Abstract
Background
We aimed to compare the ten different scores (by Kobayashi, Egami, Harada, Formosa, Sano, Piram et al., Wu et al., Yang et al., Tan et al., and Kanai et al.) to assess their performance in predicting IVIG resistance in Turkish children.
Methods
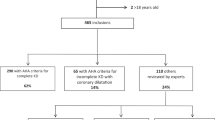
Complete and incomplete KD patients diagnosed with KD at Hacettepe University between June 2007 and September 2019 were evaluated retrospectively.
Results
A total of 129 patients, 79 boys (61.2%), with a median age 36 (IQR 19.5–57.0) months were evaluated. Sixteen patients (12.4%) had IVIG resistance. Sensitivity was low for all the ten scores. Tan, Sano, and Egami predictive models had the highest specificity (97.3, 89.4, 86.7%, respectively). Almost all scoring systems distinguished the group of patients with low risk for IVIG resistance but could not differentiate IVIG-resistant patients. Multivariate analysis for the laboratory features showed that platelet count <300 × 109/L and GGT serum levels were independent risk factors for IVIG resistance (OR: 3.896; 95% CI: 1.054–14.404; p = 0.042 and OR: 1.008; 95% CI: 1.001–1.015; p = 0.050).
Conclusions
The current scoring systems had a low sensitivity for predicting the risk for IVIG resistance in Turkish children. On the other hand, increased serum GGT levels and low platelet count were risk factors for predicting IVIG resistance.
Impact
-
Intravenous immunoglobulin (IVIG) resistance may be observed in 10–20% of patients diagnosed with Kawasaki disease.
-
Coronary artery involvement is more frequent in IVIG-resistant patients.
-
It is important to predict the patients who might develop IVIG resistance to improve prognosis.
-
The performance of the IVIG resistance predictive models in Kawasaki disease in our population is limited due to the low sensitivity.
Similar content being viewed by others
Introduction
Kawasaki disease (KD) is an acute systemic vasculitis predominantly affecting medium-sized vessels, mainly the coronary arteries.1 The incidence of disease varies between countries but is more common in East Asian countries, such as Japan, Korea, and Taiwan.2 There are no epidemiologic studies on the incidence of KD in Turkey. We only know that it constitutes about 9% of the childhood vasculitis.3 Coronary artery lesions are the most important complication of the disease. Intravenous immunoglobulin (IVIG) treatment within the first 10 days of disease significantly reduces the prevalence of coronary artery involvement.4,5 While 25% of the untreated patients develop coronary artery abnormalities, this rate decreases to 3–5% in patients who had early treatment.6 However, 10–20% of the KD patients are resistant to IVIG treatment.7 The definition of IVIG resistance is persistent or recurring fever at least 36 h after the end of the IVIG infusion.4,8 These patients require second-line therapy with a repeated dose of IVIG and/or corticosteroids, infliximab, or other biologics.9 Coronary artery involvement is higher in IVIG-resistant patients compared to IVIG-responsive patients.10 It is important to predict the patients who might develop IVIG resistance to improve prognosis.
In order to detect the risk factors of IVIG resistance, a number of predictive models including clinical and laboratory parameters of patients have been identified, such as Kobayashi, Egami, Sano scoring systems from Japan and Formosa scoring system from Taiwan. Sensitivity and specificity of scores may differ between populations. Do et al. reported that positive Kobayashi score could be used to identify high-risk population for IVIG resistance in Korean patients with KD.11 Davies et al. reported that Kobayashi score had a low sensitivity for predicting IVIG resistance in British population.12 A predicted model may not be sensitive or specific enough when performed in other ethnic groups. In our study, we aimed to evaluate and compare ten different risk scores to predict IVIG resistance in Turkish children. We also identified the predictors of IVIG resistance in our population.
