Abstract
Background
Scoring tools used to quantify withdrawal in infants with neonatal abstinence syndrome (NAS) are often confounded by subjective measurements. This study assessed salivary cortisol as an objective biomarker of withdrawal severity in opioid-exposed newborns.
Methods
A prospective study was conducted in 25 full-term opioid-exposed newborns monitored for NAS. Morning and evening salivary cortisol levels were collected starting within 48 h post birth until initiation of pharmacologic treatment for withdrawal (Pre-Treatment) or when the infant was discharged without pharmacotherapy (No Treatment).
Results
Cortisol levels in the Pre-Treatment group (n = 11) were significantly higher within the first week of life (median 1.74 µg/dl) than in the No Treatment group (n = 11; median 0.72 µg/dl; P = 0.003); three infants had inadequate saliva volume for cortisol assay. Cortisol significantly decreased after 72 h post birth among infants discharged without pharmacotherapy (≤72 h median 1.25 µg/dl; ≥72 h median 0.58 µg/dl; P = 0.022), whereas cortisol remained elevated for infants subsequently treated for severity of withdrawal. No cortisol circadian rhythm was observed for either group.
Conclusions
Salivary cortisol in opioid-exposed newborns may provide an index of stress and help identify infants who will have more severe clinical presentation of NAS. Such a biomarker would allow risk stratification for early treatment and discharge decisions.
Similar content being viewed by others
Introduction
The incidence of neonatal abstinence syndrome (NAS) due to in utero exposure to prescribed and/or illicit drugs in the United States has more than doubled between 2009 and 2012, with estimated hospitalization costs surging from US$732 million to US$1.5 billion.1 Newborns with NAS present with physiologic and behavioral impairments that manifest as central nervous system dysregulation, gastrointestinal symptoms, and autonomic instability.2,3,4 Signs and symptoms of drug withdrawal typically develop within 72 h post birth.2,3,4 NAS symptoms result from maternal use of full-opioid agonists such as heroin, oxycodone, methadone, fentanyl and morphine, and partial or mixed agonists such as buprenorphine and tramadol.2,4,5
Non-pharmacologic strategies such as swaddling, minimizing environmental stimuli, breastfeeding, and skin-to-skin care are first-line treatments for reducing the severity of withdrawal in infants with NAS.3,4,6,7 However, many infants still need pharmacologic treatment to manage withdrawal.2,3,4
Current clinical decisions for the initiation, maintenance, and weaning of pharmacologic treatment of infants with NAS are determined by scores on symptom checklists.3,8 Lack of consistency and accuracy in assessing symptoms may result in discrepancies among caregiver ratings, which has implications for management decisions.9
The hypothalamic pituitary adrenal (HPA) axis is part of the neuroendocrine system that helps maintain homeostasis, with a key function of controlling the body’s response to stress. In newborns exposed to opioids in utero, the abrupt cessation of opioids at birth causes the upregulation of cyclic adenosine monophosphate, which differentially stimulates and hinders the production and release of several neurotransmitters, leading to symptoms of drug withdrawal, for example, tachypnea, tachycardia, hypertonicity, hyperthermia, sleep disturbances, vomiting, and poor feeding.2,10,11 The major endogenous glucocorticoid secreted in response to stress is cortisol.12 Serum and salivary cortisol levels are highly correlated in pain-related stress response studies in infants.12 Salivary cortisol may yield more accurate levels of underlying stress compared to serum cortisol because pain and discomfort experienced during invasive blood draws may trigger physiologic responses that affect serum cortisol levels.13,14 Obtaining salivary cortisol is an easy, minimally invasive procedure not confounded by painful venipuncture, which is particularly helpful when working with infants.
Autonomic dysregulation observed in opioid-exposed newborns may be indexed by elevated salivary cortisol levels. We hypothesized that newborns who are subsequently medicated to treat severity of withdrawal would have higher salivary cortisol levels during the first week of life compared to at-risk infants who did not develop severe signs and symptoms of withdrawal and were not pharmacologically treated.
