Abstract
Background
Anemia is a nearly universal diagnosis in preterm infants, caused by phlebotomy, and exacerbated by the underlying erythropoietic immaturity. Newborn infants are exposed to the unique stressor of fetal-to-neonatal transition, which requires significant adaptation ex utero. Accordingly, the preterm infant’s response to anemia may alter the ability to confront underlying illness. This study utilized our preclinical mouse model of phlebotomy-induced anemia (PIA) to comprehensively investigate associated hematological changes.
Methods
C57BL/6 mice were subjected to timed phlebotomy between postnatal days 2–-10 to induce severe anemia. Complete blood counts were determined by the Sysmex XT-2000iV analyzer.
Results
Anemic pups showed a gradual reduction of RBC and hemoglobin (Hb) and increased reticulocyte (RET) counts and red cell distribution width (RDW), however, with reduced RET-Hb from postnatal day (P) of 4 onwards. Elevated levels of high fluorescent RET and immature reticulocyte fraction (IRF) were noted in anemic mouse pups, but low and medium fluorescent RET were reduced. Also, the reduction of mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), and mean corpuscular hemoglobin concentration (MCHC) were noted in anemic pups. No changes were seen in lymphocytes, but monocytes and neutrophils were significantly elevated from P4-P6.
Conclusions
PIA in mouse pups is associated with hematological changes that may be exacerbating factors in neonatal diseases.
Impact
-
Anemia is common and often severe in premature infants.
-
Investigation of hematological parameters in settings of preclinical anemia may be an index of therapeutic strategies.
-
Preclinical model evaluating the effects of neonatal anemia on the remainder of complete blood count.
-
Detailed time kinetic phlebotomy-induced anemic mice enable us to study the impact on developmental delays in erythropoiesis and possible strategic intervention.
-
Hematological effects of severe anemia in mice might provide insight on how best to investigate anemia in preterm infants.
Similar content being viewed by others
Introduction
Anemia is a nearly universal diagnosis in preterm infants and is associated with increased morbidity and mortality worldwide.1,2,3,4,5,6,7,8 The severity of anemia often correlates with the acuity of illness, as it is caused primarily by phlebotomy essential for intensive care. Each instance of phlebotomy leads to acute blood loss, requiring adaptations that preterm infants are not mature enough to achieve.1 Low erythropoietin levels,9,10,11 low iron stores,12,13 and inadequacy of the developing bone marrow1,14 are some examples. Additionally, infants of all gestational ages experience suppression of hematopoiesis soon after birth, owing to high postnatal oxygen tension in the ambient air relative to the in utero environment.15 The overall result is that preterm infants can experience severe iatrogenic anemia without the intrinsic ability to recover.16,17,18 Red blood cell (RBC) transfusion is, therefore, a common occurrence, though it is laden with risks of its own.
Blood is a dynamic fluid predominantly composed of RBCs and plasma, with smaller proportions of white blood cells (WBCs) and platelets. Typically developing infants at term gestation are born with hematocrits nearing 60% or more, which in older children and adults would be considered polycythemia. Preterm infants often have hematocrits in the 40–50% range at birth, either due to birth prior to further RBC genesis or in some cases, due to the circumstances that led to preterm delivery.19,20,21 The primary function of RBCs is the transport of oxygen and carbon dioxide; however, carbon dioxide diffusion occurs 20× faster than oxygen and does not require as robust of a hematocrit to be expelled from the bloodstream into the lungs.22 Therefore, traditionally, the primary physiologic focus in anemic babies is hypoxemia and organ hypoxia. This study hopes to investigate further, particularly the effects of anemia on leukocytes. Leukocytes are the effector cells necessary to combat neonatal sepsis and other inflammatory diseases commonly found in preterm infants,23 and may experience alterations by phlebotomy.
In this investigation, we define the hematological changes in mouse pups due to phlebotomy-induced anemia (PIA) and the findings may help in understanding their importance in anemia-associated co-morbidities during the neonatal period.
