Abstract
Background
Immature gut motility in preterm neonates may be a risk factor for necrotizing enterocolitis (NEC). Using preterm pigs as a model for infants, we hypothesized that intestinal dysmotility precedes NEC development.
Methods
Eighty-five preterm pigs were fed increasing amounts of milk diets to induce NEC lesions, as detected at autopsy on day 5. Gut transit time was determined on day 4 by x-ray imaging after oral intake of contrast solution.
Results
No clinical or radiological signs of NEC were detected on day 4, but macroscopic NEC lesions were recorded in 59% of pigs (n = 50) on day 5. Relative to pigs without NEC (noNEC, n = 35), pigs with small intestinal lesions (siNEC, n = 18) showed delayed stomach emptying time (StEmpty) and time for contrast to reach cecum (ToCecum) already on day 4. Pigs with lesions only in colon (coNEC, n = 20) showed more diarrhea, shorter ToCecum time, but longer small intestinal emptying time (SiEmpty). ToCecum time predicted siNEC and coNEC lesions with a receiver-operator characteristic area under the curve of 78–81%.
Conclusions
Region-dependent changes in gut transit time is associated with early NEC development in preterm pigs. How gut dysmotility is related to NEC in preterm infants requires further investigations.
Impact
-
Using preterm pigs as a model for preterm infants, we show that gut transit time, using serial x-ray contrast imaging, was changed in individuals with NEC-like lesions before they showed the typical radiological signs of NEC. Thus prolonged transit time across the entire gut was recorded when NEC lesions appeared in the small intestine but not when lesions were detected only in the colon.
-
Until now, recordings of food transit have mainly investigated changes in the upper gut. Using serial x-rays, this study describes food transit across the entire gut and documents a region-dependent effect of NEC lesions on gut transit changes in preterm individuals.
-
The findings provide proof of concept for use of x-ray contrast imaging as a tool to monitor gut transit in preterm pigs as models for infants. Delayed passage across the entire gut may be an early sign of small intestinal NEC, at least in pigs. More studies are needed to confirm relations in infants. In the future, it might be possible to use x-ray contrast imaging in preterm infants to better understand gut motility in relation to early NEC progression and need for medical NEC treatment.
Similar content being viewed by others
Background
Normal gastrointestinal motility is required for continuous food passage and proper digestion of nutrients in both infants and adults. A well-coordinated intestinal motility pattern matures toward birth and depends on many factors, including the enteric nerve system (ENS), interstitial cells of Cajal, and intestinal smooth muscle cells.1 In human fetuses, spontaneous gut motility appears at 25 weeks’ gestation, but it remains immature until at least 36 weeks’ gestation, when migrating motor complexes (MMCs) appear.2 This may partly explain why very preterm infants (<32 weeks’ gestation) frequently develop signs of gut dysmotility, as observed by feeding intolerance, abdominal distention, and slow gastric emptying with enlarged gastric residuals (GRs).3,4
Very preterm infants have a high risk to develop necrotizing enterocolitis (NEC, up to 10% of hospitalized preterm infants), an acute gut inflammatory disease with high risk of co-morbidities and mortality.5 Enteral feeding and bacterial colonization are known risk factors of NEC, but a primary gut dysmotility has also been considered to predispose to NEC, considering the clinical and radiological signs of feeding intolerance in early stage of NEC, together with ENS abnormalities observed in late stage.6,7 However, it remains unknown whether gut dysmotility is the cause or consequence of NEC and how gut motility associates with NEC progression in various parts of the gastrointestinal tract (GIT). In infants undergoing surgery for NEC (late-stage NEC), severe lesions are most frequent in the small intestine (especially terminal ileum), but in more severe cases lesions can be present throughout the GIT.8
