Abstract
Background
States which reduce foetal oxygen delivery are associated with impaired intrauterine growth. Hypoxia results when barometric pressure falls with ascent to altitude, and with it the partial pressure of inspired oxygen (‘hypobaric hypoxia’). birthweight is reduced when native lowlanders gestate at such high altitude (HA)—an effect mitigated in native (millennia) HA populations. Studying HA populations offer a route to explore the mechanisms by which hypoxia impacts foetal growth.
Methods
Between February 2017 and January 2019, we prospectively studied 316 pregnant women, in Leh, Ladakh (altitude 3524 m, where oxygen partial pressure is reduced by 1/3) and 101 pregnant women living in Delhi (low altitude, 216 m above sea level).
Results
Of Ladakhi HA newborns, 14% were small for gestational age (<10th birthweight centile) vs 19% of newborn at low altitude. At HA, increased maternal body mass index, age, and uterine artery (UtA) diameter were positively associated with growth >10th weight centile.
Conclusions
This study showed that Ladakhi offspring birthweight is relatively spared from the expected adverse HA effects. Furthermore, maternal body composition and greater UtA size may be physiological HA adaptations and warrant further study, as they offer potential mechanisms to overcome hypoxia-related growth issues.
Impact
-
Reduced foetal oxygen delivery seen in native lowlanders who gestate at HA causes foetal growth restriction—an effect thought to be mitigated in native HA populations.
-
We found that greater maternal body mass and UtA diameter were associated with increased offspring birthweight in a (Ladakh) HA population.
-
This supports a role for them as physiological mediators of adaptation and provides insights into potential mechanisms that may treat hypoxia-related growth issues.
Similar content being viewed by others
Introduction
Birthweight is an important determinant of foetal and infant survival.1,2,3,4 Small newborns are particularly vulnerable to morbidity and mortality.5,6,7 Conditions which reduce foetal oxygen delivery (such as significant maternal cardiac disease) are associated with lower birthweight.8
Exploring the pathogenesis of this impact in disease states is difficult. One approach is to study otherwise healthy individuals exposed to the environmental hypoxia, which results from residency at high altitude (HA; ‘hypobaric hypoxia’), among whom birthweight is reduced by 100 g per 1000 m ascent beyond 1500 m.9,10,11,12 Such impacts are seen especially amongst native lowlanders. Native highland populations (historically exposed to hypobaric hypoxia for millennia) have undergone selection for advantageous genetic variants,13 and this might contribute to the partial mitigation of HH impacts on foetal growth seen in such populations, such as those in the Andes.14 Likewise, babies born to Tibetan women are <300 and <500 g heavier than those born to Han Chinese (native lowlander) women at 2700 and >3000 m, respectively.15
In this regard, a variety of advantageous phenotypes may have been selected for. The uterine artery (UtA) supplying blood to the growing pregnant womb increases in diameter as gestation advances.16 At 20 weeks gestation at altitude, UtA blood flow rises more in Andean than European native lowlanders,17 while third trimester UtA flow at HA is greater in Tibetans than Han Chinese.18,19 Increased UtA diameter and foetal birthweight in Andean women appears influenced by selection on the PRKAA1 gene, which encodes the alpha-1 catalytic subunit of adenosine monophosphate-activated protein kinase (AMPK), a central regulator of cellular energy metabolism.20
Foetal genotype influences birthweight at low altitude, independent of maternal genotype.21 However, selection pressure on such elements at HA remain little studied.
The Ladakhi people of the Indian Jammu and Kashmir regions represent an ancestral HA population, dwelling between the Karakoram and Himalayan mountain ranges at ≥3400 m. They share some elements of ancestral history with neighbouring Tibetans,22 but have been less extensively studied. The few papers investigating birthweights from this population are >15 years old23,24 and, while supporting the protective influence of Tibetan ancestry on birthweight, they failed to confirm the same protective effect on Ladakhi offspring. Wiley et al. reported mean birthweight of 168 Ladakhi babies to be 2764 g, but gestational age was not measured. Instead, fundal height and head circumference were used as proxies.23
We thus set out to perform a larger prospective observational study, in order to elucidate the effects of HA hypoxia on birthweight in a single native HA Ladakhi population. Specifically, we sought to:
-
(i)
Report the association of maternal and offspring anthropomorphic characteristics with birthweight impacts, and specifically that of increased UtA diameter.
