Abstract
Background
Necrotizing enterocolitis (NEC) develops through exaggerated toll-like receptor 4 (TLR4) signaling in the intestinal epithelium. Breast milk is rich in non-digestible oligosaccharides and prevents NEC through unclear mechanisms. We now hypothesize that the human milk oligosaccharides 2’-fucosyllactose (2’-FL) and 6’-sialyllactose (6’-SL) can reduce NEC through inhibition of TLR4 signaling.
Methods
NEC was induced in newborn mice and premature piglets and infant formula was supplemented with 2’-FL, 6’-SL, or lactose. Intestinal tissue was obtained at surgical resection. HMO inhibition of TLR4 was assessed in IEC-6 enterocytes, mice, and human tissue explants and via in silico modeling.
Results
Supplementation of infant formula with either 2’-FL and/or 6’-SL, but not the parent sugar lactose, reduced NEC in mice and piglets via reduced apoptosis, inflammation, weight loss, and histological appearance. Mechanistically, both 2’-FL and 6’-SL, but not lactose, reduced TLR4-mediated nuclear factor kappa light-chain enhancer of activated B cells (NF-kB) inflammatory signaling in the mouse and human intestine. Strikingly, in silico modeling revealed 2’-FL and 6’-SL, but not lactose, to dock into the binding pocket of the TLR4–MD2 complex, explaining their ability to inhibit TLR4 signaling.
Conclusions
2’-FL and 6’-SL, but not lactose, prevent NEC in mice and piglet models and attenuate NEC inflammation in the human ileum, in part through TLR4 inhibition.
Impact
-
Necrotizing enterocolitis (NEC) is a major cause of morbidity and mortality in premature infants that occurs in the setting of bacterial colonization of the gut and administration of formula feeds and activation by the innate immune receptor toll-like receptor 4 (TLR4). Breast milk prevents NEC through unclear mechanisms. We now show that breast milk-enriched human milk oligosaccharides (HMOs) that are derived from lactose prevent NEC through inhibition of TLR4.
-
The human milk oligosaccharides 2’-FL and 6’-SL, but not the backbone sugar lactose, prevent NEC in mice and piglets.
-
2’-FL and 6’-SL but not lactose inhibited TLR4 signaling in cultured enterocytes, in enteroids derived from mouse intestine, and in human intestinal explants obtained at the time of surgical resection for patients with NEC.
-
In seeking the mechanisms involved, 2’-FL and 6’-SL but not lactose were found to directly bind to TLR4, explaining the inhibition and protection against NEC.
-
These findings may impact clinical practice by suggesting that administration of HMOs could serve as a preventive strategy for premature infants at risk for NEC development.
Similar content being viewed by others
Introduction
Necrotizing enterocolitis (NEC) is the leading cause of death from gastrointestinal disease in premature infants and is characterized by sudden necrosis of the small intestine, leading to overwhelming sepsis and death in many cases.1 The overall survival for patients with NEC has not improved since the disease was first described,2 and with the steady rise in the overall number of premature births worldwide,3 there exists a greater urgency than ever to understand its origins and to develop novel prevention strategies. We4,5,6 and others7 have identified a molecular explanation for NEC development, in which NEC results from exaggerated signaling in the intestinal epithelium in response to activation of the lipopolysaccharide receptor toll-like receptor 4 (TLR4), which is higher in the premature as compared with the full-term intestine.8 TLR4 activation by luminal lipopolysaccharide (LPS) leads to a disruption of the intestinal mucosa,9 resulting in bacterial translocation into the blood stream,10 where the activation of TLR4 on the endothelium results in vasoconstriction and the intestinal ischemia that characterizes NEC.11 Given the lack of specific treatments for NEC, the focus has shifted to prevention strategies, especially in those infants at the greatest risk for disease development.
Of all the strategies that are associated with NEC protection in infants, the administration of breast milk is decidedly the most effective. In seeking to understand the molecular components of breast milk that could be responsible for its protective benefits, we12 and others13,14 have shown that human milk oligosaccharides (HMOs), a family of non-digestible carbohydrates present in breast milk, can prevent NEC in experimental models, through mechanisms that are unknown. Moreover, there remains controversy regarding the role of HMOs early in life, as previous authors have shown that certain HMOs may not prevent NEC in piglets early in life.13 We now hypothesize that HMOs prevent NEC in part through direct inhibition of TLR4 signaling in the premature intestine, which we seek to test using mouse, piglet, and human tissue models of this disease.