As NEC lesions and clinical complications often progress very rapidly, it is critical to search for non-invasive diagnostic biomarkers that allow early NEC detection. Dysmotility-related signs of NEC progression (e.g., vomiting, feeding intolerance, abdominal distention, bloody stool) are non-specific and subjective, which may lead to unjustified cessation of enteral feeding, prolonged parenteral nutrition (PN), and unnecessary antibiotic treatment.9 Clinical and molecular blood biomarkers (e.g., circulating inflammatory markers, hematology, and blood biochemistry) are also non-specific and cannot differentiate NEC from sepsis.10 Finally, the radiological signs of NEC appear relatively late in disease progression.11,12 Current techniques for early evaluation of gut motility, such as manometry, gastric emptying scintigraphy, magnetic resonance imaging, and ultrasound, are relatively invasive or poorly validated as NEC markers13,14 and mainly investigate motility of the upper GIT despite that NEC lesions are most frequent in the distal bowel.4
We hypothesized that gut motility and transit time are abnormal already in the early phase of NEC progression. To test our hypothesis, we used preterm pigs because of ethical limitations in subjecting a large group of preterm infants with suspected NEC to serial x-ray investigations. Preterm pigs delivered at 90% gestation and formula-fed are very sensitive to feeding- and microbiota-related NEC, and 40–80% of preterm pigs spontaneously develop mild-to-severe NEC lesions already within the first week of life, depending on diet regimen, feeding progression rate, and bacterial colonization.15 In this model, severe clinical NEC symptoms are observed mainly when lesions are present in the small intestine, not when they are present only in the colon.16 Early NEC lesions may occur also in the stomach, probably reflecting the GIT immaturity in preterm pigs (e.g., impaired gastric acid secretion leading to bacterial overgrowth17). Preterm pigs therefore provide a good opportunity to study the relationship between region-specific NEC pathology and gut transit time using serial x-ray recordings after contrast feeding, coupled with in situ inspection of NEC lesions.
Materials and methods
Animals and experimental procedures
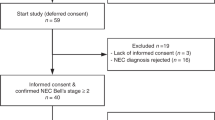
All animal procedures were approved by the Danish National Committee on Animal Experimentation (license no. 2014-15-0201-55 00418). A total of 85 preterm pigs (Danish Landrace × Large White × Duroc, male:female = 45:40, birth weight = 952 ± 23 g, final body weight on day 5 = 1055 ± 28 g), delivered from 9 sows by cesarean section on gestational day 106 (corresponding to 90% of full gestation) were included in the study. The 10–15% of preterm pigs dying or euthanized within the first 2 days of life, typically due to respiratory failure, were not included.15 Pigs were placed individually in preheated incubators (37–38 °C) and supplied with extra oxygen during the first 24 h (1–2 l/min). Body temperature was closely monitored until normal temperature (38–39 °C) was achieved. Within 2 h of delivery, pigs were prepared with an oro-gastric tube for enteral nutrition (EN) and an umbilical vascular catheter for immunization with maternal plasma and PN, as previously described.18 Pigs were orally fed every 3 h with various milk diets, e.g., bovine colostrum (n = 21) and infant formula (n = 64), with varying protein and energy densities (e.g., protein 14–105 g/l, energy 2700-4000 kJ/l) and heat treatments and feeding progression rates (reaching 64–120 ml/kg/day within 5 days). A wide range of feeding regimens was chosen to reflect the widely differing feeding strategies for preterm infants, potentially affecting their NEC risk.19 EN was supplemented with infusion of PN and saline to ensure adequate total fluid and nutrient intake (e.g., PN plus EN intake equivalent to 120–180 ml/kg/day in total) during the study period. Animals were continuously monitored during the experiment, and fecal consistency was recorded twice daily, as previously described.18 A fecal consistency >2 was defined as diarrhea. Pigs were euthanized early if they developed severe clinical symptoms (e.g., lethargy, respiratory distress). Body weight was recorded daily, and the time for first meconium passage was noted.
