 57–58 weeks showed some clear abnormalities in the MLS BAER, but the abnormalities are different from those previously reported at term age. Compared with the normal term infants, our BPD survivors showed a prolongation in wave I latency, which is related to the higher BAER threshold and slightly lower hearing level in the BPD survivors than in the term controls. Although the I–V interval in the BPD survivors did not differ significantly from that in the term controls at any click rates, the BPD survivors showed a significant shortening in the I–III interval and a significant prolongation in the III–V interval. As a result, the III–V/I–III interval ratio was significantly increased. In BAER and MLS BAER, the I–III and III–V intervals reflect neural conduction at caudal or peripheral regions and rostral or central regions of the auditory brainstem, respectively.14,15,21,22 Clearly, postnatal neural conduction, related to myelination and synaptic function, in the caudal and rostral brainstem regions is differentially abnormal in BPD survivors.
At PCA 40 weeks the slopes of MLS BAER wave V latency-rate function and I–V and particularly III–V interval-rate functions were all significantly increased, indicating increased click rate-dependent changes and impaired synaptic efficacy.16 In the present study, no statistically significant differences were found in any slopes between any of the three groups of infants. Thus, the impaired synaptic efficacy in the auditory brainstem at PCA 40 weeks has largely recovered at PCA 57–58 weeks in BPD survivors.
The abnormalities in BPD survivors are predominately attributed by BPD but not by very preterm birth
Our results showed that wave III latency in the BPD survivors was significantly shorter than that in the non-BPD controls at all click rates. This leads to a significant shortening in the I–III interval in the BPD survivors, compared with the non-BPD infants. On the other hand, the III–V in the BPD survivors was moderately longer than in the non-BPD group. The significant shortening in the I–III interval and the moderate prolongation in the III–V led to a greater III–V/I–III interval ratio in the BPD survivors. These differences, which were true at all click rates, indicate that the main abnormalities, i.e., significantly shortened I–III interval and moderately prolonged III–V interval, in our BPD survivors are predominately attributed by BPD but not by very preterm birth. Neonatal BPD and associated perinatal conditions such as chronic sublethal hypoxia adversely affect postnatal maturation of brainstem neural conduction in very preterm infants.
To assess the postnatal effect of very preterm birth on the developing brainstem auditory function we further directly compared the MLS BAER between the very preterm non-BPD and normal term controls. The latencies of BAER wave components in the non-BPD infants were all significantly longer than in the normal term controls. The prolongation in the non-BPD infants is related to their higher BAER threshold, suggesting an abnormality in the peripheral auditory pathway. This peripheral abnormality is most likely to be conductive, which is common in infants born very preterm. The prolonged latencies are also partly related to the relatively lower hearing level in non-BPD infants. Nevertheless, there were no significant differences between the two groups of infants in any interpeak intervals at any click rates. This finding indicates that at PCA 57–58 weeks, there is no significant abnormality in brainstem neural conduction in very preterm infants who do not suffer from neonatal BPD. This provides further evidence that the MLS BAER abnormalities found in our BPD survivors must be predominately attributed by the postnatal effect of neonatal BPD and associated perinatal conditions such as chronic sublethal hypoxia but not by very preterm birth.
Differential changes in caudal and rostral brainstem regions and underlying mechanisms
This significant shortening in the I-III interval in our BPD survivors indicates accelerated neural conduction in the peripheral or caudal regions of the auditory brainstem. There are two plausible interpretations for the significant shortening in the BPD survivors; the very preterm birth and the postnatal effect of neonatal BPD. The first interpretation is that the shortening in I–III interval might be related to the very preterm birth in these BPD survivors. Some previous authors reported that premature birth, particularly very premature birth, could accelerate the maturation or development of BAER in early life, leading to a slight or moderate shortening in BAER wave latencies and/or interpeak intervals.23,24,25 In the present study, the I–III interval in our very preterm BPD survivors was not only significantly shorter than in the normal term controls but also, to a similar extent, significantly shorter than in the very preterm non-BPD infants. Furthermore, the direct comparison between the very preterm non-BPD infants and the term infants did not reveal any significant difference in the I–III interval. Therefore, the shortening in I–III interval in our BPD survivors at PCA 57–58 weeks cannot be exclusively or mainly explained by the very preterm birth.