Methods
Animals
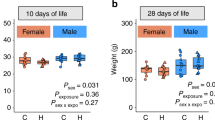
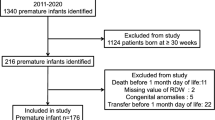
Animal studies were approved by the Institutional Animal Care and Use Committee and complied with the National Institute of Health guide for the care and use of laboratory animals. As previously described,3,24,25 PIA was generated using C57BL/6 mice of both sexes (n = 25) by subjected to facial vein phlebotomy to remove 20 µL blood per gram body weight on days P2, 4, 6, 8, and 10, and an equivalent amount of normal saline was administered subcutaneously. In all, 20 µL of blood samples were collected using ethylenediaminetetraacetic acid-rinsed pipette tip and diluted immediately in 80 µL of CellPak (Sysmex America, Lincolnshire, IL, USA). A total of 100 µL diluted blood samples were analyzed using the XT-2000iV veterinary hematology analyzer (Sysmex, Kobe, Japan) to record a full standard hematology profile. Control animal data were collected from 25 mice from multiple litters, as each mouse could only be sampled once. In all, 20 µL was collected as previously described, at one time point between P2 and P10.
Statistical methods
Statistical analysis was performed using the GraphPad Prism software, version 9.0.0 (GraphPad Software, La Jolla, CA). In detail, the values for RBC, hemoglobin, reticulocyte, Ret-Hb, mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), mean corpuscular hemoglobin concentration (MCHC), red cell distribution width (RDW), WBC, monocyte, neutrophil, and lymphocytes were statistically analyzed using a two-way analysis of variance with Šídák’s multiple-comparisons test. The values of immature reticulocyte fraction (IRF), Ret-LFR, Ret-MFR, and Ret-HFR were analyzed using Student’s t test with Mann–Whitney test. Differences were considered significant at *p < 0.05, *p < 0.01, ***p < 0.001, and ns = not significant. For comparative analysis, age-wise PIA group experiments were compared to their same-age control groups.
Results
PIA is associated with loss of RBCs and their hemoglobin
Serial timed phlebotomy (20% vol/body weight in grams) in neonatal mice resulted in a significant reduction in RBC count (×106/μL) as well as their hemoglobin (g/dL). In control mice (n = 25), the number of RBCs increased over the neonatal period from P2 (3.624 ± 0.12 SD) to P10 (4.728 ± 0.08 SD) and PIA mouse pups (n = 25) showed reduction of RBCs from P6 onwards (2.838 ± 0.05 SD), with an approximately 50% reduction at P10 (2.387 ± 0.07 SD; p < 0.001) (Fig. 1a). Corroborating this loss of RBCs, the hemoglobin content declined from P6 (6.260 ± 0.10 SD) onwards, reaching 50% reduction at P10 (3.540 ± 0.08 SD; p < 0.001) (Fig. 1b).
Neonatal anemia in mice alters reticulocyte properties
PIA pups showed significant elevation of reticulocyte percentage from P6 (3.441 ± 0.10 SD vs. control; p < 0.001) to P10 (3.599 ± 0.10 SD vs. control; p < 0.001; n = 25 per each group) (Fig. 2a). But the hemoglobin in reticulocytes (pg) gradually dropped over the period of mouse pup development (P2; 27.67 ± 0.30 to P10; 15.94 ± 0.09; n = 25 per each group), and phlebotomy exacerbated the loss of hemoglobin in reticulocytes (pg) from P4 (20.98 ± 0.20 SD) to P10 (13.32 ± 0.15 SD) (Fig. 2b). The increased reticulocyte count in P10 anemic mice suggested a likely higher IRF (%), which was confirmed (69.03 ± 0.52 SD vs. control 65.05 ± 0.77 SD; p < 0.05; n = 10 per each group) (Fig. 2c). These findings were corroborated by reticulocyte fluorescence, a marker inversely correlated with maturity, demonstrating that P10 anemic mouse pups (n = 10 per each group) showed increased percentage (%) of high-fluorescence immature or young reticulocytes (51.80 ± 0.70 SD vs. control 46.0 ± 0.72 SD; p < 0.001) compared to low (older) (30.70 ± 0.44 SD vs. control 34.95 ± 0.77 SD; p < 0.001) and medium-fluorescence reticulocytes (maturing) (18.30 ± 0.24 SD vs. control 19.05 ± 0.23; p < 0.05) (Fig. 2d).