Method
This study included retrospective analysis of 129 patients diagnosed with KD at the Hacettepe University Children’s Hospital between June 2007 and September 2019. Diagnosis of KD was based on the criteria of the American Heart Association (AHA)4: the presence of fever for at least 5 days accompanied by the presence of at least 4 of the following 5 findings: bilateral non-exudative conjunctival injection, unilateral cervical lymphadenopathy (LAP), changes in the lips and oral cavity, skin rash, and changes in extremities, including indurative angioedema and desquamation. Incomplete KD was diagnosed in the presence of unexplained prolonged fever, two or three diagnostic criteria, and supporting compatible laboratory or echocardiogram findings.4 Patients who had complete or incomplete KD were included in the study. Classification of the coronary abnormalities was performed according to the AHA guideline.4 Demographic and clinical features of patients, including sex, age, presence of symptoms, duration of fever, time until diagnosis, response to IVIG therapy, additional treatment in case of IVIG resistance, and coronary artery status, were recorded. Laboratory parameters, including hemoglobin, hematocrit, white blood cell count, number and percentage of neutrophils and lymphocytes, platelet count, mean platelet volume, alanine aminotransferase (ALT), aspartate aminotransferase (AST), total bilirubin (TB), direct bilirubin (DB), γ-glutamyl transferase (GGT), electrolytes, brain natriuretic peptide (BNP), lactic dehydrogenase (LDH), albumin, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and urine analyses, were noted prior to IVIG treatment.
The following IVIG resistance risk scores were evaluated: Kobayashi, Egami, Harada, Sano, and Kanai scoring systems from Japan10,13,14,15,16; Formosa scoring system from Taiwan17; three different scores from China18,19,20; and a scoring system for non-Asian populations21 (Table 1). Their sensitivity and specificity to predict IVIG resistance in our population were investigated. Also, the effectiveness of mean platelet volume-to-lymphocyte ratio in predicting coronary artery involvement reported by Bozlu et al. was assessed.22 A lower mean platelet volume-to-lymphocyte ratio (≤2.5) was associated with coronary artery involvement in their study. This study has been approved by Hacettepe University Ethics Commission (Approval number: GO 20/568).
Statistical analysis
Descriptive statistics were presented as frequency, percentage, mean, standard deviation (SD), median, and interquartile range (IQR). Shapiro–Wilk test, histograms, and Q-Q graphics were used for evaluation of normality of distribution. Fisher’s Exact Test was used in the analysis of relationships between categorical variables. For the comparison of continuous variables, Student’s t test was used with variables that showed normal distribution, while Mann–Whitney U test was used in those with non-normal distribution. Sensitivity and specificity of scores were calculated by generating 2 × 2 tables. receiver operating characteristic (ROC) curves and the area under the curves (AUCs) were computed to evaluate the performance of the predictive models in predicting IVIG resistance.
Univariate and multivariate logistic regression analyses were applied to identify risk factors for IVIG resistance in KD and to determine the independent risk factors. Odds ratios (ORs) were calculated with 95% confidence intervals (CIs). Statistical analyses were performed by using the SPSS version 20.0 package program. p Values of <0.05 were accepted to show statistical significance.
Results
A total of 129 patients, 79 boys (61.2%), with a median age 36 (IQR 19.5–57.0) months were included in the study. All people in Turkey are white Caucasian but have different ethnicities. The majority are Turkish but we have Kurds, Albanians, Laz people, etc. We are not able to comment on the ethnicity of the children in our study population. Sixty-nine patients (53.5%) were diagnosed in spring and winter. Complete KD was diagnosed in 87 patients (67.4%). All patients had fever and the median duration of fever was 7.0 (IQR 5–10) days. The frequency of other disease criteria were as follows: changes in the lips and oral cavity in 108 (83.7%), changes in extremities in 106 (82.2%), conjunctival injection in 104 (80.6%), skin rash in 100 (77.5%), and cervical LAP in 91 (70.5%) patients. The median time to the diagnosis following the onset of symptoms was 7 (IQR 5–10.5) days, which was significantly longer in patients with incomplete KD (p = 0.01).
The number of patients with IVIG resistance was 16 (12.4%). While cervical LAP, changes in extremities, and oral mucosal changes were more common in the patients with IVIG resistance, skin rash and conjunctival injection were more frequent in IVIG-responsive group. However, these differences did not reach statistical significance (p > 0.05; Table 2). Second-line therapy for IVIG-resistant group were as follows: second dose IVIG in 3 (18.7%), corticosteroids in 7 (43.7%), both corticosteroid and second dose IVIG in 6 patients (37.5%), and additional infliximab therapy in 1 patient (6.2%).
Ten different risk scores for IVIG resistance were calculated and their sensitivity and specificity were evaluated (Table 3). Yang score had the highest sensitivity (50%) among all scores while the sensitivity of others were all <50%. The Tan predictive model had the highest specificity, and the specificity of the other scores ranged from 51.3 to 89.4%. Yang score had the highest AUC (0.600), but the differences between scores were not statistically significant (p = 0.17; Table 3).