The second and more likely interpretation of the shortening in I–III interval in our BPD survivors is the postnatal effect of neonatal BPD and some associated clinical conditions. This effect could act as a “stress” to stimulate and accelerate neural maturation of more peripheral or caudal regions of the auditory brainstem. It has been recognized that intrauterine stress (e.g., maternal hypertension) could enhance neuromotor maturation.26 BAER wave V latency and I–V interval were shortened in infants born to mothers with preeclampsia.27 The intrauterine stress of maternal preeclampsia could accelerate the maturation of the auditory nerve and brainstem auditory pathway. In our BPD survivors, the significant shortening in the I–III interval reflects accelerated maturation of more peripheral or caudal regions of the auditory brainstem at PCA 57–58 weeks. This might be an adaptive change to the “stress” of neonatal BPD and some associated perinatal conditions, leading to precocious neural maturation (opposite to retarded or delayed maturation) in more peripheral or caudal regions of the auditory brainstem. The adaptive change may not be clearly shown at term age. With the increase in postnatal age, the acceleration effect continues and gets more evident, resulting in a clear shortening in the I–III interval in our BPD survivors at PCA 57–58 weeks.
Neonatal BPD is known to be associated with significant brain damage.18,19,20 Early reports on brain myelination in infants with BPD are somewhat controversial; myelination was accelerated in some infants but delayed in others.28 Later magnetic resonance imaging studies revealed that neonatal BPD is strongly associated with an increased risk of brain white matter damage and delay in structural brain maturation.11,19,29 The significant prolongation in the I–V and III–V intervals indicates significantly impaired or delayed myelination and synaptic dysfunction in the auditory brainstem in BPD infants at term age.12 More recently, we carried out a follow-up study. As reported in the present study at PCA 57–58 weeks, although there was no apparent abnormality in the I–V interval, the III–V interval in our BPD survivors was still moderately prolonged at all click rates, which was apparently less significant relative to the major prolongation found at term age.12 The continuous but less severe prolongation in the III–V interval in our BPD survivors indicates that the major impairment of neural conduction at more central or rostral regions of the brainstem, reported at PCA 40 weeks, has improved at PCA 57–58 weeks, but has not completely recovered. There remained a moderate degree of neural conduction impairment or delay in the rostral regions of the brainstem.
Some of our BPD survivors were followed up to 1 year of corrected age. The general trend in the differential changes in MLS BAER intervals was similar to the present study at four months of corrected age, without any major changes, including significantly shortened I–III interval, moderately prolonged III–V interval and significantly increased III–V/I–III interval ratio. During the follow-up, the clinical condition and neurodevelopment in those BPD survivors with persistent MLS BAER abnormalities are generally less favorable. As the data obtained so far remain limited and not solid enough for robust statistical analysis, no conclusion can be reached at this stage, which is a limitation of the present study. Nevertheless, such a preliminary finding does suggest that the postnatal abnormality in brainstem neural conductions in BPD survivors is likely to persist for a longer time. Further studies are warranted to elaborate our findings and explore their clinical implication.
Conclusions
Our BPD survivors at PCA 57–58 weeks showed clear abnormalities in the MLS BAER variables that reflect brainstem neural conduction, including the I–III and III–V intervals and the III–V/I–III interval ratio. The major differences in these MLS BAER variables between the BPD survivors and normal term infants and between the BPD survivors and non-BPD infants were generally similar. In addition, no major differences in these MLS BAER variables were found between the very preterm non-BPD infants and normal term infants. Thus, the major differences found in our BPD survivors from the normal infants and non-BPD infants reflect the postnatal effect of neonatal BPD and associated perinatal conditions on brainstem neural conduction.
