Abstract
Background
Kawasaki disease (KD) is an acute and systemic vasculitis whose etiology remains unclear. The most crucial complication is the formation of coronary artery aneurysm (CAA). Annexin A1 (ANXA1) is an endogenous anti-inflammatory agent and pro-resolving mediator involved in inflammation-related diseases. This study sought to investigate the serum ANXA1 levels in KD patients and further explore the relationship between ANXA1 and CAA, as well as additional clinical parameters.
Methods
Serum samples were collected from 95 KD patients and 39 healthy controls (HCs). KD patients were further divided into two groups: KD with CAAs (KD-CAAs) and KD non-CAAs (KD-NCAAs). Serum levels of ANXA1 and interleukin-6 (IL-6) were determined using enzyme-linked immunosorbent assays.
Results
Serum ANXA1 levels in the KD group were significantly lower than in the HC group. In particular, serum ANXA1 levels were substantially lower in the KD-CAA groups. Moreover, serum ANXA1 levels were positively correlated with N%, C-reactive protein (CRP), and IL-6 but negatively correlated with L% in the KD group. Positive correlations between serum ANXA1 levels and erythrocyte sedimentation rate (ESR), IL-6, and D-dimer (DD) were observed in the KD-CAA group.
Conclusions
ANXA1 may be involved in the development of KD, and downregulation of ANXA1 may lead to the hypercoagulability seen in KD.
Impact
-
For the first time, it was demonstrated that serum ANXA1 levels were significantly decreased in Kawasaki disease with coronary artery aneurysms.
-
ANXA1 might be involved in the acute phase of Kawasaki disease.
-
Low serum concentrations of ANXA1 might lead to the hypercoagulability stage in Kawasaki disease.
-
ANXA1 might be a potential therapeutic target for patients with Kawasaki disease.
Similar content being viewed by others
Introduction
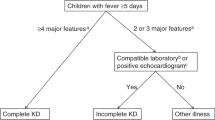
More than 50 years have passed since Tomisaku Kawasaki first reported Kawasaki disease (KD) in 1967.1 However, the etiology of this disease remains unclear.2 KD is characterized by the presence of acute, self-limiting vasculitis and predominantly occurs in children aged <5 years.3 Its major clinical manifestations are persistent fever, rash, cervical lymphadenopathy, conjunctivitis, and mucocutaneous inflammation.2 The development of coronary artery lesions (CALs) is the most critical complication of KD, rendering it the leading cause of pediatric acquired cardiac disease in the developed countries.2 Currently, the predominant treatment for KD patients is intravenous immunoglobulin (IVIG) therapy in combination with an aspirin regimen.2 However, approximately 15–25% children without effective treatment or delayed treatment develop CALs or coronary artery aneurysms (CAAs), which are high risk factors for myocardial infarction, ischemia, and even rupture.4 Previous research has shown that neutrophils participate in the initial process of vasculitis in KD.2 In the acute phase, neutrophils mediate the development of necrotizing arteritis, which primarily affects medium-sized blood vessels.5 In this stage, significant neutrophils infiltrate into the arterial wall and further destroy the vascular smooth muscle, leading to severe lesions on the vessels and leaving only a thin rim of adventitia in the affected area.5,6 Necrotizing arteritis can lead to the development of CAAs, which is a high risk factor for the formation of thrombosis and vessel rupture under the hypercoagulable state that occurs in KD patients.5
Annexin A1 (ANXA1), also known as lipocortin 1, belongs to the Annexin protein family.7 ANXA1 is widely distributed in mammals and primarily exists in the cytoplasm and cell membrane of neutrophils, lymphocytes, and endothelial cells.8 However, it can also be secreted into the circulation through paracrine or autocrine signaling pathways.9 ANXA1 exhibits various biological functions but is mostly reported as an anti-inflammatory and pro-resolution cytokine.10 ANXA1 can promote the detachment of neutrophils from the vascular endothelium and inhibit their transmigration by shedding of L-selectin, further regulating the inflammatory responses mediated by neutrophils.11,12 ANXA1 can be induced by glucocorticoid and further regulates interleukin (IL)-6 via glucocorticoid-induced leucine zipper (GILZ).13 However, IL-6 can also directly promote the expression and translocation of ANXA1.14 These evidences indicate that there is a connection between ANXA1 and IL-6 in regulating the inflammatory response. In addition, previous research has demonstrated that ANXA1 acts as a protective cytokine in myocardial infarction and atherosclerosis via inhibition of the inflammatory response.9,15,16 Taken together, we propose that the low levels of ANXA1 may be an important cause for the excessive inflammatory response mediated by neutrophils that ultimately leads to the formation of CAAs in KD patients. Moreover, ANXA1 can alter platelet phenotype from pro-pathogenic to regulatory and prevent platelets from aggregating or causing thrombosis in patients with ischemic–reperfusion reinjury,17,18 and the low serum concentrations of ANXA1 can lead to a hypercoagulable stage.18,19
Methods
Subjects’ recruitment and sample collection
KD patients were enrolled from the Children’s Hospital of Chongqing Medical University in Chongqing, China. Our rigorous diagnostic criteria was based on the guidelines proposed by the Japanese Kawasaki Disease Research Committee.20 A total of 95 children with KD were recruited (male = 57, female = 38, age = 2.686 ± 1.956 years) for the KD group and 39 healthy children (male = 21, female = 18, age = 2.784 ± 1.363 years) were recruited based on physical examinations to serve as the healthy controls (HCs) group. All the enrolled children were excluded free of inflammatory, immune, metabolic, and hematological diseases, as well as other heart diseases.
