Abstract
Background
Endothelial microparticles (EMPs) act as early biomarkers of endothelial activation and damage. No studies have investigated EMPs in preterm-born individuals.
Methods
Sixty-three preterm-born children and 52 children born full-term (controls) were studied. Circulating CD62E(+), CD144(+), and CD31(+)/CD42b(−) EMPs were measured in preterm-born children compared to controls; possible associations with cardiovascular risk factors and endothelial function parameters were also assessed.
Results
Circulating CD62E(+), CD144(+), and CD31(+)/CD42b(−) EMPs were significantly higher in preterm-born children compared to controls (p = 0.003, p < 0.001, and p < 0.001, respectively). Preterm birth was recognized as an independent predictor of each EMP subpopulation studied; moreover, the mean pressure and velocity of pulmonary artery were independently correlated with CD62E(+) (β = 0.20, p = 0.04) and CD144(+) EMPs (β = 0.22, p = 0.02), respectively, whereas age (β = 0.21, p = 0.03) and being born SGA (β = 0.26, p = 0.01) correlated independently with CD31(+)/CD42b(−) EMPs in the study population. Furthermore, diastolic blood pressure (β = 0.24, p = 0.04), being born SGA (β = 0.24, p = 0.04) and the hyperemic peak velocity of the brachial artery (β = −0.65, p = 0.02) were independently associated with CD31(+)/CD42b(−) EMPs in the preterm-born group.
Conclusion
Circulating EMPs were higher in preterm-born children compared to children born full-term. Whether EMPs could act, in clinical practice, as a complementary tool for non-invasive evaluation of endothelium in preterm-born children, remains under investigation.
Impact
-
Circulating endothelial microparticles (EMPs) are small membrane vesicles released from endothelial cells and they act as novel biomarkers of endothelial activation and damage.
-
No studies have investigated circulating EMPs in preterm-born individuals.
-
Circulating EMPs were significantly higher in prepubertal preterm-born children compared to children born at term.
-
In the preterm-born group, the hyperemic peak velocity of the brachial artery was independently associated with CD31(+)/CD42b(−) EMPs.
-
Whether assessment of circulating EMPs could act, in clinical practice, as a complementary tool for non-invasive evaluation of endothelium in preterm-born children, remains to be defined in future investigations.
Similar content being viewed by others
Introduction
Despite improvements in survival of preterm babies over the last decades, the long-term outcomes of these infants remain of serious concern. In addition to the increased risk for neurodevelopmental impairment, prematurity is associated with cardio-metabolic alterations and adverse cardiovascular health in later life.1,2,3,4,5 Previous studies have shown that children and/or adults born prematurely display elevated arterial blood pressure,6,7 increased serum insulin levels and glucose intolerance,6,8 disturbances in lipid profile,9,10 higher total body fat mass and increased risk for obesity,10 increased mean carotid (cIMT) and abdominal aortic (aIMT) intima-media thickness,11,12,13 adverse changes in heart shape and function,14,15 and also endothelial injury,16,17 in comparison with individuals born after a full-term pregnancy. Furthermore, prematurity predisposes to central hypertension and dysregulation of the cross-talk between microcirculation and macrocirculation in childhood;18 the retinal arteriolar diameters were found to be smaller, but with higher central systolic and mean arterial blood pressure and with greater forward/backward wave amplitude. The mechanisms that link prematurity with cardiovascular risk and impaired endothelial function are still under investigation; excess generation of reactive oxygen species (ROS) and/or increased intracellular oxidative stress,2 abnormal inflammatory response,19 increased circulating endothelial progenitor cells (EPCs)20 or endothelial colony-forming cells (ECFC) dysfunction21 in preterm-born individuals are potential pathways.
Circulating endothelial microparticles (EMPs) are described as small membrane vesicles, <1.0 μm in size, released from endothelial cells in response to stimuli such as inflammatory activation, apoptosis, or injury.22 EMPs act as early biomarkers of endothelial activation and damage; elevated EMPs numbers indicate endothelial dysfunction and they are related to a variety of disease states, including metabolic syndrome,23 diabetes mellitus type 2,24 acute coronary syndrome and cardiovascular disease25 among others. However, increasing evidence suggests that EMPs are more than simple markers of endothelial status;22 they interfere with coagulation pathways and vascular tone, they have thrombogenic activity, and thus they have an evolving role in the pathophysiology of endothelial dysfunction and atherosclerosis.22 To the best of our knowledge, there are no reported studies that investigated circulating EMPs in preterm-born individuals.
