Abstract
Background
Using an optical method based on tunable diode laser absorption spectroscopy, we previously assessed oxygen (O2) and water vapor (H2O) content in a tissue phantom of the preterm infant lung. Here we applied this method on newborn piglets with induced lung complications.
Methods
Five mechanically ventilated piglets were subjected to stepwise increased and decreased fraction of inspired oxygen (FiO2), to atelectasis using a balloon catheter in the right bronchus, and to pneumothorax by injecting air in the pleural cavity. Two diode lasers (764 nm for O2 gas absorption and 820 nm for H2O absorption) were combined in a probe delivering light either externally, on the skin, or internally, through the esophagus. The detector probe was placed dermally.
Results
Calculated O2 concentrations increased from 20% (IQR 17−23%) when ventilated with room air to 97% (88−108%) at FiO2 1.0. H2O was only detectable with the internal light source. Specific light absorption and transmission patterns were identified in response to atelectasis and pneumothorax, respectively.
Conclusions
The optical method detected FiO2 variations and discriminated the two induced lung pathologies, providing a rationale for further development into a minimally invasive device for real-time monitoring gas changes in the lungs of sick newborn infants.
Impact
-
Optical spectroscopy can detect pulmonary complications in an animal model.
-
Oxygen concentrations can be evaluated in the lungs.
-
Presents a novel minimally invasive method to detect lung oxygenation and complications.
-
Potential to be developed into a lung monitoring method in newborn infants.
-
Potential for bed-side detection of pulmonary complications in newborn infants.
Similar content being viewed by others
Introduction
The pulmonary transition from intrauterine environment to normal postnatal air breathing is vulnerable and may cause a multitude of pulmonary complications that are increasingly prevalent with decreasing gestational age of the newborn infant. Abnormal pulmonary aeration is common in neonatal lung diseases. Despite modern synchronized respiratory support methods or minimally invasive surfactant therapy, there is still a risk of life-threatening complications such as pneumothorax,1 and bronchopulmonary dysplasia remains a major problem and a long-term consequence of the acutely ill preterm lung.2 Thereby, a continuous measure of lung aeration may be useful for improving the precision of ventilatory support and detection of air leaks or inadequately ventilated regions of the lung.
Presently, most lung problems are diagnosed with pulmonary X-ray, which only gives a snapshot of the current condition and causes harmful radiation, increasing the risk of malignancy development later in life.3,4 Research efforts have been directed towards the development of noninvasive alternatives to X-ray imaging. Currently, lung ultrasound imaging5 can be used for the detection of pneumothorax, consolidated lung parts and pleural effusions (e.g. blood). However, since nearly 100% of the ultrasound pulses are reflected by gas, the amount of air in the lungs cannot be estimated. The technique is emerging as an alternative to chest X-ray,6 but it is user-dependent and provides only momentary information.
A new optical technique called gas in scattering media absorption spectroscopy (GASMAS),7 based on tunable diode laser absorption spectroscopy (TDLAS), detects gas concentration by free gas absorption in cavities surrounded by multiple light scattering media.8 The high-resolution spectroscopic technique detects spectrally narrow gas absorption features in the surrounding wide band absorption of the tissue. We have applied this technique on phantoms of newborn lung9,10,11 and on healthy newborn infants12 and showed that pulmonary O2 content could be detected.13 In addition, the method allows determination of water vapor (H2O) absorption path length, which enables evaluation of lung volume and pulmonary O2 concentration.10,13
A challenge when using optical methods in biological tissues is the strong light scattering and absorption leading to considerable attenuation of detectable light and weak signals. Much of the light emitted through the skin is scattered, and only a small portion of the light reaches the detector. The approach with internal illumination would increase the amount of light reaching the detector. This approach has successfully been used in our phantom studies.14
We hypothesized that the GASMAS method with an external as well as an internal light source probe would detect changes in pulmonary O2 gas concentration, including responses to induced local lung pathologies in newborn piglets.
Methods
Animal preparation and monitoring
Danish Landrace newborn piglets underwent routine care at the farm together with siblings until transported to the animal facilities of Copenhagen University. They were immediately taken to the surgical theater and anesthetized. The Danish Animal Experiments Inspectorate approved the study protocol (2018-15-0201-01403). All responsible researchers had current animal handling certificate and the experiments were performed according to FELASA (Federation of Laboratory Animal Science Associations) guidelines and national regulations.