Methods
Chemical reagents
RNeasy® Kit (catalog no. 74106; Qiagen) and QuantiTect® Reverse Transcription (catalog no. 205313; Qiagen), TUNEL (terminal deoxynucleotidyl transferase-mediated dUTP-fluorescein nick end labeling) Kit (In Situ Cell Death Detection Kit, Fluorescein, catalog no. 11684795910; Roche), 3’-nitrotyrosine (3’-NT) antibody (catalog no. ab61392; Abcam), NF-kBp65(F-6) antibody (catalog no. sc-8008; Santa Cruz Biotechnology), 4’,6-diamidino-2-phenylindole, dihydrochloride (catalog no. D9542; Sigma), and LPS from Escherichia coli 0127:B8 (Sigma; catalog no. L3129) were used. Forward and reverse primers were custom designed using NCBI Primer-BLAST online program and ordered from Integrated DNA Technologies and are listed in Table 1. The small intestinal epithelial cell IEC-6 was obtained from American Type Culture Collection (ATCC, Manassas, VA). TUNEL was from Roche Life sciences. Quantitative real-time PCR was performed using primers in Table 1 as described.15 All human intestine was obtained via a waiver of consent from the Office of Human Subjects Research, Johns Hopkins University (IRB00094036) and was collected in a de-identified manner. Galacto-oligosaccharide (GOS) was from Biosynth Carbosynth (Newbury, Berkshire, UK).
Animal studies
All experiments involving mice were carried out in accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health and are approved by Animal Care and Use Committee of The Johns Hopkins University (Protocol numbers MO17M304 and SW18M206), according to The ARRIVE Guidelines of the “NC3R.”16 Experimental NEC was induced in 7–8-day-old (approximately 3 g body weight) neonatal mice pups as previously described and validated.17 NEC was induced after the oral gavage of formula that is described in our recent paper18 and is composed of Similac Advance: Esbilac Canine Milk Replacer in equal concentrations, supplemented with bacterial stock that had been cultured from the stool of an infant with severe NEC (12.5 μl of stool slurry in 1 ml of formula). Neonatal pups were gavage-fed (50 μl/g) five times per day with formula supplemented with bacterial slurry using a 24-French angiocatheter placed into the mouse esophagus. Mice were exposed to hypoxia (5% O2, 95% N2) for 10 min in a chamber (Billups-Rothenberg Inc.) at 7 a.m. and 1 p.m. immediately after feed for 4 days. NEC formula was supplemented with 2’-FL, 6’-SL, or lactose (LAT) or GOS where indicated. In parallel, 3-week-old C57/BL6 mice were randomly divided into six groups: (i) saline-control, (ii) LPS, (iii) LPS + 2’-FL, (iv) LPS + 6’-SL, (v) LPS + 2’-FL + 6’-SL, and (vi) LPS + LAT. Where indicated, HMO, GOS, or LAT was administered orally at 10 mg/kg in 200 μl/mice 1 h before injection of LPS (5 mg/kg, intraperitonially). All mice were euthanized 6 h later, and samples of the small intestine were harvested.
NEC was induced in piglets to determine the effects of 2’-FL and 6’-SL as we have described.19 Timed-pregnant White Yorkshire (Yorkshire × Landrace) sows were obtained from Oak Hill Genetics (Ewing, IL), and piglets were delivered prematurely via cesarean section at ~90% gestation and administered either 2’-FL or 6’-SL (10 mg/ml, each individually or 5 mg/ml in combination). Piglets that were not induced to develop NEC were euthanized at birth and used as controls.
Evaluation of molecular docking of 2’-FL, 6’-SL, and LAT with TLR4-MD2
Molecular docking was used to analyze the binding efficiency of 2’-FL, 6’-SL, and a negative standard, LAT, to the LPS-binding pocket of the TLR4-MD2 complex. Spartan 18 (Wavefunction, Inc., Irvine, CA) was used to remove the antagonist Eritoran from PDB Code 2Z65, the crystal structure of the ternary eritoran-TLR4-MD2 complex,20 and to prepare the resulting TLR4-MD2 apoprotein complex for molecular docking. Biologically relevant conformations of 2’-FL and 6’-SL, extracted from PDB Code 5DUX21 and 4EN9,22 respectively, were then used for the docking experiment to TLR4-MD2. Autodock VinaTM combined with PyRxTM yielded optimized docked complexes with docking scores of −5.6 kcal/mol for 2’-FL and −6.7 kcal/mol for 6’-SL. In contrast, docking of the negative control LAT provided a lower docking score of −4.8 kcal/mol. Following the standard docking procedure, ligands were docked by defining a grid box of 20 Å × 20 Å× 20 Å around the cup-sized LPS recognition pocket of the TLR4-MD2 complex. PyMOLTM (The PyMOL Molecular Graphics System, Version 2.3.1 Schrödinger, LLC) was used for visualizations.