The aim of this study was to evaluate circulating EMPs levels in prepubertal children born prematurely, and to assess possible associations of EMPs with cardiovascular risk factors and endothelial function parameters in our study population.
Methods
Study design and population
In this cross-sectional study, 115 healthy children (51 males and 64 females) of prepubertal age (10.60 ± 1.85 years) born between January 2007 and December 2011 were enrolled. Of them, 63 children (25 males and 38 females) were born prematurely (<37 weeks of gestational age), whereas 52 children (26 males and 26 females) were born at term (37–42 weeks of gestational age) and appropriate for gestational age (AGA), thus consisting the control group; AGA was defined as birth weight between 10th and 90th percentiles for gestational age.26 The preterm group was described in a recent study investigating circulating EPCs in association with cardiovascular risk factors and endothelial parameters in prepubertal children born prematurely compared to prepubertal children born at term.20 Eleven out of 63 preterm-born children were born small for gestational age (SGA) (birth weight below 10th percentile).26
All children were hospitalized as neonates and randomly traced, by simple random sampling technique, from lists from the neonatal follow-up clinic which provides regular follow-up to all infants admitted. Medical and family history was obtained, while perinatal and neonatal data were collected from hospital medical records. Pregnancy complications and neonatal morbidity were examined; bronchopulmonary dysplasia (BPD) was defined as supplemental oxygen requirements at 36 weeks of postmenstrual age.27
Exclusion criteria were personal or family history of cardiovascular disease, congenital malformations, acute or chronic inflammatory process or any disease, or obesity [body mass index (BMI) ≥ 95th percentile for age]. The study protocol was approved by the local research and ethics committee on research on humans and it conforms to the ethical guidelines of the 1975 Declaration of Helsinki; all children included in this study provided their assent, while written informed consent was also obtained from their parents or legal guardians.
Clinical assessment
As described previously,20 participants attended the outpatient clinic at a similar time of day (07.30–9.30 AM) after a 12-h overnight fast; all children were free of physical exercise for at least 8–12 h before the examination. Standing height and weight were measured to the nearest 0.1 cm and 0.1 kg, respectively, on bare foot and subjects wearing light clothing. Waist and hip circumference were measured to the nearest 0.1 cm over an unclothed abdomen and at minimal respiration. The waist-to-hip ratio (WHR) and the BMI (kg/m2) were calculated. Neck circumference was measured with the neck in a horizontal plane at the level of the thyroid cartilage. All anthropometric measurements were performed twice; the mean was used for analysis. Both systolic (SBP) and diastolic blood pressure (DBP) were measured three times from the left brachial artery using an automatic oscillometric blood pressure monitor after a 10-m rest in a sitting position; the second and third measurements were averaged for analysis.
Blood biochemistry
Fasting serum glucose and insulin, total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, and triglycerides were measured in all participants. The homeostasis model assessment of insulin resistance (HOMA-IR) index was calculated as insulin (μU/mL) × blood glucose (mmol/L)/22.5; IR was defined as HOMA-IR > 2.5.28
Ultrasound studies
Measurements of cIMT and aIMT, measurement of FMD of the brachial artery, and echocardiography with evaluation of several parameters including left ventricular ejection fraction, shortening fraction, end-diastolic interventricular septal thickness, left ventricular end-systolic, end-diastolic internal diameters, end-diastolic left ventricular posterior wall thickness, left ventricular mass and relative wall thickness, left ventricular mass index, and mean pressure and velocity of the pulmonary artery were performed by a single experienced vascular sonographer and a single senior pediatric cardiologist, respectively, in all children studied according to standardized protocols,29,30,31,32 as described in detail previously.20 For cIMT, six measurements were performed on each side; the calculated mean provided respectively the arithmetic mean left and right cIMT of each subject. Mean aIMT was determined as the average reading of three measurements for each subject. FMD of the brachial artery was calculated using the formula: FMD = [(maximum dilatation diameter after deflation – baseline diameter)/(baseline diameter)] × 100%.
