Abstract
The human brain develops through a complex interplay of genetic and environmental influences. During critical periods of development, experiences shape brain architecture, often with long-lasting effects. If experiences are adverse, the effects may include the risk of mental and physical disease, whereas positive environments may increase the likelihood of healthy outcomes. Understanding how psychosocial stress and adverse experiences are embedded in biological systems and how we can identify markers of risk may lead to discovering new approaches to improve patient care and outcomes. Biomarkers can be used to identify specific intervention targets and at-risk children early when physiological system malleability increases the likelihood of intervention success. However, identifying reliable biomarkers has been challenging, particularly in the perinatal period and the first years of life, including in preterm infants. This review explores the landscape of psychosocial stress and adverse experience biomarkers. We highlight potential benefits and challenges of identifying risk clinically and different sub-signatures of stress, and in their ability to inform targeted interventions. Finally, we propose that the combination of preterm birth and adversity amplifies the risk for abnormal development and calls for a focus on this group of infants within the field of psychosocial stress and adverse experience biomarkers.
Impact
-
Reviews the landscape of biomarkers of psychosocial stress and adverse experiences in the perinatal period and early childhood and highlights the potential benefits and challenges of their clinical utility in identifying risk status in children, and in developing targeted interventions.
-
Explores associations between psychosocial stress and adverse experiences in childhood with prematurity and identifies potential areas of assessment and intervention to improve outcomes in this at-risk group.
Similar content being viewed by others
Introduction
For over 20 years, there has been increasing evidence that basic brain architecture is established early in life through a complex interplay of genetic and environmental influences.1,2 Social experiences shape brain structure and function, particularly during early critical or sensitive periods of development.3,4,5 As a result, experiences encountered from the perinatal period through the first few years can influence development in a manner that persists across the lifespan.6 Positive experiences often affect development positively, whereas adverse experiences may elevate the risk of atypical development, which in turn could have life-long consequences.7,8 Chronic and cumulative exposure to adversity may increase the risk of negative cognitive, psychosocial, behavioral, and physical health outcomes,1,6,9,10,11 and the biological embedding of these experiences might even influence outcomes in future generations.2 Historically, marginalized groups in society have disproportionately high exposure to adversity. When experienced early in life, such exposures might lead to maladaptive changes that can perpetuate disparities over time.9,12,13,14 How experience becomes biologically embedded, in multiple organ systems, and the identification of biomarkers of psychosocial stress and adverse experiences in childhood remains limited—especially for experiences that occur in the perinatal period and the first years of life.6,15 However, valid and reliable biomarkers of psychosocial stress and adverse experiences hold the promise of identifying children at risk of long-term negative outcomes that arise as a result of such experiences early in life, while at the same time illuminating underlying mechanisms. Identifying risk “early” is critical for facilitating effective and specific interventions targeted (a) at the developing systems that are most affected; (b) for the children who are most at risk; and (c) during developmental windows when physiological system malleability increases the likelihood of intervention success.
Despite the growing evidence that psychosocial stress and adverse experiences during childhood have long-term consequences, the definition and dimensions of adversity and adverse experiences remain unresolved.10,16 The number, timing, type, and duration of exposures, as well as individual variation, intrinsic characteristics, and developmental status (e.g., born at term or preterm) may affect perception and responses to psychosocial stress and adverse experiences. These responses may affect the lifetime risk of developmental and overall health outcomes.1,6,10,16,17 For instance, an individual may be exposed to many stressors and adversities in life but not have a “toxic stress response” which is the response to such stressors that cause a chronic activation of the stress response systems and can disrupt brain development and other systems in the absence of adequate adult support.10,16
The Adverse Childhood Experiences (ACE) Study is a landmark study launched in 1995 and the first to describe in a longitudinal cohort the strong and direct association of adversities during childhood, such as physical and sexual abuse, substance abuse in the household, and the increased lifetime risk of disease and leading causes of death in adults.9 Since that integral study, researchers have additionally assessed how not only the number of events experienced, but also the nature and timing of reported events, degree of the physiological stress response may contribute to developmental/health outcomes in different ways.18,19,20 For this review, we have chosen our terminology to extend beyond the ACEs descriptor to explicitly account for the interacting facets of psychosocial stress and adverse experiences that are predicted to elicit a physiological stress response. We included exposures such as physical or mental violence, abuse or neglect, discrimination/racism, and accumulated burden from poverty and economic hardship/ low-socioeconomic status (SES) without adequate social support, that might produce a “toxic stress response”.1,6,21 We noted specific experiences reported in the research, and the age of exposures whenever possible to facilitate differentiation between types and exposure periods.
Compounding pre-existing family stress with adversity of preterm birth
Most of the work on psychosocial stress and adverse experiences early in life has focused on the first years of childhood with less work on the prenatal and perinatal aspect. While prenatal exposures influence infant developmental outcomes (e.g., maternal conditions like diabetes, exposure to toxicants, alcohol, tobacco, and substance abuse) less is known about prenatal and perinatal exposure to psychosocial stress and adverse experiences, particularly in preterm infants. Globally, preterm birth (delivery before 37 weeks of gestation) affects ~11% of births worldwide (~10% in the US).22,23,24 Despite medical advances, preterm birth remains a leading cause of morbidity and mortality in children under 5 years of age.25,26 Many factors have been associated with an increased risk of preterm birth (e.g., smoking, maternal age, multiple births, spacing between pregnancies); however, most preterm births occur without a known risk factor.22 Preterm birth in the US is more common among Black than White birthing people (14.1% versus 9.1%).27 Historically disparities in birth outcomes had been attributed to biological or genetic variation. However, there is now strong evidence that disparities are largely due to the cumulative effects of structural racism leading to socioeconomic disadvantage, environmental toxicant exposure, and psychosocial stress.28,29,30
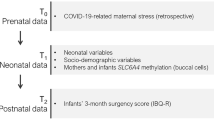
While preterm birth may arise from exposure to psychosocial stress and adverse experiences, it can be a source of stress in its own right. The stress experienced by parents and infants when the earliest days or months are spent in the Neonatal Intensive Care Unit (NICU) warrants exploration as a risk factor for ongoing development (Fig. 1). NICU admission adds levels of psychosocial stress and adverse experiences (e.g., environmental stressors such as alarms, bright lights, lack of consistent access to a caregiver, biological stressors from pain and necessary life-saving procedures, and financial pressures from hospital bills and lost wages to a baseline level of neurological and physiological immaturity). We conceptualize the NICU as a necessary, but adverse exposure, that compounds the high baseline psychosocial stress and adverse experiences that many NICU families already endure.
Dashed lines show factors that may mediate the experience of stress and contribute to a difference in susceptibility to adversity including the care environment, the interaction with the genetic endowment that may influence an individual’s biologic response, and timing of the exposure during critical or sensitive periods of development where adverse exposures may have a more significant effect. NICU neonatal intensive care unit, SES socioeconomic status.
