Abstract
Background
Assessing the inflammation is important in the follow-up of paediatric patients with inflammatory bowel disease (IBD). We aim to evaluate the value of B cell-activating factor (BAFF) in paediatric IBD as a potential biomarker for follow-up.
Method
We determined BAFF in serum and faeces and faecal calprotectin (CP) in 32 IBD children—16 Crohn’s disease (CD) and 16 ulcerative colitis (UC). Twenty-six healthy children and 10 children with irritable bowel syndrome (IBS) were included as controls.
Results
No differences were found in serum BAFF between IBD, IBS, and healthy group: 1037.35, 990.9 and 979.8 pg/ml, respectively, all p > 0.05, but faecal BAFF was higher in the IBD group: 15.1, 8.5 and 8.2 pg/ml, respectively, p < 0.05, and higher in the UC group (55.975 pg/ml) compared to the CD group (10.95 pg/ml), p = 0.015. Splitting the IBD group in relation to the CP level, the serum BAFF had no significantly different values between the subgroups, but the faecal BAFF was significantly higher in the >250 μg/g subgroup. Cut-off values of BAFF were calculated.
Conclusion
Faecal BAFF is a promising marker for monitoring the children with IBD, higher levels of BAFF being correlated with high CP.
Impact
-
Faecal BAFF is a promising marker in monitoring the children with IBD, higher levels of BAFF being correlated with high faecal calprotectin.
-
To our knowledge, this is the first paediatric study concerning BAFF evaluation in IBD.
-
Faecal BAFF levels could be considered a potential non-invasive marker in monitoring IBD activity in paediatric population with clinically mild or inactive disease.
Similar content being viewed by others
Introduction
Intestinal inflammation is a main burden for the gut health. It is encountered in the inflammatory bowel disease (IBD), but lower degrees of inflammation are also detected in irritable bowel syndrome (IBS).1,2
IBD in children represents a concerning condition, since its incidence is increasing throughout Europe.3 Several factors contribute to the pathogenesis of IBD: personal and environmental factors (diet, gut microbiota, lifestyle) acting from early childhood to adulthood,4 genetic factors (NOD2, IL23R and ATG16L1 genes5) and an excessive immune response in predisposed individuals.6,7 As a consequence, a chronic inflammatory response in the intestinal tract is triggered, leading to the release of pro- and anti-inflammatory cytokines.8,9,10
In children (as in adults), the IBD diagnosis is confirmed by multiple investigation methods, including endoscopic techniques, with serial biopsies. The procedures are difficult and not easily accepted by children and caregivers compared to adults, especially in the follow-up and in confirming the mucosal healing. The efficiency of the treatment is currently monitored using a few biological markers, such as faecal calprotectin (CP), C-reactive protein (CRP) and faecal lactoferrin,11,12,13 but these tests are not highly specific. For this reason, it is necessary to evaluate other potential biomarkers.
One of the newly emerging biomarkers for intestinal inflammation is the B cell-activating factor (BAFF).14 BAFF was recognized as an important factor for the survival and maturation of B cells.15 It belongs to the tumour necrosis factor superfamily, being produced mainly by monocytes, macrophages, neutrophils and dendritic cells.16,17,18
BAFF plays an important role in the development of autoimmunity,19 being extensively studied in systemic lupus erythematosus20 where belimumab, the first BAFF inhibitor biologic drug, was approved. Dysregulated expression or function of BAFF was demonstrated in rheumatoid arthritis,21 primary Sjogren’s syndrome,22 malignancies,19 IgA nephropathy23 or asthmatic patients.24,25,26
The potential role of BAFF in the pathogenesis of IBD seems to be related to the BAFF ability to activate multiple immune pathways: B cell differentiation and survival, T cell activation and differentiation, proinflammatory cytokines (interleukin-6 (IL-6), tumor necrosis factor-α (TNF α)) production and expression and nuclear factor kappa-light-chain-enhancer of activated B cells (NFkB) activation in epithelial cells and macrophages.27 Despite the few data published regarding the BAFF involvement in IBD mucosal inflammation, in the opinion of Uzzan et al.,27 BAFF could be a novel strategy in IBD.27 Zhang et al.11 studied the utility of BAFF as a potential biomarker for IBD in adults and reported that the concentration of BAFF in serum and in faeces could differentiate patients with active IBD from patients with IBS and from healthy controls. Fu et al.14 demonstrated a highly significant correlation between faecal BAFF and endoscopic inflammation severity in adult IBD patients.