Gut transit time measurement
Gut motility was determined by measuring gut transit time of contrast solution using x-ray photography. On day 4, animals were orally fed a contrast solution (4 ml/kg, Iodixnol, Visipaque, GE Healthcare, Brøndby, Denmark) 2 h after their regular feeding, to mimic clinical practice in many units. Abdominal x-ray images were captured using a Mobilett XP Hybrid (Siemens, Germany) at 0.4, 1, 2, 4 h, and then every second hour until the contrast solution was completely emptied from the GIT or until the time of euthanasia on day 5. The pigs were continuously fed every 3 h, also during x-ray examination on day 4. Images were analyzed by an experienced radiologist and a neonatologist, blinded to the clinical outcome of pigs with regards to the NEC lesions recorded on day 5 (examples shown in Fig. 1a–c). The time taken for a complete clearance of contrast from the stomach (StEmpty), for contrast to first appear at the cecum (ToCecum), for a complete clearance of contrast from the small intestine (SiEmpty), and to first appearance at the rectum (ToRectum) were recorded. Time taken for the contrast solution to pass through the colon (CecumToRectum) was calculated by subtracting the ToCecum time from the ToRectum time. Time taken for the contrast solution to pass through the colon (CecumToRectum) was calculated by subtracting the ToCecum time from the ToRectum time.
Contrast solution retained in the stomach (a), reaching the cecum (b), or present in both the colon and rectum (c). Representative images of pig stomach (d), intestine (e), and colon (f) without NEC lesions (score 1–2) or with mild (score 3–4) or severe (score 5–6) NEC lesions. Images are adapted from ref. 37 with modification.
NEC evaluation and GR
On day 5, animals received a bolus feeding 60 min before euthanasia and were euthanized by intracardiac sodium pentobarbital injection. The stomach, small intestine, and colon were dissected, and the GR was weighed. The GIT was graded for NEC severity using a previously validated macroscopic scoring system (i.e., score 1 = absence of macroscopic lesions; score 2 = mild symptoms such as local hyperemia and edema; score 3 = extensive hyperemia, extensive edema, and local hemorrhage; score 4 = extensive hemorrhage; score 5 = extensive hemorrhage, local necrosis, and pneumatosis intestinalis; score 6 = extensive necrosis and pneumatosis intestinalis), as shown in Fig. 1d–f. In this study, we investigated the relation between gut transit time and NEC-like lesions in the small intestine and colon, therefore 12 pigs with NEC lesions in the stomach were excluded from further analyses because lesions in this region may affect gastric emptying with subsequent effects on small intestinal and colonic transit time. Further, stomach lesions rarely appear in infants with NEC.
Animals with score 1 or 2 in both the small intestine and the colon were defined as noNEC pigs (n = 35, controls). Animals with score ≥3 in the small intestine were diagnosed as having small intestinal NEC (siNEC, n = 18), regardless of the condition of the colon. Animals with score ≥3 only in the colon were diagnosed as colon NEC (coNEC, n = 20).18 Only few pigs developed severe NEC symptoms defined as having a score 5–6 (2/18 in siNEC group and 4/20 in coNEC group). Overall NEC score was defined as the maximum score across the small intestine and colon.
Statistical analyses
All statistical analyses were performed using the statistical software R version 3.5.0. In the primary analysis, we analyzed differences between noNEC and pigs diagnosed with NEC (e.g., siNEC and coNEC pigs). The comparisons were performed using a linear mixed model for continuous variables followed by Dunnett test for post hoc comparison and non-parametric Wilcoxon test, if relevant. Generalized linear model was used to analyze binary data, such as diarrhea incidence. For time-to-event outcomes, comparisons were performed using the Cox proportional hazards model (R, survival package). The models included gender and birth weight as covariates and a random factor accounting for different feeding regimens. Receiver-operator curves (ROCs) were used and area under the curves (AUC) was calculated to evaluate the diagnostic and predictive values of using gut transit time to predict early NEC development. Data were summarized as numbers and percentages, raw arithmetic mean ± SEM, or median, as appropriate. A p value < 0.05 was considered significant and 0.05 < p < 0.15 was considered as a tendency to an effect. Correlation between time-to-event outcomes was assessed (R, SurvCorr package20).
Results
Clinical outcomes in relation to NEC diagnosis on day 5
All pigs gained similar weight irrespective of their NEC status recorded on day 5 (p > 0.05, Fig. 2a). Time taken for the first meconium to pass from rectum tended to be longer in NEC pigs, especially for those having siNEC, compared with noNEC pigs (p = 0.08, Fig. 2b). Pigs that were later diagnosed with NEC, especially in the colon, showed a tendency to higher incidence of diarrhea already before the x-ray examination on day 4, when compared with noNEC pigs (20% vs. 6%, p = 0.08, Fig. 2c). Diarrhea incidence and severity increased after ingestion of contrast solution, regardless of NEC status (21% vs. 56%, p < 0.05, Fig. 2c). Increased mass of the GRs 1 h after the last bolus meal was observed in both siNEC and coNEC pigs (both p < 0.05, Fig. 2d). The mass of GRs correlated positively with overall NEC severity score across the GIT (p < 0.01).