Compared with the IVIG-responsive group, the IVIG-resistant group had higher serum AST, GGT, TB, DB, and LDH levels; lower serum calcium levels; and a higher frequency of sterile pyuria (Table 2). The risk factors for IVIG resistance were evaluated by univariate analysis. High serum levels of TB, ALT, AST, GGT, and platelet count <300 × 109/L were associated with developing IVIG resistance (OR: 1.697; 95% CI: 1.070–2.692; p = 0.025, OR: 1,004; 95% CI: 1.001–1.008; p = 0.026, OR: 1.006; 95% CI: 1.000–1.012; p = 0.042, OR: 1.008; 95% CI: 1.001–1.015; p = 0.017, and OR: 3.708; 95% CI: 1.261–10.906; p = 0.017, respectively). On the other hand; younger age and high CRP levels were not risk factors (Table 4).
Five risk factors that were significant in the univariate analysis were re-evaluated with multivariate analysis; platelet count <300 × 109/L and GGT serum levels were independent risk factors for IVIG resistance (OR: 3.896; 95% CI: 1.054–14.404; p = 0.042 and OR: 1.008; 95% CI: 1.001–1.015; p = 0.050; Table 5).
Coronary artery involvement was detected in 44 of the 129 patients (34.1%). There were coronary artery dilatations (Z score 2–<2.5) in 14 patients (10.8%), small aneurysm (Z score ≥2.5–<5) in 18 patients (13.9%), medium aneurysm (Z score ≥5–<10 and absolute dimension <8 mm) in 7 patients (5.4%), and giant aneurysm (Z score ≥10 or absolute dimension ≥8 mm) in 5 patients (3.8%). Patients with extremity changes had more common coronary artery involvement (p = 0.04). We observed a significant association with young age, male sex, high levels of white blood cell count, high lymphocyte count, high lymphocyte percentage, low mean platelet volume-to-lymphocyte ratio (p = 0.01, p = 0.02, p = 0.04, p = 0.002, p = 0.009, p = 0.002, respectively), and coronary abnormalities. In univariate analysis, male sex, age under 1 year, changes in extremities, high lymphocyte counts, and low mean platelet volume-to-lymphocyte ratio (≤2.5) were associated with coronary involvement (OR: 0.393; 95% CI: 0.176–0.879; p = 0.023, OR: 3.873; 95% CI: 1.303–11.507; p = 0.015, OR: 2.523; 95% CI: 1.008–6.313; p = 0.048, OR: 1.239; 95% CI: 1.046–1.467; p = 0.013, and OR: 2.779; 95% CI: 1.228–6.289; p = 0.014, respectively) while duration of fever, IVIG resistance, incomplete form of disease, white blood cell count, ESR, and CRP did not reach significance (Table 4). The multivariate analysis identified young age (<1 year of age) and male sex as independent risk factors for coronary involvement (OR: 4.534; 95% CI: 1.227–16.758; p = 0.023 and OR: 0.372; 95% CI: 0.144–0.959; p = 0.041, respectively; Table 5).
Discussion
In our study, IVIG resistance was present in 12.4% of patients. This rate varies between 11 and 26% in different countries.23,24,25 Genetic and immunological predisposition might have an impact on the development of IVIG resistance. Identifying high risk factors for IVIG resistance would play an important crucial role in KD treatment. In addition to scoring systems such as the Kobayashi, Harada, and Egami scores, new prediction models have been developed in recent years to assess the risk of IVIG resistance.18,19,20
We compared the performance of ten different score models predicting IVIG resistance. The sensitivity in all scoring systems were ≤50% while specificity values were acceptable. Tan, Sano, and Egami scores had the highest specificity (97.3%, 89.4%, and 86.7%, respectively) in our population. Tan et al. had excluded incomplete KD patients, but we found that the predictive model still had high specificity despite the inclusion of incomplete KD patients to our study.20 Sleeper et al. performed the Japanese IVIG risk scores (Kobayashi, Egami, and Sano risk scores) in the North American cohort and found low sensitivity and good specificity, as in our study.26 Tremoulet et al. evaluated the performance of Egami score in 362 children with KD in San Diego county and found low sensitivity (38.3%) and good specificity (83.8%) as well.7 Existing scoring systems distinguished the group of patients with low risk for IVIG resistance but could not differentiate patients who might need second-line treatment and require closer observation. Therefore, for predicting IVIG resistance, centers could use one or more of these scoring systems. However, they should be aware of the low sensitivity for all these scoring systems in Turkish patients. We suggest that platelet counts and GGT levels could help predicting IVIG resistance in KD patients.