A recent analysis of neurodevelopmental risk factors in premature infants found that BPD could be associated with accelerated brainstem auditory maturation.30 In our present study of BPD survivors, the major MLS BAER abnormalities included a significant shortening in the I–III interval but a significant prolongation in the III–V and a significant increase in the III–V/I–III interval ratio. These abnormalities existed consistently at all click rates. Such differential changes in the I–III and III–V intervals suggest differential changes in neural conduction of caudal and rostral brainstem regions in the BPD survivors. Clearly, postnatal maturation of neural conduction at the caudal and rostral regions of the brainstem is differentially affected by neonatal BPD and associated perinatal conditions; the maturation is accelerated in caudal brainstem regions but delayed in rostral regions. Neonatal BPD has a prolonged postnatal effect on postnatal maturation of brainstem neural conduction. The survivors are associated with differential maturation in neural conduction at caudal and rostral brainstem regions, which may constitute an important risk for postnatal neurodevelopment in very preterm infants who survive neonatal BPD.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Lapcharoensap, W. et al. Hospital variation and risk factors for bronchopulmonary dysplasia in a population-based cohort. JAMA Pediatr. 169, e143676 (2015).
Sahni, M. & Bhandari, V. Recent advances in understanding and management of bronchopulmonary dysplasia. F1000Res 14, 9, https://doi.org/10.12688/f1000research.25338.1 (2020). F1000 Faculty Rev-703eCollection 2020.
Tracy, M. K. & Berkelhamer, S. K. Bronchopulmonary dysplasia and pulmonary outcomes of prematurity. Pediatr. Ann. 48, e148–e153 (2019).
Deakins, K. M. Bronchopulmonary dysplasia. Respir. Care 54, 1252–1262 (2009).
Doyle, L. W. & Anderson, P. J. Long-term outcomes of bronchopulmonary dysplasia. Semin. Fetal Neonatal Med. 14, 391–395 (2009).
Jeng, S. F. et al. Bronchopulmonary dysplasia predicts adverse developmental and outcomes in very-low-birthweight infants. Dev. Med. Child Neurol. 50, 51–57 (2008).
Karagianni, P. et al. Neuromotor outcomes in infants with bronchopulmonary dysplasia. Pediatr. Neurol. 44, 40–46 (2011).
van Marter, L. J. Epidemiology of bronchopulmonary dysplasia. Semin. Fetal Neonatal Med. 14, 358–366 (2009).
Raman, L., Georgieff, M. K. & Rao, R. The role of chronic hypoxia in the development of neurocognitive abnormalities in preterm infants with bronchopulmonary dysplasia. Dev. Sci. 9, 359–367 (2006).
Suppiej, A. et al. Neonatal cortical auditory evoked potentials are affected by clinical conditions occurring in early prematurity. J. Clin. Neurophysiol. 32, 419–423 (2015).
Neubauer, V., Junker, D., Griesmaier, E., Schocke, M. & Kiechl-Kohlendorfer, U. Bronchopulmonary dysplasia is associated with delayed structural brain maturation in preterm infants. Neonatology 107, 179–184 (2015).
Wilkinson, A. R., Brosi, D. M. & Jiang, Z. D. Functional impairment of the brainstem in infants with bronchopulmonary dysplasia. Pediatrics 120, 362–371 (2007).
Jiang, Z. D. Auditory impairment is alleviated after term in infants with neonatal chronic lung disease. Acta Paediatr. 106, 926–929 (2017).
Jiang, Z. D. Maximum length sequence technique improves detection of neuropathology involving infant brainstem. In: Pediatric Neurology (eds Lawson, P. N. & McCarthy, E. A.) 1–38 (Nova Science Publishers, New York, 2012).
Jiang, Z. D. Evoked potentials in pediatric brainstem lesions. In: Clinical Neurophysiology in Pediatrics: A Practical Approach to Neurodiagnostic Testing and Management (ed Galloway, G.) 187–213 (Demos Medical Publishing, LLC, New York, 2015).
