Abstract
Neonatal hypoxic–ischemic brain injury (HIBI) is a devastating injury resulting from impaired blood flow and oxygen delivery to the brain at or around the time of birth. Despite the use of therapeutic hypothermia, more than one in four survivors suffer from major developmental disabilities—an indication of the critical need for more effective therapies. MicroRNAs (miRNA) have the potential to act as biomarkers and/or therapeutic targets in neonatal HIBI as a step toward improving outcomes in this high-risk population. This review summarizes the current literature around the use of cord blood and postnatal circulating blood miRNA expression for diagnosis or prognosis in human infants with hypoxic-ischemic encephalopathy, as well as animal studies assessing endogenous brain miRNA expression and potential for therapeutic targeting of miRNA expression for neuroprotection. Ultimately, the lack of knowledge regarding brain specificity of circulating miRNAs and the temporal variability in expression currently limit the use of miRNAs as biomarkers. However, given their broad effect profile, ease of administration, and small size allowing for effective blood-brain barrier crossing, miRNAs represent promising therapeutic targets for improving brain injury and reducing developmental impairments in neonates after HIBI.
Impact
-
The high morbidity and mortality of neonatal hypoxic-ischemic brain injury (HIBI) despite current therapies demonstrates a need for developing more sensitive biomarkers and superior therapeutic options.
-
MicroRNAs have been evaluated both as biomarkers and therapeutic options after neonatal HIBI.
-
The limited knowledge regarding brain specificity of circulating microRNAs and temporal variability in expression currently limit the use of microRNAs as biomarkers.
-
Future studies comparing the neuroprotective effects of modulating microRNA expression must consider temporal changes in the endogenous expression to determine appropriate timing of therapy, while also optimizing techniques for delivery.
Similar content being viewed by others
Introduction
Neonatal hypoxic–ischemic encephalopathy (HIE)—the clinical phenotype resulting from perinatal hypoxic–ischemic brain injury (HIBI)—affects on average 8 out of every 1000 live births worldwide.1 Therapeutic hypothermia decreases mortality and neurodevelopmental impairment in survivors of HIE, but has not been shown to be beneficial in low- or middle-income countries.2,3 Even in high resource settings, the neuroprotection by hypothermia is incomplete, as despite its use, approximately 46% of infants still die or develop major disabilities.3 Given the significant continued morbidity and mortality after neonatal HIE, novel therapies are urgently needed. Current therapies, including hypothermia, rely on non-specific targeting of general inflammatory and excitatory injury; improving on these will likely require therapies more targeted to the specific cellular signals induced by neonatal HIBI.
In animal models, systemic injection of mesenchymal stem cells after HIBI attenuates brain injury and improves neurological outcomes.4 A phase I clinical trial demonstrated feasibility and early safety of stem cell transfusion in human neonates,5 though the availability of equipment and expertise to successfully and aseptically perform autologous stem cell transplantation is currently limited to only a few high-resource institutions. There is wide consensus that much of the therapeutic benefit of stem cell transplantation lies in the cell-to-cell signaling factors such as microRNAs (miRNA),6,7 however, which could be harnessed to provide more available neuroprotective options after neonatal HIBI.8 Although miRNA-based therapies have been tested in several adult brain injury and disease processes,9 much of the miRNA research in neonatal HIBI to date has focused on biomarker development rather than therapy. This article will review the biogenesis of miRNAs and the existing literature evaluating the therapeutic potential of altering miRNA in neonatal HIBI and will assess the current gaps in the literature for researchers interested in pursuing this avenue of pediatric research. Although preterm HIBI is also a significant issue, there are substantial differences in pathophysiology and developmental response to injury in preterm infants. Therefore, this review will focus on data from term infants and animal models representing term gestation.
MicroRNA synthesis and microRNA-regulated gene expression
MiRNAs are small non-coding RNAs that modulate gene expression primarily through post-transcriptional silencing of messenger RNAs (mRNA). MiRNAs average 22 nucleotides in length and miRNA genesis primarily occurs through the canonical pathway which uses Drosha to process the pri-miRNA to pre-miRNA and Dicer to splice the pre-miRNA into mature miRNA (Fig. 1).10 The canonical miRNA genesis pathway terminates with the 5p strand (derived from the 5’ end of the pre-miRNA) or the 3p strand (derived from the 3’ end) of the miRNA binding to argonaute (Ago) proteins in an ATP-dependent manner.11 The selection of the strand for integration with Ago depends on the thermodynamic stability at the 5’ end of the miRNA duplex or a 5’ uracil at the first nucleotide position.12 Although the design and synthesis of miRNA mimics and antagonists is outside the scope of this current review, the Ago selectivity is one of the key features of miRNA function that can be leveraged to improve the efficacy of miRNA interventions.13
After transcription, pri-miRNA are cleaved into pre-miRNA by Drosha and DiGeorge Syndrome Critical Region 8 (DGCR8) before transfer to the cytoplasm where Dicer and transactivation response element RNA-binding protein (TRBP) further cleave the pre-miRNA into a mature miRNA duplex. The mature miRNA is integrated with argonaute (Ago) proteins in the RNA-induced silencing complex (RISC) to inhibit messenger RNAs (mRNA).
The resulting miRNA-Ago complex is termed the RNA-induced silencing complex (RISC). The RISC uses its miRNA guide strand to selectively bind with complementary sequences on the 5’ untranslated region of mRNAs, referred to as miRNA response elements (MRE). Since each miRNA can target multiple mRNAs with similar MREs, small changes in miRNA expression have the potential to trigger significant physiological effects. Additionally, each mRNA may have several miRNA regulators (see Fig. 2 as example). Thus, better understanding the endogenous miRNA expression changes after injury can provide important insight into HIBI pathophysiology.