Five healthy piglets, at a mean age of 14 days (range 13−15 days) and a median weight of 3.2 kg (range 3.1–3.3 kg), were used. Anesthesia was induced by an intramuscular injection of 1 ml/kg Zoletil (tiletamine 25 mg/ml, zolazepam 25 mg/ml, xylazine 25 mg/ml, ketamine 25 mg/ml, methadone 4 mg/ml, buthorphanol 4 mg/ml) and was maintained by infusion of propofol (15 mg/kg/h) and fentanyl (7 µg/kg/h). After sedation, the piglets were endotracheally intubated and connected to a pressure-controlled ventilator. At 3 h after initiation of anesthesia, 1 ml/kg Zoletil was administered intravenously, and at any signs of distress or poor sedation additional dose of 0.1 ml Zoletil was given. Arterial CO2 was kept between 4.5 and 6.5 kPa and arterial saturation above 95%. A heat moister exchanger (Humid-vent® mini, Teleflex, Morrisville, North Carolina) was connected between the ventilator and the endotracheal tube. Arterial saturation was continuously monitored by pulse oximetry on the foreleg (Radical 7®, Massimo, Irvine, Canada). Normal rectal temperature was maintained (38.5−39.5 °C) by a heating pad. The femoral artery was cannulated for continuous invasive monitoring of mean arterial blood pressure and heart rate. Both ear veins were cannulated for infusion of propofol, fentanyl and saline 0.9%. The piglet recovered for 1 h after the surgical preparation before the experiment. Arterial blood gases and blood glucose were measured after the surgical preparation and during the experimental study. At the end of the study, the piglet was euthanized with 100 mg/kg pentobarbital.
Experimental design
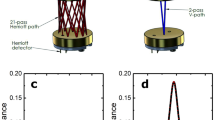
We conducted three interventions (Fig. 1) with a dermal detector probe and two different light source probes, one applied to the skin, and one internal probe located in the esophagus. The internal optical fiber probe was positioned in the esophagus at a distance of 21 cm from the snout. The localization corresponded to a position at the heart level, which was confirmed by fluoroscopy X-ray in the first two piglets (Fig. 2). This position was kept for all the following piglets as they had similar size and weight. The detector probe was placed in the right axillary line, approximately 2 cm below the foreleg. The dermal light source probe was placed in the midclavicular line on the right side of the thorax with at least 3 cm distance to the detector. The source and detector probes were fixed with elastic black nylon straps that also prevented light dispersion from the dermal laser source.
The initial procedure was a stepwise increase and decrease in inspired oxygen fraction (FiO2) in the ventilator settings with the light source on the skin and thereafter repeated in duplicate with the light source in the esophagus (Fig. 1a). The absorption of O2 and H2O vapor was measured by the GASMAS system with FiO2 at 0.21, 0.30, 0.50, 0.75 and 1.0 after the fractional end-tidal O2 (FetO2) of the ventilator had reached the target concentration. FetO2 values were considered equivalent to the fractional alveolar O2 (FaO2). At each FiO2 setting, the measured O2 and H2O absorption signals were averaged over 10 s and sampled ten times. After the measurement at FiO2 1.0, a pulmonary recruitment procedure was done by increasing the inspiration pressure, to reduce the risk of resorption atelectasis.15 Recruitment was deemed successful when tidal volumes were the same as before starting the experiment. The detector probe position, fixation and the stepwise changes of FiO2 were the same in the dermal and esophageal measurements (Fig. 2).
We then performed a partial pulmonary atelectasis with the esophageal light probe in place (Fig. 1b). The FiO2 was set to 0.30. A 4 Fr embolectomy catheter with a balloon at its tip (LeMaitre® Vascular, Sulzbach, Germany) was inserted into the trachea parallel to the endotracheal tube into the right main bronchus (Fig. 1b). In two piglets, the position was verified by fluoroscopy X-ray. Partial obstruction of the distal airways was considered confirmed when the end-tidal CO2 had decreased by 50% after balloon inflation. The balloon was deflated after approximately 1.5 min or if the piglet became circulatory unstable. Oxygen signals were continuously measured during the procedure, which was repeated three times. Between each atelectasis, mechanical recruitment of pulmonary volume was performed.
