Abstract
Background
Chronic lung disease remains a burden for extremely preterm infants. The changes in ventilation over time and optimal ventilatory management remains unknown. Newer, non-invasive technologies provide insight into these patterns.
Methods
This single-center prospective cohort study enrolled infants ≤32 0/7 weeks. We obtained epochs of transcutaneous carbon dioxide (TcCO2) measurements twice each week to describe the pattern of hypercarbia throughout their hospitalization.
Results
Patterns of hypercarbia varied based on birth gestational age and post-menstrual age (PMA) (p = 0.03), regardless of respiratory support. Infants receiving the most respiratory support had values 16–21 mmHg higher than those on room air (p < 0.001). Infants born at the youngest gestational ages had the greatest total change but the rate of change was slower (p = 0.049) compared to infants born at later gestational ages. All infants had TcCO2 values stabilize by 31–33 weeks PMA, when values were not significantly different compared to discharge. No rebound was observed when infants weaned off invasive support.
Conclusions
Hypercarbia improves as infants approached 31–33 weeks PMA. Hypercarbia was the highest in the most immature infants and improved with age and growth despite weaning respiratory support.
Impact
-
This study describes the evolution of hypercarbia as very preterm infants grow and develop.
-
The pattern of ventilation is significantly different depending on the gestational age at birth and post-menstrual age.
-
Average transcutaneous carbon dioxide (TCO2) decreased over time as infants became more mature despite weaning respiratory support. This improvement was most significant in infants born at the lowest gestational ages.
Similar content being viewed by others
Background
Despite transformative improvements in the practice of neonatology over the past 20 years, the burden of chronic lung disease remains high among very low birth weight infants and those born very premature. Infants born at <32 0/7 weeks gestational age (GA) make up a small proportion of neonatal intensive care unit (NICU) admissions but represent a disproportionately large burden of long-term disease, particularly lung disease.1,2,3,4 In all, 25–40% of very low birth weight infants continue to be diagnosed with bronchopulmonary dysplasia (BPD), while in extremely low birth weight infants the rate of BPD is as high as 50–60%.5,6,7,8,9 BPD is associated with increasing rates of poor neurodevelopmental outcomes, increased post-discharge readmissions, and increasedx mortality.8,10,11,12,13,14,15,16,17 In an attempt to decrease BPD, various lung-protective strategies have been attempted. Gentle ventilation, using controlled tidal volumes and toleration of mild hypercarbia, has become increasingly common as a standard of care to avoid ventilator-induced lung injury.18,19,20,21 Studies have also demonstrated safety and a trend toward improved outcomes with tolerance of mild hypercarbia.22,23,24,25 However, more severe hypercarbia and large fluctuations of partial pressure of carbon dioxide (pCO2) have been associated with multiple adverse events, including intraventricular hemorrhage (IVH) and mortality.26,27,28,29 Studies examining the long-term effects of a strategy of permissive hypercapnia have had mixed results.26,30,31,32,33 It is also likely that the mechanism for alterations in ventilation may change over time during a premature infant’s NICU course as lungs grow and changes associated with chronic lung disease develop.
Studies examining respiratory management, particularly ventilation, have relied on measurement of blood gases to determine pCO2 levels. Although this has been the standard of care, it has multiple disadvantages, including requiring invasive sampling techniques, cumulative blood loss for the infant, and reflection of a single point of time. Noninvasive methods of assessing pCO2, including capnography or transcutaneous monitoring, allow for collection of more frequent data points, including continuous monitoring without disturbing the infant. However, historically these methods have had several limitations in the neonatal population. Capnography using end tidal monitors may be inaccurate in infants for multiple reasons, including the use of uncuffed endotracheal tubes, the addition of a significant amount of dead space in the endotracheal tube–ventilator circuit, and the trend toward non-invasive ventilation. Use of transcutaneous carbon dioxide (TcCO2) monitors has also been limited by technological pitfalls. Earlier technology had been associated with inconsistent accuracy, skin irritation, and burns.34 Newer technology has made it possible to accurately and safely monitor TcCO2,35,36,37 using heated skin probes that measure local CO2 within the capillary bed and then adjusted to reflect arterial values. These more technologically sophisticated probes have been studied in multiple neonatal populations and show good correlation with arterial blood pCO2.38,39
Currently, there is a lack of understanding regarding the variability of hypercarbia in premature infants and how changes over time may relate to neonatal outcomes. There has been significant attention drawn to hypoxia because of the non-invasive oximetry data that are readily available and allow for continuous monitoring and recording. Less focus has been placed on the role of variation and trends in pCO2 due to the need for invasive collection, and therefore less availability, of such data. The purpose of this study is to describe the trends observed in hypercarbia in a cohort of premature infants born at <32 0/7 weeks GA.
