Abstract
Background
Intestinal recovery after NEC is difficult to predict in individuals. We evaluated whether several biomarkers predict intestinal recovery after NEC in preterm infants.
Methods
We measured intestinal tissue oxygen saturation (rintSO2) and collected urinary intestinal-fatty acid binding protein (I-FABPu) levels 0–24 h and 24–48 h after NEC onset, and before and after the first re-feed. We assessed intestinal recovery in two ways: time to full enteral feeding (FEFt; below or equal/above group’s median) and development of post-NEC complications (recurrent NEC/post-NEC stricture). We determined whether the rintSO2, its range, and I-FABPu differed between groups.
Results
We included 27 preterm infants who survived NEC (Bell’s stage ≥ 2). Median FEFt was 14 [IQR: 12–23] days. Biomarkers only predicted intestinal recovery after the first re-feed. Mean rintSO2 ≥ 53% combined with mean rintSO2range ≥ 50% predicted FEFt < 14 days with OR 16.7 (CI: 2.3–122.2). The rintSO2range was smaller (33% vs. 51%, p < 0.01) and I-FABPu was higher (92.4 vs. 25.5 ng/mL, p = 0.03) in case of post-NEC stricture, but not different in case of recurrent NEC, compared with infants without complications.
Conclusion
The rintSO2, its range, and I-FABPu after the first re-feed after NEC predicted intestinal recovery. These biomarkers have potential value in individualizing feeding regimens after NEC.
Similar content being viewed by others
Introduction
Preterm infants who develop NEC are managed with a nil p.o. (NPO) regimen and are temporarily fed by total parenteral nutrition (TPN).1,2,3 Currently, the duration of this NPO regimen is determined by consensus-based guidelines, mostly dictated by NEC stage.3,4,5,6 As enteral feeding is essential for gut function and for growth and development of the infant, and TPN is associated with complications such as cholestatic liver disease, it is desirable to minimize the NPO duration.7,8,9,10,11 Reintroduction of enteral feeding too fast, however, has been associated with the development of recurrent NEC.5,12,13 Therefore, the optimal timing for reintroduction of enteral feeding may be related to the rapidity of intestinal recovery and may be individually determined.
Evidence regarding intestinal recovery after NEC remains limited. The time to full enteral feeding or the development of post-NEC complications can be used to indirectly assess whether the intestine is recovering. Since NEC is associated with a diminished intestinal perfusion affecting gut-integrity, two potential biomarkers for prediction of NEC diagnosis are the regional intestinal oxygen saturation (rintSO2) and intestinal-fatty acid binding protein (I-FABP).14,15,16,17,18,19,20,21,22,23
The rintSO2 represents the intestinal oxygen saturation and can be measured continuously using NIRS, a noninvasive tool used to assess end-organ perfusion.24,25,26 Lower rintSO2 has been reported in preterm infants who subsequently developed NEC,14,16 but also in infants with complicated NEC versus uncomplicated NEC.18,19 I-FABP is a urinary biomarker that represents gut injury as it is released by intestinal enterocytes into the circulation in case of intestinal wall damage.19,20,21,22,23,27 Urinary I-FABP (I-FABPu) levels are higher in NEC infants than in healthy infants and also in infants who developed complicated NEC compared with infants with uncomplicated NEC.22,27 In addition, higher I-FABPu levels are associated with a larger length of subsequent intestinal resection.23
An important first step before individualizing the optimal timing to reintroduce enteral feeding is to establish markers that are helpful in predicting intestinal recovery after NEC. Therefore, we aimed to evaluate whether previously described biomarkers, rintSO2 and I-FABPu, can predict intestinal recovery in preterm infants after NEC.