Box whisker plots show the measurements of reticulocyte counts [%] (a) and reticulocyte hemoglobin [pg] (b) in C57BL/6 pups during each phlebotomy (P2, P4, P6, P8, and P10) with PIA-groups and non-phlebotomized control groups. Data represent 25 mice/each group; Šídák’s multiple comparisons test; ***P < 0.001 vs. respective age control. c Box whisker plot shows the concentrations of immature reticulocyte fraction [%] in P10 of control vs. PIA; data represent 10 mice/each group; Mann–Whitney U-test; **P < 0.01 vs. control. d Box whisker plots show the level of reticulocyte’s fluorescence [%] in P10 of control and PIA groups; (left) low-fluorescence, (middle) medium-fluorescence and (right) high-fluorescence; data represent 10 mice/each group; Mann–Whitney U-test; *P < 0.05, **P < 0.01, ***P < 0.001 vs. control.
RBC morphology in phlebotomy-induced anemia
We further investigate the RBC morphology in PIA pups by analyzing RBC indices. PIA exacerbated the normal reduction of anemic red cell indices, including MCV, MCH, and MCHC. PIA pups showed a significantly decreased MCV (fL) on P8 (68.07 ± 1.12 SD vs. control 76.89 ± 0.38 SD; p < 0.001; n = 25 per each group) (Fig. 3a), and MCH (pg) was found to be significantly reduced from P6 (22.16 ± 0.40 SD vs. 24.58 ± 0.41 control; p < 0.05) to P10 (14.67 ± 0.37 SD vs. 17.71 ± 0.41 control; p < 0.001; n = 25 per each group) (Fig. 3b). MCHC (g/dL) was slightly decreased from P6, then dropped down further at P10 (26.54 ± 0.41 SD vs. 29.40 ± 0.36 control; p < 0.001; n = 25 per each group) (Fig. 3c). The red cell distribution width (%) significantly increased at P8 (20.0 ± 0.31 SD vs. control 16.21 ± 0.28 SD; p < 0.001) and P10 (22.53 ± 0.45 vs. control 18.70 ± 0.33 SD; p < 0.001; n = 25 per each group) (Fig. 3d).
Representative box whisker plots show the measurement of RBC indices including mean corpuscular volume [fL] a, mean corpuscular hemoglobin [pg] b, mean corpuscular hemoglobin concentration [g/dL] c, and red cell distribution width [%] d in serial time points of both the non-phlebotomized control and phlebotomized anemic groups. N = 25 mice per group. Šídák’s multiple comparisons test, *P < 0.05, ***P < 0.001.
WBC response in phlebotomy-induced anemia
Compared to their age-specific control mice, P4 and P6 anemic mouse pups (n = 20 per each group) showed relatively high WBC counts (×103/μL) (P4; 4.47 ± 0.17 vs. control 2.71 ± 0.06 SD; p < 0.001 and P6; 4.78 ± 0.18 vs. control 3.68 ± 0.16 SD; p < 0.001), which then dropped below P10 (3.58 ± 0.12 vs. control 4.95 ± 0.13 SD; p < 0.001; n = 20) (Fig. 4a). Monocytes (%) were the primary contributor to the increase in total WBC (P4; 26.55 ± 1.30 vs. control 20.40 ± 1.59 SD; p < 0.05 and P6; 31.91 ± 1.38 vs. control 24.30 ± 1.38 SD; p < 0.001; n = 20 per each group) (Fig. 4b) though neutrophils (%) also had a significant rise at P4 (26.20 ± 2.22 vs. control 19.45 ± 1.06 SD; p < 0.05; n = 20 per each group) (Fig. 4c). Both monocytes and neutrophils significantly dropped after P6. No significant lymphocyte (%) changes were noted between the two groups (n = 25 per each group) (Fig. 4d).