Materials and methods
Participants
From April 2017 to April 2019, we identified all infants admitted to the University of Massachusetts Memorial Medical Center (UMMMC) NICU with a birth GA ≤32 0/7 weeks. Parents of these infants were approached on or after day of life 2 if the infants had a current or previous requirement for positive pressure respiratory support (i.e., mechanical ventilation, non-invasive positive pressure ventilation (NiPPV) or continuous positive airway pressure (CPAP). Informed consent was obtained from parents or legal guardians prior to enrollment. The study protocol was approved by the Institutional Review Board of the University of Massachusetts Medical School. Infants were excluded if they had parents/guardians who were not English or Spanish speaking, had any underlying genetic syndromes, or had been diagnosed with pulmonary disease other than BPD.
At UMMMC, all infants born ≤32 0/7 weeks GA are provided non-invasive positive pressure at delivery in addition to any resuscitation as indicated following Neonatal Resuscitation Program guidelines. Those born at <27 0/7 weeks GA are initiated on nasal NiPPV and those 27 0/7 through 31 6/7 are initiated on nasal CPAP (nCPAP). Infants are then weaned or escalated on their respiratory support at the discretion of the clinical team. However, all infants born <32 weeks GA are maintained on CPAP through 32 0/7 weeks post-menstrual age (PMA). In addition, all infants born <32 0/7 weeks GA are started on caffeine therapy within 6 h of birth.40
Data collection
Transcutaneous digital monitors (SDMs) (SenTec, Switzerland) were utilized to prospectively record TcCO2 levels in consented infants. Twice per week throughout the NICU stay, respiratory therapists placed the transcutaneous SenTec V-Sign Sensor on consented infants immediately after a feeding. The infants were recorded for a period of at least 40 min. This allowed for 20 min of consecutive data to be obtained after filtering for artifact. Data points were recorded once per second by the monitors with a sensor temperature of 41 °C. Following each recording, data were downloaded from the SDMs using the V-STATS 4.01 Software. PMA and level of respiratory support were also tracked at the time of each recording. The average TcCO2 values for each epoch of 20 min were calculated using drift-corrected data. A chart review was performed to extract relevant clinical variables and outcomes.
Statistical analyses
To evaluate the effect of PMA on pCO2, a gamma regression model with Generalized Estimating Equation option was used in order to take into account the skewed nature of the distribution of pCO2 and correlations due to repeated measures of pCO2 over time. The independent variable, PMA, was categorized into 7 groups: 26–<28, 28–<29, 29–<30, 30–<31, 31–<32, 32–<33, and 33–<45. Logarithmic link function was used, which resulted in rate ratio (RR) pCO2 of each PMA category compared to the last category (33–<45) as the reference. The model was adjusted for sex, race, birth weight, discharged with or without oxygen, and the level of respiratory support.
To analyze pCO2 based on level of respiratory support, the support types were categorized by conventional ventilation, high frequency ventilation (either oscillator or JET ventilator), NiPPV, CPAP, high-flow nasal canula (1.5 L of flow or greater with varying FiO2), or low-flow nasal canula (1 L/min of flow or less of 100% FiO2). A gamma regression model was performed to exhibit the association between pCO2 and level of respiratory support.