-
(ii)
Collect biological samples to investigate genetic and metabolic mechanisms that might help explain the phenotypes identified.
Methods
Two linked prospective observational cohort studies were carried out. Pregnant women were recruited from Sonam Norboo Memorial (SNM) Hospital, Leh, Ladakh (the HA site, 3524 m) from the antenatal clinics and antenatal ultrasound departments over a 2-year period (Feb 2017–Jan 2019). Infants born at the All India Institute for Medical Sciences, New Delhi (216 m above sea level) were studied in parallel over a 1-year period (Jan 2018–December 2018). Ethical permissions were granted for the study from the Indian Health Ministry’s Screening Committee (HMSC) on the 7th September 2016, the Office of the Chief Medical Officer Leh (3rd August 2016), the All India Institute for Medical Sciences and the University College London research ethics committee (3634/002).
Pregnant women were eligible if they were aged over 18; not known to be genetically related to the father (first cousin or closer); having a singleton pregnancy; planning to deliver at the hospital; <28 weeks gestation using last menstrual period (LMP) and in whom an estimated due date (EDD) could be confirmed by ultrasound. Where LMP was uncertain or where there was a difference of >5 days by an appropriate early ultrasound, the ultrasound determined EDD was used. Excluded were those pregnancies with obvious foetal structural or chromosomal abnormalities.
Pregnant women completed a questionnaire documenting their dietary patterns (meat eater/vegetarian); and family, obstetric and medical histories (including smoking, alcohol, chronic medical problems and medications). Geographical ancestry was recorded with, where possible, birth locations for more than five generations. Blood pressure and anthropomorphic measures (height and weight pre-pregnancy and at attendance) were recorded using standard anthropometric techniques at the enrolment, booking appointment. UtA diameters were measured in longitudinal section at its crossover with the external iliac artery using transcutaneous ultrasound, between 18 and 24 weeks gestation17 by a single trained operator at each site (4-MHz curved linear array probe ALOKA Prosound, Hitachi Aloka. Medical Ltd, Chennai, India) in Leh and a VolusonTM E6 (GE Healthcare, Chicago, Illinois) in Delhi. The process was repeated bilaterally, and values of six readings (three per side) recorded. Colour imaging was not used, so as to avoid artefactual increases in UtA diameter. A second operator verified 10% of images and calculated average UtA diameters.
Information concerning the birth process (mode of delivery) and the neonatal characteristics (sex, weight, head circumference, crown-heel length and APGAR score) were recorded. Arterial transdermal oxygen saturation was recorded by pulse oximeter within first 15 min of birth from both a finger and toe with babies lying, resting and not crying and in the absence of supplemental oxygen delivery.
Deliveries were classified preterm, if <37 weeks gestation. All deliveries up to 42 weeks’ gestation were included in the analysis. Small for gestational age (SGA) infants were defined by a birthweight of <10th centile, according to the Intergrowth software package (https://intergrowth21.tghn.org).
Statistical analysis
Outcome measures were defined by cases—pregnancies affected by SGA vs controls (pregnancies with appropriately grown for gestational age (AGA) offspring). Analysis was first undertaken to compare maternal characteristics between SGA and AGA pregnancies in the HA and LA locations. Comparisons between HA and LA locations were also undertaken for the entire cohorts, and then stratified by SGA and AGA outcome.
Statistical analysis was performed using the STATA 16 package. Normality was confirmed through visual representation of birthweight distribution by histogram plot. Maternal baseline characteristics are reported as means [standard deviation, SD] unless otherwise stated. Unpaired t test were performed and reported for baseline characteristics between women who delivered AGA babies and those that delivered SGA babies.
Birthweight centiles and birthweight centile ratios were calculated using Intergrowth standards, as previously documented. Ponderal index was calculated as infant birthweight (g) × 100/birth length (cm)3. Logistic regression was used to identify factors contributing to the probability of SGA delivery in the HA population. Logistic regression results are reported as odds ratios with 95% confidence limits. Explanatory variables are assessed as significant at the 5% level. Univariable logistical analysis of maternal variables was first undertaken from the entire HA cohort. Maternal variables that retained significance in the first model were included in the final multivariable model to identify the association of UtA diameter and being an SGA case. Data were initially analysed by univariable logistic regression and those with the lowest P value used to generate the final multivariable model. Sensitivity analysis using forward stepwise regression confirmed the validity of this approach.
