ABSTRACT
Background
Inflammation is strongly associated with premature birth and neonatal morbidities. Increases in infant haptoglobin, haptoglobin-related protein (Hp&HpRP), and interleukin-6 (IL-6) levels are indicators of intra-amniotic inflammation (IAI) and have been linked to poor neonatal outcomes. Inflammation causes epigenetic changes, specifically suppression of miR-29 expression. The current study sought to determine whether miR-29b levels in cord blood or neonatal venous blood are associated with IAI, identified by elevated IL-6 and Hp, and subsequent clinical morbidities in the infant.
Methods
We tested 92 cord blood samples from premature newborns and 18 venous blood samples at 36 weeks corrected gestational age. MiR-29b, Hp&HpRP, and IL-6 were measured by polymerase chain reaction and enzyme-linked immunosorbent assay, respectively.
Results
Decreased levels of miR-29b were observed in infants exposed to IAI with elevated Hp&HpRP and IL-6 levels and in infants delivered by spontaneous preterm birth. Lower miR-29 levels were also observed in women diagnosed with histological chorioamnionitis or funisitis and in infants with cerebral palsy. Higher levels of miR-29 were measured in infants small for gestational age and in venous samples from older infants.
Conclusions
MiR-29 may be an additional biomarker of IAI and a potential therapeutic target for treating poor newborn outcomes resulting from antenatal exposure to IAI.
Impact
-
Decreases in miR-29b are associated with intrauterine inflammation.
-
Hp&HpRP increases are associated with decreased miR-29b.
-
MiR-29b may be an additional biomarker for neonatal outcomes and a potential therapeutic target for intrauterine inflammation.
Similar content being viewed by others
INTRODUCTION
Premature birth before 37 weeks gestational age (GA) has a global incidence of ~15 million per year, according to a World Health Organization report in 2018.1 Moreover, the March of Dimes reported a preterm birth (PTB) rate of 9.93% in 2017 in the United States.2 Despite increased survival of extremely premature infants related to advances in neonatal care, this subpopulation remains at high risk for significant short- and long-term morbidities. These morbidities include necrotizing enterocolitis (NEC), bronchopulmonary dysplasia (BPD), retinopathy of prematurity (ROP), and neurodevelopmental sequelae, such as cerebral palsy (CP), periventricular leukomalacia (PVL), and intraventricular hemorrhage (IVH).3 The wide clinical spectrum of chronic disease and severity among this population suggest a multifactorial etiology, including prematurity, maternal and fetal inflammation, and exposure to the postnatal interventions required to compensate for organ system immaturity. These adverse exposures are thought to lead to epigenetic changes, which predispose preterm infants to more severe disease in response to life-saving interventions after birth.4
MicroRNAs (miRs) are small non-coding RNAs (~22 nucleotides) that act as epigenetic regulators of normal physiologic processes and are implicated in abnormal pathologic processes.4 miRs have been investigated in a variety of diseases, and changes in miR expression have been proposed as biomarkers of disease severity.5,6,7,8 MiR-29 regulates extracellular matrix deposition and has been implicated in cancers and fibrotic diseases.9,10,11,12,13 Inflammation has been shown to suppress miR-29 expression via multiple pathways.14,15 Given the significant role of maternal inflammation on PTB and health of the infant, miR-29 may be a significant modulator of the risk for prematurity-related neonatal complications.
Interleukin-6 (IL-6) is a well-characterized pro-inflammatory cytokine and an activator of acute-phase responses. Elevated IL-6 levels at birth are considered a risk factor for sepsis-induced disseminated intravascular coagulation, pneumonia, PVL, and NEC.16,17,18,19 Haptoglobin (Hp), a well-characterized acute-phase reactant, is an abundant plasma protein synthesized primarily by the liver. Hp was previously considered to be nearly absent at birth, with an increase to adult levels throughout the first year of life.20,21 Hp acts as a potent antioxidant, which counters lipid peroxidation 20-fold more effectively than vitamin E and has indirect antioxidant effects by binding plasma-free hemoglobin with high affinity to inhibit its oxidative activity.22,23 Buhimschi et al.24 revealed that the antenatal exposure to intra-amniotic infection and/or inflammation (IAI) induces a precocious “switch-on” of Hp expression in the cord blood of premature neonates and this could serve as a biomarker for the inflammatory context of PTB.23,25 Because the employed immunoassays do not discriminate Hp from the near-homologous Hp-related protein (HpRP), this cord blood biomarker is denoted as Hp&HpRP. Further studies identified that the subpopulation of preterm neonates exposed to IAI, who are unable to switch on Hp&HpRP expression thus remain an- or hypohaptoglobinemic despite elevated cord blood IL-6, had higher odds of the composite outcomes of CP or death and grade III/IV IVH and/or death than those newborns with appropriate Hp production.22
Using the combination of increased IL-6 levels and “switch-on” Hp as the indicator of exposure to intrauterine inflammation, the current study sought to determine whether miR-29b levels in cord blood or neonatal blood are associated with antenatal exposure to IAI and subsequent clinical morbidities. By identifying the population of premature infants at the greatest risk for long-term disease, we can target our interventions to the infants most likely to benefit.