Methods
Study design
We performed a prospective observational cohort study between January 2015 and May 2017. All preterm infants (GA < 37 weeks) admitted to our tertiary referral NICU with confirmed NEC (Bell’s classification Stage ≥ 2),28 were eligible for inclusion. We excluded infants with congenital abdominal malformations, large chromosomal defects, congenital heart disease with the exception of a PDA, and intraventricular hemorrhage (≥grade 3). Clinical suspicion of NEC was defined as nonspecific signs, such as abdominal distension and/or bloody stools. Definite diagnosis was based on the presence of pneumatosis intestinalis and/or portal venous gas and/or pneumoperitoneum on abdominal radiographs. In infants who needed surgical intervention, pathological/surgical findings were used to confirm or change the staging of NEC. Definite NEC diagnosis and classification were determined by a team of three clinicians (E.M.W.K., J.B.F.H., and A.F.B.), according to the modified Bell’s classification criteria, after completion of the study. All were blinded to the results of the NIRS and I-FABPu data. Agreement was reached in all cases. We defined NEC onset as the time of the first abdominal radiographic examination after clinical suspicion (radiographic examinations from referring hospitals included). The study was approved by the local ethical review board and was registered online (NaNEC-Trial, Dutch Trial Registry NTR4816). We obtained approval for deferred consent, i.e. data collection could start directly after supposed NEC onset for every infant that met the inclusion criteria before parental consent was obtained. To continue participation, informed parental consent was obtained as soon as possible, given the clinical situation.
Data collection
All infants were treated according to the local NEC protocol, consisting of bowel rest (NPO approximately 5 days), antibiotics (7–10 days), and respiratory and/or cardiovascular support if needed. Laparotomy was performed in case of signs of an intestinal perforation or a deteriorating clinical condition despite maximal conservative treatment. Reintroduction of enteral feeding after NPO was based on the hospital protocol, starting with 20 mL/kg on day 6 after NEC, irrespective of Bell’s stage, but on condition that abdominal distension and tenderness had disappeared, bloody stools were absent, and pneumatosis intestinalis had disappeared for at least 24 h on abdominal radiographs.28 Enteral feeding after NEC consisted of mother’s own milk. When mother’s milk was unavailable or of insufficient quantity, the feeding consisted of preterm formula or a combination of both. When reintroduction of feeding was tolerated, feeding volumes were increased daily by 20 mL/kg/day. All infants received enteral feeding through nasogastric tubes. Infants who weighed less than 1250 g received enteral bolus feeding every 2 h and infants who weighed more than 1250 g were fed once every 3 h.
We started to collect rintSO2 values and I-FABPu as soon as possible after suspicion of NEC. Data collection ended when full enteral feeding (FEF) was reached, defined as tolerating enteral feeding of 150 mL/kg/day for at least 24 h. Data collection was ceased in case of earlier discharge from the NICU, when FEF was not reached on day 36 after NEC onset, when NEC diagnosis was rejected, or in case the infant did not survive.
Near-infrared spectroscopy
We used INVOS 5100C near-infrared spectrometers in combination with neonatal SomaSensors (Medtronic, Dublin, Ireland). Underneath each sensor we attached Mepitel® (Mölnlycke, Sweden) to protect the vulnerable skin of the preterm infants and to keep the sensor in place. Previous research reported no adverse effects of Mepitel® on INVOS integrity and validity.26 We placed the sensor infraumbilically on the central abdomen to measure the rintSO2 continuously for at least 2 h every day during the entire study period. rintSO2 values were collected at 0.2 Hz and stored offline. Other vital parameters from the bedside monitor, such as the transcutaneous arterial oxygen saturation (SpO2), were simultaneously stored in the same database. Artifacts of the rintSO2, i.e. moments recorded as sensor displacement, or a sudden major nonphysiological increase/decrease of the rintSO2 values suggesting an incorrect measurement, were removed. After removing these artifacts rintSO2 data of less than 30 min were recorded as missing. Next, we calculated mean rintSO2 values. As the development of NEC might be associated with a loss of variability of the rintSO2, we additionally determined the range (max−min) (rintSO2range) for the same period, as a measure of rintSO2 variability.29 We chose to determine the range instead of other measures for variability,25,26,29 as we sought to assess variability during clinical care. The minimum and maximum rintSO2 values are quickly reproducible on the NIRS monitor, and do not require complex calculations.