Results
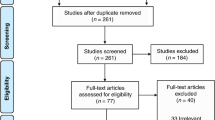
Of the 167 potentially eligible infants during the study period, a total of 54 infants were enrolled, and of these 51 were included in this analysis. Please see Supplemental Material for consort flow diagram (Supplement 1). Infants approached for consent were more likely to have lower birth weight, lower GA at birth, and longer length of stay than those not approached (Supplement 2). Almost all infants received antenatal steroids and the rates of significant morbidities such as severe IVH, necrotizing enterocolitis, and patent ductus arteriosus requiring treatment were low in this cohort (Table 1). The vast majority of infants were managed with non-invasive positive pressure until 32 0/7 weeks PMA. Approximately one quarter of the cohort was diagnosed with moderate-to-severe BPD, and approximately the same number was discharged home on supplemental oxygen.
From the cohort of 51 infants, a total of 637 individual 20-min epochs of continuous TcCO2 recordings were obtained (Table 2) between 26 and 44 weeks PMA. We stratified infants into three groups by birth GA: 24 5/7 to 26, >26 to 29, and >29 to 32 weeks. To test differences in pCO2 among three groups, F-test for repeated measures yielded power of >0.999 for alpha = 0.05, and 0.996 for alpha = 0.01. The estimated effect size was 0.3 (Supplement 3). The average pCO2 values for each epoch were calculated using drift-corrected data. Of these recordings, the majority were between 40 and 55 mmHg. To ensure the accuracy of the pCO2 measurement, we randomly selected one third of the patients in the study and compared pCO2 values between TcCO2 and blood gas assessments. Correlation between the two sets of measurements was very high at 0.8 (p < 0.001; Supplement 4). The figure also shows the regression line of PCO2 on TcCO2 through the origin. The slope was estimated to be 1.02, which is not statistically different from 1 (p = 0.47), and the regression R-square was as high as 0.97. These are indications of high agreement between two measures. To further demonstrate the agreement, a Bland–Altman plot is shown in Supplemental Material 5. Only two points (2/31 = 6.5%) fall outside of +/−1 standard deviation (SD) from the mean difference between two measures. The paired t test showed that the mean difference of 2.15 (+/−9.13 SD) mmHg between them was statistically insignificant (p = 0.20). In addition to accuracy of the pCO2 measurement by TcCO2, we also investigated the reliability of using 20-min epoch mean of TcCO2 second-by-second recordings. We randomly selected 25% of the infants from our sample and then randomly selected a total of 192 epochs using a computer algorithm. Using the second-by-second TcCO2 data, we found that the coefficient of variation (CV) ranged between 0.0019 to 0.33, with a median of 0.02; 95% of CVs were <0.08. CV (=mean/SD) is a measure of the degree of variation. In addition, we calculated the proportion of second-by-second data points that fell between mean ± 1.96 SD. The proportion for the entire sampled epochs ranged from 0.9 to 1, with more than half of the proportions >0.96.
Significant changes were noted over time and across PMAs (Fig. 1). The average CO2 at younger GAs was 55–60 mmHg but trended to the mid-low 40s by 36–40 weeks PMA.
There was a great deal of variability in the measurements. Examining the raw data revealed that there is a clear trend to decreasing pCO2 with increasing PMA (p = 0.03; Fig. 1). This trend remains true examined at different GA categories at birth (Fig. 2a). There was an increase in variability of pCO2 in the youngest birth GAs.
a Shows both the average level of TcCO2 as it changes by post-menstrual age and the rate of that change, demonstrating the inverse relationship. Those infants who are the youngest post-menstrual age have the highest average TcCO2 and then the steepest rate of change. b Shows the same information corrected for respiratory support.
The mean pCO2 exhibited a downward trend from early PMA of 26–44 weeks (p < 0.001). The estimated pCO2 before 32 weeks PMA was in the mid-50 mmHg and was reduced to approximately 45 mmHg at 40 weeks PMA. The rate of “reduction” in pCO2 is fastest for infants born at older GAs in the first postnatal weeks of life and eventually plateaus in consecutive weeks. The fitted curves and rates of changes over weeks of life are displayed in Fig. 2a, b.