MicroRNA detection and measurement of expression
Multiple technologies currently exist for the detection and quantification of miRNAs. Microarrays provide quantitative expression values for a selected number of miRNAs, and were the standard high-throughput method used for many years. Although the number of miRNAs analyzed by a single microarray now exceeds 30,000, the decreasing cost of next-generation sequencing and its ability to provide results for both known and novel miRNAs has resulted in increased use of this technology. Regardless of the method used, however, because the large amount of data from high-throughput studies results in relatively high risk for false discovery, subsequent confirmatory studies are vital for the validation of any target miRNA. These studies are generally performed using polymerase chain reaction, which has a wider range, more sensitive quantification limits, and less biased results, but is much more time intensive when sequencing many miRNAs.
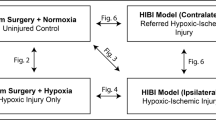
Although several miRNA studies have been performed in humans with hypoxic-ischemic encephalopathy, studies of organ-specific miRNA expression, mechanistic studies, and early therapeutic trials rely on animal models. The process of miRNA genesis and processing is well conserved among animals,14 and though only ~30% of human miRNA genes are highly conserved across mammalian species, those 30% are the most highly expressed miRNAs in humans.15 The remaining miRNAs that are not strongly conserved, however, complicate the interpretation of animal-based miRNA studies. For instance, miR-374a is discussed several times in this review but is a human miRNA that is not expressed in rodents. It still may be possible to test the therapeutic potential of human-specific miRNA interventions in the rodent model, as one study using the rat model of neonatal HIBI demonstrated significant attenuation of inflammatory cytokines and brain injury after intracerebroventricular injection of miR-374a-5p mimic developed from the human miR-374a sequence.16 The translational potential of these cross-species studies, however, has not yet been determined. Lastly, although several studies have examined the conservation of baseline miRNA expression across species, very little is known at this time about the conservation of miRNA expression response to injury such as HIBI across different species.
Effects of hypoxia–ischemia on endogenous microRNA expression
MiRNAs are thought to play a significant role in modulating neuroinflammation after HIBI and therefore represent promising targets for therapeutic intervention.17 Much of the literature to date regarding miRNAs in neonatal HIBI has focused on a class of miRNAs known as hypoxamiRs. HypoxamiRs, including the commonly studied miR-21 and -210 but also miR-335, -137, and -376c, undergo regulation by hypoxia and in turn regulate cells’ response to decreased oxygen.18 These hypoxamiRs have been shown to play a significant role in several pathological states, from cardiac injury to cancer,19,20 and modulating their concentrations in the brain after HIBI may provide neuroprotection.21,22,23 Due to their small size, miRNAs are more likely to cross the blood-brain-barrier than other larger molecules currently being tested as therapeutics.24 The question of which miRNA(s) to target remains a significant hurdle in the path toward developing successful miRNA-based therapies.
MicroRNA expression changes in human cord blood
To date, three published studies have attempted to profile the serum miRNA changes in human newborns with HIE using high-throughput analyses.25,26,27 Two of these studies assessed only cord blood changes, with the third (discussed in the next section) also assessing postnatal miRNA changes. The two earlier studies25,26 used the same cohort of infants but two different approaches to miRNA detection: next generation sequencing versus microarray. Between the two studies, the investigators identified at least 107 microRNAs that were significantly up- or downregulated in newborns diagnosed with HIE. Differences in reporting of the miRNA species/strands hinders rigorous comparison of results from the two studies, though 18 miRNAs were found to have altered regulation in both studies. Only 1 of the 18—miR-142—was also dysregulated in cord blood in the recently published study by Winkler et al.,27 though there were three additional miRNAs with altered regulation in the Winkler study that were demonstrated to be altered in just one of the two previous studies (Supplementary Table 1).
Several of the miRNAs found to be altered in cord blood have also been shown to have altered regulation in the peripheral blood of neonates after HIE. For example, down-regulated miR-30b was strongly associated with increased platelet activation marker CD26P and the plasma fibrinolytic marker plasminogen activator inhibitor 1 (PAI-1).28 In a validation cohort of one of the cord studies described above, the investigators re-demonstrated decreased expression of miR-374a in infants diagnosed with HIE versus controls.29 Downregulation of miR-374a and miR-376c in umbilical cord blood were also confirmed by separate research teams.30,31 Additionally, the activin-A receptor type IIb gene, which is a predicted target of miR-374a, has been shown to be elevated in infants with severe HIE (though not moderate or mild HIE) compared to controls.32 Overexpression of miR-376c has been associated with increased cell viability, in part due to inhibition of ING5.33 Although miR-376c has been evaluated in several oncological studies, its role in brain development and/or injury has not yet been well defined. Lastly, although not consistently demonstrating altered expression in their previous studies,25,26,29 an additional study by Looney et al. evaluated umbilical cord blood levels of miR-181b and its predicted target ubiquitin C-terminal hydrolase-L1 (UCH-L1). In this most recent study, miR-181b was significantly downregulated in infants with moderate to severe HIE compared to controls, with a corresponding upregulation of UCH-L1 mRNA.34
Probably the most well studied hypoxia-related miRNA is miR-210. Although none of the high-throughput studies of umbilical cord blood described above demonstrated HIE-related changes in miR-210, another study that analyzed only miR-374a and miR-210 in cord blood did demonstrate significant decreases in both miR-210 and miR-374a expression in infants with HIE versus healthy controls.30 A recent study showed the inverse pattern: increased miR-210 expression in cord blood of infants with perinatal asphyxia.35 This study did not separate those with HIE and those with asphyxia without encephalopathy, however, so the results may not be directly comparable between the two studies.