Results
Supplementation of infant formula with 2’-FL and 6’-SL prevents NEC in mice in a dose-dependent manner
We first sought to evaluate whether the most abundant neutral HMO, namely, 2’-FL, and the most abundant acidic HMO, namely, 6’-SL could prevent NEC, either alone or in combination, in well-established models of NEC. As shown in Fig. 1, the intestine of mice that were induced to develop NEC show extensive edema, thinning of the wall, and air within the bowel wall (also called pneumatosis intestinalis, a signature finding in human NEC), which is not seen in dam-fed control mice, where the intestine is pink and healthy appearing (Fig. 1a(i, ii)). Histological examination of NEC intestine revealed extensive villous sloughing, separation of submucosa, and edema in the submucosal and muscular layers (Fig. 1b(i, ii)). NEC induction also resulted in significant inflammation in the intestinal mucosa, as indicated by the expression of pro-inflammatory cytokine tumor necrosis factor (TNF)-α and high NEC severity score as assessed using our well-validated scoring system,23 in comparison to breast-fed controls, in which pro-inflammatory cytokine induction and disease severity scores were both minimal (Fig. 1e, f). Since both 2’-FL and 6’-SL are derived from the milk carbohydrate LAT, we evaluated LAT as a negative control, given that it is an carbohydrate that can be enzymatically digested, unlike the HMOs 2’-FL and 6’-SL, and because it serves as the molecular backbone of these HMOs.24 As shown in Fig. 1, the administration of infant formula that was supplemented with LAT resulted in no protective benefit against NEC, as measured by gross appearance of the intestine (Fig. 1aiii), intestinal histology (Fig. 1biii), cytokine induction (Fig. 1e), NEC severity (Fig. 1f), and body weight (Fig. 1g). By contrast, supplementation of the infant formula with either 2’-FL or 6’-SL significantly protected against NEC development, as manifest by improved gross appearance of the intestine (Fig. 1aiv, ci), intestinal histology (Fig. 1biv, di), cytokine induction (Fig. 1e), NEC severity (Fig. 1f), and body weight (Fig. 1g). The combination of 2’-FL and 6’-SL together and at the same total HMO dosage as either carbohydrate alone yielded no additional protection (Fig. 1e, f). It is noteworthy that lower doses of either 2’-FL or 6’-SL had no effect on NEC severity, especially at the shorter time points (Supplementary Fig. s1).
a(i–iv), c(i, ii) Photomicrographs showing gross morphology, b(i–iv), d(i, ii) Hematoxylin–eosin (H&E)-stained images showing histology of the small intestine (ileum), e quantitative real-time PCR (qRT-PCR) of pro-inflammatory cytokine tumor necrosis factor-alpha (TNF-α), f NEC severity scores, g nested graph showing body weight changes in neonatal mice subjected to no treatment (Ctrl, control breast-fed) or experimental NEC treatments without or with supplementation with lactose (10 mg/ml), 2’-FL (10 mg/ml), 6’-SL (10 mg/ml), or 2’-FL + 6’-SL (5 mg/ml, each). **p < 0·01, ***p < 0·001, each dot in dot graphs represents data from an individual mouse.
To further evaluate the extent to which 2’-FL and 6’-SL could prevent NEC, two additional measurements that are integral into the pathogenesis of NEC were undertaken: reactive oxygen species-mediated mucosal damage, as revealed by the expression of 3’-NT in the intestinal mucosa,25 and enterocyte apoptosis, as measured by TUNEL staining. As shown in Fig. 2, 3’-NT and TUNEL staining were both strongly expressed within the intestinal epithelium of mice with NEC (Fig. 2a(ii, ii’), b(ii, ii’)), while breast-fed control mice showed minimal expression (Fig. 2a(i, i’), b(i, i’)), consistent with our prior reports.23,26 Importantly, both 3’-NT and TUNEL staining in the intestinal mucosa were significantly reduced in mice with NEC in which the infant formula was supplemented with either 2’-FL or 6’-SL (Fig. 2a(iii, iv, iii’, iv’), b(iii, iv, iii’, iv’)) or their combination (Fig. 2a(v, v’), b(v, v’)), see quantification in Fig. 2c, d. Taken together, these findings illustrate that the administration of 2’-FL and 6’-SL, alone or in combination, protect against NEC in a mouse model. To evaluate the potential translational significance of these findings, we next evaluated a well-validated piglet model of the disease.19
a (i–v, i’–v’) Immunofluorescence images of 3'-nitrotyrosine (3’-NT, green fluorescence) as an indicator of oxidative injury and b(i–v, i’–v’) immunofluorescence images of TUNEL (green fluorescence) as an indicator of apoptosis in ileal sections of neonatal mice subjected to no treatment (Ctrl, control breast-fed) or experimental NEC without or with supplementation with 2’-FL (10 mg/ml), 6’-SL (10 mg/ml), or 2’-FL + 6’-SL (5 mg/ml, each), c quantification of fluorescent intensity of 3’-NT staining and d TUNEL staining measured using the ImageJ software, ***P < 0·001. Each dot in dot graphs represents data from an individual mouse.