Sample size calculation
Sample size was calculated prior to commencement of the study using the STATA statistical software package. At 90% power with a 0.05 significance level, 184 subjects would allow for detection of a 300 g birthweight difference between SGA and AGA cases. This assumes a SD of 540 g, which is based on previous studies23,24 with a 3:1 AGA:SGA allocation (so recruitment of 46 SGA cases). A planned sample size of 300 HA residents was thus selected based on a predicted SGA case rate of 15% SGA pregnancies in Leh (supported by earlier audit data) equating to 45 SGA babies. For the logistic regression model, ten events (SGA outcomes) are required for each coefficient estimated, so 45 cases would allow for analysis of up to four coefficients in a final model.
Results
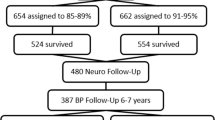
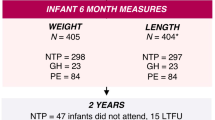
Overall, 316 pregnant women were recruited in Leh (HA), and 101 in Delhi (LA; 1 year due to later start of enrolment). Over the 2-year period, all women where gestational age could be ascertained and thought to be <28 weeks, were approached to be in the study. Maternal characteristics are presented in Table 1 and birthweight traits in Table 2.
In Leh, >96% of women considered themselves of Ladakhi descent (with a five generation or more documented history of living at altitude), while ten (3.2%) described themselves as Tibetan. Birthweight was greatest in the Tibetan ancestry group (3.62 kg) vs Ladakhi (3.14 kg), p 0.0009.
Of AIIMS participants, the majority of women had lived in Delhi for >5 years, but more than half came originally from outside of Delhi area. Overall, 94/101 (93.1%) described themselves as Indoaryan ethnicity, 2 as IndoEuropean and 5 as Dravidian.
Characteristics of HA women who delivered SGA vs AGA babies were similar. Maternal ethnicity, parity, smoking status (no subjects disclosed being a smoker at HA), chronic illness and socio-economic (as evidenced through maternal education, occupation, income and educational status) did not differ (Table 1). No significant maternal illness was reported in either group (hypothyroidism was reported in both groups). At HA, maternal BMI (AGA 24.1 vs SGA 22.3 kg/m2, p = 0.002) and age (AGA 27.2 vs SGA 26.5 years, p = 0.03) differed. Compared to women who delivered an AGA baby, those who delivered an SGA baby were statistically older and lighter.
Baseline maternal characteristics of women who delivered at LA revealed a similar pattern. Ethnicity, parity, age and smoking (one woman with an SGA pregnancy reported current smoking) were not found to be different between groups. Maternal BMI was different between groups (AGA 23.4 vs SGA 21.1 kg/m2 [p = 0.03]). Hypothyroidism was reported once in each group with one report of maternal hypertension in the SGA group.
Of the 316 HA women, UtA data were obtained in 221 (69.9%). Missing UtA data were due to the sonologist not being available to scan (n = 29), women being outside of 18–24-week gestation period (n = 34) or if the blinded analysis disagreed (n = 32). Data were not used where the second operator disagreed on blinded analysis by >0.1 cm.
At HA, mean UtA diameter was 56.5 [10.7] mm in AGA pregnancies vs 51.5 [9.3] mm in SGA pregnancies (p = 0.009). Birthweights in the 187 AGA neonates where UtA data were available were similar to that in the overall cohort recruited (3.23 kg). SGA pregnancies with UtA data reported (n = 34) were also found to have similar birthweight (2.51 kg) to overall study population (2.52 kg in total SGA cohort), and SGA was reported at a similar rate (15%). In the SGA group, there was no statistical difference in birthweight between those with UtA measurements (2.51 kg) and those without (2.54 kg), p = 0.69.
Univariable logistical regression analysis of maternal characteristics between AGA and SGA babies at HA revealed body mass index (BMI) and age to be significantly different between groups. Therefore, a final multivariable logistical regression model was run incorporating maternal BMI, age and UtA diameter in babies born AGA vs SGA at HA. Maternal UtA diameter remained statistically different between women who had an SGA baby vs those who had an AGA baby (OR 1.06, p = 0.0001) with increased maternal UtA positively associated with having an AGA baby (Table 3).