METHODS
Sample population and study design
The study used bio-banked cord blood specimens obtained at delivery and infant blood samples obtained at 36–40 weeks corrected GA. Mothers were recruited at The Ohio State University Wexner Medical Center and samples were obtained as part of a biorepository (Maternal Fetal Medicine Preterm Birth Repository (IRB #17-0079). Inclusion criteria were infants born ≤32 weeks gestation with no genetic or anatomic anomalies. Informed consent was obtained from the mother. For the purpose of this study, GA selection for infants who were born ≤30 weeks, to include the subpopulation at highest risk for morbidities associated with prematurity, and had available cord blood samples was incorporated. These criteria resulted in 92 individual samples. A total of 88 placentas from these patients were sent for pathologic analysis.
In addition, venous blood samples obtained at 36–40 weeks postmenstrual age were identified through the Perinatal Research Repository at Nationwide Children’s Hospital (Perinatal Research Repository, IRB# 10-00035) for 18 of these same infants. Both repositories contained detailed fetal and postnatal data for the infant as well as for the mother, including cytokine and biomarker analysis. Clinical outcomes of the newborns and the results of placental pathology were obtained through retrospective chart review.
Analysis of IL-6, Hp&HpRP, and miR-29b
Umbilical cord blood was collected immediately after delivery and neonatal venous blood (36–40 weeks) was collected in the Neonatal Intensive Care Unit. All blood samples were separated within 45–120 minutes, plasma frozen within 12 h of blood collection, and stored at −80 °C until analysis. IL-6 and Hp&HpRP were measured on 92 cord blood samples as previously described.24 Hp was measured as Hp&HpRP because the antibody employed in enzyme-linked immunosorbent assay does not discriminate between Hp and the closely related HpRP in cord blood.
MiR-29b levels were measured using reverse transcription-polymerase chain reaction (RT-PCR) and normalized to the internal expression of SP2 for the 92 cord blood samples and 18 36–40 weeks GA plasma samples. A RNeasy Mini Kit (Qiagen; Hilden, Germany) was used to isolate total RNAs from plasma samples. Complementary DNA (cDNA) was synthesized using a Maxima First Strand cDNA Synthesis Kit for RT-Quantitative PCR (K1642, Thermo Fisher, Waltham, MA). A MasterCycler epgradient RealPlex RT-PCR Detection System (Eppendorf, Hamburg, Germany) was used for quantitative real-time PCR analyses with Maxima SYBR Green/ROX qPCR Master Mix (K0221, Thermo Fisher, Waltham, MA). Quantitative real-time PCR analyses for miR-29b were performed using the miRCURY LNA RT Kit (339340, Qiagen, Maryland) for cDNA synthesis and the RNA Spike-In Kit (339347, Qiagen, Maryland).
Data analysis
Log transformation was applied to the biomarkers (i.e., Hp and IL-6, miR-29). We performed a sensitivity analysis to assess if the inclusion of twins changed the analysis outcomes due to the familial effect (i.e., shared genetics and environment). No imputation of missing data was performed. Categorical by categorical relationships were assessed using Barnard’s test on the contingency tables as a uniformly more powerful test than Fisher’s exact test.26,27 Categorical by quantitative relationships were tested using the Kruskal–Wallis rank-sum test.28 Comparisons with p values <0.05 were considered statistically significant. R version 3.6.0 (https://CRAN.R-project.org) was used for testing, tabulations, and to assess data.
RESULTS
Maternal and infant demographics
Demographics from the GA selected cohort are presented in Table 1. The average infant GA was 27.3 weeks and the average birth weight was ~1000 g. Racial distribution matched the distribution of the geographical area. All mothers received antenatal corticosteroids and the majority (66.3%) was delivered by C-section. Approximately 14% were multiple gestations and sensitivity analysis was performed to assess if newborn relatedness affected results. PTB was defined as spontaneous (i.e., due to spontaneous preterm labor or preterm pre-labor rupture of membranes) or medically indicated (i.e., due to maternal or fetal indications including pre-eclampsia). Overall, there were twice as many spontaneous as medical PTBs in the dataset.