Echocardiography was performed 1 day before IVIG treatment in children with KD. Subjects with a z-value >2.5 were distributed to the KD with CAA group (KD-CAAs, n = 45), while those with z-value <2.5 were distributed to the KD non-CAA group (KD-NCAAs, n = 50).21
All venous blood samples were collected before treatment with IVIG or anticoagulants. The samples were centrifuged at 3000 rpm for 10 min to separate the serum. After that, the serum samples were immediately stored at −80 °C. The collection of serum from healthy children used the same procedure.
This study was approved by the Ethics Committee of Children’s Hospital, Chongqing Medical University and informed consent was obtained from the patients’ parents or appropriate guardians.
Measurement of serum levels of ANXA1, IL-6, and general laboratory variables
Serum levels of ANXA1 and IL-6 were measured using enzyme-linked immunosorbent assays (ELISAs) according to the manufacturer’s instructions (RayBiotech, USA).
General laboratory variables of the samples were also measured, including white blood cell count (WBC), red blood cell count (RBC), hemoglobin (Hb), platelet counts (PLT), percentage of neutrophils (N%), percentage of leukomonocytes (L%), C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), procalcitonin (PCT), aspartate aminotransferase (AST), alanine aminotransferase (ALT), and creatine kinase-MB (CK-MB), in addition to blood coagulation parameters such as prothrombin time (PT), activated partial thromboplastin time (APTT), fibrinogen (FIB), thrombin time (TT), and D-dimer (DD).
Statistical analysis
Statistical analyses were completed using the SPSS25.0 software for Windows (SPSS, Chicago, IL). To compare the differences between groups, Student’s t tests were used for data that displayed normal distribution, whereas data that failed the normality assumption were analyzed via the nonparametric Mann–Whitney U test. Chi-square test was used to compare frequencies between groups. Spearman rank correlation was used to analyze the association between serum ANXA1 levels and various clinical parameters. All values are shown as mean ± standard deviation, median (P25, P75), or number and percentage (n, %). A P value <0.05 was used as a threshold for determining statistical significance.
Results
Serum ANXA1 levels
There were no significant differences in gender or age between the KD and HC groups (P > 0.05). As shown in Fig. 1, serum ANXA1 levels in the KD group (39.37 ng/ml (15.36, 72.79), n = 95) were significantly lower than the levels in the HC group (83.39 ng/ml (42.49, 199.60), n = 39) (P = 0.018) and substantially lower in the KD-CAA group (22.64 ng/ml (6.43, 45.90), n = 45) than in the KD-NCAA group (50.69 ng/ml (15.96, 122.60), n = 50) (P = 0.047).
General laboratory variables and IL-6 levels in the KD-CAA and KD-NCAA groups
As shown in Table 1, there were no significant differences in IVIG treatment, WBC, RBC, Hb, PLT, N%, L%, CRP, ESR, PCT, AST, ALT, or CK-MB between the KD-CAA and KD-NCAA groups (P > 0.05). However, compared to the KD-NCAA group, the serum level of IL-6 was significantly higher in the KD-CAA group (P < 0.05).