To the best of our knowledge, no study was realized in paediatric population.
Given the encouraging data from the studies on IBD in adults, we assessed the value of the serum and faecal BAFF levels in the IBD paediatric patients.
Methods
Protocol
This is a prospective study carried out in two tertiary centres of paediatrics. The study was carried out on IBD patients and two control groups. The recruitment was performed in chronological order and included cases that had been referred for follow-up between October 2018 and April 2019.
Subjects
The inclusion criteria for the IBD group were: subjects between 3 and 18 years old with prior diagnosis of IBD (ulcerative colitis (UC) or Crohn’s disease (CD)) using the standard clinical criteria, serology, endoscopy, histology and abdominal imaging,28 with clinical inactive disease. We used the paediatric ulcerative colitis activity index (PUCAI)29 and weighted paediatric Crohn’s disease activity index (wPCDAI)30 to establish the status of the clinical inactive disease (wPCDAI < 12.5, PUCAI < 10).
Two groups served as control: one group with IBS and one group of apparently healthy participants.
For the IBS group, the inclusion criteria were: age 3–18-year-old, diagnosed with IBS diarrhoea/constipation/mixed form using ROME IV criteria.31
The control group included patients recorded in our Department for Pathologies unrelated to gastrointestinal system and without acute illnesses, recruited from ambulatory/outpatient service during the periodic visits to the paediatrician.
We excluded patients not in the 3–18 year old interval range, presenting with acute/chronic gastrointestinal symptoms (other than IBD) or acute diseases (pneumonia, acute asthma exacerbations, infectious diarrhoea, etc.), patients who did not provide a stool sample and patients with no legal tutor at visit.
All subjects (IBD, IBS or control) underwent a thorough clinical examination (age, sex, weight, height, body mass index, time of diagnosis, symptoms at diagnosis, initiation of immunomodulatory/immunosuppressant/biologic therapy, possible complications—strictures, fistulas, abscesses, surgery) and laboratory tests (blood and faecal sample) all in the same day. All included patients had endoscopic examination in the previous 12 months. Ultrasonography was also performed.
Laboratory tests
Two blood samples were drawn from the antecubital vein on the morning after the patient had fasted for 12 h. One sample was used to determine the CRP level and erythrocyte sedimentation rate (ESR). The other blood sample was centrifuged at 2000 rotations/min for 5 min and the serum was collected and stored at −80 °C in Eppendorf tubes until processed.
From the stool specimens, one sample was used to determine the CP level (enzyme-linked immunosorbent assay (ELISA)) and the other sample was stored at −80 °C until processed. Before BAFF determination, the faeces were mixed with 0.9% saline solution resulting in a final concentration of 200 mg/ml. The sample was vortexed for 10 min at 10,000 rotations/min and the supernatants filtered.
BAFF concentration in faecal and serum samples was measured using the ELISA kit (Quantikinine ELISA Human BAFF/BLyS/TNFSF13B, Minneapolis MN) according to the manufacturer’s instructions. All samples were expressed in pg/ml, and the quantification range of the assay was between 62.5 and 4000 pg/ml.
Statistical analysis
The distribution of continuous variables was tested using Shapiro–Wilks test. Data were presented as mean and standard deviation (SD) for normally distributed continuous variables, median and interquartile range for non-normally distributed continuous variables and absolute number and percent for categorical variables. The Mann–Whitney U test was used for the comparison of non-normally distributed continuous variables between the groups. Receiver operating characteristic (ROC) analysis was used to evaluate the diagnostic performances of faecal BAFF and the areas under the ROC curve (AUC) were calculated. The discriminant cut-off values were selected corresponding to the highest sensitivity (Se) and specificity (Sp). A p value less than 0.05 was considered statistically significant. The Spearman correlation coefficient was calculated to evaluate the correlations between continuous values. The statistical analysis was performed using IMB SPSS Statistics v.23 and Microsoft Office 365 Excel.