After the piglet had recovered from atelectasis, a small thoracostomy was prepared in the right axillary line, 1 cm below the dermal detector probe, and a drainage tube was placed and fixated with sutures. The piglet was ventilated with FiO2 1.0 while 100 ml of ambient air (FiO2 0.21) was injected into the pleural space through the tube (Fig. 1c). In two piglets, we confirmed the pneumothorax with fluoroscopy X-ray. Oxygen signals were continuously measured during the pneumothorax phase. Approximately 2 min after induction, the air was withdrawn from the pleural cavity and pulmonary recruitment followed. The procedure was repeated three times.
Optical experimental setup
The GASMAS system (GPX Medical AB, Sweden) measured gas absorption at two wavelengths, 764 nm for O2 gas absorption and 820 nm for H2O vapor absorption. The measured gas absorption is expressed in a dimension of [%m] which is the product of the relative gas concentration [%] and the absorption path length [m].13 The instrument was calibrated using known concentrations and absorption path lengths. The relative humidity in the lung is approximately 100%, and together with the knowledge of tissue temperature and air pressure, the H2O vapor gas concentration can numerically be estimated.16 The measured H2O vapor gas absorption in [%m] thus provides the absorption path length in [m] for light at 820 nm. Assuming that the light at 764 nm travels the same average distance in the gas volume, the measured O2 gas absorption in [%m] then provides the O2 concentration in [%].
The two diode lasers providing light at 764 and 820 nm, respectively, were focused into an optical fiber (core diameter 400 µm), which provided an output power at the tissue interface of 25 and 8.1 mW, respectively. The diode lasers and the light combining optics were enclosed in a nitrogen-filled box to eliminate offsets in the absorption signal due to ambient air.
The gas absorption signal was obtained by sequentially scanning the wavelength of the lasers, at a rate of 1 kHz, over one of the absorption lines of the O2 molecule at 764 nm and of H2O at 820 nm. The two gases were measured in sequence with a measurement time of 100 s before switching.
Optical fibers with two different light distributions at the distal end were employed for skin and esophageal light administration, respectively. The rationale for using internal light illumination is the fact that when light is applied on the skin and detected from the skin surface, theoretically, only 1% of the light that reaches lung tissue would reach the detector. If the light source is placed internally, e.g. through a nasogastric feeding tube or an endotracheal tube, the light travels through the air-filled lung with a shorter path through solid tissue before reaching the skin surface, thereby theoretically leading to higher light intensity at the detector with a larger portion of photons subjected to gas absorption. Taking as an example if 1% of the light emitted at the surface would reach the lung tissue and then be scattered back after interacting with the gas, again only 1% of that light would reach a detector on the surface. Clearly, if the light instead would only need to travel in one direction, using internal illumination, a factor of about 100 in detected intensity could typically be gained. Also, by internal illumination, a larger fraction of the detected light would have passed through the gas-bearing lung tissue, laying between the light injection point and the detector. For skin light administration, a diffusing cylindrical object was used to create a homogeneous emission over an area of 1 cm2 with an irradiance of 25 mW/cm2 and 8.1 mW/cm2 for 764 and 820 nm, respectively. For the internal light administration, the end of the fiber was diffusing over a longitudinal distance of 10 mm with an outer diameter of 0.9 mm, giving an irradiance of 88 and 29 mW/cm2 for 764 and 820 nm, respectively. Due to the diffuse emission and low light intensities, both fiber probe designs are eye-safe (Laser Class I, IEC 60825-1:2014) and no significant tissue heating is expected as the irradiance is kept below 150 mW/cm2.17
After propagating through the tissue, the transmitted light was detected by a photodiode (active area 10 mm × 10 mm) incorporated into a detector probe attached to the skin. The detector probe area was covered with a layer of ultrasonic gel in order to reduce offsets in the absorption signal. The detected absorption signal was intensity normalized and frequency filtered by the electronic platform, which acquires the absorption magnitude through proprietary algorithms.