Next, pCO2 assessments were analyzed accounting for the level of respiratory support the infant was receiving at the time of measurement. Infants were managed at the discretion of the clinical neonatologist; there was no specific clinical guidelines specifying level of support for range of pCO2. Selective surfactant administration was used per unit guidelines. Invasive mechanical ventilation was used for infants who failed non-invasive support regardless of GA, per the clinical team. The pCO2 values were reflective of the infants’ level of respiratory support at a time of relative stability rather than an independent variable that necessitated a change in support. Our results demonstrate that infants on the highest amount of respiratory support had the highest pCO2 values, likely reflecting their clinical illness severity (Fig. 3a, b). As the infants were weaned in their support, our measurements show that their CO2 did not rebound to higher values but actually decreased over time (Fig. 4). Infants on room air were more likely to have CO2 within the normal range compared to those on higher levels of respiratory support, such as NiPPV. It was only for low flow nasal cannula (LFNC) that this trend was not seen. Instead, there was a slight increase in pCO2. Although this could be a random variation associated with small sample size, it is possible that this reflects a true difference (Fig. 3a).
a, b The average, range, and CI for TcCO2 for infants on different levels of respiratory support. The TcCO2 was obtained on a stable level of respiratory support. Infants with the highest level of respiratory support such as those on mechanical ventilation or NiPPV had the highest TcCO2 while infants on less support tended to have lower levels of TcCO2.
Regression analysis of pCO2 (dependent variable) on level of respiratory support (independent variable) showed that, for the periods receiving high support (NiPPV and high frequency oscillatory ventilation/conventional mechanical ventilation), mean pCO2 was, respectively, 26 and 52% higher than those periods when receiving no support (p < 0.001, Fig. 3b). For the periods receiving LFNC and CPAP, mean pCO2 was 14 and 12% higher (p < 0.001).
When the cohort was stratified by birth GA category, the mean pCO2 for the youngest PMA group (26–<28 weeks) was noted to be 24% higher than that of infants at PMA 33–44 weeks (RR = 1.24; 95% confidence interval (CI) 1.00–1.54; p = 0.049). For the next group, 28–<29 weeks, the mean rate is 20% higher (RR = 1.20; 95% CI 1.11–1.30, p < 0.001). For infants born at 29–<30 weeks, the mean rate is 11% higher (RR = 1.11; 95% CI 1.06–1.17, p < 0.001) and those born at 30–<31 weeks GA, the mean rate is 8% higher (RR 1.08; 95% CI 1.04–1.12, p < 0.001). The mean pCO2 for infants born at ≥31 weeks GA did not vary significantly from the reference of stable values seen in infants’ measurements at 33–44 weeks PMA (Fig. 5).
The figure shows the average TcCO2 by gestational age groups. The average is compared to “normal” value observed at 33–44 weeks, significance of which is shown by p value. RRs for post-menstrual age were calculated using logistic regression model, adjusted for age, race, birth weight, whether discharged with O2, and level of respiratory support.
Discussion
We examined the trends over time of hypercarbia and variation of pCO2 via TcCO2 monitoring in a cohort of very premature infants throughout their NICU course. Utilizing newer technology with TcCO2 monitors, we were able to describe the pattern of ventilation over time and with different levels of support. With this study, we found a pattern of higher pCO2 in the first weeks of life, regardless of birth GA and level of respiratory support. In the infants born >29 weeks gestation, pCO2 values rapidly trended to values considered “normal” in healthy subjects (low 40s) and remained relatively stable throughout the remainder of their NICU course. Infants born <29 0/7 weeks gestation required a longer time to achieve pCO2 levels in the 40s, but on average, infants trended to a stable value by 31–33 weeks PMA, which was not significantly different from that at 36 weeks PMA. Infants born <26 0/7 weeks GA took significantly longer to reach pCO2 levels in the 40s but ultimately approached this same range. The rate at which the values decreased to the 40s was also different between GA groups; infants at the lowest GAs had the highest pCO2 values in the first weeks and took the longest time to achieve those stable values seen in babies born at later GAs. It is important to note that the optimal pCO2 levels for premature infants at different chronological or corrected GA remains unknown. However, it is reassuring that, off respiratory support, many premature infants did in fact achieve the same pCO2 levels (low 40s) that are considered healthy in term infants, older children, and adults.