Both the vascular sonographer and the pediatric cardiologist were blinded to the gestational age of the subjects and unaware of the clinical and laboratory characteristics of the study population.20
Flow cytometric analysis of circulating EMPs
Blood samples (3 mL) were collected in 3.2% sodium citrate tubes following an overnight fast in an atraumatic fashion using a 21-gauge needle; the first 5 mL of withdrawn blood were used for routine blood tests, including blood biochemistry, in order to avoid contamination with EMPs due to vascular injury.33 The citrated blood samples were processed within 1–2 h after collection. Circulating EMPs were detected and measured in platelet-poor plasma, after a two-step centrifugation protocol, as previously described.33 EMPs in plasma samples were phenotyped and quantified by flow cytometry; 50 μL of platelet-poor plasma were incubated with fluorochrome labeled antibodies specific for CD31 [CD31-FITC (ImmunoTools)], CD62E [CD62E-PE (Santa Cruz Biotechnology)], CD144 [CD144-PerCP (Santa Cruz Biotechnology)], and CD42b [CD42b-APC (ImmunoTools)], for 20 m at 4 °C in the dark. After staining, samples were diluted with phosphate-buffered saline (PBS) and then they were analyzed in a fluorescence activated cell sorter (FACS) Calibur flow cytometer (BD FACSCaliburTM, BD Biosciences).34 The data obtained were analyzed using the Flowing Software version 2.5.1.
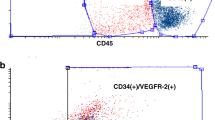
Three EMPs subpopulations were identified as CD62E(+), CD144(+), or CD31(+)/CD42b(−) events; values are reported as the percentage of each EMP subpopulation among the total microparticle population. CD62E(+) and CD144(+) EMP subpopulations are microparticles that express CD62E and CD144 surface markers respectively. CD31(+)/CD42b(−) EMP subpopulation are microparticles that express CD31 surface marker, but they do not express CD42b surface marker at the same time. As CD31 is present not only on EMPs, but also on activated platelets and platelet microparticles, CD42b was also used, as a platelet-specific marker to distinguish CD31(+) EMPs from platelet-derived microparticles.35 All samples were analyzed in triplicate with excellent repeatability for all EMPs subpopulations [intraclass correlation coefficient (ICC) greater than 0.90 is indicative of excellent reliability]; ICC = 0.98 for CD62E(+), ICC = 0.92 for CD144(+), and ICC = 0.93 for CD31(+)/CD42b(−) EMPs. Measurements were performed blinded to the gestational age of the subjects and to the clinical, laboratory, and ultrasound characteristics of the study population.
Sample size calculation
As our study was the first study to evaluate circulating EMPs levels in prepubertal children born prematurely compared to children of same age born at term, the a priori statistical power analysis was based on previous studies that investigated potential differences of EMPs subpopulations in several other groups of children. The effect size (ES) in the studies used was medium to large for the three EMPs subpopulations studied using Cohen’s (1988) criteria; ES = 0.77 for CD62E(+) EMPs,36 ES = 1.13 for CD144(+) EMPs,37 and ES = 0.64 for CD31(+)/CD42b(−) EMPs34. With an alpha risk = 0.05 and a power = 0.80, the projected sample size needed with this effect size (GPower 3.1.9.2 software) was estimated to be at least N = 41 for each of the groups of children studied.
Statistical analysis
Statistical analysis was performed using SPSS version 23.0 (SPSS Inc., Chicago, IL). In parameters with normal distribution, results are given as mean ± SD; for parameters not normally distributed, results are expressed as medians (25th–75th percentile). Groups were compared using independent t-test or Mann–Whitney test, as appropriate, for continuous variables and chi-square test for categorical variables. Univariate regression analyses between variables of interest were calculated. Multiple linear regression analyses were then applied, with each EMP subpopulation as a dependent variable, in order to examine whether the associations observed in univariate regression analyses remained significant; multiple linear regression models were run in a stepwise method with a probability of 0.05 to enter and 0.10 to remove. Due to skewed distribution, EMPs values were log-transformed before applying regression analyses. Multiple stepwise linear regression analysis was also used to investigate independent determinants of the hyperemic peak velocity and the FMD of the brachial artery, as parameters of endothelial function.
In multiple regression analyses, the model goodness-of-fit was evaluated by both estimating R2 (multiple coefficient of determination) and graphically by examining the residuals from the multiple regression models. Multicollinearity was evaluated by assessing bivariate correlations among independent variables; correlation coefficients had to be less than 0.80 in order to eliminate multicollinearity.