Correlation between serum ANXA1 levels and general laboratory variables in the KD group
In the KD group, IVIG treatment, WBC, RBC, Hb, PLT, ESR, PCT, AST, ALT, and CK-MB were not significantly correlated with serum ANXA1 levels (P > 0.05). However, serum ANXA1 levels were positively correlated with N%, CRP, and IL-6 levels and negatively correlated with L% in the KD group (P < 0.05; Table 2).
Correlation between serum ANXA1 levels and general laboratory variables in the KD-CAA and KD-NCAA groups
Serum ANXA1 levels were not significantly correlated with IVIG treatment, WBC, RBC, Hb, PLT, N%, L%, PCT, AST, ALT, or CK-MB (P > 0.05) in KD-CAA group and were positively correlated with ESR and IL-6 (P < 0.05).
In the KD-NCAA group, serum ANXA1 levels were positively correlated with N%, CRP, and IL-6 and negatively correlated with L% (P < 0.05; Table 3).
Correlation between serum ANXA1 levels and blood coagulation parameters
In the KD and KD-NCAA groups, there was a significant positive correlation between serum ANXA1 levels and FIB (P < 0.05). In the KD-CAA group, there was a significant positive correlation between serum ANXA1 levels and DD (P < 0.05; Table 4).
Discussion
ANXA1 belongs to the Annexin family of proteins, which are characterized by a highly conserved Ca2+-binding site in the protein core and an unique NH2-terminal domain.7 Certain members of the Annexin family are reported to be involved in a variety of diseases as an inhibitor of neutrophil migration and blood coagulation.7 ANXA1 could interfere with the migration and chemotaxis of neutrophils to endothelial cells and further regulating the inflammatory response mediated by neutrophils.11 Previous studies have shown that neutrophils was important in the formation of CAAs during the acute phase of KD.6 In addition, ANXA1 can inhibit platelet function to prevent aggregation in circulation, enabling ANXA1 to serve as a resolving agent.18 In this study, we sought to measure the serum ANXA1 concentration in the KD patients and further explore the relationship between ANXA1 and the formation of CAAs.
In this study, we found that serum ANXA1 levels in the KD group were significantly lower than in the HC group. In particular, the serum ANXA1 levels were substantially lower in the KD-CAA group compared to the KD-NCAA group. Correlation analysis showed that serum ANXA1 levels were positively correlated with N%, CRP, IL-6 levels, and FIB but negatively correlated with L% in the KD group. In the KD-CAA group, serum ANXA1 levels were positively correlated with ESR, IL-6 levels, and DD, whereas in the KD-NCAA group, serum ANXA1 levels were positively correlated with N%, CRP, IL-6 levels, and FIB but negatively correlated with L%.
ANXA1 has been primarily reported as a critical anti-inflammatory and pro-resolving protein cytokine, which exhibited various biological functions.11,19 It has been shown that ANXA1, via ANXA/FPR2 signaling, negatively regulates Rap-1-dependent integrin activation in the recruitment of monocytes and neutrophils to protect coronary endothelial cells in atherosclerosis.15 Downregulation of ANXA1 led to more severe coronary lesions in the mouse model for atherosclerosis.15,22 Furthermore, in sepsis and other inflammatory-related diseases, ANXA1 was involved in regulating the excessive inflammatory response by preventing neutrophils from migrating and adhering to the endothelial cells.23,24 ANXA1 also acts as a protective cytokine in the development process of ischemia–reperfusion injury and myocardial infarction. ANXA1 can regulate abnormal platelets and promote thrombus dissolution, thus protecting the cardiovascular system from injury.17,18,19 The purpose of this study was to investigate the association between ANXA1 and KD and uncover any connections between ANXA1 and the formation of CAAs. Here we found that serum ANXA1 levels in the KD group were significantly lower than those in the HC group. This result and above evidences indicated that ANXA1 might be involved in the development process of KD, and the low serum concentrations of ANXA1 might be a cause for the excessive inflammatory responses characteristic of KD. In addition, some studies have shown that IL-6 and other inflammatory cytokines synergistically mediated the development of vasculitis during the acute phase of KD.25 ANXA1 could inhibit the expression of IL-6 via GILZ;13 low serum ANXA1 levels might lead to the increased expression of IL-6. Interestingly, our result was consistent with previous research that serum IL-6 levels were higher in KD patients compared to healthy controls.26 Furthermore, our study also found that serum ANXA1 levels were positively correlated with CRP and IL-6 levels in the KD group. CRP and IL-6 levels were strongly correlated with the degree of inflammation. Excessive inflammatory response could induce the expression of ANXA1 to maintain homeostasis.24 Solito et al. also suggest that IL-6 could directly promote the expression of ANXA1 to regulate inflammation.14 Taken together, ANXA1 and IL-6 might synergistically participate in the development of vasculitis in KD, and low serum concentrations of ANXA1 might lead to more severe inflammatory responses in KD.