The difference in the incidence of IVIG resistance among populations may also be related to genetic and immunological factors.7,27 Although we expected the non-Asian 2020 score suggested by Piram et al. to perform better in our eastern Mediterranean population, this was not the case.
The association between clinical parameters and IVIG resistance varies among KD patients in different ethnic groups and regions. A meta-analysis of 28 studies comprising 4442 IVIG-resistant and 21,818 IVIG-responsive KD patients showed that patients with cervical LAP, swelling of the extremities, polymorphous rash, oral mucosa alterations, and taking IVIG treatment within the first 4 days of symptoms were associated with IVIG resistance.28 However, there was no significant association between clinical symptoms and IVIG resistance in our study.
The IVIG-resistant group had increased serum AST, GGT, TB, DB, and LDH levels; decreased serum calcium levels; and increased frequency of sterile pyuria compared to the IVIG-responsive patients (Table 2). Platelet count <300 × 109/L and increased GGT serum levels were detected as independent predictors for IVIG resistance (Table 5). Previous studies have confirmed the association between IVIG resistance and GGT.7,29,30 It is hypothesized that changes in GGT levels can contribute to IVIG resistance by blocking IVIG-induced neutrophil apoptosis.29
Low platelet count was used as a parameter predicting IVIG resistance in Kobayashi, Egami, and Tan scoring systems. Chantasiriwan et al. reported low platelet count as an IVIG resistance risk factor, as well.31 In a study evaluating 5151 KD patients in Korea, high serum N-terminal pro-BNP, CRP, AST, and ALT levels were associated with IVIG resistance.32 In our previous study, we also reported increased GGT serum levels as an independent predictor for IVIG resistance.30
KD is the leading cause of acquired heart disease in children in developed countries.4 The previous studies reported the rate of coronary artery involvement around 15–20%, whereas it was 34.1% in our study.33,34 On the other hand, the incidence of coronary artery involvement has been reported as approximately 25–33%, and the rate of IVIG resistance was noted as 3–15% in studies from Turkey.35,36 Increased incidence of coronary artery involvement despite low IVIG resistance may be due to the genetic or environmental factors in the eastern Mediterranean or may be due to being a tertiary reference hospital. The high variability in timing of IVIG administration (2–45 days) might explain the high frequency of coronary artery involvement, including the high rate of giant aneurysms. Li et al. reported that initial administration of IVIG ≤4 days after the onset of symptoms were more likely to be IVIG resistant.28 Also, receiving IVIG treatment beyond 10 days of onset of symptoms was identified as a risk factor for coronary involvement.37 Raising awareness about KD among physicians and starting treatment rapidly in the early period might decrease this rate. Previous studies had showed that the risk of coronary involvement increased in patients younger than 1 year and in those with male sex.14,38,39,40
This study has some limitations. First, it was a retrospective study. Second, since our hospital is a tertiary reference center, the rate of coronary artery involvement may not reflect the population. In addition, the high variability in the timing of IVIG administration might have affected the results of our study. Third, the study consists of single-center data, and multi-center studies are needed. Despite this limitations, the strengths of our study was to evaluate and compare the performances of IVIG resistance scores, many of which were recently published. Turkey is an Eastern Mediterranean country with a Caucasian population and many of the minorities whose exact number is unknown. We evaluated the effectiveness of IVIG prediction models developed in both Asian and non-Asian patients.
Conclusion
Current risk-scoring systems had good specificity but low sensitivity for predicting IVIG resistance in the Turkish population. Increased serum GGT levels and low platelet count were risk factors for predicting IVIG resistance in our society. Further multi-center studies are necessary to develop risk score systems with an effective performance.
References
Jennette, J. C. et al. 2012 revised International Chapel Hill Consensus Conference nomenclature of vasculitides. Arthritis Rheum. 65, 1–11 (2013).
Singh, S., Vignesh, P. & Burgner, D. The epidemiology of Kawasaki disease: a global update. Arch. Dis. Child. 100, 1084–1088 (2015).