UtA diameter was statistically smaller in the LA group vs HA groups 47.3 [4.65] vs 55.5 [11.2] mm, respectively, p = 0.0001). In LA babies, UtA diameter was appropriately recorded in 61 (60.3%). In this group, the average birthweight was 2.99 kg in AGA pregnancies (n = 47) and 2.43 kg (n = 14) in SGA pregnancies. There was no difference in size in the UtA diameter between AGA and SGA pregnancies (47.2 [4.9] vs 47.2 [4] mm, p = 0.97) in the LA cohort.
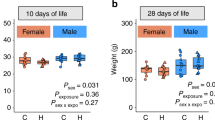
Neonatal data for HA and LA sites are presented in Table 2. At HA, the mean birthweight was 3.15 [0.44] kg, and 44 infants (14%) were classified as SGA (mean birthweight 2.52 [0.26] kg). SGA babies were significantly lighter than AGA babies 3.25 [0.39], p = 0.00001. Mean gestational age (days) did not differ between AGA and SGA babies (275.3 vs 277.4 days, respectively, p = 0.21). Mean birth length at HA was 49.9 [2.6] cm with SGA babies being significantly shorter 47.5 [2.4] cm vs AGA babies 50.3 [0.15] cm, p = 0.0001.
The mean birthweight in the LA cohort was 2.89 [0.4] kg, significantly less than the HA cohort (p = 0.0001) with 19 (19%) infants identified as SGA (mean 2.43 [0.22] kg). Birth length was 48.1 [1.7] cm and SGA babies were again shorter at 47.1 [1.44] vs AGA babies 48.3 [0.19] cm, p = 0.0067. Babies were born earlier than HA counterparts (268.7 [8.7] vs 275.6 [10.4] days, p = 0.0001). No significant difference was noted between gestational age that AGA vs SGA babies born (268.8 [8.9] vs SGA 269 [8] days, p = 0.91).
Birthweight was greater in male vs female babies at both locations. Males at HA were heavier than females weighing 3.21 [0.45] kg vs females at 3.1 [0.45] kg, p = 0.03. At LA, male vs female weight difference was not found to be statistically significant (p = 0.19). Male/female numbers were similar at both HA and LA sites (HA male sex 45% vs LA 46%). Overall babies born at HA of Ladakhi descent were heavier (3.15 vs 2.89 kg, p = 0.0001 and longer (49.9 vs 48.1 mm, p = 0.0001) than their LA counterparts. Comparing just SGA pregnancies at HA and LA, significant differences between birthweights and length were not maintained.
At birth, there was no statistically significant difference between baby APGAR scores at 1 min between HA 8.26 [1.17] vs LA 8.47 [1.45], p = 0.11 (Table 2). At HA, APGARs at 1 min for SGA babies were 8 [1.26] vs AGA babies 8.3 [1.15], p = 0.21). SaO2 shortly after birth was lower at HA than LA (88.9 [8.32]% vs 92.5 [13.2]%, respectively), p = 0.005. SaO2 did not differ between SGA and AGA babies at HA (88.7%), but initial SaO2 was higher in AGA than SGA babies born at LA (93.1 [13]% vs 88.7 [8.49]%, p = 0.39), respectively, although not reaching significance.
Discussion
We performed a comprehensive prospective study of a HA native population in relation to reproductive outcomes and compared this with a LA non-native population.
Individuals gestated and born at HA had a significantly higher birthweight than expected for an Indian population. The only other published study specifically of birthweight in the Ladakhi population reported significantly lower birthweights than those recorded in this study, as well as shorter birth lengths with a much higher rate of low birthweight <2500 g (27% vs 7.8%).23 It is difficult to know the exact reason for this disparity. The previous study is >25 years old and tourism in the region has had a significant impact during this time, potentially altering parental diet and lifestyle. The sample size in our study is twice as large and was performed over a much longer time frame, and may better represent the population especially given that almost all eligible pregnant women consented to be in the study.