KD predominantly affects the systemic medium-sized blood vessels. The most critical complication of this disease is CAAs.2 Our results indicated that ANXA1 might be a key factor involved in the development process of CAAs. First, we found that serum ANXA1 levels in the KD-CAA group were significantly lower than in the KD-NCAA group. In the acute phase of KD, a large amount of neutrophils infiltrate into the vascular wall, which would mediate severe lesions on endothelial cells and smooth muscle cells of the vessels.6 Under this condition, affected vessels were left with only a weak adventitia and were much more susceptible to CAA formation.5 Previous studies demonstrated that ANXA1 plays an important role in modulating the chemotaxis and adhesion of neutrophils to vascular endothelial cells.11 The above evidences indicated that low serum ANXA1 levels might be a reason for the excessive inflammatory response experienced by the vascular wall. Furthermore, our study found that, in the KD-CAA group, serum ANXA1 levels were positively correlated with ESR and IL-6 levels. Previous research has confirmed that IL-6 is involved in the development process of CALs in KD.26 ESR is thought to be a predictive marker for the occurrence of CAAs in KD patients.27 Our observation that serum ANXA1 levels were positively correlated with these CAL-related inflammation parameters indicated that ANXA1 might be involved in the development process of CAAs and would be stimulated in the excessive inflammation state via a feedback mechanism.14 This phenomenon was also observed in the KD-NCAA group, where we observed that patient serum ANXA1 concentrations were positively correlated with inflammation-related parameters including N%, CRP, and IL-6 levels. This further confirmed that ANXA1 would be stimulated by the inflammatory factors and act as an anti-inflammatory cytokine.11,13,14 Finally, previous studies have shown that ANXA1 was involved in the atherosclerosis and myocardial infarction as a protective factor via preventing inflammatory cells from infiltrating into the vascular walls.15,28 In a mouse model of atherosclerosis, ANXA1 knockout led to an increased propensity for presenting coronary artery injuries.22,29,30 Taken together, all the above evidences indicates that the low serum ANXA1 levels might be a key factor for CAA formation in KD patients.
In a multicenter, prospective randomized, controlled trial in Japan, Kobayashi et al. demonstrated that, compared with IVIG alone, treatment that combined IVIG with prednisolone significantly reduced the incidence of CALs in the acute phase of KD.31 Wardle et al. indicated that the use of steroids could effectively attenuate the development of CALs in the acute phase of KD and further reduced the duration of clinical symptoms as well as hospital stay.32 ANXA1 is a glucocorticoid-regulated protein. Glucocorticoid can bind to cytoplasmic glucocorticoid receptors, which would further promote the expression of ANXA1 genes. This would cause a large amount of ANXA1 to be secreted into circulation to regulate the inflammation mediated by neutrophils.12 In addition, ANXA1 was also involved in regulating IL-6 and other inflammatory cytokines.13 This may be one of the potential mechanisms that glucocorticoids could attenuate the development of CALs in KD, and ANXA1 might be a new therapeutic target for KD patients, especially those with CALs or CAAs. However, further research is still needed to verify and further elucidate this potential treatment option.
ANXA1 was also involved in regulating coagulation function. Senchenkova et al. indicated that ANXA1 was able to inhibit the activation and aggregation of platelets and alter platelet phenotype from pathological to regulatory via the Fpr2/ALX signaling pathway.18 In our study, we found a significant positive correlation between serum ANXA1 levels and FIB in the KD group, as well as a significant positive correlation with DD in the KD-CAA group. DD and FIB are both clinical parameters that reflect the degree of hypercoagulability. Previous studies demonstrated that ANXA1 acts as a protective factor in ischemia–reperfusion injury and myocardial infarction via platelet regulation and inhibition of inflammatory responses.16,17,18 In a mouse model of ischemia–reperfusion injury, decreased expression of ANXA1 led to an increase in platelet adhesion to the endothelium and more severe vascular damage.18 Moreover, our results showed that serum ANXA1 levels in the KD group were significantly lower than those in the HC group, indicating that low serum ANXA1 might be related to the hypercoagulability in KD patients.