Intestinal-fatty acid binding protein
We collected urine once a day during the entire study period in a urine tube of 1.5 mL. If present for clinical reasons, we collected urine from an indwelling catheter. If not, we placed a small cotton wool in the diaper. Once the cotton was saturated, it was squeezed into a sterile syringe pressing the urine into the urine tube wearing rubber gloves. Next, the urine tubes were frozen at −80 °C. Batch analysis was performed by a laboratory technician blinded for patient characteristics. To determine the concentrations of I-FABPu we used sandwich ELISA, based on capture and biotin-labeled detection antibodies with a Human FABP2 kit from R&D Systems (Abingdon, UK). To quantify the concentration of I-FABPu we used a Streptavidin-HRP and OPD substrate. The standard curve had a highest level of 2000 pg/mL. Samples were diluted 100 times in 0.1% BSA/PBS Buffer. Since we previously reported that I-FABPu results of preterm infants are not influenced by creatinine levels, we chose not to correct for creatinine levels.27
Intestinal recovery
We used two different outcomes to assess intestinal recovery. First, as tolerating full enteral feeding by the intestine after NEC onset is used as indicator of intestinal recovery, we used the time to reach FEF as surrogate for intestinal recovery rate. Therefore, we divided surviving infants into two groups, based on the total cohort’s median time to reach FEF (FEFt); one with a rapid intestinal recovery rate (FEFt below median), and the other with a longer intestinal recovery rate (FEFt equal/above median). FEFt was defined as the total amount of days between the first re-feed after NEC onset and FEF. Second, we evaluated whether infants developed recurrent NEC or a post-NEC stricture within the first 6 months after NEC onset and compared them with infants without short-term post-NEC complications.
Demographic and clinical variables
We recorded patient characteristics from the patients’ medical files, including data on prenatal and postnatal characteristics. Furthermore, we collected data regarding NEC development, including postnatal day and PMA at NEC onset, type of NEC treatment (conservative vs. surgical), duration of NPO and the time to the first re-feed, and clinically determined laboratory findings within the first 72 h after NEC onset, short-term complications, and mortality. Furthermore, we collected data concerning respiratory- and circulatory support and other (co)morbidities.
Statistical analysis
We performed the statistical analyses using SPSS 23.0 (IBM Corp., Armonk, NY, USA). To check for differences in patient characteristics between groups, we used the Mann−Whitney U or the chi-square test.
To predict intestinal recovery rate or the development of short-term post-NEC complications, we used the rintSO2, the rintSO2range, and I-FABPu measurements collected within the first 24 h, 24–48 h after NEC onset, and the last measurement before and the first measurement after the first re-feed. First, we determined whether rintSO2, rintSO2range, and I-FABPu levels differed between infants with a rapid and a longer intestinal recovery rate using Mann−Whitney U tests. We also performed this analysis between infants with and without short-term post-NEC complications (for each complication separately). We determined ORs using logistic regression analyses to assess the predictive value of the biomarkers for intestinal recovery rate. Due to the small sample size of the infants who developed short-term post-NEC complications we refrained from determining ORs for this outcome. To facilitate interpretation and present assumed clinically relevant differences, we arbitrarily determined ORs per 10% difference of the rintSO2 and rintSO2range values and per 100 ng/mL difference of I-FABPu, as validated data on clinically relevant differences are lacking. We determined ORs to predict intestinal recovery rate for the entire group and for conservatively treated infants separately, as surgical removal of (ischemic/necrotic) bowel tissue will probably affect the recovery process. We checked whether GA, SGA, gender, and Bell’s NEC classification (Bell’s stage 3 vs. Bell’s stage 2) were associated with intestinal recovery rate. We only checked whether Bell’s NEC classification was associated with intestinal recovery rate in the entire group, as in the conservatively treated group only one infant had Bell’s stage 3A.
Next, we built multiple regression models including independent variables related to outcome with a p value < 0.1. Because interrelated parameters cannot be added into one model, we first checked for multicollinearity using the Spearman’s Rank-Order Correlation test. To determine the added value of combining variables in a multiple model, we evaluated the change in % of the explained variance by the univariate and multiple model, using Nagelkerke R2.
Finally, we generated ROC curves and determined cut-off points for every biomarker that turned out statistically significant in the univariate logistic regression analysis. Next, we performed a multiple regression analysis based on the selected cut-off points. Because of the exploratory nature of our study we chose not to correct for multiple testing. A p value < 0.05 was considered statistically significant.
Results
Patient characteristics
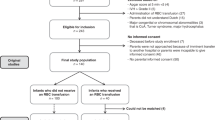
Sixty-seven preterm infants were eligible for inclusion. We excluded 27 infants due to mortality before data could be collected, missing data, lack of consent, or rejection of NEC diagnosis. From the remaining 40 infants, 13 infants (33%) died on median day 2 [IQR: 1–5] after data collection started. Therefore, our final study cohort consisted of 27 surviving infants (Fig. 1). These 27 infants had a median GA of 28.1 [IQR: 26.7–30.9] weeks and a median BW of 1120 [IQR: 810–1525] g. The infants developed NEC on median postnatal day 10 [IQR: 8–20] (PMA: 30.7 [IQR: 29.0–34.3] weeks). Six infants (22%) needed surgical intervention. Three infants (11%) developed recurrent NEC and six infants (22%) developed a post-NEC stricture within the first 6 months after NEC. From the infants who survived the study period, two infants died later on: one due to recurrent NEC (postnatal day 43) and one due to ongoing severe abdominal problems (postnatal day 115). The patient characteristics of the study group are presented in Table 1. The 13 infants who died had a significantly younger median GA of 25.4 [IQR: 24.9–27.6] weeks and a lower median BW of 830 [IQR: 665–1035] g than the survivors.