Birthweights in Ladakhi subjects were on average 3.15 kg, up to a maximum birthweight of 4.4 kg. Within this population, those individuals who identified as Tibetan still showed the greatest adaptation with an average birthweight of 3.62 kg. These figures correspond to other adapted high-altitude populations. A retrospective review of a cohort of South American birthweights revealed an average birthweight for HA Andean (longest adapted) subjects of 3.15 kg (n = 728), compared with their European (shortest) counterparts at HA at 2.96 kg (n = 167).9
Our data also support the idea that rates of poor foetal growth (as defined by Intergrowth reference standards) were lower than expected in the Ladakh population with significantly lower rates than documented by the recent Indian National family health survey 4 2015–2016 (https://dhsprogram.com/pubs/pdf/FR339/FR339.pdf) for term low birthweight (LBW) individuals of 16.6% (vs 7.8% in our Leh population). The proportion of babies defined as SGA (according to birthweight centile) at HA (14%) was lower than at LA (19%). Birthweight centiles take into account gestational age and this finding suggests adaptation in HA cohort is not purely a result of gestational age differences.
The differences seen in adaptation are driven by the appropriately grown individuals at HA. These infants are both heavier and longer than their counterparts born at low altitude, but this growth sparring effect is lost in infants born smaller than their expected weight with their birth length and ponderal index being equivalent whether at high or low altitude. This suggests that intrinsic mechanisms that influence body size and composition may have a role to play in positive adaptation at HA.
From this study, increased maternal BMI and decreased age associated with birthweight offspring at HA. This is consistent with recognised maternal traits that associate with appropriate birthweight25, but other classically recognised risk factors for low birthweight do not appear to be significant in this HA cohort,26 which is of interest given the concurrence with the neonatal anthropomorphic findings described above. The absence of retained significance in the multivariable model along of other classic risk factors for low birthweight in this HA population is in keeping with earlier HA work from Colorado that associated HA as an independent risk factor influencing birthweight.10 A major limitation of this study was the absence of a comparative native low-altitude population. For practical reasons, this was not possible, but by studying the LA Delhi population in the same detailed way as at HA, we were able to eliminate many recognised factors, leaving ancestry traits as a plausible mediator of the birthweight protection afforded to this population.
Maternal UtA diameter in the second trimester was strongly associated with birthweight in HA subjects. Women who went on to have AGA babies had larger UtA diameters at 18–24 weeks than women who went on to have a pregnancy complicated by SGA. This finding is independent of foetal sex differences. Similar UtA adaptation was not identified in a group of pregnant women at low altitude. UtA diameters were smaller and no difference was identified between women who had a pregnancy with either an AGA or SGA foetus. This supports the suggestion that one of the mechanisms through which HA adaptation maybe presenting in pregnancy is in early modulation of UtA diameter, enhancing blood flow and thereby oxygen, to the developing placenta and foetus. In a separate cohort of high-altitude pregnancies studied, UtA blood flow was markedly greater at both weeks 20 and 36 of pregnancy in Andean vs European women, with such differences shown to be due to greater UtA diameters, not flow velocity.27
Animal studies of the mechanisms underpinning UtA vasodilation supports a role for the metabolic sensor, AMPK. AMPK was found to be present in utero-placental tissue and influenced vasodilation in the presence of chronic hypoxia28, and its activation implicated in myometrial artery vasodilation in appropriate for gestational age human pregnancies at altitude in Colorado.29 Furthermore, pharmacological activation of AMPK in a murine model has been shown to partially present hypoxia-induced foetal growth restriction.30 Peroxisome proliferator-activated receptor gamma (PPAR γ) has also been postulated to protect against hypoxia-associated growth restriction with lower levels of expression in human growth restricted pregnancies compared with controls.31 Recently, using a murine model of hypoxia-induced growth restriction, it was shown that exposure to a PPAR γ agonist was able to reverse induced vasoconstriction of uterine arteries with increased sensitivity of response in the hypoxic vs normoxic dams30,32, which mimics our human physiological findings.
Given that gene variants in PRKAA1 (a subunit of AMPK) and PPAR γ expression differences associate with both birthweight and maternal UtA diameter, physiological mechanisms through which they may be acting warrant further investigation as they offer the potential to overcome hypoxia-related growth issues.