Wilkinson, A. R. & Jiang, Z. D. Brainstem auditory evoked response in neonatal neurology. Semin. Fet. Neonatol. 11, 444–451 (2006).
Jiang, Z. D., Pin, L. L. & Wilkinson, A. R. Functional abnormality of the auditory brainstem in high-risk late preterm infants. Clin. Neurophysiol. 123, 993–1001 (2012).
Chess, P. R., D’Angio, C. T., Pryhuber, G. S. & Maniscalco, W. M. Pathogenesis of bronchopulmonary dysplasia. Semin. Perinatol. 30, 171–178 (2006).
Gagliardi, L., Bellù, R., Zanini, R. & Dammann, O. Bronchopulmonary dysplasia and brain white matter damage in the preterm infant: a complex relationship. Paediatr. Perinat. Epidemiol. 23, 582–590 (2009).
Gien, J. & Kinsella, J. P. Pathogenesis and treatment of bronchopulmonary dysplasia. Curr. Opin. Pediatr. 23, 305–313 (2011).
Jiang, Z. D., Brosi, D., Wu, Y. Y. & Wilkinson, A. R. Relative maturation of the peripheral and central regions of the auditory brainstem from preterm to term and the influence of preterm birth. Pediatr. Res. 65, 657–662 (2009).
Jiang, Z. D. & Ping, L. L. Functional integrity of rostral regions of the immature brainstem is impaired in babies born extremely preterm. Clin. Neurophysiol. 127, 1581–1588 (2016).
Collet, L., Soares, I., Morgon, A. & Salle, B. Is there a difference between extrauterine and intrauterine maturation on BAEP? Brain Dev. 11, 293–296 (1989).
Pasman, J. W., Rotteveel, J. J., de Graaf, R., Stegeman, D. F. & Visco, Y. M. The effect of preterm birth on brainstem, middle latency and cortical auditory evoked responses (BMC AERs). Early Hum. Dev. 31, 113–129 (1992).
Pasman, J. W., Rotteveel, J. J., de Graaf, R., Maassen, B. & Visco, Y. M. The effects of early and late preterm birth on brainstem and middle-latency auditory evoked responses in children with normal neurodevelopment. J. Clin. Neurophysiol. 13, 234–241 (1996).
Amiel-Tison, C. & Pettigrew, A. G. Adaptive changes in the developing brain during intrauterine stress. Brain Dev. 13, 67–76 (1991).
Kim, C. R., Vohr, B. R. & Oh, W. Effects of maternal preeclampsia on brain-stem auditory evoked response in very low birth weight infants. J. Pediatr. 127, 123–127 (1995).
Takashima, S. & Becker, L. E. Developmental neuropathology in bronchopulmonary dysplasia: alteration of glial fibrillary acidic protein and myelination. Brain Dev. 6, 451–457 (1984).
Thompson, D. K. et al. Perinatal risk factors altering regional brain structure in the preterm infant. Brain 130, 667–677 (2007).
Borenstein-Levin, L. et al. Effects of neurodevelopmental risk factors on brainstem maturation in premature infants. Pediatr. Res. https://doi.org/10.1038/s41390-021-01849-0 (2021).
Acknowledgements
We are indebted to doctors and nurses at Neonatal Division of Children’s Hospital for their enthusiastic assistance in the recruitment of the subjects and collection of data.
Author information
Authors and Affiliations
Contributions
J.K.J. made a major contribution to data analysis and manuscript writing. C.W. was responsible for recording MLS BAER and collecting clinical data. Z.D.J. designed and supervised the study and was responsible for the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent to participate
Informed parental consent was obtained for each infant.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jiang, J.K., Wang, C. & Jiang, Z.D. Postnatal abnormality in brainstem neural conduction in neonatal bronchopulmonary dysplasia survivors. Pediatr Res 93, 1679–1686 (2023). https://doi.org/10.1038/s41390-022-02222-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02222-5