Ozen, S. et al. Childhood vasculitides in Turkey: a nationwide survey. Clin. Rheumatol. 26, 196–200 (2007).
McCrindle, B. W. et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation 135, e927–e999 (2017).
Jamieson, N. & Singh-Grewal, D. Kawasaki disease: a clinician’s update. Int. J. Pediatr. 2013, 645391 (2013).
Shulman, S. T. & Rowley, A. H. Kawasaki disease: insights into pathogenesis and approaches to treatment. Nat. Rev. Rheumatol. 11, 475 (2015).
Tremoulet, A. H. et al. Resistance to intravenous immunoglobulin in children with Kawasaki disease. J. Pediatr. 153, 117–121 (2008).
Song, M. S. Predictors and management of intravenous immunoglobulin-resistant Kawasaki disease. Korean J. Pediatr. 62, 119 (2019).
Phuong, L. K., Curtis, N., Gowdie, P., Akikusa, J. & Burgner, D. Treatment options for resistant Kawasaki disease. Pediatr. Drugs 20, 59–80 (2018).
Sano, T. et al. Prediction of non-responsiveness to standard high-dose gammaglobulin therapy in patients with acute Kawasaki disease before starting initial treatment. Eur. J. Pediatr. 166, 131–137 (2007).
Do, Y.-S. et al. Predicting factors for refractory Kawasaki disease. Korean Circ. J. 40, 239–242 (2010).
Davies, S. et al. Predicting IVIG resistance in UK Kawasaki disease. Arch. Dis. Child. 100, 366–368 (2015).
Kobayashi, T. et al. Prediction of intravenous immunoglobulin unresponsiveness in patients with Kawasaki disease. Circulation 113, 2606–2612 (2006).
Harada, K. Intravenous γ‐globulin treatment in Kawasaki disease. Pediatr. Int. 33, 805–810 (1991).
Egami, K. et al. Prediction of resistance to intravenous immunoglobulin treatment in patients with Kawasaki disease. J. Pediatr. 149, 237–240 (2006).
Kanai, T. et al. The combination of the neutrophil-to-lymphocyte and platelet-to lymphocyte ratios as a novel predictor of intravenous immunoglobulin resistance in patients with Kawasaki disease: a multicenter study. Heart Vessels 35, 1463–1472 (2020).
Lin, M.-T. et al. Risk factors and derived formosa score for intravenous immunoglobulin unresponsiveness in Taiwanese children with Kawasaki disease. J. Formos. Med. Assoc. 115, 350–355 (2016).
Wu, S. et al. Prediction of intravenous immunoglobulin resistance in Kawasaki disease in children. World J. Pediatr. 16, 607–613 (2020).
Yang, S., Song, R., Zhang, J., Li, X. & Li, C. Predictive tool for intravenous immunoglobulin resistance of Kawasaki disease in Beijing. Arch. Dis. Child. 104, 262–267 (2019).
Tan, X.-H. et al. A new model for predicting intravenous immunoglobin-resistant Kawasaki disease in Chongqing: a retrospective study on 5277 patients. Sci. Rep. 9, 1–9 (2019).
Piram, M. et al. Defining the risk of first intravenous immunoglobulin unresponsiveness in non-Asian patients with Kawasaki disease. Sci. Rep. 10, 1–10 (2020).
Bozlu, G., Karpuz, D., Hallioglu, O., Unal, S. & Kuyucu, N. Relationship between mean platelet volume-to-lymphocyte ratio and coronary artery abnormalities in Kawasaki disease. Cardiol. Young 28, 832–836 (2018).
Moffett, B. S., Syblik, D., Denfield, S., Altman, C. & Tejtel-Sexson, K. Epidemiology of immunoglobulin resistant Kawasaki disease: results from a large, national database. Pediatr. Cardiol. 36, 374–378 (2015).
Kim, G. B. et al. Epidemiology and clinical features of Kawasaki disease in South Korea, 2012–2014. Pediatr. Infect. Dis. J. 36, 482–485 (2017).
Jakob, A. et al. Kawasaki disease in Germany. Pediatr. Infect. Dis. J. 35, 129–134 (2016).
Sleeper, L. A. et al. Evaluation of Kawasaki disease risk-scoring systems for intravenous immunoglobulin resistance. J. Pediatr. 158, 831.e3–835.e3 (2011).