Statistical analysis
The oxygen concentration, \(X_{{\mathrm{O}}_2}\), was evaluated assuming that the absorption path length of water vapor \(\left( {L_{{\mathrm{H}}_2{\mathrm{O}}}} \right)\) and oxygen \(\left( {L_{{\mathrm{O}}_2}} \right)\) is equal. \(L_{{\mathrm{H}}_2{\mathrm{O}}}\) was obtained from the absorption signal of water vapor (\(A_{{\mathrm{H}}_2{\mathrm{O}}}\)) and by calculating the temperature-dependent water vapor concentration \(X_{{\mathrm{H}}_2{\mathrm{O}}}\).18
For each measurement series, i.e. a set value of inspired oxygen, the \(A_{{\mathrm{O}}_2}\) and \(A_{{\mathrm{H}}_2{\mathrm{O}}}\) were sequentially obtained, as described above. The oxygen concentration in the equation was determined by using the measured oxygen absorption and the median value of the water vapor absorption. Every measurement series yielded between 8 and 12 data points and the FiO2 was repeated between two and five times for each piglet, with the exception for piglet number 3, where the FiO2 challenge was done only once. For statistical analyses, a one-way ANOVA test was performed.
Results
Determination of oxygen and water vapor absorption
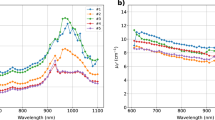
With the internal light probe placed in the esophagus, the detected absorption signal was roughly one order of magnitude larger compared to the measurements with the dermal light source (Fig. 3). Water vapor absorption was variably detected when using the skin light source (Fig. 3b). As the evaluation of O2 concentration is dependent on the absorption of both O2 and H2O, determination was not possible for all piglets.
When using the internal light source, the signals from both O2 and H2O were clearly detectable, and the absorption values changed with the set value of FiO2 (Fig. 3c, d). The calculated O2 concentrations, using the internal light source, are shown in Fig. 4. A clear agreement between the evaluated O2 concentrations and the set FiO2 values was observed. The one-way ANOVA test showed that the calculated mean of the O2 concentration values significantly differed following the set FiO2 values on the ventilator (p < 10−4).
The O2 concentrations were determined from O2 and H2O absorption signals obtained using the internal light source (Fig. 3c, d). The median and the 25th and 75th quartiles are shown.
Atelectasis and pneumothorax
Atelectasis was induced in four piglets while continuously monitoring the O2 absorption and light transmission using the internal light source. During the atelectasis, the O2 absorption signal and the light transmission were both observed to decrease over a time scale of 10−30 s (Fig. 5). When the balloon was deflated, the absorption and light transmission returned in most cases to the initial value before atelectasis. The continuously monitored O2 absorption decreased rapidly when the pneumothorax was induced and simultaneously the light transmission increased (Fig. 6a). When the air was removed from the pleural space, the O2 absorption and the light transmission returned to their initial values. Using an optical measurement exposure time of 0.333 s in one piglet during the pneumothorax, the variation in transmission and absorption followed each breath provided by the ventilator (Fig. 6b).
a O2 absorption signal (black line) and light transmission (red line) in response to induced pneumothorax in four piglets. In all four piglets (upper left, upper right, lower left, lower right), a typical pattern was observed with a rapid increase in transmission and a decrease in O2 absorption, changes that were restored when the air was suctioned out of the pleural cavity about 200 s later. b O2 absorption signal and corresponding light transmission changes to each breath during induced pneumothorax in one piglet. With a respiratory rate of 20 breaths per minute (set by the ventilator) and sampling time 0.333 s, the O2 absorption and transmission values are presented during 180 s (left) and 40 s (right), respectively, showing that their variations follow each breath provided by the ventilator.
Discussion
In this study, for the first time, we have successfully determined pulmonary O2 concentration using an internal laser light source. We show here that the detected amount of O2 in the lungs correlated with inhaled O2 concentrations and that the pathophysiological changes of aeration produced in the experimental setting were detectable by the GASMAS system. We were not able to estimate O2 concentrations when using a dermal light source, due to too weak H2O absorption signal.
Using the internal light source placed in the esophagus, we detected distinct and prompt changes in absorption and transmission signals in response to stepwise changes in FiO2, as well as to induced pneumothorax. Interestingly, a breath-related change was observed both in O2 absorption and light transmission during pneumothorax. The observed decrease in O2 absorption during atelectasis was less robust with variations between piglets.