Supplementation of nutritional formula with 2’-FL and 6’-SL protects against NEC development in a piglet model of NEC
As compared to piglets administered control formula without the addition of HMOs, the supplementation of formula with either 2’-FL (10 mg/kg) or 6’-SL (10 mg/kg) or their combination at 10 mg/kg each, significantly reduced NEC severity (Fig. 3), as revealed by improved gross morphological appearance (Fig. 3a), intact histological architecture (Fig. 3b), normal levels of pro-inflammatory cytokines TNF-α and interleukin-1β (Fig. 3c), and significantly lower average NEC scores (Fig. 3d). Moreover, while 3’-NT expression and mucosal epithelial apoptosis were both abundant in the intestinal mucosa of piglets with NEC (Fig. 3e, f), these findings were both significantly reduced to the levels of expression in the control piglets (Fig. 3e(i, i’), f(i, i’)), in NEC piglets supplemented with 2’-FL alone (Fig. 3e(iii, iii’), f(iii, iii’)), 6’-SL alone (Fig. 3e(iv, iv’), f(iv, iv’)), or both HMOs combined (Fig. 3e(v, v’), F(v, v’), and fluorescence quantification of 3’-NT and TUNEL staining is shown in Fig. 3g, h. Taken together, these findings illustrate that 2’-FL and 6’-SL protect against NEC development in both small and large animal models. We next sought to investigate the mechanisms involved, and so we next determined whether these HMOs could inhibit TLR4 signaling.
a (i–v) Representative photomicrographs of gross morphology and b (i–v) hematoxylin–eosin (H&E)-stained images of premature piglets that were either untreated and euthanized at birth (controls) or induced to develop experimental NEC in the absence or presence of 2’-FL, 6’-SL, or 2’-FL + 6’-SL, 5-μm paraffin-embedded sections of the small intestine (ileum), c (i, ii) quantitative real-time PCR (qRT-PCR) of pro-inflammatory cytokines tumor necrosis factor-alpha (TNF-α) and interleukin-beta (IL-1β), d NEC severity scores. ***P < 0·001, each dot in dot graphs represents data from an individual piglet. e–h 2’-FL) and 6’-SL supplementation prevents small intestinal mucosal damage in a piglet model of necrotizing enterocolitis (NEC). e (i–v, i’–v’) Immunofluorescence images of 3'-nitrotyrosine (3’-NT, green fluorescence) as an indicator of oxidative mucosal injury and f (i–v, i’–v’) immunofluorescence images of TUNEL (green fluorescence) as an indicator of apoptosis injury in the small intestine (ileum) sections of premature piglets subjected to no treatment (Ctrl, control breast-fed) or experimental NEC treatments without or with supplementation with 2’-FL (10 mg/ml), 6’-SL (10 mg/ml), or 2’-FL + 6’-SL (5 mg/ml, each); g quantification of fluorescent intensity of 3’-NT staining and h quantification of fluorescent intensity of TUNEL staining measured using the ImageJ software, ***P < 0·001. Each dot in dot graphs represents data from an individual piglet.