Landscape of biomarkers assessed in the perinatal period and early childhood
Though a full review of adult biomarkers is beyond the scope of the present manuscript, we note that considerable work has reported associations between exposure to adverse childhood experiences and biomarkers in adulthood.9,31,32,33 This body of work provides critical evidence that psychosocial stress and adverse experiences influence physiology in the long term. In our present narrative review, we explore the landscape of biomarkers in early childhood, which have received less attention, and which may differ from biomarker expression observed in adulthood in important ways. With these considerations, the aims of this review are to (a) explore the landscape of biomarkers of psychosocial stress and adverse experiences in the perinatal period and early childhood (up to ~5 years); (b) explore and highlight potential benefits of identifying at-risk infants early, while considering whether different sub-signatures of toxic stress might inform more targeted interventions; (c) discuss forthcoming challenges of using biomarkers in clinical settings with varying resources; (d) discuss concerns regarding how to interpret individual differences and exposures to multiple types of adversity; and (e) propose directions for future research and areas of opportunity, including the proposal that preterm birth acts in tandem with psychosocial stress and early adversity to amplify risk for abnormal development. There is limited research in this last area, but we highlight ways that psychosocial stress and early adversity might interact with preterm birth, indicating a particular need to focus on infants born preterm when identifying stress and adversity biomarkers (Fig. 1).
We define a biomarker as a biological tool that can be quantified, measured, or evaluated to indicate differences in response to psychosocial stress and adverse experiences, and that is expected to be modulated as a result of intervention. Historically, biomarkers may aid in screening, diagnosis, prognosis, or biologic response measurement. An acceptable biomarker needs to be both sensitive in detecting risk and reliable across time, with variability reflecting individual differences in the physiological response to stress.34 Additionally, for clinical use, biomarkers would ideally be affordable and non-invasive (e.g., saliva, urine, skin cells, blood collected for clinical use). For this review, we include all biomarkers that have been associated with psychosocial stress and adverse experiences (as described above), including non-conventional biomarkers of brain function (e.g., those identified using electroencephalography (EEG)).
Psychosocial stress and adverse experiences in childhood can impact multiple systems. Animal and human models demonstrate changes in brain structure and function, chronic inflammation, reduced immunity and autoimmunity (immune dysfunction), premature aging and mortality, and poor health outcomes that arise from chronic and metabolic disease.6,9 We reviewed recent studies from PubMed searching for terms associated with psychosocial stress and adverse experiences and individual biomarker terms. We included recent studies and reviews in humans published in English in children ≤5 years of age (see Supplementary Fig. 1 for search strategy). We present biomarkers in different systems and organs, including 1. Biomarkers of brain structure and function, 2. Biomarkers of neuroendocrine function, and 3. Biomarkers of immune function. Table 1 summarizes the benefits and limitations of each biomarker reviewed.
Biomarkers of brain structure and function
Tools that have been used to assess associations between early psychosocial stress and adverse experiences and neurodevelopment during infancy and early childhood primarily include magnetic resonance imaging (MRI), electroencephalography (EEG), and functional near-infrared spectroscopy (fNIRS).
Magnetic resonance imaging (MRI)
Studies using MRI have revealed critical information about the impact of early exposure to psychosocial stress and adverse experiences on the developing brain. Given that MRI is feasible but challenging to perform without sedation during infancy and early childhood, and that sedation, even if minimal, may present some risks,35 the majority of studies have retrospectively examined how structural and functional changes in adolescence and adulthood are associated with adverse experiences that happened early in life.36,37 A body of work examining associations between psychosocial stress and adverse experiences and neurodevelopment in infancy and early childhood (i.e., from the neonatal period up to 6 years)38 has revealed that prenatal, and early postnatal experiences (e.g., poverty, abuse/neglect, maternal depression, etc.), including preterm birth,39,40 are associated with global reductions in white matter integrity and myelination,41,42 changes to brain volume, cortical thickness,43,44,45 and functional networks,46 as well as structural and functional alterations to brain regions that contribute specifically to the stress response system (i.e., hippocampus, amygdala, prefrontal cortex).47,48,49,50 Effects from maternal prenatal stress exposure are also seen in preterm infants as early as term-equivalent age.51 These neurodevelopmental changes map onto patterns observed later in life.36,37
Electroencephalography (EEG)
EEG is relatively inexpensive and well-tolerated by even very young infants, compared to MRI (described above). Although EEG provides relatively poorer spatial localization compared to MRI and does not allow for structural analyses, EEG does provide a readout of cortical function and can be used to probe network-level disruptions in neural development.52,53 Critically, analyses of both baseline and task-related EEG power, functional connectivity, and event-related potentials (ERPs) have revealed that early adverse experiences are associated with perturbations in the developing EEG that underlie later cognitive, language, and socioemotional outcomes.53,54,55
Several distinct EEG patterns have been observed within baseline and task-based EEG. For example, a pattern of elevated power in low-frequency bands (e.g., delta and theta) alongside concomitantly reduced power in high-frequency bands (e.g., beta and gamma) has been observed in children exposed to psychosocial adversity,56,57 as well as in children from low-SES backgrounds,58,59,60 and those exposed to high levels of maternal stress (both self-reported and physiological, as measured by cortisol).61,62 This pattern may reflect delayed maturation, and associations have been observed between white matter architecture, EEG rhythms,63 and performance on cognitive tasks.59 Low gamma power in particular, especially at frontal electrode locations, has also been associated with low-SES status, poverty, and maternal stress.58,59,61,64,65,66 Critically, (frontal) gamma power from as early as the neonatal period appears to predict performance on language and cognitive measures throughout childhood.59,67,68,69,70 Furthermore, differences in functional neural networks and functional connectivity patterns, particularly cross-gamma and cross-alpha coupling, have been associated with exposure to early psychosocial stressors, suggesting that communication between local and long-distance brain regions may be impacted by certain adverse experiences that occur early in life.71 In the socioemotional domain, a considerable body of work has found associations between patterns of frontal alpha asymmetry (FAA) and both psychosocial stress and adverse experiences72 and maternal depression.73 FAA is thought to be associated with temperamental approach/avoidance behavior in infants and children and is predictive of later development of mood disorders such as depression and anxiety.74,75,76 Features of the EEG have also been associated with preterm birth, and interactions between preterm birth and exposure to psychosocial stress and adverse experiences warrant further investigation.77
There is also evidence that certain ERP components of the EEG provide a readout of neural processing that is influenced by early experience and maps on specific sensory and cognitive domains as well. Adverse experiences in childhood (e.g., stress, poverty, malnutrition) have been associated with perceptual/sensory development and cortical maturation, as reflected by reduced amplitude and increased latency of the visual (VEP) and auditory (AEP) evoked potential components.78,79 Experiences associated with living in a low-SES context (as measured by parental income or education levels), or exposure to maternal psychosocial stress and adverse experiences early in life are also associated with diminished selective attention and attention allocation (particularly in the auditory domain),80,81,82,83,84,85,86,87 and differences in error/reward processing,88,89 executive function,90,91 and emotional processing of faces.92,93,94 Some of these effects are mediated by factors such as maternal sensitivity88 and sympathetic nervous system activation of the child,80 and in some cases, appear to be moderated by differential genetic susceptibility(i.e., 5-HTTLPR polymorphism).81
Functional near-infrared spectroscopy (fNIRS)
The majority of studies reporting associations between early psychosocial stress and childhood adversity with neurodevelopment have used MRI and EEG, yet increasing evidence supports the use of fNIRS as a tool for evaluating early neurodevelopment. While fNIRS has been used as early as the neonatal period to reveal the influence of experience on neurodevelopment,95 some studies deployed in low- and middle-income countries are beginning to see adversity-related perturbations in the fNIRS signal later in life as well. For example, a study in rural India used fNIRS in children (4–48-months) to demonstrate that early adverse experiences were associated with brain network activation underlying visual working memory.96 In a study of children (6 and 36-months) in Bangladesh, maternal education, maternal stress, and caregiving environment were associated with the magnitude of a neural response to social stimuli.97 While the use of fNIRS in this context is in its early days, this tool is relatively affordable and easy to administer in a wide range of contexts, making it a promising emerging tool to understand how early psychosocial stress and adverse experiences shape the developing brain. However, more research is needed before its deployment for clinical purposes.