Ethical issues
The study protocol was approved by the local Ethics Committee. All the patients enrolled (diseases and control group) were minors and a written informed consent was signed by their legal tutors.
Results
In our study we recruited 38 patients with IBD (age 4–17 years), 10 patients with IBS (age 8–14 years) and 26 healthy children (age 3–17 years). Three patients with IBD were excluded due to the impossibility to provide faecal samples. Finally, the IBD group included 32 patients, 16 with UC and 16 with CD.
The demographics characteristics of the four groups and main data about the disease as well as the medication used by the IBD paediatric patients are presented in Table 1.
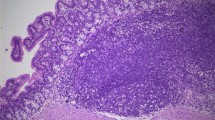
CRP and ESR values had no significant differences between groups (all p > 0.05), but the CP level was higher in the IBD group compared to control and IBS groups (all p < 0.001). The serum value of BAFF had no significant differences between the healthy group and IBS or IBD groups (all p > 0.05) but the faecal value of BAFF was significantly higher in IBD patients (p < 0.05) vs both control groups. Moreover, the concentration of faecal BAFF was significantly higher in UC compared with CD (p = 0.015), IBS (p < 0.05) and the healthy group (p < 0.05). In CD, the concentration of faecal BAFF had no significant differences compared to the healthy group or IBS (all p > 0.05) (Table 2 and Figs. 1 and 2).
Depending on the CP values (<250 and >250 μg/g, according to ESPGHAN revised Porto criteria for the diagnosis of IBD in children and adolescents27), we divided the IBD group in two subgroups (23 and 9 patients). The serum level of BAFF had no significant difference between the subgroups: 1047.0 (802.55–1182.6) vs 939.5 (622.8–1168.9), p > 0.05—but the faecal level of BAFF was significantly higher in the >250 μg/g subgroup: 13.4 (9.1–38.35) vs 94.5 (15.7–111.0), p = 0.02. No statistically significant results were obtained when the analysis was performed in relation to the IBD category (UC or CD) (all p > 0.05) (Fig. 3).
The results of ROC curve analyses used to establish the cut-off values of faecal level of BAFF in order to discriminate the patients with IBD from other groups are listed in Table 3. The best AUC, Se and Sp of faecal level of BAFF was obtained for UC vs Control (0.858, 75% and 92.3%, respectively).
Discussion
In this study we assessed the blood and faecal BAFF levels in paediatric patients with IBD and compared them to the levels in IBS and apparently healthy control group; the data were correlated with the disease activity index and CP levels. We found that the faecal BAFF concentrations in the IBD group were significantly higher when compared to the control and IBS groups and higher in patients with UC compared to CD patients. We calculated the faecal BAFF cut-off values, useful in differentiating the IBD patients from patients with IBS and healthy subjects. As the faecal levels of BAFF was the highest in patients with increased CP levels, we can consider faecal BAFF as a promising marker in the evaluation of the remission status. The production of inexpensive test kits would be a solution for monitoring IBD in children.
Serum BAFF levels did not differentiate between IBD patients and either of the control groups. These results could be explained by the fact that faecal BAFF reflects better the intestinal inflammation, compared to serum BAFF.
To our knowledge, this is the first paediatric study regarding BAFF in IBD; therefore, we cannot compare our results with other paediatric studies.
Zhang et al.11 demonstrated significant differences between the faecal and the serum BAFF in adult IBD patients when compared to IBS or healthy controls, suggesting its potential role in the pathogenesis of IBD. They analysed 78 UC and 37 CD patients and they found that in active disease, the BAFF values were significantly higher compared to inactive disease, both in serum and faeces. In order to differentiate the IBD patients from IBS and healthy ones, they established the serum and faecal BAFF cut-off values. Interestingly, these cut-off values confer higher sensitivity and specificity to faecal BAFF compared to serum BAFF (84 and 96% vs 55 and 93%). We found no differences between serum BAFF in our groups, but this is probably related to the absence of patients with clinically active IBD enrolled. But, as Zhang et al.11 found in adult patients with inactive disease, we observed higher faecal BAFF level in the IBD group (especially in the UC group). These findings could be relevant for monitoring the disease activity, as it appears that the BAFF levels return to values similar to healthy subjects more rapidly in the serum and persist longer in faeces. Strong correlations between BAFF, disease activity and proinflammatory cytokine (TNF alfa, IL1β) were found, suggesting the role of BAFF in IBD pathogenesis.11 Our study complements the data obtained in adults with inactive disease. As the level of faecal BAFF was increased in both adults11 and children with inactive disease, it could be speculated that BAFF is not only related to the disease flares but also to the pathogenetic substrate of IBD.