In conclusion, our study was the first to demonstrate that serum ANXA1 levels in KD patients are significantly lower than those in healthy controls. Serum ANXA1 levels were substantially decreased in KD patients with CAAs compared to those without. In addition, serum ANXA1 concentrations were positively correlated with ESR and IL-6 levels in the KD-CAA group. These results indicate that ANXA1 might relate to the development process of KD, and low serum ANXA1 concentrations might be one of the mechanisms through which CAAs develop. ANXA1 may possess the potential to serve as a new therapeutic target for patients with KD, especially those with CALs or CAAs. Furthermore, our study showed that serum ANXA1 levels were positively correlated with DD and FIB in the KD-CAA and KD-NCAA groups, respectively. These coagulation-related clinical parameters could reflect the degree of hypercoagulability, indicating that low serum levels of ANXA1 might lead to hypercoagulability in KD patients. However, our study also has some limitations and further studies are required to investigate the way signaling pathway of ANXA1 participates in the development process of KD and the formation of CAAs.
References
Burns, J. C. History of the worldwide emergence of Kawasaki disease. Int. J. Rheum. Dis. 21, 13–15 (2018).
Newburger, J. W., Takahashi, M. & Burns, J. C. Kawasaki Disease. J. Am. Coll. Cardiol. 67, 1738–1749 (2016).
Nakamura, Y. Kawasaki disease: epidemiology and the lessons from it. Int. J. Rheum. Dis. 21, 16–19 (2018).
Kato, H. et al. Fate of coronary aneurysms in Kawasaki disease: serial coronary angiography and long-term follow-up study. Am. J. Cardiol. 49, 1758–1766 (1982).
Shulman, S. T. & Rowley, A. H. Kawasaki disease: insights into pathogenesis and approaches to treatment. Nat. Rev. Rheumatol. 11, 475–482 (2015).
Orenstein, J. M. et al. Three linked vasculopathic processes characterize Kawasaki disease: a light and transmission electron microscopic study. PLoS ONE 7, e38998 (2012).
Gerke, V. & Moss, S. E. Annexins: from structure to function. Physiol. Rev. 82, 331–371 (2002).
Perretti, M. et al. Annexin I is stored within gelatinase granules of human neutrophil and mobilized on the cell surface upon adhesion but not phagocytosis. Cell Biol. Int. 24, 163–174 (2000).
Purvis, G. S. D., Solito, E. & Thiemermann, C. Annexin-A1: therapeutic potential in microvascular disease. Front. Immunol. 10, 938 (2019).
Perretti, M. & Flower, R. J. Annexin 1 and the biology of the neutrophil. J. Leukoc. Biol. 76, 25–29 (2004).
Perretti, M. & D’Acquisto, F. Annexin A1 and glucocorticoids as effectors of the resolution of inflammation. Nat. Rev. Immunol. 9, 62–70 (2009).
Yang, Y. H., Morand, E. & Leech, M. Annexin A1: potential for glucocorticoid sparing in RA. Nat. Rev. Rheumatol. 9, 595–603 (2013).
Yang, Y. H., Aeberli, D., Dacumos, A., Xue, J. R. & Morand, E. F. Annexin-1 regulates macrophage IL-6 and TNF via glucocorticoid-induced leucine zipper. J. Immunol. 183, 1435–1445 (2009).
Solito, E., de Coupade, C., Parente, L., Flower, R. J. & Russo-Marie, F. IL-6 stimulates annexin 1 expression and translocation and suggests a new biological role as class II acute phase protein. Cytokine 10, 514–521 (1998).
Butcher, M. J. & Galkina, E. V. wRAPping up early monocyte and neutrophil recruitment in atherogenesis via Annexin A1/FPR2 signaling. Circ. Res. 116, 774–777 (2015).
Qin, C. et al. Cardioprotective potential of annexin-A1 mimetics in myocardial infarction. Pharmacol. Ther. 148, 47–65 (2015).