Prediction of intestinal recovery rate
We present the mean rintSO2 values, rintSO2range, and I-FABPu in Fig. 2. Median FEFt was 14 [IQR: 12–23] days. We found that the rintSO2 and the rintSO2range after the first re-feeding predicted a rapid intestinal recovery rate, both in the entire group and in the subgroup of conservatively treated infants. For every 10% increase in rintSO2 and in rintSO2range, the OR to reach FEF within 14 days was 1.8 (CI: 1.1–3.0) and 3.0 (CI: 1.1–8.1) in all infants and 2.7 (95% CI: 1.1–6.6) and 13.5 (CI: 1.2–157.8) in conservatively treated infants, respectively. Levels of I-FABPu did not significantly predict intestinal recovery rate (Table 2). Intestinal recovery rate was not associated with GA, SGA, gender, or Bell’s classification (Table 2). We did not find a significant multicollinearity between rintSO2 and rintSO2range after the first feeding in the entire group (Spearman’s rho 0.34, p = 0.09), thus we continued with multiple logistic regression analyses. Both variables tended to independently predict a rapid intestinal recovery rate. For every 10% increase in rintSO2 and in rintSO2range the OR to reach FEF within 14 days was 1.7 (CI: 1.0–3.1, p = 0.07) and 2.8 (CI: 1.0–8.1, p = 0.06), respectively. Combining the rintSO2 and rintSO2range in a multiple model increased the explained variance of FEFt within 14 days compared with the univariate models. The percentage of the explained variance increased by 19% for rintSO2 and by 15% for rintSO2range (Nagelkerke R2 increased from 28% to 47% and from 32% to 47%, respectively) compared with the univariate models.
Biomarkers distinguishing between rapid and long intestinal recovery in surviving infants. The boxes represent the individual rintSO2, rintSO2range, and I-FABPu values between the 25th and 75th centiles (interquartile range) between infants with a rapid (<median FEFt of 14 days) and infants with a long intestinal recovery (≥median FEFt of 14 days) presented at four moments; 24 h after NEC (a), 48 h after NEC (b), before the first feeding (c), and after the first feeding (d); the whiskers represent the range of the values with the exception of outliers. Outliers are represented by the circles and diamonds, defined as values between 1.5 interquartile range and 3 interquartile ranges from the end of a box. Significant differences are marked with asterisks: *p < 0.05
Prediction of short-term post-NEC complications
The three infants who developed recurrent NEC did not have a different rintSO2, rintSO2range, and I-FABPu compared with infants who did not develop any short-term post-NEC complication (Fig. 3). The six infants who developed a post-NEC stricture had a smaller rintSO2range (33% [IQR: 32–41] vs. 51% [IQR: 45–57], p < 0.01) and a higher I-FABPu (92.4 ng/mL [IQR: 59.3–398.4] vs. 25.5 ng/mL [IQR: 0.68–42.04], p = 0.03) measured after the first re-feed compared with infants without short-term post-NEC complications (Fig. 3). The rintSO2 after the first re-feed did not differ between infants with and without short-term complications. The rintSO2, rintSO2range, and I-FABPu measured within the first 24 h after NEC onset, 24–48 h after NEC onset and before the first re-feed did not differ between infants with a post-NEC stricture and infants without short-term post-NEC complications.