Previous studies of ventilation in premature infants have focused on setting pCO2 goals and then checking at various intervals with blood gas measurement.22,24,25,26,41 Respiratory support was then determined by these laboratory values in the setting of a clinical study rather than assessment of infant status. By examining trends of pCO2 twice each week throughout the course of a NICU hospitalization, our project describes the trends of hypercarbia over the course of postnatal development in a range of GAs. Although the pCO2 values were highest on the highest levels of support, this also correlated with the most immature, fragile, and critically ill infants. It is more likely that the higher pCO2 levels were present despite the higher levels of respiratory support, not because of the support level; the hypercarbia likely would have been worse if not for the support provided. Interestingly, the infants did not demonstrate a rebound phenomenon after decreasing the level of respiratory support. This either reflects the fact that higher levels of support promote improvement in lung growth or healing or that the progression to lower respiratory support levels might have been possible earlier than performed in our NICU. The only group where this trend was not seen was in those infants on LFNC. These infants had slightly higher pCO2 than infants on HFNC and nCPAP. Although the small sample size of this group means that this could be the result of random variation, there is also physiologic plausibility to the hypothesis that it represents a true variation. LFNC does not support ventilation by supporting functional residual capacity and decreasing atelectasis as do both CPAP and HFNC. This trend may be reflective of that decreased support. Other studies have shown that providing distending pressure via nCPAP during periods of lung growth in the NICU support improved pulmonary function later.42,43,44 We believe that the use of gentle non-invasive respiratory support with continuous distending pressure supports lung growth and allows for normalization of ventilation as reflected in our results.
Studies randomizing infants to moderately higher pCO2 targets (permissive hypercarbia) have shown no difference in morbidities between groups, but those targeting even higher levels showed a trend toward increase in rates of IVH and periventricular leukomalacia (PVL).17,29,31,41 Despite clinical use of permissive hypercapnia and less invasive ventilation, our cohort had extremely low rates of IVH; only 1.9% had severe IVH and no infants were diagnosed with PVL.
We found that birth GA and PMA were the most predictive factors determining pCO2 rather than the level of respiratory support. In this cohort study, there was no mandated respiratory management or explicit pCO2 targets. Variability among clinical providers was therefore likely. However, the data suggest that time (and growth), rather than ventilatory strategy is what ultimately led to greater respiratory stability. Previous studies have shown that lung growth continues in the postnatal period and is correlated with somatic growth.45,46,47 Conversely, fetal growth restriction has been associated with poor lung growth and function both in human and animal models.1,45,46,48,49,50,51 It is possible that lung growth with increasing age resulted in increase in alveolar surface area and thinning of the interstitium, allowing for improved gas exchange.
To our knowledge, this is the first prospective, longitudinal cohort examining variation of pCO2 in premature infants during their NICU hospitalization. Previous research has relied on blood gas assessment of PaCO2, with blood gases obtained at the discretion of the clinical team. This study describes the trends observed during periods of both clinical stability and instability. TcCO2 monitors are still a newer technology. To validate our data, we reviewed study participants’ medical charts and found excellent correlation between transcutaneous values and capillary blood gas values obtained within an hour of the measurement (see Supplementary Material 4 and 5). In addition, our results are consistent with what was observed in the trials by Thome and Ambalavanan, that highest values of pCO2 are markers of respiratory illness severity, which in this population is most determined by birth GA and PMA.24,25,26
A limitation of this study is the potential incorrect assumption that the infants’ ventilation status during the two 20-min epochs recorded each week accurately represents the infants’ status for the other approximately 167 h each week. It is possible that there was significant variability that was not captured in our data. The trend that emerges, then, is even more striking, as more limited discrete data would be more prone to random variability. Another limitation is the smaller sample size of those infants born at <26 weeks GA. Given the known respiratory morbidity risk in this population, further evaluation of this vulnerable group of infants is needed. Finally, this is a single-center study so the hypercarbia trends reflect our unit’s respiratory practices and may not be generalizable.