Ansari, J., Kaur, G. & Gavins, F. N. E. Therapeutic potential of Annexin A1 in ischemia reperfusion injury. Int. J. Mol. Sci. 19, E1211 (2018).
Senchenkova, E. Y. et al. Novel role for the AnxA1-Fpr2/ALX signaling axis as a key regulator of platelet function to promote resolution of inflammation. Circulation 140, 319–335 (2019).
Zhao, C., Zhang, B., Jiang, J., Wang, Y. & Wu, Y. Up-regulation of ANXA1 suppresses polymorphonuclear neutrophil infiltration and myeloperoxidase activity by activating STAT3 signaling pathway in rat models of myocardial ischemia-reperfusion injury. Cell Signal. 62, 109325 (2019).
JCS Joint Working Group. Guidelines for diagnosis and management of cardiovascular sequelae in Kawasaki disease (JCS 2013). Digest version. Circ. J. 78, 2521–2562 (2014).
Manlhiot, C., Millar, K., Golding, F. & McCrindle, B. W. Improved classification of coronary artery abnormalities based only on coronary artery z-scores after Kawasaki disease. Pediatr. Cardiol. 31, 242–249 (2010).
Drechsler, M. et al. Annexin A1 counteracts chemokine-induced arterial myeloid cell recruitment. Circ. Res. 116, 827–835 (2015).
Gavins, F. N. et al. Leukocyte recruitment in the brain in sepsis: involvement of the annexin 1-FPR2/ALX anti-inflammatory system. FASEB J. 26, 4977–4989 (2012).
Tsai, W. H., Li, I. T., Yu, Y. B., Hsu, H. C. & Shih, C. H. Serial changes in plasma annexin A1 and cortisol levels in sepsis patients. Chin. J. Physiol. 57, 1–7 (2014).
Feng, S., Su, Y., Luo, L., Jing, F. & Yi, Q. Serum levels of C1q/tumor necrosis factor-related protein-1 in children with Kawasaki disease. Pediatr. Res. 83, 999–1003 (2018).
Liu, R., He, B., Gao, F., Liu, Q. & Yi, Q. Relationship between adipokines and coronary artery aneurysm in children with Kawasaki disease. Transl. Res. 160, 131–136 (2012).
Qiu, H. et al. Delayed intravenous immunoglobulin treatment increased the risk of coronary artery lesions in children with Kawasaki disease at different status. Postgrad. Med. 130, 442–447 (2018).
Qin, C. X. et al. Endogenous Annexin-A1 regulates haematopoietic stem cell mobilisation and inflammatory response post myocardial infarction in mice in vivo. Sci. Rep. 7, 16615 (2017).
Bergstrom, I. et al. Annexin A1 in blood mononuclear cells from patients with coronary artery disease: Its association with inflammatory status and glucocorticoid sensitivity. PLoS ONE 12, e0174177 (2017).
de Jong, R. J. et al. Protective aptitude of Annexin A1 in arterial neointima formation in atherosclerosis-prone mice-brief report. Arterioscler. Thromb. Vasc. Biol. 37, 312–315 (2017).
Kobayashi, T. et al. Efficacy of immunoglobulin plus prednisolone for prevention of coronary artery abnormalities in severe Kawasaki disease (RAISE study): a randomised, open-label, blinded-endpoints trial. Lancet 379, 1613–1620 (2012).
Wardle, A. J., Connolly, G. M., Seager, M. J. & Tulloh, R. M. Corticosteroids for the treatment of Kawasaki disease in children. Cochrane Database Syst. Rev. 1, CD011188 (2017).
Acknowledgements
We appreciate the recruited children for their kindness to support the development of medicine. This study was supported by Chongqing Municipal Education Commission under Grant: CYS19197.
Author information
Authors and Affiliations
Contributions
H.W. made substantial contribution to the conception and design of this study, acquisition of data, analysis of data, and drafting the article. Y.P. contributed to design of this study, interpretation of data, and revision of the article. Q.P. contributed to acquisition and interpretation of data. F.J. contributed to interpretation of data. M.Y. contributed to interpretation of data. Q.Y. made substantial contribution to revise the article critically for important intellectual content and final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Weng, H., Peng, Y., Pei, Q. et al. Decreased serum Annexin A1 levels in Kawasaki disease with coronary artery aneurysm. Pediatr Res 89, 569–573 (2021). https://doi.org/10.1038/s41390-020-0898-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0898-2