Each of the studies above investigated cord blood miRNA expression, with the primary goal of determining the prognostic potential of miRNAs as biomarkers. When considering miRNAs as therapeutic targets, however, it is important to note that hypoxic-ischemic encephalopathy is rarely differentiated from perinatal depression or birth asphyxia (which may or may not result in encephalopathy) prior to 30–60 min of life and, at least in the piglet model of HIBI, many of the key miRNAs that were differentially expressed at the time of injury (equivalent to cord blood in humans) returned to baseline by 30 min after injury.36 Thus, studies assessing therapeutic potential must also assess miRNA expression throughout the first hours to days after HIBI.
Temporal miRNA expression changes after HIBI
Neonatal HIBI is a triphasic injury.37 The first phase starts with the initial hypoxic-ischemic insult, and the primary energy failure and hypoperfusion result in necrotic cell death in the first minutes to hour after the restoration of normoxia and adequate perfusion. The secondary phase starts between 6 and 12 h after injury and continues until about 72 h after injury. It is characterized by deteriorating mitochondrial function and an acute inflammatory response, with apoptosis being the hallmark cell death process during this phase. Then the tertiary phase includes partial recovery from the injury as well as continued inflammation and gliosis.38 Importantly, between the primary and secondary phases of injury is a latent phase characterized by partial metabolic recovery; this is the target period for initiating therapeutic hypothermia, in order to partially prevent the secondary phase injury.
Consistent with the triphasic nature of neonatal HIBI, miRNA expression also varies over time after ischemic injury. Several miRNAs have been shown to have multiple phases of expression throughout the first 72 h after injury, thought to be related to the multiphasic nature of the expression of hypoxia inducible factor 1 subunit α (HIF1α) and other hypoxia-regulating genes after ischemia. For instance, miR-335 was shown to be downregulated in the first hours after middle cerebral artery occlusion, followed by significant upregulation around 24 h, and then downregulation again after 24 h.23 As a consequence of this multiphasic expression pattern, miR-335 mimic was shown to be neuroprotective when administered immediately after injury but miR-335 antagonist was neuroprotective when administered at 24 h after injury, corresponding to inverse endogenous expression between the two time points.23 Our group observed similar multiphasic expression patterns of miR-335 and other miRNAs (including miR-137 and −376c) in a study of neonatal mouse brain miRNA expression at 24 and 72 h after HIBI.39
Only one study of human HIBI miRNA expression used high-throughput analyses outside of cord blood,27 using microarray to assess differential miRNA expression at the time of NICU admission and at 72 h of life (Table 1). Several other studies, however, have assessed expression of individual miRNAs in the first hours or days after injury. One such study demonstrated decreased expression of miR-410 in the circulating blood at around 6 h after injury,40 which is consistent with the direction of altered expression in cord blood. After subsequently observing overexpression of miR-410 in a cell culture oxygen-glucose deprivation (OGD) model, the authors proposed that miR-410 and the beneficial effects of its upregulation are related to interactions with phosphatase and tensin homolog (PTEN). Consistent with these findings, investigators recently demonstrated that administering miR-410 from mesenchymal stem cell-derived extracellular vesicles also increased cell viability and decreased neuronal apoptosis in an OGD model.41
One study in humans demonstrated elevations in miR-21 at 24–48 h after HIE that were associated with elevated HIF1 levels.42 Another study assessed dried blood spot miRNA values at 18–19 h after neonatal HIE, demonstrating strong correlation between miRNA levels in dried blood spot versus whole blood samples, but showed no differences between HIE and controls in any of the five miRNAs that they assessed, which included miR-21 as well as let-7b, miR-29b, miR-124, and miR-155.43
The expression of miR-210 outside of the immediate injury period has been evaluated in a few studies, including one human study. In a study using a piglet model of HIBI, plasma miR-210 increased from pre-injury to immediately post-injury by 3.5-fold, but then returned to baseline levels by 30 min and remained near baseline at 9.5 h after injury.36 This study did not assess brain levels of miRNAs, which may explain the difference between their findings and those of investigators evaluating brain miR-210 levels in the rat model of HIBI. In the rat model, studies demonstrated prolonged higher brain miR-210 expression at 3, 6, 12, and 24 h after HIBI compared to sham operated normoxic control animals.8,44 A separate study in the rat model demonstrated decreased expression of miR-210 in the brain at 72 h after neonatal HIBI compared to controls.45 In the one human study specifically assessing miR-210 levels after the immediate injury period, investigators demonstrated significant elevations (1.8-fold) of peripheral blood miR-210 expression at 72 h of life in infants who had suffered perinatal asphyxia versus healthy controls,46 which was inverse to the brain-specific levels seen in the rodent study. Taken together (Fig. 3), these results suggest a discordance between brain and plasma miRNA expression, so future studies should consider obtaining paired plasma and brain samples to better evaluate the specificity of circulating blood microRNAs as a readout for changes in brain miRNAs. Differences in technique and species expression, however, must also be considered.
In the cord blood study performed by Looney et al., miR-374a was the most sharply downregulated miRNA in infants with HIE compared to healthy controls, a finding they and others have subsequently confirmed in validation studies.25,30,47 Despite the downregulation in human umbilical cord blood which has been consistently demonstrated across several studies, miR-374a levels were found to be upregulated in the plasma of the piglet model after HIBI.36 Levels were elevated immediately after injury, but then decreased rapidly so that, although still elevated at 30 min, they were back to baseline by 3.5 h after injury.