No consensus was established about the definition of remission in paediatric IBD. The “clinical remission” is the most accepted and used term and is defined by composite scores (wPCDAI < 12.5 for CD30 and PUCAI < 1029 for UC), in which clinical items are taken in consideration (abdominal pain, rectal bleeding, stool frequency and consistency, number of stools per 24 h, nocturnal stools, activity level, weight). Laboratory findings (ESR and albumin) are used only in the wPCDAI calculation. It has been shown that there are discrepancies between the clinical remission and the laboratory, endoscopic and histologic findings,32,33,34 so there is a need for a global approach, including clinical, imaging, histologic and laboratory items.
The ESPGHAN guide.28 recommends the use of CP to assess the intestinal inflammation. A level >250 μg/g of CP predicts more accurately the existent inflammation, and further investigations such as endoscopy or a change in treatment should be taken in consideration. In clinical practice, however, in asymptomatic patients, the follow-up is preferred to further investigation. The higher level of faecal BAFF found in our patients with CP > 250 μg/g could reinforce the suspicion about local inflammation and to reconsider the status of these patients.
The differential diagnosis between IBD and IBS represents a challenge, especially in patients with mild IBD, as both categories present abdominal pain and diarrhoea.35 ESPGHAN guide28 recommends as initial work up ileocolonoscopy and esophagogastroduodenoscopy with multiple biopsies for all suspected IBD cases. But these invasive procedures may have complications such as bleeding and perforations, adverse events related to the sedation and anaesthesia, and increased discomfort,36 which prompts for a need for non-invasive diagnosis. CP already demonstrated its utility in differentiating patients with organic gastrointestinal disease from those with functional disorders.37 We found the same utility for BAFF in distinguishing between IBD and IBS, even in clinically inactive patients. This might be useful as an initial work up for a better selection of patients who need endoscopic examination.
The ROC curve analysis for the cut-off value of faecal BAFF for discriminating between IBD and IBS/control had high specificity (92–93%) but a lower sensitivity (50%), probably due to the low number of clinically active IBD patients.
In our country, the only available data are on the adult population and there are no published studies on paediatric IBD.38 The disease course of UC and CD in the adult population of Romania tends to be less severe, with fewer extra-intestinal complications and extension.39 There is a lower frequency of IBD in Eastern Europe compared to other parts of Europe, but with a continuous increasing incidence.40,41 However, our study is underlining the role of BAFF to assess intestinal inflammation in inactive or mild IBD cases, and to be used in settings such as ours where severe cases of IBD are not frequent. Thus, BAFF should be considered as another biomarker for intestinal inflammation.
Our study’s main limitation is the low number of patients enrolled in each group. In our country IBD is mainly mild; therefore, we could not test severe forms of IBD. Also, we did not correlate the faecal and serological findings to endoscopy and ultrasonography. Due to ethical considerations, risks, discomfort and costs, in our department the patients in clinical remission are not routinely evaluated using endoscopy.
Conclusions
In paediatric patients with mild or inactive IBD, faecal BAFF levels could be considered as a potential non-invasive marker for disease monitoring. Larger longitudinal studies are needed in order to establish the real utility of this factor not only for diagnosis but especially for the non-invasive follow-up of the patients.
References
Long, M. D. & Drossman, D. A. Inflammatory bowel disease, irritable bowel syndrome, or what?: A challenge to the functional-organic dichotomy. Am. J. Gastroenterol. 105, 1796–1798 (2010).
David, L. E., Surdea-Blaga, T. & Dumitrascu, D. L. Semiquantitative fecal calprotectin test in postinfectious and non-postinfectious irritable bowel syndrome: cross-sectional study. Sao Paulo Med J. 133, 343–349 (2015).