Given that a proportion (17.5%) of the preterm group was also born SGA, sensitivity analyses were undertaken excluding SGA children from comparisons between groups and also from the regression models to assess the influence of prematurity per se on EMPs, endothelial function parameters, and cardiovascular risk factors studied.
A p value ≤0.05 was considered statistically significant.
Results
The baseline clinical, perinatal, and biochemical characteristics, as well as the vascular assessment and echocardiography of the preterm-born children were reported previously20 and are summarized, along with data in children born at term (controls), in Tables 1 and 2.
In preterm-born children, circulating CD62E(+) [8.71 (6.40–11.96)% vs. 6.70 (4.59–9.66)%, p = 0.003], CD144(+) [1.61 (0.62–4.38)% vs. 0.83 (0.42–1.45)%, p < 0.001] and CD31(+)/CD42b(−) [24.35 (8.50–53.73)% vs. 7.1 (3.39–14.39)%, p < 0.001] EMPs were significantly higher compared to controls (Fig. 1 and Supplementary Fig. 1). No differences were found between males and females regarding EMPs subpopulations studied.
In the total study population, circulating CD62E(+) EMPs correlated significantly with preterm birth, gestational age, birth weight, mean pressure, and velocity of pulmonary artery by univariate regression analysis; circulating CD144(+) EMPs correlated with preterm birth, gestational age, birth weight, SBP, mean pressure, and velocity of pulmonary artery; circulating CD31(+)/CD42b(−) EMPs correlated with age, preterm birth, being born SGA, DBP, mean cIMT, mean pressure, and velocity of pulmonary artery (Table 3 Supplementary Fig. 2). In multiple regression analysis, preterm birth was recognized as an independent predictor for each EMP subpopulation studied (Table 3). Moreover, the mean pressure of pulmonary artery was independently correlated with CD62E(+) EMPs, the mean velocity of pulmonary artery was independently correlated with CD144(+) EMPs, while age and being born SGA were independently correlated with CD31(+)/CD42b(−) EMPs (Table 3).
In the preterm-born group, in univariate analysis, circulating CD31(+)/CD42b(−) EMPs correlated significantly with gestational age (β = 0.35, p = 0.005), birth weight (β = 0.29, p = 0.02), being born SGA (β = 0.29, p = 0.02), and DBP (β = 0.28, p = 0.03). In multiple regression analysis, with EMPs levels as a dependent variable, gestational age (β = 0.36, p = 0.003), SGA (β = 0.24, p = 0.04), and DBP (β = 0.24, p = 0.04) were found to be independent predictors of CD31(+)/CD42b(−) EMPs (R2 of model = 0.53, p < 0.001). Furthermore, following evaluation of the independent associations between parameters of endothelial function (namely FMD and hyperemic peak velocity of the brachial artery, as dependent variables) and variables of interest, it was shown that age (β = −0.38, p = 0.002) and the peak diameter of the brachial artery (β = 0.54, p < 0.001) correlated independently with FMD (R2 of model = 0.45, p < 0.001), while age (β = 0.43, p = 0.001) and CD31(+)/CD42b(−) EMPs (β = −0.65, p = 0.02) were independently associated with the hyperemic peak velocity of brachial artery (R2 = 0.46, p < 0.001) in the preterm group.
The sensitivity analyses excluding preterm children born SGA from comparisons between groups showed essentially same results with those of the main analyses. In preterm-born AGA children, circulating CD62E(+) [8.55 (6.46–11.71)%], CD144(+) [1.57 (0.60–4.89)%], and CD31(+)/CD42b(−) [15.88 (5.32–50.22)%] EMPs were significantly higher compared to controls (p = 0.01, p = 0.001, and p = 0.01, respectively). Moreover, the associations among variables of interest remained robust in sensitivity analyses. The above associations remained also significant when the impact of maternal and neonatal morbidity, including the days of mechanical ventilation and the duration of hospitalization, were assessed in multiple regression analysis.