Conclusion
In the Ladakhi population, HA adaptation is represented through enhanced birthweight protection seen by lower than expected rates of SGA. Adaptation in pregnancy may be mediated through increased UtA diameter with resultant improved oxygenation to the placenta and foetus.
References
Barker, D. J., Osmond, C., Forsen, T. J., Kajantie, E. & Eriksson, J. G. Trajectories of growth among children who have coronary events as adults. N. Engl. J. Med. 353, 1802–1809 (2005).
Costantine, M. M. et al. Population versus customized fetal growth norms and adverse outcomes in an intrapartum cohort. Am. J. Perinatol. 30, 335–341 (2013).
Kajantie, E. et al. Size at birth as a predictor of mortality in adulthood: a follow-up of 350 000 person-years. Int. J. Epidemiol. 34, 655–663 (2005).
McIntire, D. D., Bloom, S. L., Casey, B. M. & Leveno, K. J. Birth weight in relation to morbidity and mortality among newborn infants. N. Engl. J. Med. 340, 1234–1238 (1999).
Ludvigsson, J. F., Lu, D., Hammarstrom, L., Cnattingius, S. & Fang, F. Small for gestational age and risk of childhood mortality: a Swedish population study. PLoS Med. 15, e1002717 (2018).
Hales, C. N. et al. Fetal and infant growth and impaired glucose tolerance at age 64. BMJ 303, 1019–1022 (1991).
Gilbert, W. M. & Danielsen, B. Pregnancy outcomes associated with intrauterine growth restriction. Am. J. Obstet. Gynecol. 188, 1596–1599 (2003). discussion 9-601.
Presbitero, P. et al. Pregnancy in cyanotic congenital heart disease. Outcome of mother and fetus. Circulation. 89, 2673–2676 (1994).
Soria, R., Julian, C. G., Vargas, E., Moore, L. G. & Giussani, D. A. Graduated effects of high-altitude hypoxia and highland ancestry on birth size. Pediatr. Res. 74, 633–638 (2013).
Jensen, G. M. & Moore, L. G. The effect of high altitude and other risk factors on birthweight: independent or interactive effects? Am. J. Public Health 87, 1003–1007 (1997).
Tissot van Patot, M. C. et al. Human placental metabolic adaptation to chronic hypoxia, high altitude: hypoxic preconditioning. Am. J. Physiol. Regul. Integr. Comp. Physiol. 298, R166–R172 (2010).
Bailey, B. A., Donnelly, M., Bol, K., Moore, L. G. & Julian, C. G. High Altitude Continues to Reduce Birth Weights in Colorado. Matern Child Health J. 23, 1573–1580 (2019).
Julian, C. G. & Moore, L. G. Human genetic adaptation to high altitude: evidence from the andes. Genes (Basel). 10, 150 (2019).
Haas, J. D., Stepcik, C., Beard, J. & Hurtado, L. Altitude, ethnic and sex differences in birth weight and length in Bolivia. Hum. Biol. 52, 459–477 (1980).
Moore, L. G., Young, D., McCullough, R. E., Droma, T. & Zamudio, S. Tibetan protection from intrauterine growth restriction (IUGR) and reproductive loss at high altitude. Am. J. Hum. Biol. 13, 635–644 (2001).
Palmer, S. K. et al. Quantitative estimation of human uterine artery blood flow and pelvic blood flow redistribution in pregnancy. Obstet. Gynecol. 80, 1000–1006 (1992).
Julian, C. G. et al. Augmented uterine artery blood flow and oxygen delivery protect Andeans from altitude-associated reductions in fetal growth. Am. J. Physiol. Regul. Integr. Comp. Physiol. 296, R1564–R1575 (2009).
Moore, L. G., Zamudio, S., Zhuang, J., Sun, S. & Droma, T. Oxygen transport in tibetan women during pregnancy at 3,658 m. Am J Phys Anthropol. 114, 114 42–53 (2001).
Chen, D., Zhou, X., Zhu, Y., Zhu, T. & Wang, J. Comparison study on uterine and umbilical artery blood flow during pregnancy at high altitude and at low altitude. Zhonghua Fu Chan Ke Za Zhi. 37, 69–71 (2002).
Bigham, A. W. et al. Maternal PRKAA1 and EDNRA genotypes are associated with birth weight, and PRKAA1 with uterine artery diameter and metabolic homeostasis at high altitude. Physiol. Genomics. 46, 687–697 (2014).