Biomarkers distinguishing between infants with and without short-term post-NEC complications. The boxes represent the individual rintSO2, rintSO2range, and I-FABPu values between the 25th and 75th centiles (interquartile range) between infants who did and did not develop short-term post-NEC complications presented at four moments; 24 h after NEC (a), 48 h after NEC (b), before the first feeding (c), and after the first feeding (d); the whiskers represent the range of the values with the exception of outliers. Outliers are represented by the circles and diamonds, defined as values between 1.5 interquartile range and 3 interquartile ranges from the end of a box. Significant differences are marked with asterisks: *p < 0.05
ROC curves and cutoff points of r intSO2 values to predict intestinal recovery rate
To establish cut-off points for the assessed biomarkers that predict a rapid intestinal recovery, we generated ROC curves for the rintSO2 and rintSO2range values after the first enteral re-feeding. The area under the rintSO2 curve was 0.77 (CI: 0.58–0.96, p = 0.02) and the area under the rintSO2range curve was 0.79 (CI: 0.59–0.98, p = 0.02). Selecting the optimal cut-off rintSO2 value, we found that rintSO2 after the first re-feed of 53% or higher predicted a rapid intestinal recovery with an OR of 12.0 (CI: 1.2–123.7), with a specificity of 92%, a sensitivity 50%, and a positive predictive value of 86%. Selecting the optimal cut-off rintSO2range value, we found that rintSO2range after the first re-feed of 50% predicted a rapid intestinal recovery with an OR of 11.0 (CI: 1.6–75.5), with a specificity of 85%, a sensitivity of 67%, and a positive predictive value of 80%. The OR for FEFt < 14 days if both the rintSO2 is >53% and the rintSO2range was >50%, was 16.7 (CI: 2.3–122.2).
Adverse events
We observed skin-related effects of the sensor in one of the included infants. This infant showed little skin irritation, which fully resolved 1 day after the sensor was removed. Measurements could be continued without redevelopment of this skin irritation. Furthermore, in two infants, the rintSO2 measurements were interrupted for 1 day after surgery because of severe abdominal tenderness.
Discussion
Our study demonstrates that the intestinal tissue oxygen saturation and its range, but not I-FABPu, measured after the first enteral re-feed after NEC strongly predicts the possibility to reach full enteral feeding within 2 weeks after the first re-feed after NEC onset. In addition, the rintSO2range after the first re-feed was smaller and I-FABPu levels after the first re-feed were higher in infants who developed a post-NEC stricture compared with infants who did not develop a short-term post-NEC complication. These biomarkers were, however, not associated with the development of recurrent NEC. During the first 48 h after NEC onset, the rintSO2 and its range, and I-FABPu did not predict intestinal recovery rate nor the development of short-term post-NEC complications. Our results suggest that these biomarkers have potential value in individualizing feeding regimens after NEC onset.
To distinguish preterm infants with NEC followed by a rapid intestinal recovery from those with longer intestinal recovery, we determined cutoff points for the rintSO2 and rintSO2range after the first enteral re-feed. We intended to establish cut-off points with a high specificity and positive predictive value as we wanted to identify rapid intestinal recovery rather than ruling it out. We found that when the rintSO2 has a value 53% or higher combined with an rintSO2range of 50% or larger, the chance to reach FEF within 14 days is more than 16 times higher. Using these cut-off points may enable physicians to identify infants who may need a more careful reintroduction of enteral feeding.
Possibly, the first enteral feeding after NPO elicits a different physiological intestinal response between infants whose intestine did and did not yet fully recover. A lower rintSO2 after re-feeding suggests that the blood supply to the intestine was still inadequate or the metabolic oxygen demand was still high in infants that needed more time for intestinal recovery. As previous reports described that an impaired intestinal perfusion has been associated with the development of NEC, it is likely that intestinal recovery after NEC is associated with an adequate restoration of perfusion enabling the intestine to respond to physiological changes again.17,18,19,30,31,32 The importance of enabling the intestine to respond to physiological changes has been shown by several studies reporting that loss of variability of rintSO2 measurements is indicative of intestinal distress and associated with the development of NEC.25,29 This suggests that an adequate intestinal perfusion is not only represented by the absolute rintSO2 values but also by a certain amount of variability. This is supported by our findings the chance to reach FEF within 2 weeks increases independently with both a higher rintSO2 and a larger rintSO2range, a coarse measure for variability.
We found similar or even stronger associations after excluding infants who underwent surgery, demonstrated by the higher ORs of the rintSO2 values and its range to predict a rapid intestinal recovery rate in the group of conservatively treated infants. We hypothesize that infants who needed surgical intervention might need more time to tolerate enteral feeding, not only due to a diminished intestinal perfusion or intestinal damage, but also due to a shorter bowel length, attenuating the predictive value of the biomarkers.