Discussion
In this study, circulating CD62E(+), CD144(+), and CD31(+)/CD42b(−) EMPs were found to be significantly higher in prepubertal children born prematurely compared to children born at term. Preterm birth was recognized as an independent predictor of all EMPs subpopulations studied; moreover, the mean pressure of pulmonary artery was independently correlated with CD62E(+), the mean velocity of pulmonary artery correlated independently with CD144(+) EMPs, whereas age and being born SGA correlated independently with CD31(+)/CD42b(−) EMPs. Furthermore, DBP, being born SGA and the hyperemic peak velocity of the brachial artery were independently associated with CD31(+)/CD42b(−) EMPs in the preterm-born group.
To the best of our knowledge, this is the first study investigating circulating EMPs in preterm-born individuals. The study population derived from the follow-up outpatient clinic of our Neonatal Unit, whereas healthy prepubertal children born either prematurely or after a full-term pregnancy were enrolled; perinatal data and medical records were reliably recorded and easily accessed. Comparisons of EMPs between preterm AGA and full-term children maintained significant; thus, the influence of prematurity per se was highlighted. Several endothelial surface markers have previously been used to detect circulating EMPs, including CD31, CD51, CD54, CD62E, CD105, CD144, and CD146; nevertheless, most of them are not restricted to endothelial cells.35 In our study, we focused on three different subpopulations of EMPs—CD62E(+), CD144(+), and CD31(+)/CD42b(−) EMPs—using surface markers that are expressed only on endothelial cells and are considered to be the most specific for the endothelium; all the above consisted the main strengths of this study.
EMPs have been examined in a variety of diseases in children; they have been found significantly elevated in obese and overweight children,34 in children with Kawasaki disease,38 Henoch–Scholein purpura,39 and pulmonary hypertension,40 among others. Normal values of EMPs in children have not been determined yet; however, levels of EMPs observed in controls in the studies mentioned above are similar to EMPs levels of the controls in our study.
The potential mechanisms that may link prematurity with cardiovascular risk are not well defined;2,3,4 diminished nitric oxide generation, excess generation of reactive oxygen species (ROS) and/or increased intracellular oxidative stress, impaired cytokine release which exaggerates the inflammatory response, as well as increased plasma renin and angiotensin II levels, and smooth muscle cell proliferation and migration to the intima causing intima-media thickness, are potential pathways.2 The abnormal inflammatory response, the vascular hyper-activity and potential endothelial dysfunction, as well as genetic factors, epigenetic modifications, and gut microbiome abnormalities may also increase the cardiovascular risk of preterm-born individuals in later life.2 Besides, there is evidence that EMPs possess a negative impact on cardiovascular health in a similar way; studies conducted in adult rats showed that EMPs contribute to endothelial dysfunction by reducing acetylcholine-induced vascular relaxation and by decreasing nitric oxide generation and increasing the release of ROS.41 Furthermore, EMPs stimulate the release of cytokines, IL-6 and IL-8, and they promote endothelial and vascular inflammation.22 The significant associations between EMPs and cardiovascular risk factors examined in our study population may highlight the impact of endothelial dysfunction on future cardiovascular morbidity of individuals born prematurely.
Ultrasound measurement of flow-mediated dilation (FMD) of the brachial artery is commonly used as a non-invasive measure of conduit artery endothelial dysfunction. In our study population, we did not find any significant difference in FMD measurements between preterm-born children and controls. This is consistent with similar studies in children42 and can possibly be explained by the fact that we enrolled healthy children of young age. Age-related endothelial dysfunction has been already demonstrated in previous studies in adults,43,44 whereas in our preterm-born group, a negative correlation between FMD and age was observed. Regular follow-up of the above population is needed in order to identify possible adverse FMD alterations that may become apparent in later life.
In contrast with FMD, the hyperemic peak velocity of the brachial artery differed significantly between preterm and full-term group in our study. Besides, CD31(+)/CD42b(−) EMPs were found to be independent predictors of hyperemic peak velocity of the brachial artery in preterm-born children. Hyperemic peak velocity, the maximal velocity of blood flow after cuff deflation, generates the brachial artery shear stress that is responsible for FMD.45 However, these two indices of brachial artery reactivity are mediated by different mechanisms,46 while hyperemic peak velocity better reflects microvascular dysfunction.45 Interestingly, hyperemic peak velocity was reported to be more strongly related to traditional cardiovascular risk factors than was FMD and also more sensitive to the early stages of atherosclerosis.47 Thus, the significantly lower hyperemic peak velocity of the brachial artery in preterm-born children of our study may indicate a dysregulation of microvascular function and an early stage of endothelial dysfunction, while EMPs levels might be helpful for identifying high-risk preterm-born individuals.