The rapid decrease in O2 absorption signal during the pneumothorax can be explained by the collapse of the lung enabling the light to predominately travel through a hollow, nonstructured pleural cavity. The FiO2 was 1.0, and upon lung collapse, the remaining absorption signal equivalents the O2 content in ambient air injected into the pleural cavity. Conversely, when removing the air, the incremental absorption signal can be explained by the lung gradually regaining its original gas-filled form. Noteworthy, the method appeared to be sensitive enough to detect inspiration and expiration changes to each breath. The O2 absorption decrease during atelectasis may be related to O2 consumption and induced physical change of the lung structure resulting in a reduced absorption path length, i.e. smaller gas volume in a denser lung. This pathophysiologic difference between pneumothorax and atelectasis explains the patterns of absorption changes. Thus, this experimental study provides a proof of concept that the GASMAS technique has the potential to detect neonatal life-threatening pulmonary complications.
The incidence of pneumothorax is up to 5−7% in infants with a birth weight less than 1500 g treated in ventilators19 and it carries a risk of mortality. Continuous monitoring of pulmonary oxygen content could possibly reduce the time from onset of pneumothorax until diagnosis and intervention. The GASMAS technique, if applied with an indwelling probe in the nasogastric tube, is not more invasive than the routinely used NAVA-ventilation, and according to one study no adverse effects of the NAVA catheter were observed.20 We envision that the technique could be developed into a surveillance for preterm infants in need of respiration support.
Pulmonary pathophysiology has been subject to investigation with a range of noninvasive techniques with continuous monitoring.21 In general, newer techniques, such as electromagnetic inductance plethysmography and electrical impedance tomography, provide clinically useful data, including the detection of pneumothoraxes.22 The techniques, however, are restricted in the applicability due to difficulties in electrode placement on the tested subjects, especially in infants with very low birth weight.23 Optoelectronic plethysmography is a noninvasive 3D motion capture method, measuring chest wall movements, estimating lung volumes. The technique reconstructs the chest wall surface by using up to 89 surface markers (24 can be used in the infant setting) and 8 infrared cameras, mounted in the room. This is a promising research technique for lung volume assessment, but not feasible for clinical bed-side continuous monitoring, nor can it provide information on oxygen distribution throughout the lungs.24 Electrical impedance tomography25,26 gives information on global and regional changes in lung impedance correlating with intrathoracic changes in air content and thereby lung volume. However, this technique only gives information on a transversal “slice” of the lung and does not provide any information on O2 content.
Lung ultrasound is another noninvasive technique used in intensive care units to detect e.g. atelectasis5; however, it is highly user-dependent, gives no information on oxygen distribution, and does not allow for continuous surveillance. In comparison to the above mentioned, the GASMAS technique enables continuous monitoring of the oxygen concentration in the lung as well as an indication of changes in gas volume with one light probe (preferably internal) and one or several detection probes.
Conventional pulse oximetry is routinely used for arterial oxygen saturation monitoring, and in the newborn infant information about pre- and postductal differences in oxygen saturation can be obtained. The proposed technique in the present study should be considered as a complement to pulse oximetry as it has the ability to detect lung pathologies quickly, most probably before changes in arterial oxygenation occur.
A considerable signal variation in the absorption signal between the piglets during the induced atelectasis was observed. However, the decrease in transmission observed in all piglets was consistent. This is physiologically well understood, since the induced atelectasis leads to distal lung parenchyma collapse, resulting in concomitant decreased transmission of light. This needs to be further investigated, focusing on the transmission variation as a response to varying degrees of atelectasis.