Biomarkers of neuroendocrine function
Hypothalamus–pituitary–adrenal-axis (HPA)
Dysregulation of the HPA axis in response to early life and chronic stress has been studied and reviewed at length.98,99,100 Under the influence of stress, the HPA axis is activated and releases glucocorticoids, cortisol, and derivatives, into the bloodstream. Glucocorticoids can be measured across development from saliva, hair, nails, and other fluids (e.g., plasma). These samples are relatively easy to collect and, thus, provide promising biomarkers for assessing HPA functioning in pediatric populations. However, the timing of sample collection (e.g., measuring basal levels of cortisol vs. cortisol awakening response) and the timing of stress (e.g., acute stress best captured by saliva vs. chronic stress best captured by hair) must be addressed when interpreting HPA axis biomarkers.101,102
Despite the extensive literature, a recent meta-analysis across 14 vertebrate species, including humans, only supported small-to-moderate effects of maternal distress on offspring glucocorticoid levels.103 This could be explained by various studies yielding seemingly contradictory results, as both hyper- and hypo-activation of the HPA axis have been found in response to early psychosocial stress and adverse experiences.104,105 Hyper-activation of the HPA axis may suggest an acquired resistance to glucocorticoid negative feedback, while hypo-activation may suggest attenuated stress reactivity or an exaggerated suppression of the axis with chronic stress.106,107 Both have been found in response to early psychosocial stress and adverse experiences and predict downstream stress-related chronic illness.108
The effects of early psychosocial stress and adverse experiences on the HPA axis appear to be impacted by the age at which these events were experienced and the sex of the offspring.109,110,111 Some studies suggest an interaction whereby the sex of a fetus moderates maternal cortisol at certain points in pregnancy.112 However, variation in the timing of the stress response, and the stress paradigm used, could explain varying results. Although studies using physical stressors have produced consistent cortisol increases in young infants, studies using psychosocial stressors have produced mixed or null results.113 A recent meta-analysis on psychosocial stress paradigms and cortisol responses in infants <18-months found the normative response to be small, even when controlling for age.114 As such, more research is essential to tease apart methodological noise from differential effects of early psychosocial stress and adverse experiences on the HPA axis.
Biomarkers of immune function
Exposure to early psychosocial stress and adverse experiences has been associated with an increased risk of psychiatric and medical conditions later in life. Alteration of the immune system has been suggested as one of the biological mechanisms mediating this relationship.6,115,116 Chronic exposure to psychosocial stress and adverse experiences leads to chronic low-grade inflammation, which is also aided by the concurrent downregulation of anti-inflammatory pathways such as the HPA axis.14,117,118 The link between early psychosocial stress and adverse experiences and inflammation was initially identified in adults who were exposed to such experiences during childhood and had increased baseline levels of inflammatory markers like C-Reactive Protein (CRP) and pro- and anti-inflammatory cytokines.116,119,120 Maintaining a pro-inflammatory state due to early psychosocial stress and adverse experiences has been additionally associated with metabolic dysfunction later in life, increasing the risk of immunosuppression (linked to increased risk of infections and cancer) as well as chronic and metabolic diseases in adulthood (i.e., cardiovascular risk, diabetes, obesity).6,115,116,121 A meta-analysis of 25 studies showed the associations of childhood trauma with CRP and two pro-inflammatory cytokines (IL-6 and TNF- α) to be small yet significant.116
While most studies have examined associations later in life, a few have examined the association of psychosocial stress and adverse experiences with inflammation in children <5 years (including infants).122 A study determining the association of low-SES, maternal psychosocial stress, depression, and familial stress in infancy showed an association with increased salivary CRP and a composite measurement of pro-inflammatory cytokines (e.g., IL-1β, IL-6, IL-8, and TNF- α) in 17-month-old children.123,124 In Tanzania, a study demonstrated that increased levels of CRP in infants (1–10 months) was associated with lower maternal education and maternal depression.125 Another study, also in Tanzania, found that maternal experiences of intimate partner violence during the previous 12 months were associated with increased CRP levels in children ages 6 months to 5 years of age.126 However, other studies in 3–5-year-old children found no association between psychosocial stress and adverse experiences and CRP.127 Only some variables measured (number of recent and lifetime contextual stressors and traumatic life events) were positively associated with increased salivary interleukin (IL-1β).127
Approaching the question from a different perspective, Riis et al. investigated how psychosocial stress and adverse experiences impact the regulatory mechanisms of inflammation in 5-year-olds and found that maternal distress (measured by depression, anxiety, and parenting stress index) moderates the relationship between cortisol and pro-inflammatory cytokines (IL-1b, IL-6, IL-8, TNF-a).128 As levels of distress increased, the relationship between cortisol and cytokines shifted from negative to positive, supporting the idea that chronic inflammation associated with adverse experiences is also explained by less efficient regulation of anti-inflammatory mechanisms.
A recent meta-analysis of studies of children and adolescents found effect sizes for CRP and IL-6 to be similar in magnitude as those reported in adult studies, but associations were not statistically significant.129 While data suggest that effects are stronger in infancy and adolescence, the authors invite caution when interpreting these findings, given the limited number of available studies and the heterogeneity in methodological approaches.
Projected benefits of recognizing individual differences in risk
Focusing on exposures that occur during critical or sensitive periods prenatally and in early childhood is essential to prevent lasting effects throughout the lifespan.3 The biomarkers reviewed herein may inform our understanding of neurodevelopmental and physiological changes and help predict long-term negative health and developmental outcomes, mainly if measured early and longitudinally. Many of these biomarkers can be collected in an efficient, reliable, and impactful way prenatally, in nurseries or the NICU after birth, in pediatric clinics, and even at home with mobile technology.
In addition to identifying precise mechanisms and individual indicators of risk for adverse outcomes, biomarker analysis can begin to identify different sub-signatures of toxic stress—namely, whether different types of early exposures lead to different types of physiological change in different sub-groups. Identifying markers associated with very specific exposures, or categories of exposures will help develop more specific and targeted interventions for families.16,130 Nonetheless, we recognize that the resolution of disparities will ultimately require large-scale structural changes to reduce exposure to psychosocial stress and adverse experiences among populations facing discrimination and barriers in access to resources and social supports.
Forthcoming challenges and limitations of the use of biomarkers in the clinical setting
It remains unknown whether there are specific periods of development during which exposure to psychosocial stress and adverse experiences is most deleterious, and whether this varies by type of exposure or outcome measured.17 Concomitantly, some conceptual models have suggested that cumulative exposure to multiple adverse experiences over time may influence development more profoundly than acute exposures alone, regardless of their timing.131 Given the difficulty in separating types of adversity, since many occur concurrently, few studies have compared these factors directly to determine each unique influence and their interaction.