Non-exposed vs. exposed to IAI
IL-6 and Hp&HpRP were measured on all 92 cord blood plasma samples and the results were segregated by “non-exposed” and “exposed” status as previously described.22 Briefly, “non-exposed” to IAI status was assigned in those samples with Hp&HpRP levels <2000 ng/mL and IL-6 levels <100 pg/mL. All samples with Hp&HpRP levels ≥2000 ng/mL were subjected to western blot to confirm switch-on status (in the presence of Hp beta band). Newborns with switch-on Hp status (visible Hp beta band) were assigned as “exposed” irrespective of IL-6 levels. Newborns with switch-off status (absent beta band) by western blot were assigned as non-exposed if IL-6 levels were <100 pg/mL and as exposed if IL-6 levels ≥100 pg/mL.24 There were only three exposed hypohaptoglobimenic newborns in this dataset. Clinical outcomes were analyzed for differences between non-exposed and exposed status. Biochemical criteria, rather than histologic placenta examination for chorioamnionitis and/or funisitis, were chosen to distinguish exposed vs. non-exposed because placental pathology was not performed for all patients. In addition, IAI is generally a clinical, rather than histological, diagnosis.29 Both placental pathologies analyzed, funisitis and chorioamnionitis, demonstrated significant differences in diagnoses between exposed and non-exposed status (Table 2). On the other hand, there was a significantly higher rate of early-onset neonatal sepsis in the non-exposed group. This was potentially due to maternal intrapartum antibiotic exposure, with a significantly higher proportion of the “exposed” group receiving antibiotics around the time of labor and delivery (81.6% vs. 51.9%, Barnard test, S = −2.93, p = 0.002). No other differences were observed in neonatal outcomes.
MiR-29b and clinical outcomes
Expression of miR-29b was not normally distributed, so Kruskal–Wallis test was applied to assess miR-29b with categorical clinical outcomes. MiR-29b levels were measured on all 92 cord blood plasma samples and tested for correlations between miR-29b levels and placental pathology, specifically funisitis and chorioamnionitis, as well as fetal and neonatal outcomes: fetal growth restriction, NEC, ROP, IVH, PVL, CP, and BPD (Table 3). MiR-29b CT values were higher in cases considered “exposed” (mean = 11.51, SD = 2.53) than in “non-exposed” (mean = 10.97, SD = 1.52) (Kruskal–Wallis rank-sum test, d.f. = 1, χ2 = 5.29, p = 0.02), indicating that there is a greater number of miR-29b transcripts in the non-exposed group. We also observed that miR-29b CT levels were greater in infants born by spontaneous PTB (mean = 11.25, SD = 1.76) than those whose PTB was medically indicated (mean = 10.51, SD = 2.42) (Kruskal–Wallis rank-sum test, d.f. = 3, χ2 = 10.28, p = 0.02), again indicating fewer miR-29b transcripts in the spontaneous PTB group. Similar findings were observed with umbilical cord funisitis, with higher CT values in the funisitis group compared to the non-funisitis group, indicating lower levels of miR-29b transcript in the group with diagnosed funisitis (Kruskal–Wallis rank-sum test, d.f. = 1, χ2 = 4.17, p = 0.04).
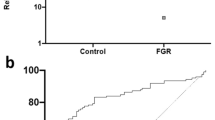
For neonatal outcomes, high CT values for miR-29b indicating lower transcript numbers were observed for infants diagnosed with CP (mean = 11.93, SD = 0.57) than those who were not (mean = 10.92, SD = 2.12) (t test, d.f. = 12, t = 2.34, p = 0.02) (Table 3). A reverse correlation was observed for infants with small for gestational age (SGA) with lower miR-29b CT values and thus higher transcript numbers in the infants diagnosed with SGA (Kruskal–Wallis rank-sum test, d.f. = 1, χ2 = 6.38, p = 0.01) (Table 3).
Venous blood samples collected at 36–40 weeks postmenstrual age from 18 of the original subjects were also analyzed (n = 18 samples). As shown in Table 4, lower miR-29b CT values and higher transcript levels in these samples were associated with IVH for cases with (mean = 4.27, SD = 3.27) compared to cases without (mean = 8.19, SD = 1.56) (Kruskal–Wallis rank-sum test, χ2 = 4.00, p = 0.04). No other morbidities tested were associated with miR-29 levels at this time point, including BPD.