The number of recordings and the longitudinal nature of the data spanning virtually the entire NICU course until discharge is a strength of this study. The finding that most of the preterm infants in our cohort, once off respiratory support, can eventually achieve and maintain pCO2 levels that are considered normal and healthy in older heathy populations (i.e., low 40s) is an important finding. While the timing to achieve this may reflect our individual unit’s respiratory practice, it demonstrates that these levels are achievable; correlation of these levels with other health outcomes is now needed.
In conclusion, infants born at earlier GAs have significantly higher pCO2 values in the first weeks of life despite being on higher levels of respiratory support. These values trend toward levels considered normal in other populations (low 40s) by 31–32 weeks PMA regardless of the birth GA. Further work is needed to better describe the variability of pCO2, particularly for those infants born <29 weeks GA and in the first weeks of life and how the degree of variability may influence later outcomes.
References
Laughon, M. M. et al. Prediction of bronchopulmonary dysplasia by postnatal age in extremely premature infants. Am. J. Respir. Crit. Care Med. 183, 1715–1722 (2011).
Smith, V. C. et al. Trends in severe bronchopulmonary dysplasia rates between 1994 and 2002. J. Pediatr. 146, 469–473 (2005).
Younge, N. et al. Survival and neurodevelopmental outcomes among periviable infants. N. Engl. J. Med. 376, 617–628 (2017).
Younge, N. et al. Improved survival and neurodevelopmental outcomes among extremely premature infants born near the limit of viability. Early Hum. Dev. 95, 5–8 (2016).
Stoll, B. J. et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA 314, 1039–1051 (2015).
Natarajan, G. et al. Outcomes of extremely low birth weight infants with bronchopulmonary dysplasia: impact of the physiologic definition. Early Hum. Dev. 88, 509–515 (2012).
Jobe, A. H. & Steinhorn, R. Can we define bronchopulmonary dysplasia? J. Pediatr. 188, 19–23 (2017).
Cheong, J. L. & Doyle, L. W. An update on pulmonary and neurodevelopmental outcomes of bronchopulmonary dysplasia. Semin. Perinatol. 42, 478–484 (2018).
Stoll, B. J. et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 126, 443–456 (2010).
Anderson, P. J. & Doyle, L. W. Neurodevelopmental outcome of bronchopulmonary dysplasia. Semin. Perinatol. 30, 227–232 (2006).
Gibson, A.-M. & Doyle, L. W. Respiratory outcomes for the tiniest or most immature infants. Semin. Fetal Neonatal Med. 19, 105–111 (2014).
Doyle, L. W. & Anderson P. J. Long-term outcomes of bronchopulmonary dysplasia. Semin. Fetal Neonatal Med. 14, 391–395 (2009).
Doyle, L. W. et al. Bronchopulmonary dysplasia in very low birth weight subjects and lung function in late adolescence. Pediatrics 118, 108–113 (2006).
Greenough, A. Long-term pulmonary outcome in the preterm infant. Neonatology 93, 324–327 (2008).
Greenough, A. et al. Health care utilisation of infants with chronic lung disease, related to hospitalisation for RSV infection. Arch. Dis. Child. 85, 463–468 (2001).
Van Marter, L. J. et al. Does bronchopulmonary dysplasia contribute to the occurrence of cerebral palsy among infants born before 28 weeks of gestation? Arch. Dis. Child. Fetal Neonatal Ed. 96, F20–F29 (2011).