We have included a wide range of potentially negative experiences (e.g., accumulated burden from poverty, abuse, neglect, maternal mental health issues, etc.). However, we know that different experiences might impact development in different ways and that not every child exposed to the same experience will have the same response; perception of stressors, support/resources (extrinsic in the case of environmental context, intrinsic in the case of differential genetic susceptibility), and resiliency tools to overcome exposure to these events vary. Thus, it is difficult to interpret individual differences in physiological responses and, in turn, how to “treat” or intervene.
Another key limitation in research to date is that the identification of generalizable biomarkers requires large and diverse samples. Even when able to include diverse samples, there are still vulnerable and isolated groups with additional barriers to research participation, including indigenous populations, undocumented immigrants, refugees, and asylum seekers, that may have experienced different types of psychosocial stressors and extreme adversity.
Once biomarkers have proven to be reliable, feasible, and highly predictive, another factor to consider is that the availability of tools varies across settings. Collection of blood, saliva, or urine samples may be widely implemented across contexts, however in some remote locations ability to run assays on physiological samples might be limited. Neuroimaging tools are becoming more portable and have been used effectively in very low-resource settings; however, restrictions still exist in terms of cost and ease of access for the most vulnerable populations. Moving forward, the combination of tools will be critical to determine how to identify children at risk and uncover underlying mechanisms that lead to long-lasting effects on health and development. Finally, ethical considerations are paramount when incorporating the use of biomarkers to assess risk into clinical practice (e.g., making sure biomarkers are equally available for all and when risks are identified, interventions to improve outcomes must be promptly deployed).132,133,134
Directions for future research and areas of opportunity
Biomarkers of epigenetic change (Accelerated telomere shortening and DNA methylation)
In addition to the biomarkers reviewed, associations between psychosocial stress and adverse experiences, and biological aging has received recent attention, though predominantly in older children and adults. In particular telomeres, or repeating segments of noncoding DNA that serve as protective caps at the ends of chromosomes and help maintain chromosomal integrity,135 have been found to shorten with each cell division contributing to aging and disease in humans.136,137 Accelerated shortening may be due to higher oxidative stress and inflammation affecting telomerase activity.138 Telomeres are easily collected from saliva or blood139,140 and although more research is required to standardize TL assessment, TL is a promising biomarker. In addition to being linked to health, longevity, and chronic diseases, TL has been associated with psychosocial stressors and adverse experiences (e.g., family violence and disruption, discrimination, and racism).141,142,143,144,145 According to a large meta-analysis, telomere heritability could be as high as 70%, contributing to intergenerational transmission of stress exposure.146 Recently, accelerated telomere shortening has been studied in the context of stressors in the perinatal period and early childhood adversity.147,148,149,150,151,152,153 While shorter telomeres have been associated with various psychological and physiological health ailments in adults, further research is required to determine whether TL at birth and/or in infancy can predict TL later in life.
DNA methylation may also be used to obtain as a marker of aging that may explain intergenerational transmission of stress.154 However, most studies have been conducted in adult populations. Recently, multidisciplinary teams have been working on developing accurate and non-invasive methods to assess biological aging by using mathematical models to characterize an “epigenetic clock” that can measure and predict biological age, including in children. In the future, this clock may help to evaluate the impact of psychosocial and environmental factors on child development by revealing how gene expression is modified as a result of psychosocial stress and adverse experiences and, as a result, how these modifications impact health outcomes in the long term.155
Preterm birth and NICU environment as a critical avenue for future research
Considerable research has explored the influence of preterm birth on development156,157 and the exposure to biological stress (i.e., from pain).158 However, little work to date has explored the interaction of familial psychosocial stress and adverse experiences that pre-dated the preterm birth with adversity that resulted from the preterm birth. Together these stressors likely affect developmental and health outcomes159 which may be modified by identifying infants and families “at risk” and targeting tailored early interventions inclusive of parental education, support and follow up programs.160,161 Admission to the NICU offers an opportunity to assess risk, study biomarkers within other studies assessing neurodevelopmental outcomes, and to design interventions to empower families and support infant neurodevelopment.162
Other areas of opportunity
In the future, studies may consider performing economic evaluations to assess the cost of incorporating biomarker screening in the clinical setting and the cost of early interventions for children at risk versus the potential cost of the consequences of toxic stress in adult life (e.g., chronic and metabolic diseases in adulthood). Several questions remain regarding the biological embedding of early experiences with long-term development and the clinical use of biomarkers in the perinatal and early childhood period. More studies are needed—particularly longitudinal studies with larger sample sizes and diverse demographic representation.
References
Shonkoff, J. P. & Garner, A. S. The lifelong effects of early childhood adversity and toxic stress. Pediatrics 129, e232–246 (2012).
Buss, C. et al. Intergenerational transmission of maternal childhood maltreatment exposure: Implications for fetal brain development. J. Am. Acad. Child Adolesc. Psychiatry 2017, 373–382 (2017).
Fox, S. E., Levitt, P. & Nelson, C. A. How the timing and quality of early experiences influence the development of brain architecture. Child Dev. 81, 28–40 (2010).
Nelson, C. A., Zeanah, C. H. & Fox, N. A. How early experience shapes human development: The case of psychosocial deprivation. Neural Plast. 2019, 1676285 (2019).
Hertzman, C. Putting the concept of biological embedding in historical perspective. Proc. Natl. Acad. Sci. USA 109, 17160–17167 (2012).
Berens, A. E., Jensen, S. K. G. & Nelson, C. A. Biological embedding of childhood adversity: From physiological mechanisms to clinical implications. BMC Med. 15, 135 (2017).
Johnson, S. B., Riley, A. W., Granger, D. A. & Riis, J. The science of early life toxic stress for pediatric practice and advocacy. Pediatrics 131, 319 LP–327 (2013).
National Scientific Council on the Developing Child. Excessive stress disrupts the development of brain architecture. J. Child Serv. 9, 143–153 (2014).
Felitti, V. J. et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. Am. J. Prev. Med. 14, 245–258 (1998).
Nelson, C. A. & Gabard-Durnam, L. J. Early adversity and critical periods: neurodevelopmental consequences of violating the expectable environment. Trends Neurosci. 43, 133–143 (2020).
Committee on Psychosocial Aspects of Child and Family Health. The new morbidity revisited: A renewed commitment to the psychosocial aspects of pediatric care. Pediatrics 108, 1227–1230 (2001).
Moog, N. K. et al. Intergenerational effect of maternal exposure to childhood maltreatment on newborn brain anatomy. Biol. Psychiatry 83, 120–127 (2018).
National Scientific Council on the Developing Child. Connecting the Brain to the Rest of the Body: Early Childhood Development and Lifelong Health Are Deeply Intertwined Working Paper No. 15. www.developingchild.harvard.edu (2020).
Danese, A. & McEwen, B. S. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol. Behav. 106, 29–39 (2012).
Nelson, C. A. III The implications of early adversity even before birth. JAMA Netw. Open. 3, e1920030 (2020).
Nelson, C. A. et al. Adversity in childhood is linked to mental and physical health throughout life. BMJ 371, m3048 (2020).
Gabard-Durnam, L. J & McLaughlin, K. A. Do sensitive periods exist for exposure to adversity? Biol Psychiatry 85, 789–791 (2019).