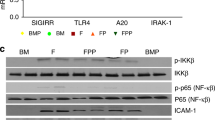
2’-FL and 6’-SL inhibit TLR4 signaling in IEC-6 enterocytes
Given the critical importance of TLR signaling in the pathogenesis of NEC,4,5,8 we next sought to determine whether 2’-FL and 6’-SL could protect against NEC development through TLR4 inhibition. To determine whether 2’-FL or 6’-SL could block TLR4 signaling, we first measured the effects of these HMOs on LPS-induced nuclear factor kappa light-chain enhancer of activated B cell (NF-kB) translocation from the cytoplasm into the nucleus (Fig. 4) and on TLR4-induced enterocyte apoptosis, pathways which are central to the mucosal inflammation that leads to NEC induction. These studies were performed using the model cell line IEC-6, which is a non-transformed crypt cell line that expresses TLR4 abundantly and responds to LPS,27 and thus allows for the direct study of HMO–TLR4 interactions without the potential influence of circulating factors. As shown in Fig. 4, as compared with control cells in which the p65 subunit of NF-kB is localized in the cytoplasm (Fig. 4a(i, i’)), LPS induced its translocation to the nucleus (Fig. 4a(ii, ii’), quantification in Fig. 4b). Although pretreatment with LAT had no effect on the degree of LPS-induced NF-kB translocation (Fig. 4a(iii, iii’), b), treatment of IEC with 2’-FL or 6’-SL, either alone or in combination, significantly blocked LPS-induced NF-kB signaling (Fig. 4a(iv–vi, iv’–vi’), b). In parallel, while LPS induced significant apoptosis (Fig. 4c(ii, ii’), d) of IEC-6 cells, the degree of apoptosis was not reduced by LAT (Fig. 4c(iii, iii’), d), but was markedly reduced by both 2’-FL and 6’-SL, either alone or in combination (Fig. 4c(iv–vi, iv’–vi’)). Taken together, these findings illustrate that 2’-FL and 6’-SL prevent TLR4 signaling in vitro, providing a mechanism by which they reduce NEC severity. We next sought to determine the impact on TLR4 signaling in human and mouse explants.
a (i–vi, i’–vi’) Photomicrographs of IEC6 cells immunostained for NF-kB p65 and b quantification of fluorescence intensity measured using ImageJ, ***P < 0·001. Each dot in dot graphs represents data from an individual cell. c, d 2’-FL and 6’-SL but not lactose prevents LPS-induced apoptosis in cultured intestinal epithelial (IEC6) cells. c(i–vi, i’–vi’) Photomicrographs of IEC6 cells immuno-stained with in situ death staining kit, TUNEL; d quantification of fluorescent intensity measured using the ImageJ software, **P<0.01, ***P < 0·001. Each dot represents data from an individual cell.
2’-FL and 6’-SL inhibit TLR4 signaling in NEC and in human and mouse intestinal explants
We next evaluated the potential effects of 2’-FL and 6’-SL on LPS-TLR4 signaling in vivo. As shown in Fig. 5, the induction of NEC in mice and piglets led to an increase in the expression of TLR4 in the intestine as compared to controls—consistent with increased TLR4 signaling—and was reduced after 2’-FL and 6’-SL administration (Fig. 5a(i, ii)). To directly evaluate whether 2’-FL or 6’-SL could inhibit LPS-TLR4 signaling in vivo, newborn mice were administered a single dose of either 2’-FL or 6’-SL by oral gavage 1 h before the intraperitoneal injection of LPS, and TLR4 expression and TLR4-induced cytokine expression were assessed in the intestinal epithelium. As shown in Fig. 5b, the injection of LPS significantly upregulated both TLR4 and TNF-α (Fig. 5b(i, ii)), and these were both reduced by 2’-FL, 6’-SL, or their combination (Fig. 5b(i, ii)). Further, the treatment of intestinal explants from either embryonic mice or premature human infants (obtained during stoma closure surgery) with LPS similarly led to increased expression of both TLR4 and TNF, which were both reduced by treatment with 2’-FL or 6’-SL (Fig. 5c(i, ii), d(i, ii)). In additional negative control experiments, we tested the effects of GOS on TLR4 signaling in vitro and in vivo, given that Autran et al. have shown that GOS do not impact NEC severity.14 As shown in Supplementary Fig. s2, GOS supplementation of formula did not reduce NEC as reflected by gross morphological and the histological appearance of the small intestine, which were still typical of NEC. GOS treatment also failed to reduce LPS signaling in the intestinal mucosa of 7-day-old mice or in IEC-6 enterocytes (Supplementary Fig. s3) and did not reduce LPS-induced NF-kB translocation (Supplementary Fig. s4i–iii, vii) or apoptosis (Supplementary Fig. s4iv–vi, viii) in IEC-6 cells. Taken together, these findings illustrate that the HMOs 2’-FL and 6’-SL can inhibit TLR4 signaling, both in vitro and in vivo. We next sought to assess the underlying mechanisms involved and focused on the possibility that 2’-FL and 6’-SL could directly bind to TLR4 and thus interfere with LPS signaling, as assessed below.