Due to too weak H2O signal with dermal light administration, the pulmonary O2 concentration could not be estimated. Piglets have an elongated and narrow thorax compared to human infants and the front leg makes the apical part of the thorax less accessible. This disturbs the required balance between the need for a minimum light source-detector distance and proximity to lung tissue with volumes large enough for the light not to travel through extra-pulmonary tissue (e.g. trachea, mediastinum, and abdominal organs). Light from a dermal light source will theoretically scatter more at entrance to the lungs than from an internal source. Moreover, the characteristics of the skin of the piglet differ from preterm infants and thereby piglets may not be the optimal model to mimic human infants, when evaluating the dermal light source. However, using internal light administration, we obtained clear signal changes in response to the right-sided pneumothorax, suggesting robust signal conductance from source to detector. In previous studies, we have obtained strong O2 absorption signals in healthy full-term infants with a dermal light source.13 In the present study, when delivering the light internally, reliable pulmonary O2 concentrations could, for the first time in an experimental animal, be determined using the H2O absorption signal. Thus, the internal light source was superior to the dermally positioned. Likewise, calculations of oxygen concentrations were possible on a 3D phantom of a newborn infant´s torso, when applying the light source internally.14
Autopsy of one piglet did not reveal any visually detected damage to the esophagus. However, we did not study the possible microscopic damages to the tissue from slight temperature increases or physical damage from the optical fiber probe. The diffuse light emission was significantly lower than the maximum irradiance allowed, 150 mW/cm2, which when exposed on the skin would generate a maximum temperature increase of 2 °C.17 Whether this local increase in temperature of the nasogastric tube could have any adverse effects on neonatal esophagus needs to be investigated. We envision that for clinical investigations to avoid contact with esophagus, the light probe would be inserted into or embedded in a nasogastric tube, and could even be used together with NAVA ventilation.
Future studies of the GASMAS technique should focus on the reliability and accuracy of the measurements in sufficient number of subjects with an improved equipment developed from the prototype used in this study. Further, the applicability of the technique to detect changes in lung volume parameters (e.g. tidal volume) can be studied by changing ventilator settings in the experimental model, as indicated by the possibility to follow each breath. Before clinical studies in newborn infants can be designed, the safety aspects of the technique, such as heating effects, must be assessed. Also, ensuring a simple and robust applicability with well-designed light probes and detectors suitable for fragile preterm infants is essential for the technique to be investigated in the neonatal intensive care unit environment.
Conclusion
GASMAS enables measurement of pulmonary O2 concentration using an internal light probe along with distinct signal changes during pneumothorax in a neonatal piglet model. Compared to electric impedance and ultrasound, GASMAS has the advantage to detect oxygen content and lung volume changes of each breath. We were not able to reliably detect pulmonary O2 content using a dermal light probe. Future studies should focus on the accuracy and reliability along with safety of this method.
References
Dargaville, P. A., Ali, S. K. M., Jackson, H. D., Williams, C. & De Paoli, A. G. Impact of minimally invasive surfactant therapy in preterm infants at 29−32 weeks gestation. Neonatology 113, 7–14 (2018).
Doyle, L. W. et al. Ventilation in extremely preterm infants and respiratory function at 8 years. N. Engl. J. Med. 377, 329–337 (2017).
Hall, E. J. & Brenner, D. J. Cancer risks from diagnostic radiology. Br. J. Radiol. 81, 362–378 (2008).
Pearce, M. et al. Radiation exposure from Ct scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 380, 499–505 (2012).
Liang, H.-Y. et al. Ultrasound in neonatal lung disease. Quant. Imaging Med. Surg. 8, 535–546 (2018).
Hiles, M. et al. Neonatal respiratory distress syndrome: chest X-ray or lung ultrasound? A systematic review. Ultrasound 25, 80–91 (2017).
Svanberg, S. Gas in scattering media absorption spectroscopy—from basic studies to biomedical applications. Laser Photon. Rev. 7, 779–796 (2013).
Persson, L., Andersson, M., Cassel-Engquist, M., Svanberg, K. & Svanberg, S. Gas monitoring in human sinuses using tunable diode laser spectroscopy. J. Biomed. Opt. 12, 054001 (2007).
Lewander, M., Bruzelius, A., Svanberg, S., Svanberg, K. & Fellman, V. Nonintrusive gas monitoring in neonatal lungs using diode laser spectroscopy: feasibility study. J. Biomed. Opt. 16, 127002 (2011).
Larsson, J. et al. Development of a 3-dimensional tissue lung phantom of a preterm infant for optical measurements of oxygen—laser-detector position considerations. J. Biophotonics 11, e201700097 (2018).
Liao, P. et al. Computer simulation analysis of source-detector position for percutaneously measured O2-gas signal in a three-dimensional preterm infant lung. J. Biophotonics 11, e201800023 (2018).
Lundin, P. et al. Noninvasive monitoring of gas in the lungs and intestines of newborn infants using diode lasers: feasibility study. J. Biomed. Opt. 18, 127005 (2013).
Svanberg, E. K. et al. Diode laser spectroscopy for noninvasive monitoring of oxygen in the lungs of newborn infants. Pediatr. Res. 79, 621–628 (2016).