Clinical outcomes, including body weight gain (a), time of rectal passage of meconium after birth (b), and fecal consistency before and after ingestion of contrast solution and x-ray scan on day 4 (c). The mass of gastric residual 60 min after the last bolus of feeding on day 5 (d). NEC category was recorded on day 5, according to macroscopic lesions, either noNEC (pigs not showing any evidence of NEC lesions) and NEC (pigs with NEC lesions in either small intestine or colon regions). Asterisk (*) indicates significant difference between groups, p < 0.05. noNEC: pigs not showing any evidence of NEC lesions; siNEC: pigs with NEC lesions in the small intestine, with or without colon lesions; coNEC: pigs with NEC lesions only in the colon region.
Gut transit time on day 4 in relation to NEC diagnosis on day 5
The time points for the contrast solution to be completely cleared from stomach were recorded for all pigs and the median value was around 2 h across all animals. StEmpty time was longer in siNEC pigs than the other groups (both p < 0.01, median time, siNEC 4 h vs. noNEC 2 h and coNEC 1 h, Fig. 3a). The difference between the siNEC and other groups were greatest 3–4 h after ingestion of the contrast solution where 69% of noNEC pigs and 70% of coNEC pigs had already emptied the contrast solution from the stomach, compared with only 29% of siNEC pigs (p < 0.05). Neither coNEC nor overall NEC status (pooled values from the siNEC and coNEC groups) affected the StEmpty time (p > 0.1).
Proportion of pigs, with or without NEC lesions detected on day 5, showing complete passage of contrast solution from the stomach (a), passage to cecum (b), being fully emptied from the small intestine (c), passing to the rectum (d), or passage through the colon (e). The table shows the overview of NEC-related changes on gut transit (f). Dashed line across y-axis at 50% indicates median time. noNEC: pigs not showing any evidence of NEC lesions; siNEC: pigs with NEC lesions in the small intestine, with or without colon lesions; coNEC: pigs with NEC lesions only in the colon region.
The median time for the contrast solution to first reach to the cecum was 2 h. The ToCecum time was longer in siNEC pigs and shorter in coNEC pigs, compared with noNEC pigs (median time, siNEC 4 h vs. coNEC and noNEC 2 h, both p < 0.05, Fig. 3b). This resulted in significant longer ToCecum time in siNEC pigs than in coNEC pigs (p < 0.01). The difference between the siNEC and other groups were greatest 3–4 h after ingestion of contrast solution where only 28% of siNEC pigs showed contrast solution at Cecum, compared with 64% in noNEC and 80% in coNEC pigs (both p < 0.05).
Median time taken for the contrast to empty from the small intestine (SiEmpty) was 11 h. The coNEC pigs showed a tendency of prolonged SiEmpty time, especially when compared with noNEC pigs, with values from siNEC pigs being intermediate (p < 0.05, p = 0.18, respectively, median time coNEC 12 h, siNEC and noNEC 10.3 h, Fig. 3c). Longer SiEmpty time was detected across pigs diagnosed with NEC (pooled values of siNEC and coNEC pigs, median time, 11.62 h vs. 10.33 h, p < 0.05).
Median time taken for the contrast to first reach the rectum (ToRectum) was 12 h. ToRectum time was longer in siNEC pigs but tended to be shorter in coNEC pigs, relative to noNEC pigs (p < 0.05, p = 0.1, respectively, median time, siNEC 16 h vs. noNEC 12 h and coNEC 9 h, Fig. 3d). ToRectum time was therefore markedly longer in siNEC pigs compared with coNEC pigs (p < 0.01, Fig. 3d).