Roberts, S. E. et al. A systematic review and meta analysis of paediatric inflammatory bowel disease incidence and prevalence across Europe. J. Crohns Colitis https://doi.org/10.1093/ecco-jcc/jjaa037 (2020)
Sýkora, J. et al. Current global trends in the incidence of pediatric-onset inflammatory bowel disease. World J. Gastroenterol. 24, 2741–2763 (2018).
Ananthakrishnan, A. N. et al. Environmental triggers in IBD: a review of progress and evidence. Nat. Rev. Gastroenterol. Hepatol. 15, 39–49 (2018).
Xavier, R. J. & Podolsky, D. K. Unravelling the pathogenesis of inflammatory bowel disease. Nature 448, 427–434 (2007).
Guan, Q. & Zhang, J. Recent advances: the imbalance of cytokines in the pathogenesis of inflammatory bowel disease. Mediators Inflamm. 2017, 4810258 (2017).
de Souza, H. S. & Fiocchi, C. Immunopathogenesis of IBD: current state of the art. Nat. Rev. Gastroenterol. Hepatol. 13, 13–27 (2016).
Bevivino, G. & Monteleone, G. Advances in understanding the role of cytokines in inflammatory bowel disease. Expert Rev. Gastroenterol. Hepatol. 12, 907–915 (2018).
Friedrich, M., Pohin, M. & Powrie, F. Cytokine networks in the pathophysiology of inflammatory bowel disease. Immunity 50, 992–1006 (2019).
Zhang, P. et al. Cell-activating factor as a new potential marker in inflammatory bowel disease. Dig. Dis. Sci. 61, 2608–2618 (2016).
Galgut, B. J., Lemberg, D. A., Day, A. S. & Leach, S. T. The value of fecal markers in predicting relapse in inflammatory bowel diseases. Front. Pediatr. 5, 292 (2018).
Diederen, K. et al. Raised faecal calprotectin is associated with subsequent symptomatic relapse, in children and adolescents with inflammatory bowel disease in clinical remission. Aliment Pharm. Ther. 45, 951–960 (2017).
Fu, Y. et al. Comparison of non-invasive biomarkers faecal BAFF, calprotectin and FOBT in discriminating IBS from IBD and evaluation of intestinal inflammation. Sci. Rep. 7, 2669 (2017).
Schneider, P. et al. BAFF, a novel ligand of the tumor necrosis factor family, stimulates B cell growth. J. Exp. Med. 189, 1747–1756 (1999).
Mackay, F. & Schneider, P. Cracking the BAFF code. Nat. Rev. Immunol. 9, 491–502 (2009).
Nardelli, B. et al. Synthesis and release of B-lymphocyte stimulator from myeloid cells. Blood 97, 198–204 (2001).
Craxton, A., Magaletti, D., Ryan, E. J. & Clark, E. A. Macrophage- and dendritic cell-dependent regulation of human B-cell proliferation requires the TNF family ligand BAFF. Blood 101, 4464–4471 (2003).
Vincent, F. B., Saulep-Easton, D., Figgett, W. A., Fairfax, K. A. & Mackay, F. The BAFF/APRIL system: emerging functions beyond B cell biology and autoimmunity. Cytokine Growth Factor Rev. 24, 203–215 (2013).
Jackson, S. W. & Davidson, A. BAFF inhibition in SLE—is tolerance restored? Immunol. Rev. 292, 102–119 (2019).
Shabgah, A. G., Shariati-Sarabi, Z., Tavakkol-Afshari, J. & Mohammadi, M. The role of BAFF and APRIL in rheumatoid arthritis. J. Cell Physiol. 234, 17050–17063 (2019).
Thompson, N., Isenberg, D. A., Jury, E. C. & Ciurtin, C. Exploring BAFF: its expression, receptors and contribution to the immunopathogenesis of Sjögren’s syndrome. Rheumatology 55, 1548–1555 (2016).
Cao, Y., Lu, G., Chen, X., Guo, N. & Li, W. BAFF is involved in the pathogenesis of IgA nephropathy by activating the TRAF6/NK ‑κB signaling pathway in glomerular mesangial cells. Mol. Med. Rep. 21, 795–805 (2020).