McLaughlin, K. A. & Sheridan, M. A. Beyond Cumulative Risk: A Dimensional Approach to Childhood Adversity. Curr. Dir. Psychol. Sci. 25, 239–245 (2016).
McLaughlin, K. A., Sheridan, M. A., Humphreys, K. L., Belsky, J. & Ellis, B. J. The value of dimensional models of early experience: thinking clearly about concepts and categories Katie. Perspect. Psychol. Sci. 16, 1463–1472 (2020).
Lanier, P., Maguire-Jack, K., Lombardi, B., Frey, J. & Rose, R. Adverse childhood experiences and child health outcomes: comparing cumulative risk and latent class approaches. Matern. Child Health J. 22, 288–297 (2018).
Hertzman, C. & Stefanowicz, A. The significance of early childhood adversity. Paediatr. Child Heal. 18, 127–128 (2013).
Vogel, J. P. et al. The global epidemiology of preterm birth. Best. Pract. Res Clin. Obstet. Gynaecol. 52, 3–12 (2018).
Martin, J. A., Hamilton, B. E., Osterman, M. J. K. & Driscoll, A. K. Births: final data for 2018. Natl Vital Stat. Rep. 68, 1–47 (2019).
Liu, L. et al. Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet 388, 3027–3035 (2016).
Harrison, M. S. & Goldenberg, R. L. Global burden of prematurity. Semin. Fetal Neonatal Med. 21, 74–79 (2016).
World Health Organization. Preterm birth fact sheet. who.int. https://www.who.int/news-room/fact-sheets/detail/preterm-birth (2018).
Martin, J. A., Hamilton, B. E., Osterman, M. J. K. & Driscoll, A. K. Births: final data for 2018. Natl Vital Stat. Rep. 68, 1–46 (2019).
Burris, H. H. et al. Racial disparities in preterm birth in USA: a biosensor of physical and social environmental exposures. Arch. Dis. Child 104, 931–935 (2019).
March of Dimes Perinatal Data Center. 2021 March of Dimes Report Card. https://www.marchofdimes.org/materials/March_of_Dimes_US_2021_Report_Card_11152021.pdf
Geronimus, A. T. The weathering hypothesis and the health of African-American women and infants: evidence and speculations. Ethn. Dis. 2, 207–221 (1992).
Chapman, D. P. et al. Adverse childhood experiences and the risk of depressive disorders in adulthood. J. Affect Disord. 82, 217–225 (2004).
Dong, M. et al. Insights into causal pathways for ischemic heart disease: adverse childhood experiences study. Circulation 110, 1761–1766 (2004).
Brown, D. W. et al. Adverse childhood experiences and the risk of premature mortality. Am. J. Prev. Med. 37, 389–396 (2009).
Aronson, J. K. & Ferner, R. E. Biomarkers—a general review. Curr. Protoc. Pharmacol. 76, 9.23.1–9.23.17 (2017).
Dong, S. Z., Zhu, M. & Bulas, D. Techniques for minimizing sedation in pediatric MRI. J. Magn. Reson. Imaging 50, 1047–1054 (2019).
Bick, J. & Nelson, C. A. Early adverse experiences and the developing brain. Neuropsychopharmacology 41, 177–196 (2016).
McLaughlin, K. A., Weissman, D. & Bitrán, D. Childhood adversity and neural development: a systematic review. Annu Rev. Dev. Psychol. 1, 277–312 (2019).
Graham, A. M. et al. The potential of infant fMRI research and the study of early life stress as a promising exemplar. Dev. Cogn. Neurosci. 12, 12–39 (2015).
Brummelte, S. et al. Procedural pain and brain development in premature newborns. Ann. Neurol. 71, 385–396 (2012).
Vinall, J. et al. Invasive procedures in preterm children: brain and cognitive development at school age. Pediatrics 133, 412–421 (2014).
Jha, S. C. et al. Environmental influences on infant cortical thickness and surface area. Cereb. Cortex 29, 1139–1149 (2019).
Rifkin-Graboi, A. et al. Antenatal maternal anxiety predicts variations in neural structures implicated in anxiety disorders in newborns. J. Am. Acad. Child Adolesc. Psychiatry 54, 313–321 (2015).
Knickmeyer, R. C. et al. Impact of demographic and obstetric factors on infant brain volumes: a population neuroscience study. Cereb. Cortex 27, 5616–5625 (2017).
Betancourt, L. M. et al. Effect of socioeconomic status (SES) disparity on neural development in female African-American infants at age 1 month. Dev. Sci. 19, 947–956 (2016).
Qiu, A. et al. COMT haplotypes modulate associations of antenatal maternal anxiety and neonatal cortical morphology. Am. J. Psychiatry 172, 163–172 (2015).
Gao, W. et al. Functional network development during the first year: Relative sequence and socioeconomic correlations. Cereb. Cortex 25, 2919–2928 (2015).
Wu, Y. et al. Association of prenatal maternal psychological distress with fetal brain growth, metabolism, and cortical maturation. JAMA Netw. open 3, e1919940 (2020).
Wu, Y. & Limperopoulos, C. Pregnancy stress, anxiety, and depression sequela on neonatal brain development-reply. JAMA Pediatr. 174, 908–909 (2020).
Abbasi, H. & Puusepp-Benazzouz, H. Pregnancy stress, anxiety, and depression sequela on neonatal brain development. JAMA Pediatr. 174, 908 (2020).
Rotem-Kohavi, N., Williams, L. J. & Oberlander, T. F. Advanced neuroimaging: a window into the neural correlates of fetal programming related to prenatal exposure to maternal depression and SSRIs. Semin. Perinatol. 44, 151223 (2020).
Lautarescu, A. et al. Maternal prenatal stress is associated with altered uncinate fasciculus microstructure in premature neonates. Biol. Psychiatry 87, 559–569 (2020).
Xie, W. & Nelson, C. A. in Chapter on Handbook of Paediatric Brain Imaging: Methods, Modalities and Applications (eds Huang, H. & Robert, T.) (Elsevier, 2020).
Saby, J. N. & Marshall, P. J. The utility of EEG band power analysis in the study of infancy and early childhood. Dev. Neuropsychol. 37, 253–273 (2012).
Anderson, A. J. & Perone, S. Developmental change in the resting state electroencephalogram: Insights into cognition and the brain. Brain Cogn. 126, 40–52 (2018).
Bhavnani, S. et al. EEG signatures of cognitive and social development of preschool children-a systematic review. PLoS ONE 16, e0247223 (2021).
Marshall, P. J. & Fox, N. A. A comparison of the electroencephalogram between institutionalized and community children in Romania. J. Cogn. Neurosci. 16, 1327–1338 (2004).
McLaughlin, K. A. et al. Delayed maturation in brain electrical activity partially explains the association between early environmental deprivation and symptoms of attention-deficit/hyperactivity disorder. Biol. Psychiatry 68, 329–336 (2010).
Tomalski, P. et al. Socioeconomic status and functional brain development - associations in early infancy. Dev. Sci. 16, 676–687 (2013).
Brito, N. H., Fifer, W. P., Myers, M. M., Elliott, A. J. & Noble, K. G. Associations among family socioeconomic status, EEG power at birth, and cognitive skills during infancy. Dev. Cogn. Neurosci. 19, 144–151 (2016).