a (i, ii) TLR4 expression in mouse and piglet models of necrotizing enterocolitis, b (i, ii) TLR4 and pro-inflammatory cytokine TNF-α levels in mouse model of LPS-endotoxemia alone or 1 h pretreated (oral gavage) with 2’-FL and 6’-SL, c (i, ii) TLR4 expression and pro-inflammatory cytokine TNF-α expression in embryonic (embryonic day 18.5 (e18.5)) intestinal tissue ex vivo, d (i, ii) TLR4 and pro-inflammatory cytokine TNF-α levels in resected human intestinal tissue obtained at the time of NEC stoma closure surgery, treated with LPS, lactose, 2’-FL, and 6’-SL HMOs. *P<0.5, **P < 0·01, ***P < 0·001, each dot in dot graphs represents data from each individual sample.
2’-FL and 6’-SL but not LAT dock into the LPS-binding pocket of TLR4
In the final series of studies, we considered whether 2’-FL and 6’-SL could dock into the LPS-binding pocket of TLR4 as an explanation of their ability to inhibit TLR4 signaling and prevent NEC. To assess this possibility directly, we performed molecular modeling studies of binding using Autodock VinaTM in PyRxTM. As shown in Fig. 6, both 2’-FL and 6’-SL were found to dock with relative affinities of −5.6 and −6.7 kcal/mol, respectively, into the narrow, deep pocket of the TLR4-MD2 complex (Fig. 6a, b). This pocket is thought to bind LPS through a combination of internal hydrophobic residues and positively charged residues lining the rim of the cavity. Importantly, and in contrast, LAT was found to be a poorer fit (Fig. 6c), and its docking score into the same cavity is only −4.8 kcal/mol, which is consistent with the lack of protective activity of LAT against TLR4 signaling or NEC in Fig. 1. Taken together, these findings reveal that 2’-FL and 6’-SL inhibit TLR4 signaling through direct binding, providing a direct mechanism to explain their protection against the development of NEC in mice and piglets.
a CPK model of 2’-FL (cyan carbons) docked into the X-ray structure of the TLR4-MD2 complex 2Z65, b CPK model of 6’-SL (cyan carbons) docked into the X-ray structure of the TLR4-MD2 complex 2Z65, c CPK model of lactose (cyan carbons) docked into the X-ray structure of the TLR4-MD2 complex 2Z65, d structure of the TLR4-MD2-LPS symmetrical dimer complex 3FXI. The dimerization interface is triggered by LPS (cyan carbons) insertion into the MD2 hydrophobic binding pocket.
Discussion
We now demonstrate that the HMOs 2’-FL and 6’-SL play important roles in preventing the development of NEC in both mice and piglet models. In defining their mechanisms of action, we show that 2’-FL and 6’-SL, but not the control lactose backbone, inhibit TLR4 signaling in cultured enterocytes, as well as in intestinal explants from mice and humans, an effect that was revealed through computational analysis to involve direct binding to the LPS docking pocket. Given the critical role of TLR4 in the pathogenesis of NEC,4 these findings provide an explanation as to how HMOs can prevent NEC and also explain their protective effects on intestinal epithelial apoptosis and mucosal barrier injury. Perhaps most importantly, these findings suggest the possibility that HMOs may soon be part of the armamentarium of tools that could be administered to neonates at risk of NEC, with the hope of either preventing or treating this devastating disease. Further, ours is the first study to evaluate both 2’-FL and 6’-SL alone or in combination, to evaluate their roles in mouse, piglet and human tissue, and to link HMO effects to the inhibition of TLR4 signaling.
While we now show that HMOs 2’-FL and 6’-SL exert their NEC protective effects through TLR4 inhibition, other protective mechanisms have been described and are almost certain to play contributing roles. Specifically, prior authors have shown that 2’-FL and disialyl-lacto-N-tetraose act as prebiotics with putative effects on the ability of bacteria to bind to the colonic epithelium.28 In addition, HMOs are thought to encourage the growth of Bifidobacterium that are associated with a non-inflammatory state within the intestinal mucosa, suggesting a possible protective mechanism.29 While certainly plausible, it is not clear how these various oligosaccharides would interface with the rich oligosaccharides containing mucus layer, which itself has important effects on the microflora, and which would seemingly be endowed with oligosaccharides at much greater concentrations than that of any exogenously provided molecules. More recently, Pierro and colleagues have revealed that HMOs can modify the transcriptional profile of the intestinal epithelium, resulting in a shift toward goblet cells, with subsequent protective effects on the intestinal mucosa and protection from barrier injury.30 Our group has shown using cultured endothelial cells that the addition of HMOs can lead to an induction of the vasodilatory enzyme endothelial nitric oxide synthase (eNOS), resulting in the observation that mesenteric perfusion is significantly elevated in HMO-fed mice, and that the eNOS inhibitor can reverse the proactive effects of HMO for NEC.11 Given the various differences in the proposed and also demonstrated mechanisms of action of individual HMOs, additional studies will be required in order to evaluate their roles as preventive strategies specifically for infants at risk for the development of NEC.