Kang, J. S. et al. B cell-activating factor is a novel diagnosis parameter for asthma. Int Arch. Allergy Immunol. 141, 181–188 (2006).
Jee, H. M. et al. Increased B cell-activating factor (BAFF) level in the sputum of children with asthma. Korean J. Pediatr. 53, 795–800 (2010).
Dilidaer et al. Increased BAFF expression in nasal polyps is associated with local IgE production, Th2 response and concomitant asthma. Eur. Arch. Otorhinolaryngol. 274, 1883–1890 (2017).
Uzzan, M., Colombel, J. F., Cerutti, A., Treton, X. & Mehandru, S. B cell-activating factor (BAFF)-targeted B cell therapies in inflammatory bowel diseases. Dig. Dis. Sci. 61, 3407–3424 (2016).
Levine, A. et al. ESPGHAN revised porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J. Pediatr. Gastroenterol. Nutr. 58, 795–806 (2014).
Turner, D. et al. Development, validation, and evaluation of a pediatric ulcerative colitis activity index: a prospective multicenter study. Gastroenterology 133, 423–432 (2007).
Hyams, J. S. et al. Development and validation of pediatric Crohn’s disease activity index. J. Pediatr. Gastroenterol. Nutr. 12, 439–447 (1991).
Hyams, J. S. et al. Functional disorders: children and adolescents. Gastroenterology https://doi.org/10.1053/j.gastro.2016.02.015 (2016).
Aggarwal, V. et al. Role of capsule endoscopy and fecal biomarkers in small-bowel Crohn’s disease to assess remission and predict relapse. Gastrointest. Endosc. 86, 1070–1078 (2017).
Kopylov, U. et al. Detection of small bowel mucosal healing and deep remission in patients with known small bowel Crohn’s disease using biomarkers, capsule endoscopy, and imaging. Am. J. Gastroenterol. 110, 1316–1323 (2015).
El-Matary, W., Abej, E., Deora, V., Singh, H. & Bernstein, C. N. Impact of fecal calprotectin measurement on decision-making in children with inflammatory bowel disease. Front. Pediatr. 5, 7 (2017).
Spiller, R. & Major, G. IBS and IBD—separate entities or on a spectrum? Nat. Rev. Gastroenterol. Hepatol. 13, 613–621 (2016).
Thakkar, K., El-Serag, H. B., Mattek, N. & Gilger, M. Complications of pediatric colonoscopy: a five-year multicenter experience. Clin. Gastroenterol. Hepatol. 6, 515–520 (2008).
An, Y. K. et al. Faecal calprotectin testing for identifying patients with organic gastrointestinal disease: systematic review and meta-analysis. Med. J. Aust. 211, 461–467 (2019).
Zaharie, R. et al. Diagnostic delay in romanian patients with inflammatory bowel disease: risk factors and impact on the disease course and need for surgery. J. Crohns Colitis 10, 306–314 (2016).
Gheorghe, C. et al. Epidemiology of inflammatory bowel disease in adults who refer to gastroenterology care in Romania: a multicentre study. Eur. J. Gastroenterol. Hepatol. 16, 1153–1159 (2004).
Vadan, R., Gheorghe, L. & Gheorghe, C. Low prevalence and mild course of inflammatory bowel diseases in South Eastern Europe. J. Gastrointestin Liver Dis. 18, 385–386 (2009).
Ng, S. C. et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet 390, 2769–2778 (2018).
Acknowledgements
This work was supported by “Iuliu Hatieganu” University of Medicine and Pharmacy Cluj-Napoca, grant number 3066/20/ from 1 February 2018.
Author information
Authors and Affiliations
Contributions
I.F. and O.S. performed the data acquisition, analysis and interpretation. I.F. D.L.D., D.E.S. and S.C.M. concepted the work and designed the study. I.F. wrote the paper. D.L.D., D.E.S. and S.C.M. critically revised the paper for intellectual content. All the authors approved the final version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fodor, I., Serban, O., Serban, D.E. et al. B cell-activating factor (BAFF) in children with inflammatory bowel disease. Pediatr Res 89, 1798–1803 (2021). https://doi.org/10.1038/s41390-020-01155-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-01155-1