Larsson, J. et al. Comparison of dermal versus internal light administration in human lungs using the TDLAS-GASMAS technique—phantom studies. J. Biophotonics 12, e201800350 (2019).
Hedenstierna, G. & Edmark, L. Effects of anesthesia on the respiratory system. Best Pract. Res. Clin. Anaesthesiol. 29, 273–284 (2015).
Buck, A. New equations for computing vapor-pressure and enhancement factor. J. Appl. Meteorol. 20, 1527–1532 (1981).
Pålsson, S. et al. Kinetics of the superficial perfusion and temperature in connection with photodynamic therapy of basal cell carcinomas using esterified and non-esterified 5-aminolaevulinic acid. Br. J. Dermatol. 148, 1179–1188 (2003).
McRae, G. J. A simple procedure for calculating atmospheric water vapor concentration. JAPCA J. Air Waste Ma. 30, 394–394 (1980).
Litmanovitz, I. & Carlo, W. A. Expectant management of pneumothorax in ventilated neonates. Pediatrics 122, e975–e979 (2008).
Stein, H., Hall, R., Davis, K. & White, D. B. Electrical activity of the diaphragm (Edi) values and Edi catheter placement in non-ventilated preterm neonates. J. Perinatol. 33, 707–711 (2013).
Reiterer, F., Sivieri, E. & Abbasi, S. Evaluation of bedside pulmonary function in the neonate: from the past to the future. Pediatr. Pulmonol. 50, 1039–1050 (2015).
Bhatia, R., Schmolzer, G. M., Davis, P. G. & Tingay, D. G. Electrical impedance tomography can rapidly detect small pneumothoraces in surfactant-depleted piglets. Intensive Care Med. 38, 308–315 (2012).
Pillow, J. J., Frerichs, I. & Stocks, J. Lung function tests in neonates and infants with chronic lung disease: global and regional ventilation inhomogeneity. Pediatr. Pulmonol. 41, 105–121 (2006).
Massaroni, C. et al. Optoelectronic plethysmography in clinical practice and research: a review. Respiration 93, 339–354 (2017).
Miedema, M., de Jongh, F. H., Frerichs, I., van Veenendaal, M. B. & van Kaam, A. H. Changes in lung volume and ventilation during surfactant treatment in ventilated preterm infants. Am. J. Respir. Crit. Care Med. 184, 100–105 (2011).
Chatziioannidis, I., Samaras, T., Mitsiakos, G., Karagianni, P. & Nikolaidis, N. Assessment of lung ventilation in infants with respiratory distress syndrome using electrical impedance tomography. Hippokratia 17, 115–119 (2013).
Acknowledgements
This work was financially supported in part by the European Community (EUREKA EUROSTARS) NEOLUNG project (E! 9833 Neo-Lung), the LASERLAB-EUROPE (EUH2020 654148) JRA project BIOAPP and Departments of Pediatrics and Physics, Lund University, Lund, Sweden.
Author information
Authors and Affiliations
Contributions
Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data: E.K.S., J.L., M.R., M.L., D.L., S.B., G.G., V.F. Drafting the article or revising it critically for important intellectual content: E.K.S., J.L., M.R., M.L., D.L., S.B., J.B., G.G., V.F. Final approval of the version to be published: all authors.
Corresponding author
Ethics declarations
Competing interests
GPX Medical is a startup company responsible for the development of the GASMAS prototype used in the study. D.L. and S.B. are employed by the company. E.K.S., J.L., M.R., M.L., J.B., G.G. and V.F. have nothing to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Svanberg, E.K., Larsson, J., Rasmussen, M. et al. Changes in pulmonary oxygen content are detectable with laser absorption spectroscopy: proof of concept in newborn piglets. Pediatr Res 89, 823–829 (2021). https://doi.org/10.1038/s41390-020-0971-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0971-x
This article is cited by
-
Initial non-invasive in vivo sensing of the lung using time domain diffuse optics
Scientific Reports (2024)
-
Evolution of gas in scattering media absorption spectroscopy as a neonatal pulmonary monitoring device
Pediatric Research (2022)
-
Gas in scattering media absorption spectroscopy as a potential tool in neonatal respiratory care
Pediatric Research (2022)