Across all pigs, colon transit time, measured by CecumToRectum time, was 10 h (median value). CecumToRectum time was longer in siNEC pigs, relative to coNEC pigs, with intermediate values in noNEC pigs (p < 0.01, p = 0.15, respectively, median time, siNEC 12 h vs. coNEC 7 h and 9 h noNEC, Fig. 3e). CecumToRectum time was similar between coNEC and noNEC pigs (p = 0.22, Fig. 3e), but significantly longer in siNEC pigs relative to the pooled values of the other pigs (p < 0.05). The summary of gut transit time points in the noNEC, siNEC, and coNEC groups is shown in Fig. 3f. Across all animals, StEmpty time correlated with ToCecum time (correlation coefficient 0.66, interquartile ranges 0.50–0.77, p < 0.01). The presence of diarrhea before the x-ray examination was associated with shorter ToCecum, CecumToRectum, and ToRectum times, reflecting an increase in initial transit speed in both the small intestine and colon (p < 0.01, p < 0.01, p < 0.05, respectively).
The most pronounced differences in StEmpty and ToCecum time points between NEC and noNEC pigs were observed 3–4 h after ingestion of the contrast solution (see above). The diagnostic value of StEmpty and ToCecum time points to predict siNEC and coNEC was therefore evaluated for this time period. The ROC analysis revealed a reasonable precision to predict siNEC when using StEmpty time (AUC = 0.76, 83% sensitivity, 55% specificity, 85% positive predictive value, 53% negative predictive value) and ToCecum time (AUC = 0.81, 86% sensitivity, 66% specificity, 89% positive predictive value, 60% negative predictive value). ToCecum time could be used to predict coNEC with AUC 0.78, 95% sensitivity, 52% specificity, 43% positive predictive value, and 96% negative predictive value.
Discussion
NEC is a rapidly progressing gut inflammatory disease that may affect up to 10% of very preterm infants.5 Signs of gut dysmotility (i.e., reduced gastric emptying, ENS functional abnormalities) have been reported, but it remains unknown whether these are causes or consequences of NEC.21 Ethical considerations and a poor clinical condition often prevent assessment of GIT motility patterns in NEC-suspected preterm infants and most studies have described only upper GIT motility.6,22,23,24 Using preterm pigs as a model for preterm infants, we report here changes in gut transit time when mild NEC lesions develop within the first week of life. When pigs were observed with altered transit time points on day 4, without any radiologic signs of NEC, the majority of them were 12–24 h later (day 5) diagnosed with mild NEC lesions in the small intestine and/or colon (e.g., hyperemia and/or local, mild hemorrhage, NEC scores 3–4). We suspect that such mild NEC lesions may often pass by unnoticed in infants, as such lesions would not necessarily be associated with severe clinical symptoms or clear evidence of NEC at standard x-ray examinations (e.g., intramural gas, portal vein gas, ileus).
Concerning gut development and NEC sensitivity, 90% gestation preterm pigs may reflect the physiological conditions of 70–80% gestation preterm infants.15 The magnitude of changes in gut transit time in preterm pigs with mild NEC lesions was region dependent, and especially NEC lesions in the small intestine were associated with a delay in transit time across most of the gut regions (e.g., longer time for stomach emptying, for the contrast to reach the cecum or rectum, and for passage through the colon). In contrast, NEC lesions only in the colon (leading to less clinically affected individuals, at least in pigs) were associated with accelerated contrast passage through the small intestine but a delay of complete emptying. We conclude that NEC lesions in the small intestine affects gut motility differently than NEC lesions in the colon region in preterm pigs.