MiR-181a was also evaluated in the piglet model, with upregulation compared to controls only at 1 h after injury, but not before or after that time point.26 Of note, this finding was also inverse to what has been shown in the human cord blood studies. Upregulation of miR-181a shortly after ischemic brain injury is supported by studies in adult ischemic stroke demonstrating upregulation 30 min after injury in a rat model.48 One potential issue with using circulating miR-181a as a biomarker of ischemic brain injury, however, is that it is not specific to the brain and has also been found to be upregulated after myocardial ischemia,49 which may also occur after neonatal asphyxia. Additionally, in one study of adult stroke, miR-181a was only upregulated in the brains of male mice, with no difference after injury in female mice.50
Human studies of miRNA expression are understandably limited to only circulating blood values, as the availability of invasively collected neonatal tissue samples is extremely limited. As such, the human miRNA expression may not fully reflect brain injury and the findings from cord blood studies or neonatal peripheral blood could therefore vary based on the amount of systemic organ (e.g. heart, liver, kidney, etc.) injury that results from the asphyxia. It has been shown that the traditional laboratory markers of hepatic injury (e.g. aspartate transaminase, alanine transaminase) and kidney injury (e.g. creatinine) can vary greatly and do not consistently correlate with the diagnosis or severity of neonatal HIE,51 so there is no reason to suspect that miRNA levels would be different. Although cord blood testing is appealing due to the ease and non-invasive nature of obtaining cord blood versus circulating blood from the newborn, additional care must be taken when interpreting cord blood values, especially for small molecules such as miRNAs that easily cross the placenta. Several studies have demonstrated that placental development and disorders significantly alter the circulating miRNA profile in both humans and animals.52,53
Brain miRNA changes after HIBI
To overcome some of the current limitations of human miRNA testing, several investigators including our research group have begun to develop brain specific profiles of miRNA expression after neonatal HIBI. These studies provide more organ-specific data for therapeutic targeting and have brought to light the importance of injury timing when measuring miRNA expression levels. Specifically, they have confirmed the multi-phasic expression changes that have been demonstrated in adult studies and neonatal plasma studies. The miRNA expression findings from these studies and the correlation with the studies evaluating expression patterns in the circulating blood are summarized in Table 1. A comprehensive list of all miRNA alterations after neonatal HIBI is included in Supplementary Table 1.
Inspired by the studies in adult diseases, several investigators have begun to investigate the therapeutic potential of altering miRNA expression before, during, and after neonatal brain injury (Table 2).
MicroRNAs as therapeutic targets for hypoxic–ischemic brain injury
A few groups have attempted to modulate miR-210 expression to attenuate brain injury after hypoxia-ischemia. In the study of brain miR-210 levels described above, miR-210 was persistently upregulated between 3 and 24 h after injury.8 As such, most of the interventional studies have attempted to decrease miR-210 through administration of antagonists. In models of neonatal HIBI, miR-210 inhibition improved expression of glucocorticoid receptors,8 suppressed microglia-mediated inflammation in part by stimulating increases in nuclear factor (NF)-kB,44,54 ameliorated mitochondrial dysfunction caused by miR-210-associated downregulation of the iron–sulfur cluster assembly protein,55 and reduced cerebral edema and IgG leakage into brain parenchyma, suggesting improvement in blood-brain barrier integrity.56 One potentially contradictory study demonstrated that augmenting miR-210 expression after HIBI by intracerebroventricular injection of miR-210 mimic (rather than antagonist, as in the studies above) led to decreased apoptosis.45 The authors did not specifically state the timing of when the injections were performed relative to the injury, however, making it difficult to truly compare their results to the other studies that have all demonstrated consistent neuroprotective effects of miR-210 antagonism.
Other miRNAs that were shown to be altered after neonatal HIBI (Supplementary Table 1) and have been successfully manipulated in neonatal HIBI include miR-374a, -326, -134, -181a, and -185. Overexpression of miR-374a through intracerebroventricular injection of miR-374a mimic attenuated brain injury and inhibited release of pro-inflammatory cytokines in a neonatal rat model, potentially through NOD-, LRR-, and pyrin domain-containing protein 3 (NLRP3) inflammasome alteration.16 Similarly, knockdown of miR-326 upregulated the expression of the δ-opioid receptor, improved cell survival, and decreased caspase-3- and Bax-related apoptosis.57 MiR-134 inhibition by intracerebroventricular injection attenuated HIBI in a rat model, related to C/EBPa and KPNA3 expression.58 MiR-181a antagonist administered at 60 min after injury reduced infarct size and improved neurological outcomes in a mouse model.59 Lastly, miR-185 knockout by CRISPR/CAS9 resulted in decreased infarct size, higher neuronal survival, and improved motor and cognitive deficits in a rat model.60 This effect was determined to be related to IGFBP3 expression.
Additionally, a few other miRNA alterations have been tested despite a lack of prior data to suggest that they are significantly altered in the brain or plasma after neonatal HIBI. For example, neuroprotective benefits were demonstrated with the administration of miR-204 mimic, resulting in increased neuronal proliferation and decreased neuronal apoptosis.61 Overexpression of miR-124 promoted cell survival and attenuated neuronal apoptosis, resulting in improved testing of memory and neurological function at one and two months after injury.62 Finally, administration of miR-454 mimic improved cell viability in OGD injured neurons, likely related to effects on suppression of tumorigenicity 18 (ST18) expression.63
Once potentially therapeutic miRNA alterations are established, the next step in designing miRNA-based therapeutics is to determine the optimal mode of delivery. Although many studies have used direct intracerebroventricular injection of free oligonucleotides, this is not an approach that is universally accepted as clinically feasible, and the kinetics of administering free oligonucleotides by other routes has not been thoroughly evaluated in neonatal HIBI.
MicroRNA delivery
Free circulating miRNAs have a half-life as short as 90 min, which could limit the feasibility of intravascular administration of miRNA-based therapeutics.64 However, miRNAs can be administered intranasally,8,65 bypassing the blood–brain barrier and minimizing possible off-target systemic effects compared to intravenous administration,66 with adequate brain tissue penetration within 30 min after administration of 0.5–1 nmol of miRNA.21,65,67 If intravenous administration is preferred, however, another method to extend the miRNA half-life and improve brain tissue targeting is by binding the miRNAs to nanoparticles (as has been used in studies of preterm brain injury68) or inserting the miRNAs into protective vessels such as extracellular vesicles (EVs) to decrease their uptake by the reticuloendothelial system.