DISCUSSION
More than 50% of deliveries at <30 weeks gestation are associated with intrauterine or maternal inflammation.30 In addition, these infants are at risk for increased incidence of neonatal morbidities and poor long-term outcomes.31,32,33 Those who survive beyond infancy are at greatest risk for developing adult disease; in fact, infection-related PTB has been associated with the development of early-onset sepsis and neonatal morbidities, including NEC, ROP, IVH, PVL, CP, and BPD.34,35,36
Previous studies to identify epigenetic changes that occur due to prematurity and/or inflammation have found an association between miR-29b levels and development of BPD in human neonates. Specifically, decreased circulating miR-29b levels from plasma in the first week of life are found in those infants who are subsequently diagnosed with BPD at 36 weeks corrected GA. A significant inverse association was demonstrated between BPD severity and miR-29b level shortly after birth, suggesting that decreased miR-29b early in life may predict or contribute to disease severity.4 Similar findings were recapitulated in animal models.4,12
This current investigation was designed to identify whether cord blood miR-29b levels were associated with perinatal/neonatal inflammation and thus increased risk for neonatal morbidities. Using measures of Hp&HpRP and IL-6, infants were designated as “exposed” vs. “non-exposed’ to antenatal inflammation as described in prior studies from our group.22,24,37 This current study identified a negative correlation with miR-29b levels and exposed infants. Similarly, we observed a negative correlation between miR-29b levels and births classified as spontaneous PTB. Both criteria, “exposed” status and spontaneous nature of PTB, have been linked to intrauterine inflammation and agree with our previous findings of decreased miR-29b in response to inflammation.4
Prior studies have reported correlations between amniotic fluid or blood levels of IL-6 and the relative severity of intrauterine inflammation.37 Negative correlations were identified between miR-29b and IL-6 levels in the infant cord blood and clinical inflammatory conditions, including funisitis. Buhimschi et al.38 has reported associations between maternal funisitis and infant sepsis. Our findings further support the hypothesis that miR-29b levels are suppressed by intrauterine inflammation and early suppression may be involved in altering developmental pathways.
Our earlier publication reported a strong association between decreased miR-29b levels and development of BPD in infant blood samples obtained during the first week of life.4 We did not observe a similar correlation in cord blood samples. This may be due to the timing of development of BPD, as BPD is not clinically diagnosed until 36 weeks postmenstrual age. Moreover, postnatal rather than antenatal factors may be important determinants of risk for BPD than for neurological abnormalities.39 We did observe associations between miR-29b levels in cord blood and neurological morbidities, specifically CP. In addition, miR-29b levels in the older infants (~36–40 weeks postmenstrual age) were also associated with diagnosis of neurological morbidities, specifically IVH. The vast majority of IVHs occur in the first 3 days of life, so the increased miR-29b levels at 36–40 weeks postmenstrual age do not play a role in diagnosis of IVH, but may represent a biomarker of previous injury.40 A previous study revealed elevated plasma levels of miR-29b in patients diagnosed with intracerebral hemorrhage, compared to controls.41
MiR-based therapies are being explored as novel approaches to treatment for other diseases, including metabolic disorders, cardiovascular disease, cancer, and infections.42,43 Using our murine model of perinatal inflammation, we demonstrated improved alveolarization and attenuated defects in matrix protein expression and localization by supplementing miR-29b on postnatal day 3.4 Our data indicate that miR-29b is associated with inflammation in the infants, and that further investigation of the pathways associated with miR-29b may provide an avenue for therapeutic development.
CONCLUSION
Lower miR-29b levels in cord blood correlate with clinical and biochemical markers of inflammation, including IL-6 and Hp. We found an association between miR-29b levels with neurologic morbidities, including IVH and CP. There was no significant association between miR-29b levels and BPD at the time points tested. These data provide promising results that further investigation of miR-29b in the fetus and neonate will allow for early diagnosis or therapeutic intervention for those at highest risk for morbidities.
References
Preterm Birth. http:who.int/news-room/fact-sheets/detail/preterm-birth. (2018).
Premature Birth Report Cards. www.marchofdimes.org/mission/reportcard.aspx. (2018).
Glass, H. C. et al. Outcomes for extremely premature infants. Anesth. Analg. 120, 1337–1351 (2015).