Collins, M. P., Lorenz, J. M., Jetton, J. R. & Paneth, N. Hypocapnia and other ventilation-related risk factors for cerebral palsy in low birth weight infants. Pediatr. Res. 50, 712–719 (2001).
Keszler, M. & Sant’Anna, G. Mechanical ventilation and bronchopulmonary dysplasia. Clin. Perinatol. 42, 781–796 (2015).
Carlo, W. Gentle ventilation: the new evidence from the SUPPORT, COIN, VON, CURPAP, Colombian Network, and Neocosur Network trials. Early Hum. Dev. 88, S81–S83 (2012).
Kennedy, K. A., Cotten, C. M., Watterberg, K. L. & Carlo, W. A. Prevention and management of bronchopulmonary dysplasia: lessons learned from the Neonatal Research Network. Semin. Perinatol. 40, 348–355 (2016).
Davis, P. G., Morley, C. J. & Owen, L. S. Non-invasive respiratory support of preterm neonates with respiratory distress: continuous positive airway pressure and nasal intermittent positive pressure ventilation. Semin. Fetal Neonatal Med. 14, 14–20 (2009).
Thome, U. H. & Ambalavanan, N. Permissive hypercapnia to decrease lung injury in ventilated preterm neonates. Semin. Fetal Neonatal Med. 14, 21–27 (2009).
Thome, U. H. & Carlo, W. A. Permissive hypercapnia. Semin. Neonatol. 7, 409–419 (2002).
Thome, U. H. et al. Permissive hypercapnia in extremely low birthweight infants (PHELBI): a randomised controlled multicentre trial. Lancet Respir. Med. 3, 534–543 (2015).
Mariani, G., Cifuentes, J. & Carlo, W. A. Randomized trial of permissive hypercapnia in preterm infants. Pediatrics 104, 1082–1088 (1999).
Ambalavanan, N. et al. PaCO2 in surfactant, positive pressure, and oxygenation randomised trial (SUPPORT). Arch. Dis. Child. Fetal Neonatal Ed. 100, F145–F149 (2015).
Fabres, J., Carlo, W. A., Phillips, V., Howard, G. & Ambalavanan, N. Both extremes of arterial carbon dioxide pressure and the magnitude of fluctuations in arterial carbon dioxide pressure are associated with severe intraventricular hemorrhage in preterm infants. Pediatrics 119, 299–305 (2007).
McKee, L. A. et al. PaCO2 and neurodevelopment in extremely low birth weight infants. J. Pediatr. 155, 217–221. e211 (2009).
Hagen, E. W., Sadek-Badawi, M., Carlton, D. P. & Palta, M. Permissive hypercapnia and risk for brain injury and developmental impairment. Pediatrics 122, e583–e589 (2008).
Toms, R. & Ambalavanan, N. Permissive hypercapnia during mechanical ventilation of neonates. Indian Pediatr. 41, 775–778 (2004).
Varughese, M., Patole, S., Shama, A. & Whitehall, J. Permissive hypercapnia in neonates: the case of the good, the bad, and the ugly. Pediatr. Pulmonol. 33, 56–64 (2002).
Chonghaile, M. N., Higgins, B. & Laffey, J. G. Permissive hypercapnia: role in protective lung ventilatory strategies. Curr. Opin. Crit. Care 11, 56–62 (2005).
Miller, J. D. & Carlo, W. A. Safety and effectiveness of permissive hypercapnia in the preterm infant. Curr. Opin. Pediatr. 19, 142–144 (2007).
Berardesca, E. & Maibach, H. Transcutaneous CO2 and O2 diffusion. Ski. Pharmacol. Physiol. 6, 3–9 (1993).
Domingo, C. et al. Transcutaneous measurement of partial pressure of carbon dioxide and oxygen saturation: validation of the SenTec monitor. Arch. Bronconeumol. 42, 246–251 (2006).
Hejlesen, O. K., Cichosz, S. L., Vangsgaard, S., Andresen, M. F. & Madsen, L. P. Clinical implications of a quality assessment of transcutaneous CO2 monitoring in preterm infants in neonatal intensive care. Stud. Health Technol. Inf. 150, 490–494 (2009).