Kuo, H.-C., Yang, K. D., Chang, W.-C., Ger, L.-P. & Hsieh, K.-S. Kawasaki disease: an update on diagnosis and treatment. Pediatr. Neonatol. 53, 4–11 (2012).
Li, X. et al. Predictors of intravenous immunoglobulin-resistant Kawasaki disease in children: a meta-analysis of 4442 cases. Eur. J. Pediatr. 177, 1279–1292 (2018).
Wang, Y. et al. Unique molecular patterns uncovered in Kawasaki disease patients with elevated serum gamma glutamyl transferase levels: implications for intravenous immunoglobulin responsiveness. PLoS ONE 11, e0167434 (2016).
Aydin, E. A. et al. The factors affecting the disease course in Kawasaki disease. Rheumatol. Int. 39, 1343–1349 (2019).
Chantasiriwan, N., Silvilairat, S., Makonkawkeyoon, K., Pongprot, Y. & Sittiwangkul, R. Predictors of intravenous immunoglobulin resistance and coronary artery aneurysm in patients with Kawasaki disease. Paediatr. Int. Child Health 38, 209–212 (2018).
Kim, M. K., Song, M. S. & Kim, G. B. Factors predicting resistance to intravenous immunoglobulin treatment and coronary artery lesion in patients with Kawasaki disease: analysis of the Korean nationwide multicenter survey from 2012 to 2014. Korean Circ. J. 48, 71–79 (2018).
Ghelani, S. J., Kwatra, N. S. & Spurney, C. F. Can coronary artery involvement in Kawasaki disease be predicted? Diagnostics 3, 232–243 (2013).
Ogata, S. et al. Coronary artery outcomes among children with Kawasaki disease in the United States and Japan. Int. J. Cardiol. 168, 3825–3828 (2013).
Ozdemir, H. et al. Clinical and epidemiological characteristics of children with Kawasaki disease in Turkey. J. Trop. Pediatr. 56, 260–262 (2010).
Yılmazer, M. M. et al. Kawasaki disease in Turkish children: a single center experience with emphasis on intravenous immunoglobulin resistance and giant coronary aneurysms. Turk. J. Pediatr. 61, 648–656 (2019).
Yan, F., Pan, B., Sun, H., Tian, J. & Li, M. Risk factors of coronary artery abnormality in children with Kawasaki disease: a systematic review and meta-analysis. Front. Pediatr. 7, 374 (2019).
Sudo, D. et al. Case–control study of giant coronary aneurysms due to Kawasaki disease: the 19th nationwide survey. Pediatr. Int. 52, 790–794 (2010).
Belay, E. D. et al. Kawasaki syndrome and risk factors for coronary artery abnormalities: United States, 1994–2003. Pediatr. Infect. Dis. J. 25, 245–249 (2006).
Zhang, T. et al. Factors related to cardiac sequelae of Kawasaki disease. Eur. J. Pediatr. 158, 694–697 (1999).
Author information
Authors and Affiliations
Contributions
U.K.A., E.A.A., O.S., E.S., S.D., E.A., and M.K. conceptualized and designed the study, drafted the initial manuscript, reviewed and revised the manuscript. H.H.A. conceptualized and designed the study, drafted the initial manuscript, and critically reviewed the manuscript for important intellectual content. E.D.B. and T.K. conceptualized and designed the study, coordinated and supervised data collection, and critically reviewed the manuscript for important intellectual content. Y.B. and S.O. conceptualized and designed the study, coordinated and supervised data collection, and critically reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study has been approved by Hacettepe University Ethics Commission (Approval number: GO 20/568). Due to the retrospective nature of the study, informed consent was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kaya Akca, U., Arslanoglu Aydin, E., Aykan, H.H. et al. Comparison of IVIG resistance predictive models in Kawasaki disease. Pediatr Res 91, 621–626 (2022). https://doi.org/10.1038/s41390-021-01459-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01459-w
This article is cited by
-
C-reactive protein to albumin ratio as a prognostic tool for predicting intravenous immunoglobulin resistance in children with kawasaki disease: a systematic review of cohort studies
Pediatric Rheumatology (2024)
-
Intravenous immunoglobulin resistance in Kawasaki disease patients: prediction using clinical data
Pediatric Research (2024)
-
Risk scores for Kawasaki disease, a management tool developed by the KAWA-RACE cohort
Clinical Rheumatology (2022)