We showed that I-FABPu levels at any time after NEC onset did not predict intestinal recovery rate. Previous studies described that I-FABPu is higher during the first 24 h in NEC infants with an intestinal perforation and in infants who die compared with survivors after NEC.19,22 We speculate that even in infants who will recover relatively fast, I-FABPu increases after re-feeding to similar values as in infants that will take longer to tolerate FEF. This means that I-FABPu levels are not able to discriminate between these two groups. It seems that whether the intestine tolerates the reintroduction and increase of feeds does not depend on newly epithelial cell damage. This speculation is supported by an earlier reported piglet model that demonstrated an increased enterocyte turnover after reintroducing enteral feeding.33 Moreover, Reisinger et al. reported that I-FABPu increased after reintroduction of enteral feeding compared with I-FABPu just before the re-feed in NEC infants with a favorable outcome, and not in NEC infants with a poor outcome.34 Although I-FABPu did not predict intestinal recovery rate, we did find higher I-FABPu levels after the first re-feed in infants who developed a post-NEC stricture compared with those who did not. Based on the aforementioned speculation regarding increasing I-FABPu after the first re-feed, infants who develop a post-NEC stricture may have an excessive enterocyte turnover in reaction to feeds, resulting in an imbalance of epithelial tissue and subsequently in the development of a stricture.
Since the first re-feed after NEC and a period of NPO might elicit a physiological intestinal response and an increased enterocyte turnover, the timing of the first re-feed after NEC might influence our previously reported findings. The timing of the first re-feed after NEC onset, however, did not significantly differ between infants with a short time to full enteral feeding and infants with a longer time to full enteral feeding. This supports that our results can be explained by a difference in physiological intestinal response and enterocyte turnover between infants whose intestine did and did not yet fully recover. Moreover, we defined FEFt as the time between the first re-feed and FEF instead of the time between NPO and FEF, to minimalize an eventual effect of the timing of the first re-feed. Furthermore, the feeding volumes of the first re-feed and type of feeding of the first re-feed did not differ between infants with a short time to full enteral feeding and infants with a longer time to full enteral feeding.
To the best of our knowledge, we are the first to demonstrate that the intestinal oxygen saturation and its range measured over a 2-h period after reintroduction of enteral feeding significantly predicted a rapid intestinal recovery rate, represented by the time to full enteral feeding within 14 days after the first re-feed after NEC onset. This is a first step to establish biomarkers to predict intestinal recovery aimed to optimize and individualize NEC treatment in preterm infants.
The strength of our study is the prospective longitudinal design together with the deferred consent to gain more insight in recovery after NEC in preterm infants using NIRS and I-FABPu. Whereas Schat et al. and Schurink et al. demonstrated that these markers are helpful to differentiate between complicated and uncomplicated NEC, we now add the use of these markers to predict intestinal recovery.18,19,22
We are aware of several limitations of our study. First, this study was performed with a small sample size. This may have introduced type-II error, leading to insufficient power to detect differences between groups. Second, we used time to FEF as estimate surrogate for intestinal recovery in the absence of a more valid value. Third, intestinal NIRS measurements might be influenced by stools and air, intestinal peristalsis, and gut movements and it is unclear which part of the intestine is exactly measured using NIRS.14,15,16,18,24,25 Although this is still a point of debate concerning the use of NIRS, previous studies showed strong correlations between rintSO2 measurements and Doppler flow measurements of the small mesenteric artery.35,36 Finally, we chose to use the range of the rintSO2 values as a measure for variability, which is a coarse but practical way to assess variability.
In conclusion, the period surrounding the first enteral re-feed may be important to determine whether an individual infant will have a subsequent rapid intestinal recovery or not. The combined intestinal oxygen saturation and its range, but not I-FABPu, were in particular helpful, whereby cut-off values of rintSO2 above 53% and its range above 50% increased the chance more than 16-fold of reaching full enteral feeding within 14 days. A smaller rintSO2range and higher I-FABPu levels after the first re-feed were associated with the development of post-NEC stricture, but not recurrent NEC. In contrast, during the first 48 h after NEC onset, the intestinal oxygen saturation, its range, and I-FABPu measured did not predict the intestinal recovery rate nor the development of short-term post-NEC complications. Our results suggest that it may be possible to partly individualize post NEC care as feeding regimens may be adjusted to the individual intestinal recovery rate. These are, however, the preliminary results of an exploratory study. Our findings therefore need to be confirmed in larger prospective intervention studies.