Jensen, S. K. G. et al. Associations of socioeconomic and other environmental factors with early brain development in Bangladeshi infants and children. Dev. Cogn. Neurosci. 50, 100981 (2021).
Pierce, L. J. et al. Association of perceived maternal stress during the perinatal period with electroencephalography patterns in 2-month-old infants. JAMA Pediatr. 173, 561–570 (2019).
St. John, A. M., Kao, K., Liederman, J., Grieve, P. G. & Tarullo, A. R. Maternal cortisol slope at 6 months predicts infant cortisol slope and EEG power at 12 months. Dev. Psychobiol. 59, 787–801 (2017).
Valdés-Hernández, P. A. et al. White matter architecture rather than cortical surface area correlates with the EEG alpha rhythm. Neuroimage 49, 2328–2339 (2010).
Otero, G. A. EEG spectral analysis in children with sociocultural handicaps. Int J. Neurosci. 79, 213–220 (1994).
Otero, G. A. Poverty, cultural disadvantage and brain development: a study of pre-school children in Mexico. Electroencephalogr. Clin. Neurophysiol. 102, 512–516(1997).
Otero, G. A., Pliego-Rivero, F. B., Fernández, T. & Ricardo, J. EEG development in children with sociocultural disadvantages: a follow-up study. Clin. Neurophysiol. 114, 1918–1925 (2003).
Benasich, A. A., Gou, Z., Choudhury, N. & Harris, K. D. Early cognitive and language skills are linked to resting frontal gamma power across the first 3 years. Behav. Brain Res. 195, 215–222 (2008).
Cantiani, C., Piazza, C., Mornati, G., Molteni, M. & Riva, V. Oscillatory gamma activity mediates the pathway from socioeconomic status to language acquisition in infancy. Infant Behav. Dev. 57, 101384 (2019).
Gou, Z., Choudhury, N. & Benasich, A. A. Resting frontal gamma power at 16, 24 and 36 months predicts individual differences in language and cognition at 4 and 5 years. Behav. Brain Res. 220, 263–270 (2011).
Pierce, L. J., Reilly, E. & Nelson, C. A. Associations between maternal stress, early language behaviors, and infant electroencephalography during the first year of life. J. Child Lang. 48, 737–764 (2021).
Stamoulis, C., Vanderwert, R. E., Zeanah, C. H., Fox, N. A. & Nelson, C. A. Early psychosocial neglect adversely impacts developmental trajectories of brain oscillations and their interactions. J. Cogn. Neurosci. 27, 2512–2528 (2015).
McLaughlin, K. A., Fox, N. A., Zeanah, C. H. & Nelson, C. A. Adverse rearing environments and neural development in children: the development of frontal electroencephalogram asymmetry. Biol. Psychiatry 70, 1008–1015 (2011).
Diego, M. A. et al. Prepartum, postpartum, and chronic depression effects on newborns. Psychiatry 67, 63–80 (2004).
Gotlib, I. H., Ranganath, C. & Rosenfeld, J. P. Frontal EEG alpha asymmetry, depression, and cognitive functioning. Cogn. Emot. 12, 449–478 (1998).
Bell, I. R., Schwartz, G. E., Hardin, E. E., Baldwin, C. M. & Kline, J. P. Differential resting quantitative electroencephalographic alpha patterns in women with environmental chemical intolerance, depressives, and normals. Biol. Psychiatry 43, 376–388 (1998).
Blackhart, G. C., Minnix, J. A. & Kline, J. P. Can EEG asymmetry patterns predict future development of anxiety and depression? A preliminary study. Biol. Psychol. 72, 46–50 (2006).
O’Toole, J. M, Pavlidis, E., Korotchikova, I., Boylan, G. B. & Stevenson, N. J. Temporal evolution of quantitative EEG within 3 days of birth in early preterm infants. Sci. Rep. 9, 4859 (2019).
Torda, C. Effects of postinatal stress on visual and auditory evoked potentials. Percept. Mot. Skills 43, 315–322 (1976).
Harvison, K. W., Molfese, D. L., Woodruff-Borden, J. & Weigel, R. A. Neonatal auditory evoked responses are related to perinatal maternal anxiety. Brain Cogn. 71, 369–374 (2009).
Giuliano, R. J. et al. Effects of early adversity on neural mechanisms of distractor suppression are mediated by sympathetic nervous system activity in preschool-aged children. Dev. Psychol. 54, 1674 (2018).
Isbell, E., Stevens, C., Hampton Wray, A., Bell, T. & Neville, H. J. 5-HTTLPR polymorphism is linked to neural mechanisms of selective attention in preschoolers from lower socioeconomic status backgrounds. Dev. Cogn. Neurosci. 22, 36–47 (2016).
Willner, C. J., Gatzke-Kopp, L. M., Bierman, K. L., Greenberg, M. T. & Segalowitz, S. J. Relevance of a neurophysiological marker of attention allocation for children’s learning-related behaviors and academic performance. Dev. Psychol. 51, 1148 (2015).
Hampton Wray, A. et al. Development of selective attention in preschool-age children from lower socioeconomic status backgrounds. Dev. Cogn. Neurosci. 26, 101–111 (2017).
van den Heuvel, M. I., Donkers, F. C. L., Winkler, I., Otte, R. A. & Van den Bergh, B. R. H. Maternal mindfulness and anxiety during pregnancy affect infants neural responses to sounds. Soc. Cogn. Affect Neurosci. 10, 453–460 (2013).
Stevens, C., Lauinger, B. & Neville, H. Differences in the neural mechanisms of selective attention in children from different socioeconomic backgrounds: an event-related brain potential study. Dev. Sci. 12, 634–646 (2009).
Stevens, C., Paulsen, D., Yasen, A. & Neville, H. Atypical auditory refractory periods in children from lower socio-economic status backgrounds: ERP evidence for a role of selective attention. Int. J. Psychophysiol. 95, 156–166 (2015).
Pierce, L. J., Carmody Tague, E. & Nelson, C. A. 3rd Maternal stress predicts neural responses during auditory statistical learning in 26-month-old children: an event-related potential study. Cognition 213, 104600 (2021).
Brooker, R. J. Maternal behavior and socioeconomic status predict longitudinal changes in error-related negativity in preschoolers. Child Dev. 89, 725–733 (2018).
Conejero, Á., Guerra, S., Abundis-Gutiérrez, A. & Rueda, M. R. Frontal theta activation associated with error detection in toddlers: influence of familial socioeconomic status. Dev. Sci. 21, e12494 (2018).
St. John, A. M., Finch, K. & Tarullo, A. R. Socioeconomic status and neural processing of a go/no-go task in preschoolers: an assessment of the P3b. Dev. Cogn. Neurosci. 38, 100677 (2019).
Ruberry, E. J. et al. Income, neural executive processes, and preschool children’s executive control. Dev. Psychopathol. 29, 143–154 (2017).
A. Porto, J., L. Nunes, M. & Nelson, C. A. Behavioral and neural correlates of emotional development: typically developing infants and infants of depressed and/or anxious mothers. J. Pediatr. 92, S14–S22 (2016).
Slopen, N., McLaughlin, K. A., Fox, N. A., Zeanah, C. H. & Nelson, C. A. Alterations in neural processing and psychopathology in children raised in institutions. Arch. Gen. Psychiatry 69, 1022–1030 (2012).