In summary, we have now shown that 2’-FL and 6’-SL—two HMOs—act to prevent NEC in mice and piglet models and that our docking studies predict that these molecules interact with the LPS-binding site of TLR4, providing a mechanism of action. Taken together, we propose that the addition of 2’-FL and 6’-SL, either alone or in combination, can exert anti-NEC effects and may offer new approaches for the prevention of this devastating disease.
References
Stoll, B. J. et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. JAMA 314, 1039 (2015).
Fitzgibbons, S. C. et al. Mortality of necrotizing enterocolitis expressed by birth weight categories. J. Pediatr. Surg. 44, 1072–1076 (2009).
Martin, J. A. & Osterman, M. J. K. Describing the increase in preterm births in the United States, 2014-2016. NCHS Data Brief 1–8 (2018)
Leaphart, C. L. et al. A critical for TLR4 in the pathogenesis of necrotizing enterocolitis by modulating intestinal injury and repair. J. Immunol. 179, 4808–4820 (2007).
Sodhi, C. P. et al. Intestinal epithelial toll-like receptor 4 regulates goblet cell development and is required for necrotizing enterocolitis in mice. Gastroenterology 143, 708.e5–718.e5 (2012).
Gribar, S. C., Richardson, W. M., Sodhi, C. P. & Hackam, D. J. No longer an innocent bystander: epithelial toll-like receptor signaling in the development of mucosal inflammation. Mol. Med. 14, 645–659 (2008).
Jilling, T. et al. The roles of bacteria and TLR4 in rat and murine models of necrotizing enterocolitis. J. Immunol. 177, 3273–3282 (2006).
Gribar, S. C. et al. Reciprocal expression and signaling of TLR4 and TLR9 in the pathogenesis and treatment of necrotizing enterocolitis. J. Immunol. 182, 636–646 (2009).
Hackam, D. J., Good, M. & Sodhi, C. P. Mechanisms of gut barrier failure in the pathogenesis of necrotizing enterocolitis: toll-like receptors throw the switch. Semin. Pediatr. Surg. 22, 76–82 (2013).
Dheer, R. S. et al. Intestinal epithelial toll-like receptor 4 signaling affects epithelial function and colonic microbiota and promotes a risk for transmissible colitis. Infect. Immun. 84, 798–810 (2016).
Yazji, I. et al. Endothelial TLR4 activation impairs intestinal microcirculatory perfusion in necrotizing enterocolitis via eNOS-NO-nitrite signaling. Proc. Natl Acad. Sci. USA 110, 9451–9456 (2013)
Good, M. et al. The human milk oligosaccharide 2′-fucosyllactose attenuates the severity of experimental necrotising enterocolitis by enhancing mesenteric perfusion in the neonatal intestine. Br. J. Nutr. 116, 1175–1187 (2016).
Bering, S. B. Human milk oligosaccharides to prevent gut dysfunction and necrotizing enterocolitis in preterm neonates. Nutrients 10, 1461 (2018).
Autran, C. A., Schoterman, M. H. C., Jantscher-Krenn, E., Kamerling, J. P. & Bode, L. Sialylated galacto-oligosaccharides and 2′-fucosyllactose reduce necrotising enterocolitis in neonatal rats. Br. J. Nutr. 116, 294–299 (2016).
Livak, K. J. & Schmittgen, T. D. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods 25, 402–408 (2001).
Kilkenny, C., Browne, W. J., Cuthill, I. C., Emerson, M. & Altman, D. G. Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. PLoS Biol. 8, e1000412 (2010).
Niño, D. F. et al. Cognitive impairments induced by necrotizing enterocolitis can be prevented by inhibiting microglial activation in mouse brain. Sci. Transl. Med. 10, eaan0237 (2018).
Sodhi, C. P. et al. Fat composition in infant formula contributes to the severity of necrotising enterocolitis. Br. J. Nutr. 120, 665–680 (2018).