Delayed stomach emptying (StEmpty) and large GRs are often used as an early sign of feeding intolerance and NEC. However, aspiration of gastric contents to record residual volume, with or without ultrasound examination, as a surrogate of stomach emptying measurement, is difficult and highly subjective.9 Both volume and color of GRls are non-specific parameters of early NEC lesions in both pigs (unpublished data) and infants.25 In this study, we observed a strong correlation between StEmpty time and NEC severity in the small intestine, consistent with results from a study in rodents.22 Besides, StEmpty time was similar to and correlated positively with time to reach the Cecum (ToCecum), reflecting that gastric emptying rate affect small intestinal peristalsis. In contrast, StEmpty time was less affected in coNEC pigs, despite an increase in GR amount 1 h after the last meal. In support, colon lesions may affect gastroparesis in experimental distal colitis, probably via extrinsic nervous system effects.26
In both siNEC and coNEC cases, there was an aberrant food transit pattern observed beyond the affected regions, i.e., not only the injured site but also the motility of its adjacent regions was affected. Presence of small intestinal NEC lesions was associated with delayed stomach emptying (StEmpty) and initial food passage through the small intestine (ToCecum) and colon (CecumToRectum). In contrast, when NEC lesions were present in the colon, this was associated with fast initial transit through the intestine (ToCecum) and to less extent also in colon (ToRectum, CecumToRectum). This may indicate that, unlike siNEC, which probably progresses rapidly and aggressively and affects motility functions more broadly throughout the gut, mild NEC lesions in colon may develop relatively slowly without reducing motility functions, at least not until lesions become more severe.27 Our data also indicated that the first passage of the contrast solution to a new gut region (e.g., ToCecum or ToRectum) was a more sensitive marker of motility than the complete clearance of contrast solution from a gut region (StEmpty, SiEmpty). Small intestinal transit time (ToCecum) may be the most promising predictor for early NEC in preterm neonates, using gut transit measurements. Birth-related immature gut motility may predispose to NEC but is clearly not the only factor. Postnatal insults (e.g., hypoxia, inflammation, bacterial colonization) may also cause gut dysmotility, probably by inducing ENS abnormalities and MMC perturbations.13,28,29,30,31 Some studies reported that small intestinal hypercontractility and vagal dysregulation might cause dysmotility and NEC.32,33 Our recordings of transit time points across the entire GIT suggest that dysmotility, likely in the lower GI (e.g., mid and distal intestine), may precede NEC development in the small intestine.
Serial imaging examinations of infants with x-ray expose these individuals to potential damaging doses of irradiation and it is unlikely that in clinical settings this approach can be applied to critically ill infants. It is therefore important to identify the optimal timing for exposing a NEC-suspected infant to contrast solution and subsequent possibly x-ray recording(s). Non-specific clinical signs of feeding intolerance (e.g., vomiting, diarrhea, high volume of GR, abdominal distention), together with ultrasound examination that provide semiquantitative data on gastric emptying and intestinal peristaltic movements as well as other parameters (e.g., bowel wall thickness, blood flow, intestinal dilation), might provide valuable information regarding the optimal timing to initiate x-ray contrast imaging.34 In this study, the majority of pigs had their contrast solution passing through the small intestine within 2–4 h (ToCecum), and the NEC-related differences in ToCecum time appeared 3–4 h after ingestion of the contrast solution. At these time points, we observed a reasonable predictive value for NEC lesions on day 5 (AUC = 0.8), considering the predictive value of another NEC-related diagnostic marker, GRs.9,35 Therefore, this approach might be a useful adjunct to other diagnostic tools like plain abdominal radiography and ultrasound. However, it remains that gut dysmotility is a rather non-specific early NEC marker and that many other factors may affect motility recordings, including diet (mother’s own milk, donor milk, formula), nutrient density, frequency, and volume of feedings.36 Future studies should document the NEC-independent effects of diet (e.g., colostrum, milk, formula, donor milk) and feeding rate (slow vs. fast) on motility patterns. Further, these studies should include other assessment tools, e.g., ultrasound, to evaluate their ability to assess intestinal motility throughout the entire intestine. While relevant as NEC predictor, ultrasound is restricted to investigate gastric emptying and intestinal peristaltic movements, which may not be affected in the early phase of NEC development. On the other hand, x-ray contrast imaging may be unethical to apply for critically ill infants. Nevertheless, we conclude that early progression of NEC in the small intestine (not colon) is associated with a delay in food passage across the entire gut, as assessed by x-ray contrast imaging. As such, our studies document a critical role of dysmotility in early NEC development and indicates that imaging tools may have the potential to better understand gut dysmotility in preterm infants and its relation to NEC.
References
Gfroerer, S. & Rolle, U. Pediatric intestinal motility disorders. World J. Gastroenterol. 21, 9683–9687 (2015).