The independent associations between pulmonary hemodynamic parameters studied (mean pressure and velocity of pulmonary artery) and EMPs subpopulations may result from shear stress of pulmonary vessels, but also enhance the suggested role of EMPs in the pathophysiology of pulmonary hypertension,47,48 as well as the impact of prematurity on dysregulation of the cross-talk between microcirculation and macrocirculation in childhood.18 Moreover, the independent correlation between DBP and CD31(+)/CD42b(−) EMPs in our preterm-born children is possibly in line with the results of previous studies showing that DBP is an independent predictor of adverse cardiovascular events and contributes significantly to cardiovascular risk.49 Interestingly, in the original Framingham Heart Study (FHS),33 EMPs were significantly correlated with DBP but not with SBP, which is in concordance with our findings. Regarding the independent influence of being born SGA on CD31(+)/CD42b(−) EMPs in preterm-born children of our study, the interaction of fetal growth restriction and/or low birth weight with cardiovascular risk has been widely investigated.50 SGA has been emerged as a potential risk factor for endothelial function alterations and cardiovascular disease in later life.51
The limitations of our study are the following; first, our study population has an adequate number of preterm-born children in order to assure statistically significant results for primary outcomes, but a greater number would be more appropriate in order to reveal possible correlations between EMPs and neonatal morbidity related to prematurity, such as BPD, intraventricular hemorrhage, retinopathy of prematurity, etc. Secondly, the present study has a cross-sectional design, which does not allow determination of causal relationships.
In conclusion, circulating levels of EMPs are increased in prepubertal children born prematurely in comparison with their peers born at term. Whether assessment of circulating EMPs is warranted in individuals born prematurely, in clinical practice, as a complementary tool for non-invasive evaluation of endothelium and risk stratification, or as a target for novel therapeutic options, remains to be defined in future investigations.
References
Heindel, J. J. et al. Developmental origins of health and disease: integrating environmental influences. Endocrinology 156, 3416–3421 (2015).
Bavineni, M. et al. Mechanisms linking preterm birth to onset of cardiovascular disease later in adulthood. Eur. Heart J. 40, 1107–1112 (2019).
Bassareo, P. P., Namana, V., Fanos, V. & Mercuro, G. Preterm birth and risk of heart failure up to early adulthood. J. Am. Coll. Cardiol. 70, 1943–1944 (2017).
Carr, H., Cnattingius, S., Granath, F., Ludvigsson, J. F. & Edstedt Bonamy, A. K. Preterm birth and risk of heart failure up to early adulthood. J. Am. Coll. Cardiol. 69, 2634–2642 (2017).
Crump, C. et al. Association of preterm birth with risk of ischemic heart disease in adulthood. JAMA Pediatr. 179, 736–743 (2019).
Markopoulou, P., Papanikolaou, E., Analytis, A., Zoumakis, E. & Siahanidou, T. Preterm birth as a risk factor for metabolic syndrome and cardiovascular disease in adult life: a systematic review and meta-analysis. J. Pediatr. 210, 69–80 (2019).
de Jong, F., Monuteaux, M. C., van Elburg, R. M., Gillman, M. W. & Belfort, M. B. Systematic review and meta-analysis of preterm birth and later systolic blood pressure. Hypertension 59, 226–234 (2012).
Kajantie, E. et al. Insulin sensitivity and secretory response in adults born preterm: the Helsinki Study of Very Low Birth Weight Adults. J. Clin. Endocrinol. Metab. 100, 244–250 (2015).
Sipola-Leppänen, M. et al. Cardiometabolic risk factors in young adults who were born preterm. Am. J. Epidemiol. 181, 861–873 (2015).
Breukhoven, P. E., Kerkhof, G. F., Willemsen, R. H. & Hokken-Koelega, A. C. Fat mass and lipid profile in young adults born preterm. J. Clin. Endocrinol. Metab. 97, 1294–1302 (2012).
Hovi, P. et al. Intima-media thickness and flow-mediated dilatation in the Helsinki study of very low birth weight adults. Pediatrics 127, 304–311 (2011).