EVs are a heterogeneous group of membrane-bound vesicles that are released by various types of cells69 and carry a variety of cargo including miRNAs, proteins and lipids.70 When administered intravenously to a mouse model of adult stroke, mesenchymal stem cell (MSC)-derived EVs improved in neuronal survival and angioneurogenesis, with results similar to a comparison group receiving MSCs.71 EVs modified to overexpress certain miRNA have shown improved neurogenesis and functional recovery in models of adult stroke72,73 and have recently received attention for their potential in neonatal brain injury.74 Although the EVs carry a range of potentially therapeutic molecules including RNAs and proteins, a recent study demonstrated that administering MSC-derived EVs to OGD-injured neurons decreased apoptosis and improved cell survival. This protection was lost when the EVs were pretreated with RNase but not when pretreated with proteinase.41 Very recently, several studies have reported the therapeutic potential of EV administration for neonatal HIBI in animal models of term brain injury,75,76 including the roles that miRNAs may play in their beneficial effects.77,78
Limitations and gaps in the current literature
Although miRNA profiling provides increased insight into the pathophysiology of neonatal HIBI and offers potential targets for future therapeutic studies, it is important to note two significant limitations: (1) differential expression of a miRNA after HIBI is not equivalent to pathologic expression, and (2) a lack of differential expression in a miRNA does not rule out therapeutic potential. The latter point may be best exemplified by miR-210, which has been demonstrated to be an effective target in multiple studies of neonatal HIBI and yet has not been consistently demonstrated to have altered expression in blood or brain studies.
Studies of circulating miRNA expression are vital in our understanding of human miRNA changes after HIBI, but currently the results are limited by the non-specific nature of the free circulating miRNAs in detecting brain injury. It is possible that this limitation could be partially overcome by identifying the miRNAs contained within circulating EVs carrying brain-specific markers such as neuronal L1 cell adhesion molecule (L1CAM).79 Additionally, although EVs are promising therapeutic vessels for miRNAs, the ideal route of delivery, dose, and frequency of EV administration have not yet been determined, and no study to date has evaluated the feasibility of manufacturing EVs that would deliver specific neuroprotective miRNAs.
Conclusions
This review has identified several promising miRNAs for future investigations into miRNA-based therapeutic interventions. Given the multifactorial nature of neonatal HIBI, it is likely that a combination of miRNAs would need to be targeted to achieve maximal benefit. In order to better translate the pre-clinical miRNA studies to human infants, more sensitive analyses of postnatal circulating miRNAs must be performed. Ultimately, given their broad effect profile, ease of administration, and small size allowing for effective blood–brain barrier crossing, miRNAs represent promising targets for improving brain injury and reducing developmental impairments in neonates who suffer from HIE.
Data availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
Lee, A. C. C. et al. Intrapartum-related neonatal encephalopathy incidence and impairment at regional and global levels for 2010 with trends from 1990. Pediatr. Res. 74, 50–72 (2013).
Pauliah, S. S., Shankaran, S., Wade, A., Cady, E. B. & Thayyil, S. Therapeutic hypothermia for neonatal encephalopathy in low- and middle-income countries: a systematic review and meta-analysis. PLoS ONE 8, e58834–e58834 (2013).
Jacobs, S. E. et al. Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst. Rev. CD003311 (2013).
Serrenho, I. et al. Stem cell therapy for neonatal hypoxic-ischemic encephalopathy: a systematic review of preclinical studies. Int. J. Mol. Sci. 22, 3142 (2021).
Cotten, C. M. et al. Feasibility of autologous cord blood cells for infants with hypoxic-ischemic encephalopathy. J. Pediatr. 164, 973.e1–979.e1 (2014).
Li, N., Long, B., Han, W., Yuan, S. & Wang, K. MicroRNAs: important regulators of stem cells. Stem Cell Res. Ther. 8, 110–110 (2017).
Gangaraju, V. K. & Lin, H. MicroRNAs: key regulators of stem cells. Nat. Rev. Mol. Cell Biol. 10, 116–125 (2009).
Ma, Q. et al. Inhibition of microRNA-210 provides neuroprotection in hypoxic–ischemic brain injury in neonatal rats. Neurobiol. Dis. 89, 202–212 (2016).
Sun, P., Liu, D. Z., Jickling, G. C., Sharp, F. R. & Yin, K.-J. MicroRNA-based therapeutics in central nervous system injuries. J. Cereb. Blood Flow Metab. 38, 1125–1148 (2018).
Abdelfattah, A. M., Park, C. & Choi, M. Y. Update on non-canonical microRNAs. Biomol. Concepts 5, 275–287 (2014).
Yoda, M. et al. Atp-dependent human RISC assembly pathways. Nat. Struct. Mol. Biol. 17, 17–23 (2010).
Khvorova, A., Reynolds, A. & Jayasena, S. D. Functional siRNAs and miRNAs exhibit strand bias. Cell 115, 209–216 (2003).
Kadekar, S. et al. Synthetic design of asymmetric miRNA with an engineered 3′ overhang to improve strand selection. Mol. Ther. Nucleic Acids 16, 597–604 (2019).
Zhang, X. et al. Conservation of differential animal microRNA processing by Drosha and Dicer. Front. Mol. Biosci. 8, 730006 (2022).
Liang, H. & Li, W.-H. Lowly expressed human microRNA genes evolve rapidly. Mol. Biol. Evol. 26, 1195–1198 (2009).