Box whisker plots shows the count of WBC [×103/μL] (a), monocytes [%] (b), neutrophil [%] (c), and lymphocytes [%] (d) in C57BL/6 pups during each phlebotomy (P2, P4, P6, P8, and P10) with the PIA groups and non-phlebotomized control groups. Data represent 20 mice/each group; Šídák’s multiple comparisons test; *P < 0.05, **P < 0.01, ***P < 0.001 vs. respective age control.
Discussion
In this study, we present a detailed investigation of the hematological effects of PIA in pre-weaned mice. We observed that serial-timed phlebotomy in neonatal mice caused abnormalities in RBC content and their hemoglobin, reticulocyte properties, RBC morphology, and immune cell responses. These observations are similar to human findings, which have already established the ubiquitous nature of anemia in preterm infants and also provide additional evidence of anemia’s contribution to common co-morbidities. For example, we have previously described3 the increase in gut mucosal permeability resulting from PIA, due to hypoxia-mediated upregulation of microRNA let-7e-5p and evidenced by decreased levels of E-cadherin, an adherens junction protein.
Anemic pups with declining hematocrits expectedly showed a gradual reduction in RBC count during the period of study, reaching a reduction of 50% at P10. This is in contrast to control pups, in whom RBC count increased over the course of development (consistent with the findings of White et al.26). In anemic pups, hemoglobin counts initially dropped at P4 and then steadily maintained until P10. Reticulocytes are erythrocyte precursors whose count represents erythropoietic activity, a clue to distinguishing anemia caused by rapid destruction or loss from anemia caused by bone marrow suppression.27 Significantly higher reticulocyte counts were observed in our phlebotomy-induced anemic mouse pups after P5, indicating that phlebotomy does indeed stimulate bone marrow reticulocyte production. This finding mirrors the fact that corrected reticulocyte counts are higher in preterm human infants with blood loss and/or anemia of prematurity.28,29 However, the reticulocyte hemoglobin content is significantly reduced after P6, which is consistent with the loss of hemoglobin in PIA groups. Reticulocyte hemoglobin content is the strongest independent predictor of iron deficiency anemia, and though the level usually decreases after birth,30 phlebotomy exacerbates the rate of Ret-Hb decline. The higher reticulocyte count in anemic mouse pups represents brisk erythropoiesis, confirmed by a higher IRF in anemic pups. This was seen microscopically as the presence of increased “young immature reticulocytes” with high fluorescence.31 However, a significant reduction of reticulocyte low and medium fluorescence in PIA groups indicated a substantial loss of mature and/or old reticulocytes. This finding is additional evidence of a sudden erythropoietic response in response to blood loss.
Red cell morphology can assist in differentiating among various etiologies of anemia; as erythrocytes affected by blood loss, marrow failure, and hemolysis will likely appear differently under the microscope. MCV is a useful RBC parameter, characterizing anemia as microcytic, normocytic, or macrocytic, which may give clues to the underlying diagnosis.32 Anemic mouse pups showed significantly lowered MCV only on P8 compared to respective age controls, indicating that microcytic anemia develops after 3 timed phlebotomies and causes no changes at P10. However, the lower MCH on P8 and P10 in anemic mouse pups might be due to decreased hemoglobin at P6 onwards. In addition, the MCHC is slightly lower on P6 and P10, indicating that these anemic RBCs are hypochromic. Increased RDW in anemic mouse pups confirms the ineffective erythropoiesis in the bone marrow during phlebotomy, causing anisocytosis where RBCs are unequal in size. The RBC indices from PIA groups are similar to indices found in human infant populations.27
Our investigation of WBCs counts is based on the fact that some types of human anemia may affect the production of WBC precursors.33 In our PIA model, the WBC counts were relatively stable and slightly increased over the period of development in control mice groups; whereas anemic mouse pups showed a sudden increase of total WBC on P4 and continued slightly on P6, but dropped down at P10. The initial increase of WBC after the first phlebotomy might be a stress response to the sudden reduction in oxygen-carrying capacity and is unlikely to be attributed to infection. Since P4 is the day of the second blood draw, its results reflect any changes that took place between the first and second phlebotomies. Our previous findings25 confirmed that serial phlebotomy in mouse pups did not show an increased plasma endotoxin level until after P8 (i.e., measured at the time of the fourth phlebotomy), indicating that any rise in white count that occurs prior to P8 should be attributed to a separate phenomenon. Monocytes and neutrophils were slightly increased in response to phlebotomy and down trended close to control groups; these low counts in blood support our existing findings25 that circulating monocytes are likely recruited from blood to anemic organs, notably the hypoxic intestine. However, no changes occurred in lymphocytes, providing evidence that phlebotomy does not induce any T or B cell response.