Lee, H., Dichtl, S., Mormanova, Z., Dalla Pozza, R. & Genzel-Boroviczeny, O. In adolescence, extreme prematurity is associated with significant changes in the microvasculature, elevated blood pressure and increased carotid intima-media thickness. Arch. Dis. Child. 99, 907–911 (2014).
Shimizu, T. et al. Abdominal aortic intima-media thickness in preschool children born preterm. Pediatr. Cardiol. 35, 121–125 (2014).
Mohlkert, L. A. et al. The preterm heart in childhood: left ventricular structure, geometry, and function assessed by echocardiography in 6-year-old survivors of periviable births. J. Am. Heart Assoc. 7, e007742 (2018).
Lewandowski, A. J. The preterm heart: a unique cardiomyopathy? Pediatr. Res. 85, 738–739 (2019).
Bassareo, P. P. et al. Reduced brachial flow-mediated vasodilation in young adult ex extremely low birth weight preterm: a condition predictive of increased cardiovascular risk? J. Matern. Fetal Neonatal Med. 23 (Suppl. 3), 121–124 (2010).
Cheung, Y. F., Wong, K. Y., Lam, B. C. & Tsoi, N. S. Relation of arterial stiffness with gestational age and birth weight. Arch. Dis. Child. 89, 217–221 (2004).
Wei, F. F. et al. Retinal and renal microvasculature in relation to central hemodynamics in 11-year-old children born preterm or at term. J. Am. Heart Assoc. 9, e014305 (2020).
Melville, J. M. & Moss, T. J. The immune consequences of preterm birth. Front. Neurosci. 7, 79 (2013).
Markopoulou, P. et al. Increased circulating endothelial progenitor cells (EPCs) in prepubertal children born prematurely: a possible link between prematurity and cardiovascular risk. Pediatr. Res. https://doi.org/10.1038/s41390-020-01190-y (2020).
Bertagnolli, M. et al. Endothelial colony-forming cells in young adults born preterm: a novel link between neonatal complications and adult risks for cardiovascular disease. J. Am. Heart Assoc. 7, e009720 (2018).
Dignat-George, F. & Boulanger, C. M. The many faces of endothelial microparticles. Arterioscler. Thromb. Vasc. Biol. 31, 27–33 (2011).
Agouni, A. et al. Endothelial dysfunction caused by circulating microparticles from patients with metabolic syndrome. Am. J. Pathol. 173, 1210–1219 (2008).
Tramontano, A. F. et al. Circulating endothelial microparticles in diabetes mellitus. Mediators Inflamm. 2010, 250476 (2010).
Bernal-Mizrachi, L. et al. High levels of circulating endothelial microparticles in patients with acute coronary syndromes. Am. Heart J. 145, 962–970 (2003).
Fenton, T. R. & Kim, J. H. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 13, 59 (2013).
Higgins, R. D. et al. Bronchopulmonary dysplasia: executive summary of a workshop. J. Pediatr. 197, 300–308 (2018).
Cutfield, W. S., Jefferies, C. A., Jackson, W. E., Robinson, E. M. & Hofman, P. L. Evaluation of HOMA and QUICKI as measures of insulin sensitivity in prepubertal children. Pediatr. Diabetes 4, 119–125 (2003).
Dalla Pozza, R. et al. Intima media thickness measurement in children: a statement from the Association for European Paediatric Cardiology (AEPC) Working Group on Cardiovascular Prevention endorsed by the Association for European Paediatric Cardiology. Atherosclerosis 238, 380–387 (2015).
Järvisalo, M. J. et al. Increased aortic intima-media thickness: a marker of preclinical atherosclerosis in high-risk children. Circulation 104, 2943–2947 (2001).
Thijssen, D. H. et al. Expert consensus and evidence-based recommendations for the assessment of flow-mediated dilation in humans. Eur. Heart J. 40, 2534–2547 (2019).
Lai, W. W. et al. Guidelines and standards for performance of a pediatric echocardiogram: a report from the Task Force of the Pediatric Council of the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 19, 1413–1430 (2006).
Amabile, N. et al. Association of circulating endothelial microparticles with cardiometabolic risk factors in the Framingham Heart Study. Eur. Heart J. 35, 2972–2979 (2014).
Bruyndonckx, L. et al. Endothelial progenitor cells and endothelial microparticles are independent predictors of endothelial function. J. Pediatr. 165, 300–305 (2014).