Durrani-Kolarik, S. et al. miR-29b supplementation decreases expression of matrix proteins and improves alveolarization in mice exposed to maternal inflammation and neonatal hyperoxia. Am. J. Physiol. Lung Cell. Mol. Physiol. 313, L339–L349 (2017).
Beermann, J., Piccoli, M. T., Viereck, J. & Thum, T. Non-coding RNAs in development and disease: background, mechanisms, and therapeutic approaches. Physiol. Rev. 96, 1297–1325 (2016).
Stolzenburg, L. R. & Harris, A. The role of microRNAs in chronic respiratory disease: recent insights. Biol. Chem. 399, 219–234 (2018).
Quinlan, S., Kenny, A., Medina, M., Engel, T. & Jimenez-Mateos, E. M. MicroRNAs in neurodegenerative diseases. Int. Rev. Cell. Mol. Biol. 334, 309–343 (2017).
Wojciechowska, A., Braniewska, A. & Kozar-Kaminska, K. MicroRNA in cardiovascular biology and disease. Adv. Clin. Exp. Med. 26, 865–874 (2017).
Tang, Y. et al. The effect of H19-miR-29b interaction on bleomycin-induced mouse model of idiopathic pulmonary fibrosis. Biochem. Biophys. Res. Commun. 479, 417–423 (2016).
Yamada, Y. et al. Novel form of miR-29b suppresses bleomycin-induced pulmonary fibrosis. PLoS ONE 12, e0171957 (2017).
Tang, K., Zhao, J., Xie, J. & Wang, J. Decreased miR-29b expression is associated with airway inflammation in chronic obstructive pulmonary disease. Am. J. Physiol. Lung Cell. Mol. Physiol. 316, L621–L629 (2019).
Velten, M. et al. Prenatal inflammation exacerbates hyperoxia-induced functional and structural changes in adult mice. Am. J. Physiol. Regul. Integr. Comp. Physiol. 303, R279–R290 (2012).
Velten, M., Heyob, K. M., Rogers, L. K. & Welty, S. E. Deficits in lung alveolarization and function after systemic maternal inflammation and neonatal hyperoxia exposure. J. Appl Physiol. (1985) 108, 1347–1356 (2010).
Cushing, L. et al. Disruption of miR-29 leads to aberrant differentiation of smooth muscle cells selectively associated with distal lung vasculature. PLoS Genet. 11, e1005238 (2015).
Montgomery, R. L. et al. MicroRNA mimicry blocks pulmonary fibrosis. EMBO Mol. Med. 6, 1347–1356 (2014).
Ng, P. C. et al. Early prediction of sepsis-induced disseminated intravascular coagulation with interleukin-10, interleukin-6, and RANTES in preterm infants. Clin. Chem. 52, 1181–1189 (2006).
Romagnoli, C. et al. Plasma levels of interleukin-6 and interleukin-10 in preterm neonates evaluated for sepsis. Eur. J. Pediatr. 160, 345–350 (2001).
Yoon, B. H. et al. Interleukin-6 concentrations in umbilical cord plasma are elevated in neonates with white matter lesions associated with periventricular leukomalacia. Am. J. Obstet. Gynecol. 174, 1433–1440 (1996).
Goepfert, A. R. et al. Umbilical cord plasma interleukin-6 concentrations in preterm infants and risk of neonatal morbidity. Am. J. Obstet. Gynecol. 191, 1375–1381 (2004).
Rausen, A. R., Gerald, P. S. & Diamond, L. K. Haptoglobin patterns in cord blood serums. Nature 191, 717 (1961).
Kanakoudi, F. et al. Serum concentrations of 10 acute-phase proteins in healthy term and preterm infants from birth to age 6 months. Clin. Chem. 41, 605–608 (1995).
Buhimschi, C. S., Eunice Kennedy Shriver National Institute of Child H, Human Development Maternal-Fetal Medicine Units N. et al. Cord blood haptoglobin, cerebral palsy and death in infants of women at risk for preterm birth: a secondary analysis of a randomised controlled trial. EClinicalMedicine 9, 11–18 (2019).
Tseng, C. F., Lin, C. C., Huang, H. Y., Liu, H. C. & Mao, S. J. Antioxidant role of human haptoglobin. Proteomics 4, 2221–2228 (2004).
Buhimschi, C. S. et al. Proteomics mapping of cord blood identifies haptoglobin “switch-on” pattern as biomarker of early-onset neonatal sepsis in preterm newborns. PLoS ONE 6, e26111 (2011).