In conclusion, this study has shown that phlebotomy-induced neonatal anemia can alter hematological parameters in mice. Our findings will lay the foundation for further preclinical investigation of the role that anemia plays in the development of neonatal co-morbidities.
References
Cibulskis, C. C., Maheshwari, A., Rao, R. & Mathur, A. M. Anemia of prematurity: how low is too low? J. Perinatol. 41, 1244–1257 (2021).
Maheshwari, A., Patel, R. M. & Christensen, R. D. Anemia, red blood cell transfusions, and necrotizing enterocolitis. Semin. Pediatr. Surg. 27, 47–51 (2018).
MohanKumar, K. et al. Severe neonatal anemia increases intestinal permeability by disrupting epithelial adherens junctions. Am. J. Physiol. Gastrointest. Liver Physiol. 318, G705–G716 (2020).
Stockman, J. A. 3rd The anemia of prematurity and the decision when to transfuse. Adv. Pediatr. 30, 191–219 (1983).
Stockman, J. A. 3rd Anemia of prematurity. Current concepts in the issue of when to transfuse. Pediatr. Clin. North Am. 33, 111–128 (1986).
Whitehead, H. V., Vesoulis, Z. A., Maheshwari, A., Rambhia, A. & Mathur, A. M. Progressive anemia of prematurity is associated with a critical increase in cerebral oxygen extraction. Early Hum. Dev. 140, 104891 (2019).
Whitehead, H. V., Vesoulis, Z. A., Maheshwari, A., Rao, R. & Mathur, A. M. Anemia of prematurity and cerebral near-infrared spectroscopy: should transfusion thresholds in preterm infants be revised? J. Perinatol. 38, 1022–1029 (2018).
Widness, J. A. Pathophysiology of anemia during the neonatal period, including anemia of prematurity. Neoreviews 9, e520 (2008).
Kling, P. J. Iron nutrition, erythrocytes, and erythropoietin in the NICU: erythropoietic and neuroprotective effects. Neoreviews 21, e80–e88 (2020).
Ohlsson, A. & Aher, S. M. Early erythropoiesis-stimulating agents in preterm or low birth weight infants. Cochrane Database Syst. Rev. 11, CD004863 (2017).
Ohlsson, A. & Aher, S. M. Early erythropoiesis-stimulating agents in preterm or low birth weight infants. Cochrane Database Syst. Rev. 2, CD004863 (2020).
Moreno-Fernandez, J., Ochoa, J. J., Latunde-Dada, G. O. & Diaz-Castro, J. Iron deficiency and iron homeostasis in low birth weight preterm infants: a systematic review. Nutrients 11, 1090 (2019).
Berglund, S., Westrup, B. & Domellof, M. Iron supplements reduce the risk of iron deficiency anemia in marginally low birth weight infants. Pediatrics 126, e874–e883 (2010).
Stockman, J. A. 3rd et al. Anemia of prematurity: determinants of the erythropoietin response. J. Pediatr. 105, 786–792 (1984).
Finne, P. H. & Halvorsen, S. Regulation of erythropoiesis in the fetus and newborn. Arch. Dis. Child. 47, 683–687 (1972).