Moulson, M. C., Fox, N. A., Zeanah, C. H. & Nelson, C. A. Early adverse experiences and the neurobiology of facial emotion processing. Dev. Psychol. 45, 17 (2009).
Pinti, P. et al. The present and future use of functional near-infrared spectroscopy (fNIRS) for cognitive neuroscience. Ann. N. Y. Acad. Sci. 1464, 5 (2018).
Wijeakumar, S., Kumar, A., Delgado Reyes, L. M., Tiwari, M. & Spencer, J. P. Early adversity in rural India impacts the brain networks underlying visual working memory. Dev. Sci. 22, e12822 (2019).
Perdue, K. L. et al. Using functional near-infrared spectroscopy to assess social information processing in poor urban Bangladeshi infants and toddlers. Dev. Sci. 22, e12839 (2019).
Monk, C., Lugo-Candelas, C. & Trumpff, C. Prenatal developmental origins of future psychopathology: mechanisms and pathways. Annu. Rev. Clin. Psychol. 15, 317–344 (2019).
McGowan, P. O. & Matthews, S. G. Prenatal stress, glucocorticoids, and developmental programming of the stress response. Endocrinology 159, 69–82 (2018).
Beijers, R., Buitelaar, J. K. & de Weerth, C. Mechanisms underlying the effects of prenatal psychosocial stress on child outcomes: beyond the HPA axis. Eur. Child Adolesc. Psychiatry 23, 943–956 (2014).
Liu, C. H. & Doan, S. N. Innovations in biological assessments of chronic stress through hair and nail cortisol: conceptual, developmental, and methodological issues. Dev. Psychobiol. 61, 465–476 (2019).
Pourkaviani, S. et al. Clinical validation of the Neonatal Infant Stressor Scale with preterm infant salivary cortisol. Pediatr. Res. 87, 1237–1243 (2020).
Thayer, Z. M., Wilson, M. A., Kim, A. W. & Jaeggi, A. V. Impact of prenatal stress on offspring glucocorticoid levels: a phylogenetic meta-analysis across 14 vertebrate species. Sci. Rep. 8, 4942 (2018).
Vedhara, K. et al. Maternal mood and neuroendocrine programming: effects of time of exposure and sex. J. Neuroendocrinol. 24, 999–1011 (2012).
Capron, L., Glover, V. & Ramchandani, P. Does maternal antenatal depression alter infant hypothalamic-pituitary-adrenal (HPA) axis functioning in the offspring at 4 months postpartum? Psychoneuroendocrinology 61, 33 (2015).
Tarullo, A. R. & Gunnar, M. R. Child maltreatment and the developing HPA axis. Horm. Behav. 50, 632–639 (2006).
Miller, G., Chen, E. & Zhou, E. If it goes up, must it come down? Chronic stress and the hypothalamic-pituitary-adrenocorical (HPA) axis in humans. Psychol. Bull. 133, 25–45 (2007).
Finegood, E. D., Rarick, J. R. D. & Blair, C. Exploring longitudinal associations between neighborhood disadvantage and cortisol levels in early childhood. Dev. Psychopathol. 29, 1649–1662 (2017).
Yong Ping, E. et al. Prenatal maternal stress predicts stress reactivity at 21/2 years of age: The Iowa Flood Study. Psychoneuroendocrinology 56, 62–78 (2015).
Stroud, L. R. et al. Prenatal major depressive disorder, placenta glucocorticoid and serotonergic signaling, and infant cortisol response. Psychosom. Med. 78, 979–990 (2016).
Palmer, F. B. et al. Early adversity, socioemotional development, and stress in urban 1-year-old children. J. Pediatr. 163, 1733–1739 (2013).
Bosquet Enlow, M. et al. Maternal cortisol output in pregnancy and newborn telomere length: Evidence for sex-specific effects. Psychoneuroendocrinology 102, 225–235 (2019).
Gunnar, M. R., Talge, N. M. & Herrera, A. Stressor paradigms in developmental studies: What does and does not work to produce mean increases in salivary cortisol. Psychoneuroendocrinology 34, 953–967 (2009).
Puhakka, I. J. A. & Peltola, M. J. Salivary cortisol reactivity to psychological stressors in infancy: a meta-analysis. Psychoneuroendocrinology 115, 104603 (2020).
Slopen, N., Koenen, K. C. & Kubzansky, L. D. Childhood adversity and immune and inflammatory biomarkers associated with cardiovascular risk in youth: a systematic review. Brain Behav. Immun. 26, 239–250 (2012).
Baumeister, D., Akhtar, R., Ciufolini, S., Pariante, C. M. & Mondelli, V. Childhood trauma and adulthood inflammation: a meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-α. Mol. Psychiatry 21, 642–649 (2016).
Raison, C. L. & Miller, A. H. When not enough is too much: the role of insufficient glucocorticoid signaling in the pathophysiology of stress-related disorders. Am. J. Psychiatry 160, 1554–1565 (2003).
Chrousos, G. P. The hypothalamic-pituitary-adrenal axis and immune-mediated inflammation. N. Engl. J. Med. 332, 1351–1362 (1995).
Danese, A., Pariante, C. M., Caspi, A., Taylor, A. & Poulton, R. Childhood maltreatment predicts adult inflammation in a life-course study. Proc. Natl Acad. Sci. USA 104, 1319–1324 (2007).
Danese, A. et al. Adverse childhood experiences and adult risk factors for age-related disease. Arch. Pediatr. Adolesc. Med. 163, 1135–1143 (2009).
Kanterman, J., Sade-Feldman, M. & Baniyash, M. New insights into chronic inflammation-induced immunosuppression. Semin. Cancer Biol. 22, 307–318 (2012).
Bush, N. R. et al. Maternal stress during pregnancy predicts infant infectious and noninfectious illness. J. Pediatr. 228, 117–125.e2 (2021).
David, J., Measelle, J., Ostlund, B. & Ablow, J. Association between early life adversity and inflammation during infancy. Dev. Psychobiol. 59, 696–702 (2017).
Measelle, J. R. & Ablow, J. C. Contributions of early adversity to pro-inflammatory phenotype in infancy: the buffer provided by attachment security. Attach Hum. Dev. 20, 1–23 (2018).
Decaro, J. A., Manyama, M. & Wilson, W. Household-level predictors of maternal mental health and systemic inflammation among infants in Mwanza, Tanzania. Am. J. Hum. Biol. 28, 461–470 (2016).
Slopen, N., Zhang, J., Urlacher, S. S., De Silva, G. & Mittal, M. Maternal experiences of intimate partner violence and C-reactive protein levels in young children in Tanzania. SSM Popul Heal. 6, 107–115 (2018).
Tyrka, A. R., Parade, S. H., Valentine, T. R., Eslinger, N. M. & Seifer, R. Adversity in preschool-aged children: effects on salivary interleukin-1β. Dev. Psychopathol. 27, 567–576 (2015).
Riis, J. L. et al. Maternal distress and child neuroendocrine and immune regulation. Soc. Sci. Med. 1982, 206–214 (2016).
Kuhlman, K. R., Horn, S. R., Chiang, J. J. & Bower, J. E. Early life adversity exposure and circulating markers of inflammation in children and adolescents: a systematic review and meta-analysis. Brain Behav. Immun. 86, 30–42 (2020).