Chen, Z., Hu, Y., Lu, R., Ge, M. & Zhang, L. MicroRNA-374a-5p inhibits neuroinflammation in neonatal hypoxic-ischemic encephalopathy via regulating Nlrp3 inflammasome targeted Smad6. Life Sci. 252, 117664 (2020).
Cho, K. H. T., Xu, B., Blenkiron, C. & Fraser, M. Emerging roles of miRNAs in brain development and perinatal brain injury. Front. Physiol. 10, 227 (2019).
Greco, S. & Martelli, F. MicroRNAs in hypoxia response. Antioxid. Redox Signal. 21, 1164–1166 (2014).
Azzouzi, H. E., Leptidis, S., Doevendans, P. A. & De Windt, L. J. Hypoxamirs: regulators of cardiac hypoxia and energy metabolism. Trends Endocrinol. Metab. 26, 502–508 (2015).
Koehler, J. et al. Differential expression of miRNAs in hypoxia (“hypoxamirs”) in three canine high-grade glioma cell lines. Front. Vet. Sci. 7, 104 (2020).
Caballero-Garrido, E. et al. In vivo inhibition of mir-155 promotes recovery after experimental mouse stroke. J. Neurosci. 35, 12446–12464 (2015).
Cuomo, O. et al. Anti-mir-223-5p ameliorates ischemic damage and improves neurological function by preventing Nckx2 downregulation after ischemia in rats. Mol. Ther. Nucleic Acids 18, 1063–1071 (2019).
Liu, F. J. et al. Mir-335 regulates Hif-1α to reduce cell death in both mouse cell line and rat ischemic models. PLoS ONE 10, e0128432 (2015).
Kumar, P. et al. Transvascular delivery of small interfering RNA to the central nervous system. Nature 448, 39–43 (2007).
Looney, A. M. et al. Downregulation of umbilical cord blood levels of mir-374a in neonatal hypoxic ischemic encephalopathy. J. Pediatr. 167, 269.e2–273.e2 (2015).
Casey, S. et al. Temporally altered miRNA expression in a piglet model of hypoxic ischemic brain injury. Mol. Neurobiol. 57, 4322–4344 (2020).
Winkler, I. et al. MicroRNA expression profiles as diagnostic and prognostic biomarkers of perinatal asphyxia and hypoxic-ischaemic encephalopathy. Neonatology 119, 204–213 (2022).
Wang, W. & Jia, L. Regulatory mechanism of microRNA-30b on neonatal hypoxic-ischemic encephalopathy (HIE). J. Stroke Cerebrovasc. Dis. 30, 105553 (2021).
O’Sullivan, M. P. et al. Validation of altered umbilical cord blood microRNA expression in neonatal hypoxic-ischemic encephalopathy. JAMA Neurol. 76, 333–341 (2019).
Wang, Z., Liu, Y., Shao, M., Wang, D. & Zhang, Y. Combined prediction of mir‐210 and mir‐374a for severity and prognosis of hypoxic–ischemic encephalopathy. Brain Behav. 8, e00835 (2018).
Midan, D. A. R. et al. Cord blood microRNA-376c and microRNA-1268a as biomarkers for neonatal hypoxic-ischaemic encephalopathy: a diagnostic accuracy study. BMJ Paediatr. Open 5, e001258 (2021).
Looney, A., Ahearne, C., Hallberg, B., Boylan, G. & Murray, D. Downstream mRNA target analysis in neonatal hypoxic-ischaemic encephalopathy identifies novel marker of severe injury: a proof of concept paper. Mol. Neurobiol. 54, 8420–8428 (2017).
Zhang, H., Zhou, J., Zhang, M., Yi, Y. & He, B. Upregulation of mir-376c-3p alleviates oxygen-glucose deprivation-induced cell injury by targeting Ing5. Cell Mol. Biol. Lett. 24, 67–67 (2019).
Looney, A. et al. Altered expression of umbilical cord blood levels of mir-181b and its downstream target Much-L1 in infants with moderate and severe neonatal hypoxic-ischaemic encephalopathy. Mol. Neurobiol. 56, 3657–3663 (2019).
Vonkova, B., Blahakova, I., Hruban, L., Janku, P. & Pospisilova, S. MicroRNA-210 expression during childbirth and postpartum as a potential biomarker of acute fetal hypoxia. Biomed. Pap. 163, 259–264 (2019).
Garberg, H. T. et al. Temporal profile of circulating microRNAs after global hypoxia-ischemia in newborn piglets. Neonatology 111, 133–139 (2017).
Hassell, K. J., Ezzati, M., Alonso-Alconada, D., Hausenloy, D. J. & Robertson, N. J. New horizons for newborn brain protection: enhancing endogenous neuroprotection. Arch. Dis. Child. Fetal Neonatal Ed. 100, F541–F552 (2015).
Volpe, J. J. et al. Volpe’s Neurology of the Newborn E-Book (Elsevier Health Sciences, 2017).
Peeples, E. S., Sahar, N. E., Snyder, W. & Mirnics, K. Temporal brain microRNA expression changes in a mouse model of neonatal hypoxic-ischemic injury. Pediatr. Res. 91, 92–100 (2022).
Meng, Q., Yang, P. & Lu, Y. MicroRNA-410 serves as a candidate biomarker in hypoxic-ischemic encephalopathy newborns and provides neuroprotection in oxygen-glucose deprivation-injured Pc12 and Sh-Sy5y cells. Brain Behav. 11, e2293 (2021).
Han, J. et al. Extracellular vesicle-derived microRNA-410 from mesenchymal stem cells protects against neonatal hypoxia-ischemia brain damage through an Hdac1-dependent Egr2/Bcl2 axis. Front. Cell Dev. Biol. 8, 579236 (2021).