Margolis, K. G. & Picoraro, J. A. in Fetal and Neonatal Physiology, 5th edn (eds Polin, R. A., Abman, S. H., Rowitch, D. H., Benitz, W. E. & Fox, W. W.) Ch. 90 (Elsevier, 2017).
Jadcherla, S. R. & Berseth, C. in Gastroenterology and Nutrition: Neonatology Questions and Controversies, 2nd edn (ed. Neu, J.) Ch. 3 (W.B. Saunders, Philadelphia, 2012).
Dicken, B. J. et al. Medical management of motility disorders in patients with intestinal failure: a focus on necrotizing enterocolitis, gastroschisis, and intestinal atresia. J. Pediatr. Surg. 46, 1618–1630 (2011).
Neu, J. & Walker, W. A. Necrotizing enterocolitis. N. Engl. J. Med. 364, 255–264 (2011).
Morriss, F. H. Jr., Moore, M., Gibson, T. & West, M. S. Motility of the small intestine in preterm infants who later have necrotizing enterocolitis. J. Pediatr. 117, S20–23 (1990).
Bush, T. G. Enteric glial cells. An upstream target for induction of necrotizing enterocolitis and Crohn’s disease? Bioessays 24, 130–140 (2002).
Kliegman, R. M. & Walsh, M. C. Neonatal necrotizing enterocolitis: pathogenesis, classification, and spectrum of illness. Curr. Probl. Pediatr. 17, 219–288 (1987).
Li, Y. F. et al. Gastric residual evaluation in preterm neonates: a useful monitoring technique or a hindrance? Pediatr. Neonatol. 55, 335–340 (2014).
Niemarkt, H. J. et al. Necrotizing enterocolitis: a clinical review on diagnostic biomarkers and the role of the intestinal microbiota. Inflamm. Bowel Dis. 21, 436–444 (2015).
Gregory, K. E. et al. Necrotizing enterocolitis in the premature infant: neonatal nursing assessment, disease pathogenesis, and clinical presentation. Adv. Neonatal Care 11, 155–166 (2011).
Esposito, F. et al. Diagnostic imaging features of necrotizing enterocolitis: a narrative review. Quant. Imaging Med. Surg. 7, 336–344 (2017).
Jones, M. P. & Bratten, J. R. Small intestinal motility. Curr. Opin. Gastroenterol. 24, 164–172 (2008).
Gounaris, A. et al. Gastric emptying of preterm neonates receiving domperidone. Neonatology 97, 56–60 (2010).
Sangild, P. T. et al. Invited review: The preterm pig as a model in pediatric gastroenterology. J. Anim. Sci. 91, 4713–4729 (2013).
Sun, J. et al. Necrotizing enterocolitis is associated with acute brain responses in preterm pigs. J. Neuroinflammation 15, 180 (2018).
Buddington, R. K. et al. Prenatal gastrointestinal development in the pig and responses after preterm birth. J. Anim. Sci. 90(Suppl 4), 290–298 (2012).
Sun, J. et al. Nutrient fortification of human donor milk affects intestinal function and protein metabolism in preterm pigs. J. Nutr. 148, 336–347 (2018).
Good, M., Sodhi, C. P. & Hackam, D. J. Evidence-based feeding strategies before and after the development of necrotizing enterocolitis. Expert Rev. Clin. Immunol. 10, 875–884 (2014).
Schemper, M., Kaider, A., Wakounig, S. & Heinze, G. Estimating the correlation of bivariate failure times under censoring. Stat. Med. 32, 4781–4790 (2013).
Koike, Y. et al. Gastric emptying is reduced in experimental NEC and correlates with the severity of intestinal damage. J. Pediatr. Surg. 52, 744–748 (2017).
Berseth, C. L. Neonatal small intestinal motility: motor responses to feeding in term and preterm infants. J. Pediatr. 117, 777–782 (1990).
al Tawil, Y. & Berseth, C. L. Gestational and postnatal maturation of duodenal motor responses to intragastric feeding. J. Pediatr. 129, 374–381 (1996).
Bode, S., Dreyer, M. & Greisen, G. Gastric emptying and small intestinal transit time in preterm infants: a scintigraphic method. J. Pediatr. Gastroenterol. Nutr. 39, 378–382 (2004).