References
Mϋller, M. J., Paul, T. & Seeliger, S. Necrotizing enterocolitis in premature infants and newborns. J. Neonatal Perinat. Med. 9, 233–242 (2016).
Lin, P. W. & Stoll, B. J. Necrotising enterocolitis. Lancet 368, 1271–1283 (2006).
Bohnhorst, B. et al. Early feeding after necrotizing enterocolitis in preterm infants. J. Pediatr. 143, 484–487 (2003).
Valpacos, M. et al. Diagnosis and management of necrotizing enterocolitis: an international survey of neonatologists and pediatric surgeons. Neonatology 113, 170–176 (2018).
Hock, A. M. et al. Initiation of enteral feeding after necrotizing enterocolitis. Eur. J. Pediatr. Surg. 28, 44–50 (2018).
Zani, A. et al. EUPSA Network. International survey on the management of necrotizing enterocolitis. Eur. J. Pediatr. Surg. 25, 27–33 (2015).
Patel, P. & Bhatia, J. Total parenteral nutrition for the very low birth weight infant. Semin. Fetal Neonatal Med. 22, 2–7 (2017).
Thureen, P. J. & Hay, W. W. Jr. Early aggressive nutrition in preterm infants. Semin. Neonatol. 6, 403–415 (2001).
Corvaglia, L. et al. Bolus vs. continuous feeding: Effects on splanchnic and cerebral tissue oxygenation in healthy preterm infants. Pediatr. Res. 76, 81–85 (2014).
Ehrenkranz, R. A. et al. Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics 117, 1253–1261. (2006).
Franz, A. R. et al. Intrauterine, early neonatal, and postdischarge growth and neurodevelopmental outcome at 5.4 years in extremely preterm infants after intensive neonatal nutritional support. Pediatrics 123, e101–e109 (2009).
Stringer, M. D. et al. Recurrent necrotizing enterocolitis. J. Pediatr. Surg. 28, 979–981 (1993).
Thyoka, M. et al. Advanced necrotizing enterocolitis Part 2: Recurrence of necrotizing enterocolitis. Eur. J. Pediatr. Surg. 22, 13–16 (2012).
Schat, T. E. et al. Early cerebral and intestinal oxygenation in the risk assessment of necrotizing enterocolitis in preterm infants. Early Hum. Dev. 131, 75–80 (2019).
Patel, A. K. et al. Abdominal near-infrared spectroscopy measurements are lower in preterm infants at risk for necrotizing enterocolitis. Pediatr. Crit. Care Med. 15, 735–741 (2014).
Fortune, P. M., Wagstaff, M. & Petros, A. J. Cerebro-splanchnic oxygenation ratio (CSOR) using near infrared spectroscopy may be able to predict splanchnic ischaemia in neonates. Intensive Care Med. 27, 1401–1407 (2001).
Chen, Y. et al. The role of ischemia in necrotizing enterocolitis. J. Pediatr. Surg. 51, 1255–1261 (2016).
Schat, T. E. et al. Near-infrared spectroscopy to predict the course of necrotizing enterocolitis. PLoS ONE 11, e0154710 (2016).
Schat, T. E. et al. The relation between splanchnic ischaemia and intestinal damage in necrotising enterocolitis. Arch. Dis. Child Fetal Neonatal Ed. 101, F533–F539 (2016).
Thuijls, G. et al. Non-invasive markers for early diagnosis and determination of the severity of necrotizing enterocolitis. Ann. Surg. 251, 1174–1180 (2010).
Frost, B. L., Modi, B. P., Jaksic, T. & Caplan, M. S. New medical and surgical insights into neonatal necrotizing enterocolitis: a review. JAMA Pediatr. 171, 83–88 (2017).
Schurink, M. et al. Intestinal fatty acid-binding protein as a diagnostic marker for complicated and uncomplicated necrotizing enterocolitis: a prospective cohort study. PLoS ONE 10, e0121336 (2015).
Heida, F. H. et al. Intestinal fatty acid-binding protein levels in Necrotizing Enterocolitis correlate with extent of necrotic bowel: results from a multicenter study. J. Pediatr. Surg. 50, 1115–1118 (2015).
Marin, T. & Moore, J. Understanding near-infrared spectroscopy. Adv. Neonatal Care 11, 382–388 (2011).
Cortez, J. et al. Noninvasive evaluation of splanchnic tissue oxygenation using near-infrared spectroscopy in preterm neonates. J. Matern. Fetal Neonatal Med. 24, 574–582 (2011).