Shonkoff, J. P. Building a new biodevelopmental framework to guide the future of early childhood policy. Child Dev. 81, 357–367 (2010).
Evans, G. W., Li, D. & Whipple, S. S. Cumulative risk and child development. Psychol. Bull. 139, 1342–1396 (2013).
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on Applying Neurobiological and Socio-Behavioral Sciences from Prenatal Through Early Childhood Development. in Vibrant and Healthy Kids: Aligning Science, Practice, and Policy to Advance Health Equity (eds Negussie, Y., Geller, A. & DeVoe, J. E.) (National Academies Press (US), Washington (DC), 2019).
Campbell, T. L. Screening for adverse childhood experiences (ACEs) in primary care: a cautionary note. JAMA 323, 2379–2380 (2020).
Harris, N. B. Screening for adverse childhood experiences. JAMA 324, 1788–1789 (2020).
Blackburn, E. H. Structure and function of telomeres. Nature 350, 569–573 (1991).
Cawthon, R. M., Smith, K. R., O’Brien, E., Sivatchenko, A. & Kerber, R. A. Association between telomere length in blood and mortality in people aged 60 years or older. Lancet 361, 393–395 (2003).
Rode, L., Nordestgaard, B. G. & Bojesen, S. E. Peripheral blood leukocyte telomere length and mortality among 64 637 individuals from the general population. J. Natl Cancer Inst. 107, djv074 (2015).
Epel, E. S. et al. Accelerated telomere shortening in response to life stress. Proc. Natl Acad. Sci. USA 101, 17312 LP–17315 (2004).
Puterman, E. & Epel, E. An intricate dance: life experience, multisystem resiliency, and rate of telomere decline throughout the lifespan. Soc. Personal. Psychol. Compass 6, 807–825 (2012).
Stout, S. A. et al. Validation of minimally-invasive sample collection methods for measurement of telomere length. Front. Aging Neurosci. 9, 397 (2017).
Epel, E. S. & Prather, A. A. Stress, telomeres, and psychopathology: toward a deeper understanding of a triad of early aging. Annu Rev. Clin. Psychol. 14, 371–397 (2018).
Shalev, I. et al. Exposure to violence during childhood is associated with telomere erosion from 5 to 10 years of age: a longitudinal study. Mol. Psychiatry 18, 576–581 (2013).
Chae, D. H. et al. Discrimination, racial bias, and telomere length in African-American men. Am. J. Prev. Med. 46, 103–111 (2014).
Drury, S. S., Mabile, E. & Brett, Z. H. et al. The association of telomere length with family violence and disruption. Pediatrics 134, e128–e137 (2014).
Rewak, M. et al. Race-related health disparities and biological aging: does rate of telomere shortening differ across blacks and whites? Biol. Psychol. 99, 92–99 (2014).
Broer, L. et al. Meta-analysis of telomere length in 19 713 subjects reveals high heritability, stronger maternal inheritance and a paternal age effect. Eur. J. Hum. Genet. 21, 1163–1168 (2013).
Coimbra, B. M., Carvalho, C. M., Moretti, P. N., Mello, M. F. & Belangero, S. I. Stress-related telomere length in children: a systematic review. J. Psychiatr. Res. 92, 47–54 (2017).
Entringer, S. et al. Stress exposure in intrauterine life is associated with shorter telomere length in young adulthood. Proc. Natl. Acad. Sci USA. 108, 201107759 (2011).
Marchetto, N. et al. Prenatal stress and newborn telomere length. Am. J. Obstet. Gynecol. 215, 94.e1–94.e8 (2016).
Nelson, B. W., Allen, N. B. & Laurent, H. Infant HPA axis as a potential mechanism linking maternal mental health and infant telomere length. Psychoneuroendocrinology 88, 38–46 (2018).
Beijers, R. et al. Testing three hypotheses about effects of sensitive-insensitive parenting on telomeres. Dev. Psychol. 56, 237–250 (2020).
Jones, C. W. et al. The transgenerational transmission of maternal adverse childhood experiences (ACEs): Insights from placental aging and infant autonomic nervous system reactivity. Psychoneuroendocrinology 106, 20–27 (2019).
Esteves, K. C. et al. Adverse childhood experiences: Implications for offspring telomere length and psychopathology. Am. J. Psychiatry 177, 47–57 (2020).
Lester, B. M., Conradt, E. & Marsit, C. Introduction to the special section on epigenetics. Child Dev. 87, 29–37 (2016).
McEwen, L. M., O’Donnell, K. J. & McGill, M. G. et al. The PedBE clock accurately estimates DNA methylation age in pediatric buccal cells. Proc. Natl Acad. Sci. USA 117, 23329–23335 (2020).
O’Reilly, H., Johnson, S., Ni, Y., Wolke, D. & Marlow, N. Neuropsychological outcomes at 19 years of age following extremely preterm birth. Pediatrics 145, e20192087 (2020).
Woythaler, M., McCormick, M. C., Mao, W. Y. & Smith, V. C. Late preterm infants and neurodevelopmental outcomes at kindergarten. Pediatrics 136, 424–431 (2015).
Ranger, M. & Grunau, R. E. Early repetitive pain in preterm infants in relation to the developing brain. Pain. Manag. 4, 57–67 (2014).
Barrero-Castillero, A., Morton, S. U., Nelson, C. A. & Smith, V. C. Psychosocial stress and adversity: effects from the perinatal period to adulthood. Neoreviews 20, e686–e696 (2019).
Cheong, J. L. Y., Burnett, A. C., Treyvaud, K. & Spittle, A. J. Early environment and long-term outcomes of preterm infants. J. Neural Transm. 127, 1–8 (2020).
Treyvaud, K. et al. Early parenting is associated with the developing brains of children born very preterm. Clin. Neuropsychol. 31, 1–19 (2020).
Erdei, C., Inder, T. E., Dodrill, P. & Woodward, L. J. The growth and development unit. A proposed approach for enhancing infant neurodevelopment and family-centered care in the Neonatal Intensive Care Unit. J. Perinatol. 39, 1684–1687 (2019).
Funding
Dr. Charles A. Nelson time was funded by the National Institutes of Health award MH091363 and the JPB Research Network on Toxic Stress: A project of the Center on the Developing Child at Harvard University (JPB Foundation award 256577-5108544).
Author information
Authors and Affiliations
Contributions
Dr. Alejandra Barrero-Castillero conceptualized the review and wrote the initial manuscript. Dr. Alejandra Barrero-Castillero, Dr. Lara Pierce, Mr. Saul Urbina-Johanson, and Dr. Laura Pirazzoli performed a detailed literature review of biomarkers of adversity, edited the manuscript, and critically reviewed it. Dr. Heather H. Burris and Dr. Charles A. Nelson critically reviewed and edited the manuscript for important intellectual content and contributed to the interpretation of findings. Dr. Charles Nelson mentored Dr. Barrero-Castillero throughout the review. All the authors together defined the scope of the review, interpreted the data, and edited the manuscript. All authors approved the final submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Barrero-Castillero, A., Pierce, L.J., Urbina-Johanson, S.A. et al. Perinatal and early childhood biomarkers of psychosocial stress and adverse experiences. Pediatr Res 92, 956–965 (2022). https://doi.org/10.1038/s41390-022-01933-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-01933-z
This article is cited by
-
Adverse childhood experiences and lifelong health
Nature Medicine (2023)