McCarthy, M. E. et al. Identification of haptoglobin switch-on status in archived placental specimens indicates antenatal exposure to inflammation and potential participation of the fetus in triggering preterm birth. Placenta 62, 50–57 (2018).
Barnard, G. A. Significance tests for 2 X 2 tables. Biometrika 34, 123–138 (1947).
Rabbee, N., Coull, B. A., Mehta, C., Patel, N. & Senchaudhuri, P. Power and sample size for ordered categorical data. Stat. Methods Med. Res. 12, 73–84 (2003).
Kruskal WHaW, W. A. Use of ranks in one-criterion variance analysis. J. Am. Stat. Assoc. 47, 583–621 (1952).
Committee on Obstetric P. Committee opinion no. 712: intrapartum management of intraamniotic infection. Obstet. Gynecol. 130, e95–e101 (2017).
Jobe, A. H. & Bancalari, E. Bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. 163, 1723–1729 (2001).
Luu, T. M., Rehman Mian, M. O. & Nuyt, A. M. Long-term impact of preterm birth: neurodevelopmental and physical health outcomes. Clin. Perinatol. 44, 305–314 (2017).
Patel, R. M. Short- and long-term outcomes for extremely preterm infants. Am. J. Perinatol. 33, 318–328 (2016).
Nuyt, A. M., Lavoie, J. C., Mohamed, I., Paquette, K. & Luu, T. M. Adult consequences of extremely preterm birth: cardiovascular and metabolic diseases risk factors, mechanisms, and prevention avenues. Clin. Perinatol. 44, 315–332 (2017).
Shi, W., Bellusci, S. & Warburton, D. Lung development and adult lung diseases. Chest 132, 651–656 (2007).
Wong, P. M. et al. Emphysema in young adult survivors of moderate-to-severe bronchopulmonary dysplasia. Eur. Respir. J. 32, 321–328 (2008).
Bhandari, V. et al. Cord blood erythropoietin and interleukin-6 for prediction of intraventricular hemorrhage in the preterm neonate. J. Matern. Fetal Neonatal Med. 24, 673–679 (2011).
Buhimschi, C. S. et al. Fetal inflammatory response in women with proteomic biomarkers characteristic of intra-amniotic inflammation and preterm birth. BJOG 116, 257–267 (2009).
Buhimschi, C. S. et al. Proteomic biomarkers of intra-amniotic inflammation: relationship with funisitis and early-onset sepsis in the premature neonate. Pediatr. Res. 61, 318–324 (2007).
Nayeri, U. A., Buhimschi, C. S., Zhao, G., Buhimschi, I. A. & Bhandari, V. Components of the antepartum, intrapartum, and postpartum exposome impact on distinct short-term adverse neonatal outcomes of premature infants: a prospective cohort study. PLoS ONE 13, e0207298 (2018).
Ment, L. R. et al. Intraventricular hemorrhage in the preterm neonate: timing and cerebral blood flow changes. J. Pediatr. 104, 419–425 (1984).
Guo, D. et al. Alteration in abundance and compartmentalization of inflammation-related miRNAs in plasma after intracerebral hemorrhage. Stroke 44, 1739–1742 (2013).
Samanta, S. et al. MicroRNA: a new therapeutic strategy for cardiovascular diseases. Trends Cardiovasc. Med. 26, 407–419 (2016).
Hayes, J., Peruzzi, P. P. & Lawler, S. MicroRNAs in cancer: biomarkers, functions and therapy. Trends Mol. Med. 20, 460–469 (2014).
Acknowledgements
We acknowledge the Ohio Perinatal Research Network Perinatal Research Repository for providing biospecimens and data for the project. These studies were support by NIH HD0880833.
Author information
Authors and Affiliations
Contributions
L.R.P. interpreted data and wrote the manuscript; S.V. performed biochemical analyses; C.W.B. performed statistical analyses of data; I.A.B. assisted in conceiving the idea, provided cord blood samples, and edited the manuscript; C.S.B. assisted in conceiving the idea, and edited the manuscript; L.K.R. conceived the idea, oversaw all analyses, and edited final draft of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
Informed consent was obtained from the mother of the infants included in this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Pavlek, L.R., Vudatala, S., Bartlett, C.W. et al. MiR-29b is associated with perinatal inflammation in extremely preterm infants. Pediatr Res 89, 889–893 (2021). https://doi.org/10.1038/s41390-020-0943-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0943-1