McNeill, S., Gatenby, J. C., McElroy, S. & Engelhardt, B. Normal cerebral, renal and abdominal regional oxygen saturations using near-infrared spectroscopy in preterm infants. J. Perinatol. 31, 51–57 (2011).
Schurink, M. et al. Intestinal fatty acid-binding protein in neonates with imminent necrotizing enterocolitis. Neonatology 106, 49–54 (2014).
Walsh, M. C. & Kliegman, R. M. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr. Clin. North Am. 33, 179–201 (1986).
Kalteren, W. S. et al. Red blood cell transfusions affect intestinal and cerebral oxygenation differently in preterm infants with and without subsequent necrotizing enterocolitis. Am. J. Perinatol. 35, 1031–1037 (2018).
Corvaglia, L. et al. Splanchnic oxygenation at first enteral feeding in preterm infants: correlation with feeding intolerance. J. Pediatr. Gastroenterol. Nutr. 64, 550–554 (2017).
Bora, R., Mukhopadhyay, K., Saxena, A. K., Jain, V. & Narang, A. Prediction of feed intolerance and necrotizing enterocolitis in neonates with absent end diastolic flow in umbilical artery and the correlation of feed intolerance with postnatal superior mesenteric artery flow. J. Matern. Fetal Neonatal Med. 22, 1092–1096 (2009).
Murdoch, E. M., Sinha, A. K., Shanmugalingam, S. T., Smith, G. C. & Kempley, S. T. Doppler flow velocimetry in the superior mesenteric artery on the first day of life in preterm infants and the risk of neonatal necrotizing enterocolitis. Pediatrics 118, 1999–2003 (2006).
Oste, M. et al. Formula induces intestinal apoptosis in preterm pigs within a few hours of feeding. JPEN J. Parenter. Enter. Nutr. 34, 271–279 (2010).
Reisinger, K. W. et al. Noninvasive measurement of intestinal epithelial damage at time of refeeding can predict clinical outcome after necrotizing enterocolitis. Pediatr. Res. 73, 209–213 (2013).
Gillam-Krakauer, M. et al. Correlation of abdominal rSO2 with superior mesenteric artery velocities in preterm infants. J. Perinatol. 33, 609–612 (2013).
Bozzetti, V. et al. Evaluation of splanchnic oximetry, doppler flow velocimetry in the superior mesenteric artery and feeding tolerance in very low birth weight IUGR and non-IUGR infants receiving bolus versus continuous enteral nutrition. BMC Pediatr. 12, 106 (2012).
Acknowledgements
We would like to acknowledge the nurses, medical staff of the NICU of Beatrix Children’s Hospital in Groningen, and the medical students, for helping with data collection and for creating the opportunity to carry out this study. This study was part of the research program of the postgraduate school for Behavioural and Cognitive Neurosciences, University of Groningen. S.J.K., W.S.K., and M.J.M. were financially supported by a grant from the Junior Scientific Master Class of the University of Groningen, Groningen, the Netherlands.
Author information
Authors and Affiliations
Contributions
S.J.K., E.M.W.K., J.B.F.H., and A.F.B. conceptualized and designed the study. S.J.K., W.S.K., and M.J.M. collected the data. S.J.K. analyzed the data and drafted the initial manuscript. E.M.W.K. supervised the study. W.S.K., M.J.M., A.F.B., J.B.F.H., and E.M.W.K. reviewed and revised the manuscript critically. All authors approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kuik, S.J., Kalteren, W.S., Mebius, M.J. et al. Predicting intestinal recovery after necrotizing enterocolitis in preterm infants. Pediatr Res 87, 903–909 (2020). https://doi.org/10.1038/s41390-019-0634-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0634-y
This article is cited by
-
Necrotizing enterocolitis: current understanding of the prevention and management
Pediatric Surgery International (2024)
-
The short-term effects of RBC transfusions on intestinal injury in preterm infants
Pediatric Research (2023)
-
Neonatal anemia relates to intestinal injury in preterm infants
Pediatric Research (2022)
-
Galectin-4 as a Novel Biomarker of Neonatal Intestinal Injury
Digestive Diseases and Sciences (2022)
-
Necrotizing enterocolitis in the preterm: newborns medical and nutritional Management in a Single-Center Study
Italian Journal of Pediatrics (2021)