Good, M. et al. Lactobacillus rhamnosus HN001 decreases the severity of necrotizing enterocolitis in neonatal mice and preterm piglets: evidence in mice for a role of TLR9. Am. J. Physiol. Gastrointest. Liver Physiol. 306, G1021–G1032 (2014).
Kim, H. M. et al. Crystal structure of the TLR4-MD-2 complex with bound endotoxin antagonist Eritoran. Cell 130, 906–917 (2007).
Bum-Erdene, K., Leffler, H., Nilsson, U. J. & Blanchard, H. Structural characterisation of human galectin-4 N-terminal carbohydrate recognition domain in complex with glycerol, lactose, 3’-sulfo-lactose, and 2’-fucosyllactose. Sci. Rep. 6, 20289 (2016).
Yamashita, S. et al. Carbohydrate recognition mechanism of HA70 from Clostridium botulinum deduced from X-ray structures in complexes with sialylated oligosaccharides. FEBS Lett. 586, 2404–2410 (2012).
Egan, C. E. et al. Toll-like receptor 4-mediated lymphocyte influx induces neonatal necrotizing enterocolitis. J. Clin. Invest. 126, 495–508 (2016).
Rudloff, S. et al. Incorporation of orally applied 13C-galactose into milk lactose and oligosaccharides. Glycobiology 16, 477–487 (2006)
Ahsan, H. 3-Nitrotyrosine: a biomarker of nitrogen free radical species modified proteins in systemic autoimmunogenic conditions. Hum. Immunol. 74, 1392–1399 (2013).
Afrazi, A. et al. Intracellular heat shock protein-70 negatively regulates TLR4 signaling in the newborn intestinal epithelium. J. Immunol. 188, 4543–4557 (2012).
Cetin, S. et al. Endotoxin inhibits intestinal epithelial restitution through activation of Rho-GTPase and increased focal adhesions. J. Biol. Chem. 279, 24592–24600 (2004).
Moukarzel, S. & Bode, L. Human milk oligosaccharides and the preterm infant: a journey in sickness and in health. Clin. Perinatol. 44, 193–207 (2017).
Musilova, S., Rada, V., Vlkova, E. & Bunesova, V. Beneficial effects of human milk oligosaccharides on gut microbiota. Benef. Microbes 5, 273–283 (2014).
Wu, R. Y. et al. Human milk oligosaccharides increase mucin expression in experimental necrotizing enterocolitis. Mol. Nutr. Food Res. 63, e1800658 (2019).
Acknowledgements
D.J.H. is supported by R01GM078238 and R01DK083752 from the National Institutes of Health, and this research was funded in part by a Sponsored Research Grant from Abbott Nutrition to D.J.H.
Author information
Authors and Affiliations
Contributions
Substantial contributions to conception and design, acquisition of data, analysis or interpretation of data: C.P.S., P.W., Y.Y., W.B.F., M.K., D.F.N., Q.Z., E.B., A.D.W., M.R.L., T.P., S.W., H.J., R.H.B., K.C.G., P.L., D.J.H.; drafting the article or revising it critically: C.P.S., R.H.B., K.C.G., D.J.H.; final approval of the version to be published: C.P.S., D.J.H., R.H.B., K.C.G.
Corresponding author
Ethics declarations
Competing interests
This work was supported in part by a sponsored research grant from Abbott Nutrition to DJH. No author has any financial relationship or conflict of interest with the current work.
Statement of consent
Samples were obtained de-identified under IRB 00094036 and consent was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Sodhi, C.P., Wipf, P., Yamaguchi, Y. et al. The human milk oligosaccharides 2’-fucosyllactose and 6’-sialyllactose protect against the development of necrotizing enterocolitis by inhibiting toll-like receptor 4 signaling. Pediatr Res 89, 91–101 (2021). https://doi.org/10.1038/s41390-020-0852-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0852-3
This article is cited by
-
Air pollution exposure may impact the composition of human milk oligosaccharides
Scientific Reports (2024)
-
β-glucan protects against necrotizing enterocolitis in mice by inhibiting intestinal inflammation, improving the gut barrier, and modulating gut microbiota
Journal of Translational Medicine (2023)
-
Human milk oligosaccharides 3′-sialyllactose and 6′-sialyllactose attenuate LPS-induced lung injury by inhibiting STAT1 and NF-κB signaling pathways
Archives of Pharmacal Research (2023)
-
Necrotizing enterocolitis: recent advances in treatment with translational potential
Pediatric Surgery International (2023)
-
Bench to bedside — new insights into the pathogenesis of necrotizing enterocolitis
Nature Reviews Gastroenterology & Hepatology (2022)