Hughes, A. E. et al. Fetal genotype and maternal glucose have independent and additive effects on birth weight. Diabetes 67, 1024–1029 (2018).
Rowold, D. J. et al. Ladakh, India: the land of high passes and genetic heterogeneity reveals a confluence of migrations. Eur. J. Hum. Genet. 24, 442–449 (2016).
Wiley, A. S. Neonatal and maternal anthropometric characteristics in a high altitude population of the western Himalaya. Am. J. Hum. Biol. 6, 499–510 (1994).
Tripathy, V. & Gupta, R. Birth weight among Tibetans at different altitudes in India: are Tibetans better protected from IUGR? Am. J. Hum. Biol. 17, 442–450 (2005).
McCowan, L. & Horgan, R. P. Risk factors for small for gestational age infants. Best. Pract. Res Clin. Obstet. Gynaecol. 23, 779–793 (2009).
McCowan, L. M., Figueras, F. & Anderson, N. H. Evidence-based national guidelines for the management of suspected fetal growth restriction: comparison, consensus, and controversy. Am. J. Obstet. Gynecol. 218, S855–S68. (2018).
Browne, V. A. et al. High-end arteriolar resistance limits uterine artery blood flow and restricts fetal growth in preeclampsia and gestational hypertension at high altitude. Am J Physiol Regul Integr Comp Physiol. 300, R1221-9 (2011).
Skeffington, K. L. et al. Hypoxia, AMPK activation and uterine artery vasoreactivity. J. Physiol. 594, 1357–1369 (2016).
Lorca, R. A. et al. AMPK activation in pregnant human myometrial arteries from high-altitude and intrauterine growth-restricted pregnancies. Am. J. Physiol. Heart Circ. Physiol. 319, H203–H212 (2020).
Lane, S. L. et al. AMP-activated protein kinase activator AICAR attenuates hypoxia-induced murine fetal growth restriction in part by improving uterine artery blood flow. J. Physiol. 598, 4093–4105 (2020).
Diaz, M. et al. Placental expression of peroxisome proliferator-activated receptor gamma (PPARgamma): relation to placental and fetal growth. J. Clin. Endocrinol. Metab. 97, E1468–E1472 (2012).
Lane, S. L. et al. Peroxisome proliferator-activated receptor gamma blunts endothelin-1-mediated contraction of the uterine artery in a murine model of high-altitude pregnancy. FASEB J. 34, 4283–92. (2020).
Acknowledgements
Financial support for this study was received from the Wellcome Trust (UK) through a SEED award to S.L.H. Initial travel expenses were provided by a University College London Global Health Challenges award and the Eden Travelling Fellowship from the Royal College Obstetrician and Gynaecologists. H.E.M. is supported by the UK National Institute for Health Research, through University College London Hospitals’ Comprehensive Biomedical Research Centre.
Author information
Authors and Affiliations
Contributions
H.E.M. helped to conceive the study with input from D.K., S.L.H. and D.J.W. S.L.H. obtained Wellcome Trust funding for the project and with D.K. identified the collaborating team in Sonam Norboo Memorial Hospital, Leh. P.D. led the team in Leh and, with the help of S.L.H. set up and ran the study for its duration. P.T.A. performed ultrasound scan, receiving training from S.L.H. V.D. scanned obstetric patients in AIIMS and V.J. acted as the local principal investigator in this site. S.L.H., P.D. and V.J. checked and verified data acquired, and performed data analysis. S.L.H. and H.E.M. prepared the text of the manuscript, and other authors contributed and reviewed.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
All patients provided written consent to be included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dolma, P., Angchuk, P.T., Jain, V. et al. High-altitude population neonatal and maternal phenotypes associated with birthweight protection. Pediatr Res 91, 137–142 (2022). https://doi.org/10.1038/s41390-021-01593-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01593-5
This article is cited by
-
Cold-inducible RNA binding protein alleviates iron overload-induced neural ferroptosis under perinatal hypoxia insult
Cell Death & Differentiation (2024)
-
Genotyped indigenous Kiwcha adults at high altitude are lighter and shorter than their low altitude counterparts
Journal of Physiological Anthropology (2022)