Chen, H.-j & Yang, T.-t Expression and significance of serum miRNA-21 control Hif-1α in newborn with asphyxia. Chin. J. Child Health Care 23, 32 (2015).
Ponnusamy, V. et al. A study of microRNAs from dried blood spots in newborns after perinatal asphyxia: a simple and feasible biosampling method. Pediatr. Res. 79, 799–805 (2016).
Li, B., Dasgupta, C., Huang, L., Meng, X. & Zhang, L. MiRNA-210 induces microglial activation and regulates microglia-mediated neuroinflammation in neonatal hypoxic-ischemic encephalopathy. Cell. Mol. Immunol. 17, 976–991 (2019).
Qiu, J. et al. Neuroprotective effects of microRNA-210 on hypoxic-ischemic encephalopathy. Biomed. Res. Int. 2013, 350419 (2013).
Xiao, P., Jin, Y., Miao-Xia, H., Yu-Dong, P. & Yan-Shan, X. miR-210 is up-regulated in the peripheral blood of asphyxiated neonates. Iran. J. Pediatr. 29, e92652 (2019).
O’Sullivan, M. P. et al. Validation of altered umbilical cord blood microRNA expression in neonatal hypoxic-ischemic encephalopathy. JAMA Neurol. 76, 333–341 (2019).
Yuan, Y. et al. MicroRNA expression changes in the hippocampi of rats subjected to global ischemia. J. Clin. Neurosci. 17, 774–778 (2010).
Zhu, J. et al. Circulating miR-181a as a potential novel biomarker for diagnosis of acute myocardial infarction. Cell. Physiol. Biochem. 40, 1591–1602 (2016).
Griffiths, B. B. et al. Abstract Wmp76: sexually dimorphic response to stroke of miR-181a and miR-200c in aged mice. Stroke 50, AWMP76 (2019).
Michniewicz, B. et al. Biomarkers in newborns with hypoxic-ischemic encephalopathy treated with therapeutic hypothermia. Childs Nerv. Syst. 36, 2981–2988 (2020).
Xu, P., Ma, Y., Wu, H. & Wang, Y.-L. Placenta-derived microRNAs in the pathophysiology of human pregnancy. Front. Cell Dev. Biol. 9, 540 (2021).
Reliszko, Z., Gajewski, Z. & Kaczmarek, M. Signs of embryo-maternal communication: miRNAs in the maternal serum of pregnant pigs. Reproduction 154, 217–228 (2017).
Ma, Q., Dasgupta, C., Shen, G., Li, Y. & Zhang, L. MicroRNA-210 downregulates Tet2 and contributes to inflammatory response in neonatal hypoxic-ischemic brain injury. J. Neuroinflammation 18, 6 (2021).
Ma, Q., Dasgupta, C., Li, Y., Huang, L. & Zhang, L. MicroRNA-210 downregulates ISCU and induces mitochondrial dysfunction and neuronal death in neonatal hypoxic-ischemic brain injury. Mol. Neurobiol. 56, 5608–5625 (2019).
Ma, Q., Dasgupta, C., Li, Y., Huang, L. & Zhang, L. MicroRNA-210 suppresses junction proteins and disrupts blood-brain barrier integrity in neonatal rat hypoxic-ischemic brain injury. Int. J. Mol. Sci. 18, 1356 (2017).
Wang, X. et al. Role of miR-326 in neonatal hypoxic-ischemic brain damage pathogenesis through targeting of the Δ-opioid receptor. Mol. Brain 13, 1–13 (2020).
Chen, W. B., Zhang, L. X., Zhao, Y. K., Li, J. & Jiao, Y. C/Ebpα-mediated transcriptional activation of miR-134-5p entails Kpna3 inhibition and modulates focal hypoxic-ischemic brain damage in neonatal rats. Brain Res. Bull. 164, 350–360 (2020).
Xu, L.-J., Ouyang, Y.-B., Xiong, X., Stary, C. M. & Giffard, R. G. Post-stroke treatment with miR-181 antagomir reduces injury and improves long-term behavioral recovery in mice after focal cerebral ischemia. Exp. Neurol. 264, 1–7 (2015).
Xiong, L. L. et al. Vi4-miR-185-5p-Igfbp3 network protects the brain from neonatal hypoxic ischemic injury via promoting neuron survival and suppressing the cell apoptosis. Front. Cell Dev. Biol. 8, 529544 (2020).
Chen, R. et al. MicroRNA‑204 may participate in the pathogenesis of hypoxic‑ischemic encephalopathy through targeting KLLN. Exp. Ther. Med. 18, 3299–3306 (2019).
Xiong, L. et al. Overexpression of miR-124 protects against neurological dysfunction induced by neonatal hypoxic–ischemic brain injury. Cell. Mol. Neurobiol. 40, 737–750 (2020).
Shi, H., Xu, Y. & Cai, W. Protective role of microRNA-454-3p in neonatal hypoxic-ischaemic encephalopathy by targeting St18. Biotechnol. Biotechnological Equip. 34, 211–220 (2020).
Coenen-Stass, A. M. L. et al. Extracellular microRNAs exhibit sequence-dependent stability and cellular release kinetics. RNA Biol. 16, 696–706 (2019).
Mai, H. et al. Intranasal administration of miR-146a agomir rescued the pathological process and cognitive impairment in an AD mouse model. Mol. Ther. Nucleic Acids 18, 681–695 (2019).
Hanson, L. R. & Frey, W. H. 2nd Intranasal delivery bypasses the blood-brain barrier to target therapeutic agents to the central nervous system and treat neurodegenerative disease. BMC Neurosci. 9, S5–S5 (2008).
Tao, H. et al. Intranasal delivery of miR-146a mimics delayed seizure onset in the lithium-pilocarpine mouse model. Mediators Inflamm. 2017, 6512620 (2017).