Abiramalatha, T., Thanigainathan, S. & Ninan, B. Routine monitoring of gastric residual for prevention of necrotising enterocolitis in preterm infants. Cochrane Database Syst. Rev. CD012937 (2019).
De Schepper, H. U. et al. Acute distal colitis impairs gastric emptying in rats via an extrinsic neuronal reflex pathway involving the pelvic nerve. Gut. 56, 195–202 (2007).
Hofma, B. R. et al. Colonic migrating motor complexes are inhibited in acute tri-nitro benzene sulphonic acid colitis. PLoS ONE 13, e0199394 (2018).
Ren, H., Han, J., Li, Z. & Xiong, Z. Stem cell factor/Kit signal insufficiency contributes to hypoxia-induced intestinal motility dysfunctions in neonatal mice. Dig. Dis. Sci. 62, 1193–1203 (2017).
Sase, M., Lee, J. J., Ross, M. G. & Buchmiller-Crair, T. L. Effect of hypoxia on fetal rabbit gastrointestinal motility. J. Surg. Res. 99, 347–351 (2001).
Nikiforou, M. et al. Global hypoxia-ischemia induced inflammation and structural changes in the preterm ovine gut which were not ameliorated by mesenchymal stem cell treatment. Mol. Med. 22, 244–257 (2016).
Rumio, C. et al. Activation of smooth muscle and myenteric plexus cells of jejunum via toll-like receptor 4. J. Cell. Physiol. 208, 47–54 (2006).
Parodi, J. et al. Hypertonicity of intestinal smooth muscle as a factor of intestinal ischemia in necrotizing enterocolitis. J. Pediatr. Surg. 22, 713–718 (1987).
Doheny, K. K. et al. Diminished vagal tone is a predictive biomarker of necrotizing enterocolitis-risk in preterm infants. Neurogastroenterol. Motil. 26, 832–840 (2014).
Cuna, A. C. et al. Bowel ultrasound for the diagnosis of necrotizing enterocolitis: a meta-analysis. Ultrasound Q. 34, 113–118 (2018).
Bertino, E. et al. Necrotizing enterocolitis: risk factor analysis and role of gastric residuals in very low birth weight infants. J. Pediatr. Gastroenterol. Nutr. 48, 437–442 (2009).
Bisset, W. M., Watt, J., Rivers, R. P. & Milla, P. J. Postprandial motor response of the small intestine to enteral feeds in preterm infants. Arch. Dis. Child. 64, 1356–1361 (1989).
Brunse, A. et al. Effect of fecal microbiota transplantation route of administration on gut colonization and host response in preterm pigs. ISME J. 13, 720–733 (2019).
Acknowledgements
We thank Jane Povlsen, Elin Skytte, Kristina Møller, Thomas Thymann, and Line Møller Willumsen from Comparative Pediatrics and Nutrition and Christel Renée Friborg from Department of Neonatology, Rigshospitalet for technical support with animal and x-ray procedures. This work was supported by NEOCOL project granted by Innovation Fund Denmark.
Author information
Authors and Affiliations
Contributions
Conception and design: L.A., S.S.K., P.T.S.; data acquisition: W.C., S.S.K., M.G., L.A.; data analysis: J.S.; data interpretation: J.S., W.C., P.T.S., L.A.; writing original draft: J.S.; critical review and editing: P.T.S., L.A.; approval of the final manuscript: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, W., Sun, J., Kappel, S.S. et al. Gut transit time, using radiological contrast imaging, to predict early signs of necrotizing enterocolitis. Pediatr Res 89, 127–133 (2021). https://doi.org/10.1038/s41390-020-0871-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0871-0
This article is cited by
-
Neonatal Necrotizing Enterocolitis: An Update on Pathophysiology, Treatment, and Prevention
Pediatric Drugs (2024)
-
Time to first passage of meconium and defecation frequency preceding necrotizing enterocolitis in preterm infants: a case–control study
European Journal of Pediatrics (2023)
-
Value of abdominal ultrasonography in predicting intestinal resection for premature infants with necrotizing enterocolitis
BMC Gastroenterology (2022)