Deng, F., Wang, S. & Zhang, L. Endothelial microparticles act as novel diagnostic and therapeutic biomarkers of circulatory hypoxia-related diseases: a literature review. J. Cell Mol. Med. 21, 1698–1710 (2017).
Shebl, S. S. et al. Thrombo-hemorrhagic liability in children with congenital heart diseases. Hematol. Oncol. Stem Cell Ther. 11, 123–128 (2018).
Adly, A. A. et al. Vascular dysfunction in patients with young β-thalassemia: relation to cardiovascular complications and subclinical atherosclerosis. Clin. Appl Thromb. Hemost. 21, 733–744 (2015).
Ding, Y. Y. et al. Correlation between brachial artery flow-mediated dilation and endothelial microparticle levels for identifying endothelial dysfunction in children with Kawasaki disease. Pediatr. Res. 75, 453–458 (2014).
Dursun, I. et al. Circulating endothelial microparticles in children with Henoch-Schönlein purpura; preliminary results. Rheumatol. Int. 31, 1595–1600 (2011).
Narin, N. et al. Are endothelial microparticles early markers of pulmonary hypertension? Biomarkers 19, 319–325 (2014).
Boulanger, C. M. et al. Circulating microparticles from patients with myocardial infarction cause endothelial dysfunction. Circulation 104, 2649–2652 (2001).
Edwards, M. O. et al. Higher systolic blood pressure with normal vascular function measurements in preterm-born children. Acta Paediatr. 103, 904–912 (2014).
Witte, D. R. et al. Is the association between flow-mediated dilation and cardiovascular risk limited to low-risk populations? J. Am. Coll. Cardiol. 45, 1987–1993 (2005).
Seals, D. R., Jablonski, K. L. & Donato, A. J. Aging and vascular endothelial function in humans. Clin. Sci. (Lond.). 120, 357–375 (2011).
Wexler, O. et al. Brachial artery reactivity in patients with severe sepsis: an observational study. Crit. Care 16, R38 (2012).
Philpott, A. & Anderson, T. J. Reactive hyperemia and cardiovascular risk. Arterioscler Thromb. Vasc. Biol. 27, 2065–2067 (2007).
Lammi, M. R. et al. Microparticles in systemic sclerosis: potential pro-inflammatory mediators and pulmonary hypertension biomarkers. Respirology 24, 675–683 (2019).
Kosanovic, D. et al. Enhanced circulating levels of CD3 cells-derived extracellular vesicles in different forms of pulmonary hypertension. Pulm. Circ. 9, 2045894019864357 (2019).
Flint, A. C. et al. Effect of systolic and diastolic blood pressure on cardiovascular outcomes. N. Engl. J. Med. 381, 243–251 (2019).
Alexander, B. T., Dasinger, J. H. & Intapad, S. Fetal programming and cardiovascular pathology. Compr. Physiol. 5, 997–1025 (2015).
Skilton, M. R. et al. Fetal growth and preterm birth influence cardiovascular risk factors and arterial health in young adults: the Cardiovascular Risk in Young Finns Study. Arterioscler. Thromb. Vasc. Biol. 31, 2975–2981 (2011).
Acknowledgements
The authors are grateful towards all children and their parents participating voluntarily in the study.
Author information
Authors and Affiliations
Contributions
All the authors assisted with study design, acquisition, analysis and interpretation of the data; P.M. performed the clinical assessment; P.M. and E.P. were responsible for the flow cytometric analysis of circulating EMPs; P.G. was responsible for the ultrasound study of cIMT, aIMT, and FMD of the brachial artery; S.L. was responsible for cardiology data; and I.P. was responsible for blood biochemistry. T.S. supervised the study. P.M. developed the first draft of the manuscript and T.S. critically reviewed it. All the authors edited the manuscript, revised it critically for important intellectual content, and approved the final version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests
Consent statement
Informed written consent was obtained from parents and children.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Markopoulou, P., Papanikolaou, E., Loukopoulou, S. et al. Elevated circulating endothelial microparticles (EMPs) in prepubertal children born preterm. Pediatr Res 91, 1754–1761 (2022). https://doi.org/10.1038/s41390-021-01655-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01655-8
This article is cited by
-
Perfused boundary region as biomarker for endothelial integrity in former preterms in adolescence
Pediatric Research (2023)