Bokobza, C. et al. miR-146b protects the perinatal brain against microglia-induced hypomyelination. Ann. Neurol. 91, 48–65 (2022).
Maas, S. L. N., Breakefield, X. O. & Weaver, A. M. Extracellular vesicles: unique intercellular delivery vehicles. Trends Cell Biol. 27, 172–188 (2017).
Zaborowski, M. P., Balaj, L., Breakefield, X. O. & Lai, C. P. Extracellular vesicles: composition, biological relevance, and methods of study. Bioscience 65, 783–797 (2015).
Doeppner, T. R. et al. Extracellular vesicles improve post-stroke neuroregeneration and prevent postischemic immunosuppression. Stem Cells Transl. Med. 4, 1131–1143 (2015).
Yang, J., Zhang, X., Chen, X., Wang, L. & Yang, G. Exosome mediated delivery of miR-124 promotes neurogenesis after ischemia. Mol. Ther. Nucleic Acids 7, 278–287 (2017).
Xin, H. et al. MicroRNA cluster miR-17-92 cluster in exosomes enhance neuroplasticity and functional recovery after stroke in rats. Stroke 48, 747–753 (2017).
Volpe, J. J. Commentary - Exosomes: realization of the great therapeutic potential of stem cells. J. Neonatal Perinat. Med. 13, 287–291 (2020).
Nguyen, N. P. et al. Brain tissue-derived extracellular vesicle mediated therapy in the neonatal ischemic brain. Int. J. Mol. Sci. 23, 620 (2022).
Shu, J. et al. Human bone marrow mesenchymal stem cells-derived exosomes protect against nerve injury via regulating immune microenvironment in neonatal hypoxic-ischemic brain damage model. Immunobiology 227, 152178 (2022).
Lawson, A., Snyder, W. & Peeples, E. S. Intranasal administration of extracellular vesicles mitigates apoptosis in a mouse model of neonatal hypoxic-ischemic brain injury. Neonatology 119, 345–353 (2022).
Du, L., Jiang, Y. & Sun, Y. Astrocyte-derived exosomes carry microRNA-17-5p to protect neonatal rats from hypoxic-ischemic brain damage via inhibiting BNIP-2 expression. Neurotoxicology 83, 28–39 (2021).
Saeedi, S. et al. Neuron-derived extracellular vesicles enriched from plasma show altered size and miRNA cargo as a function of antidepressant drug response. Mol. Psychiatry 26, 7417–7424 (2021).
Chan, Y. C., Banerjee, J., Choi, S. Y. & Sen, C. K. MiR‐210: the master hypoxamir. Microcirculation 19, 215–223 (2012).
Bavelloni, A. et al. MiRNA-210: a current overview. Anticancer Res. 37, 6511–6521 (2017).
Zhang, L., Liu, X. L., Yuan, Z., Cui, J. & Zhang, H. MiR-99a suppressed cell proliferation and invasion by directly targeting Hoxa1 through regulation of the Akt/Mtor signaling pathway and EMT in ovarian cancer. Eur. Rev. Med. Pharmacol. Sci. 23, 4663–4672 (2019).
Ning, Z.-Q. et al. MicroRNA-30e reduces cell growth and enhances drug sensitivity to gefitinib in lung carcinoma. Oncotarget 8, 4572–4581 (2017).
Men, L., Nie, D. & Nie, H. MicroRNA‑577 inhibits cell proliferation and invasion in non‑small cell lung cancer by directly targeting homeobox A1. Mol. Med. Rep. 19, 1875–1882 (2019).
Ma, Y. et al. MiR-10a-5p promotes chondrocyte apoptosis in osteoarthritis by targeting Hoxa1. Mol. Ther. Nucleic Acids 14, 398–409 (2019).
Zhang, Y., Pan, Q. & Shao, Z. Tumor-suppressive role of microRNA-202-3p in hepatocellular carcinoma through the Kdm3a/Hoxa1/Meis3 pathway. Front. Cell Dev. Biol. 8, 556004 (2021).
Mao, Y., Zhang, L. & Li, Y. Circeif4g2 modulates the malignant features of cervical cancer via the miR‑218/Hoxa1 pathway. Mol. Med. Rep. 19, 3714–3722 (2019).
Fang, H. et al. Microrna-128 Enhances Neuroprotective Effects of Dexmedetomidine on Neonatal Mice with Hypoxic-Ischemic Brain Damage by Targeting Wnt1. Biomedicine & Pharmacotherapy 113, 108671 (2019).
Niu, X. et al. Mir-17-5p Protects Neonatal Mice from Hypoxic-Ischemic Brain Damage by Targeting Casp2. Neurosci. Lett. 772, 136475 (2022).
Xin, D. Q. et al. The Delivery of Mir-21a-5p by Extracellular Vesicles Induces Microglial Polarization Via the Stat3 Pathway Following Hypoxia-Ischemia in Neonatal Mice. Neural Regen. Res. 17, 2238–2246 (2022).
Acknowledgements
The author would like to thank Matthew Sandbulte, PhD, of the Child Health Research Institute for manuscript review and editing assistance.
Funding
This research was supported by the University of Nebraska Medical Center and Children’s Hospital & Medical Center Pediatric Research Grant.
Author information
Authors and Affiliations
Contributions
E.S.P. participated in the conception and design, interpretation of data, and drafting and critical revision of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The author declares no competing interests.
Ethics approval and consent to participate
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Peeples, E.S. MicroRNA therapeutic targets in neonatal hypoxic–ischemic brain injury: a narrative review. Pediatr Res 93, 780–788 (2023). https://doi.org/10.1038/s41390-022-02196-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02196-4
This article is cited by
-
LncRNA-mir3471-limd1 regulatory network plays critical roles in HIBD
Experimental Brain Research (2024)