Tobias, J. D. Transcutaneous carbon dioxide monitoring in infants and children. Pediatr. Anesth. 19, 434–444 (2009).
Hochwald, O. et al. Continuous noninvasive carbon dioxide monitoring in neonates: from theory to standard of care. Pediatrics 144, e20183640 (2019).
Mukhopadhyay, S., Maurer, R. & Puopolo, K. M. Neonatal transcutaneous carbon dioxide monitoring—effect on clinical management and outcomes. Respir. Care 61, 90–97 (2016).
Rhein, L. et al. Optimizing noninvasive respiratory support in the delivery room and early caffeine initiation to decrease bronchopulmonary dysplasia amongst infants born ≤32 & 0/7 weeks gestational age. Am. J. Respir. Crit. Care Med. 197, A6124 (2018).
Thome, U. H. et al. Neurodevelopmental outcomes of extremely low birthweight infants randomised to different PCO2 targets: the PHELBI follow-up study. Arch. Dis. Child. Fetal Neonatal Ed. 102, F376–F382 (2017).
Lam, R. et al. The effect of extended continuous positive airway pressure on changes in lung volumes in stable premature infants: a randomized controlled trial. J. Pediatr. 217, 66–72. e61 (2020).
Thomson, M. A. et al. Treatment of immature baboons for 28 days with early nasal continuous positive airway pressure. Am. J. Respir. Crit. Care Med. 169, 1054–1062 (2004).
Zhang, S., Garbutt, V. & McBride, J. T. Strain-induced growth of the immature lung. J. Appl. Physiol. 81, 1471–1476 (1996).
Friedrich, L. et al. Growth rate of lung function in healthy preterm infants. Am. J. Respir. Crit. Care Med. 176, 1269–1273 (2007).
Jones, M. Effect of preterm birth on airway function and lung growth. Paediatr. Respir. Rev. 10, 9–11 (2009).
Panagiotounakou, P. et al. Very preterm neonates receiving “aggressive” nutrition and early nCPAP had similar long-term respiratory outcomes as term neonates. Pediatr. Res. 86, 742–748 (2019).
Maritz, G. S., Cock, M. L., Louey, S., Suzuki, K. & Harding, R. Fetal growth restriction has long-term effects on postnatal lung structure in sheep. Pediatr. Res. 55, 287–295 (2004).
Jobe, A. H. An Unknown: Lung Growth and Development after Very Preterm Birth (American Thoracic Society, 2002).
Ali, K. et al. Prediction of prolonged ventilator dependence in preterm infants. Eur. J. Pediatr. 178, 1063–1068 (2019).
O’Reilly, M., Sozo, F. & Harding, R. Impact of preterm birth and bronchopulmonary dysplasia on the developing lung: long-term consequences for respiratory health. Clin. Exp. Pharmacol. Physiol. 40, 765–773 (2013).
Acknowledgements
No financial assistance was received in support of this study. SenTec loaned several transcutaneous carbon dioxide monitors for use in this prospective cohort study.
Author information
Authors and Affiliations
Contributions
Each author has met the Pediatric Research authorship requirements. All authors made substantial contributions to the conception and design, acquisition of data, and/or analysis and interpretation of data. K.P.S. drafted the article. K.P.S., L.M.R., and H.O.W. revised it critically for important intellectual content. L.M.R., H.O.W., L.E.G., J.J.N., and A.F.L. all gave final approval of the version to be submitted for publication.
Corresponding author
Ethics declarations
Competing interests
None of the authors have any financial ties to the products used in the study.
Consent statement
Informed consent was obtained from the parents or guardians prior to enrollment.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sullivan, K.P., White, H.O., Grover, L.E. et al. Transcutaneous carbon dioxide pattern and trend over time in preterm infants. Pediatr Res 90, 840–846 (2021). https://doi.org/10.1038/s41390-020-01308-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-01308-2