Counsilman, C. E. et al. Iatrogenic blood loss in extreme preterm infants due to frequent laboratory tests and procedures. J. Matern. Fetal Neonatal Med. 34, 2660–2665 (2021).
Jakacka, N., Snarski, E. & Mekuria, S. Prevention of iatrogenic anemia in critical and neonatal care. Adv. Clin. Exp. Med. 25, 191–197 (2016).
Rosebraugh, M. R., Widness, J. A., Nalbant, D. & Veng-Pedersen, P. A mathematical modeling approach to quantify the role of phlebotomy losses and need for transfusions in neonatal anemia. Transfusion 53, 1353–1360 (2013).
Christensen, R. D., Henry, E., Jopling, J. & Wiedmeier, S. E. The CBC: reference ranges for neonates. Semin. Perinatol. 33, 3–11 (2009).
Jopling, J., Henry, E., Wiedmeier, S. E. & Christensen, R. D. Reference ranges for hematocrit and blood hemoglobin concentration during the neonatal period: data from a multihospital health care system. Pediatrics 123, E333–E337 (2009).
Kates, E. H. & Kates, J. S. Anemia and polycythemia in the newborn. Pediatr. Rev. 28, 33–34 (2007).
Farhi, L. E., Plewes, J. L. & Olszowka, A. J. Lung carbonate dehydratase (carbonic anhydrase), CO2 stores and CO2 transport. Ciba Found. Symp. 235–249 (1976).
Raymond, S. L. et al. Immunological defects in neonatal sepsis and potential therapeutic approaches. Front. Pediatr. 5, 14 (2017).
Arthur, C. M. et al. Anemia induces gut inflammation and injury in an animal model of preterm infants. Transfusion 59, 1233–1245 (2019).
MohanKumar, K. et al. A murine neonatal model of necrotizing enterocolitis caused by anemia and red blood cell transfusions. Nat. Commun. 10, 3494 (2019).
White, J. R. et al. Evaluation of hematologic variables in newborn C57/Bl6 mice up to day 35. Vet. Clin. Pathol. 45, 87–95 (2016).
Parodi, E., Romano, F. & Ramenghi, U. How we use reticulocyte parameters in workup and management of pediatric hematologic diseases. Front. Pediatr. 8, 588617 (2020).
Juul, S. Erythropoiesis and the approach to anemia in premature infants. J. Matern. Fetal Neonatal Med. 25, 97–99 (2012).
Juul, S. Erythropoietin in anemia of prematurity. J. Matern. Fetal Neonatal Med. 25, 80–84 (2012).
Al-Ghananim, R. T. et al. Reticulocyte hemoglobin content during the first month of life in critically ill very low birth weight neonates differs from term infants, children, and adults. J. Clin. Lab. Anal. 30, 326–334 (2016).
Wollmann, M., Gerzson, B. M., Schwert, V., Figuera, R. W. & Ritzel Gde, O. Reticulocyte maturity indices in iron deficiency anemia. Rev. Bras. Hematol. Hemoter. 36, 25–28 (2014).
Ford, J. Red blood cell morphology. Int. J. Lab. Hematol. 35, 351–357 (2013).
Kline, N. E. A practical approach to the child with anemia. J. Pediatr. Health Care 10, 99–105 (1996).
Acknowledgements
The authors acknowledge Sysmex America, Scientific Marketing Department for the instrument loan (Sysmex XT-2000iV) and technical support.
Funding
This study was supported by the National Institutes of Health awards HL124078, HL133022, and HD105880 (to K.M.)
Author information
Authors and Affiliations
Contributions
K.M. designed the study and wrote the manuscript; Y.C., S.D., K.N., P.G., L.H., and K.M. performed key experiments and data analysis. All the authors contributed to and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chung, Y., Desiraju, S., Namachivayam, K. et al. Hematological changes in neonatal mice with phlebotomy-induced anemia. Pediatr Res 92, 1575–1579 (2022). https://doi.org/10.1038/s41390-022-02023-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02023-w