Methods
Setting
A prospective, observational study was conducted at UMass Memorial Healthcare (UMMHC) over a 2-year period between December 2015 and January 2018. The study was approved by the UMass Medical School Institutional Review Board. Written informed consent was obtained from the biological mother of each infant either prenatally or within 48 h post birth. Enrolled infants were studied in the Mother-Baby Unit where they were admitted and cared for after birth.
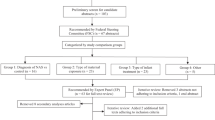
Participants
Twenty-five full-term (≥37 weeks gestational age), opioid-exposed newborns monitored for NAS participated in the study. Candidates with opioid exposure were identified to study personnel by treating physician in the prenatal clinic or Mother-Baby Unit at UMMHC. Inclusion criteria required in-utero opioids with or without other drug exposures. Exclusion criteria included participation in other research studies that included an intervention, preterm (<37 weeks gestational age), congenital defects, hydrocephalus, intraventricular hemorrhage >grade 2, clinically significant cardiac anomalies, anemia (hemoglobin <8 g/dl), human immunodeficiency virus, and/or methicillin-resistant Staphylococcus aureus or other infection requiring treatment at the time of study. Custodial placement into the Department of Children and Families was a withdrawal criterion after initial enrollment.
Procedures
Infants were studied at their bedside in the Mother-Baby Unit during the clinical observation period for opioid withdrawal as per standard of care at UMMHC, that is, on average 4–7 days. The study end time was defined by when medical providers determined pharmacotherapy was warranted and the infant was transferred to the neonatal intensive care unit (NICU) for treatment (Pre-Treatment cohort), or medical providers determined it was safe to discharge the infant without medication (No Treatment cohort). Nurses performed routine clinical assessment of the infant’s withdrawal severity in accordance with the Institution’s standard clinical care, approximately every 3 to 4 h using the Restructured Finnegan Scoring Tool.9 Prenatal drug exposure was determined by confirmation of a positive opioid screen with or without poly-drug exposure (9-panel: Amphetamines, Barbiturates, Benzodiazepines, Cocaine Metabolite, Marijuana Metabolite, Methadone Metabolite, Opiates, Oxycodone, Phencyclidine) from infant urine or meconium toxicology, maternal urine toxicology, or from documented prescribed maternal opiate medications (in instances when buprenorphine toxicology was not performed). Finnegan scores and toxicology reports were obtained by study staff from the infant and maternal medical records.
Salivary cortisol collection
Buccal/sublingual salivary samples were collected twice daily, between ~7 a.m. and 10 a.m. (morning sample) and between ~4 p.m. and 6 p.m. (evening sample). Salivary cortisol collection began within 48-h post birth while the infant was being observed clinically for withdrawal. Collection continued throughout the infant’s hospital stay until the infant was either started on pharmacologic treatment for severe withdrawal symptoms (i.e., three consecutive Finnegan scores ≥8 or two consecutive Finnegan scores ≥12) or the infant was discharged from the hospital without pharmacologic treatment.
Salivary cortisol collection started before anticipated feed or 30 min after infant completed feed.15 To collect the samples, research study staff held one end of a salivary swab (Salimetrics® SalivaBio Infant Swab, Carlsbad, CA) and placed the other end of the swab inside the infant’s buccal mucosa or sublingually to absorb saliva. Infant was placed supine with head to the side in his/her crib to help ensure pooling of saliva.
Research staff noted the infant’s behavioral state at the start and end of the sample collection on a continuum: 0 = Sleeping defined by eyes closed, no/minimal sound, minimal movement; 1 = Quiet Awake defined by eyes opened, no/minimal sound, minimal movement; 2 = Partial Distress defined by eyes opened or closed, movements, intermittent cries; 3 = Full Distress defined by eyes opened or closed, movements, continuous cries. Sample collection time was increased during the study sessions to improve the saliva quantity output (recommended collection volume 75 µl for a test volume 25 µl16). Immediately following salivary collection, swabs were placed in a de-identified coded swab storage tube (Salimetrics®, State College, PA). Samples were either immediately placed in frozen storage (−30 °C) or centrifuged (15 min; 3000 r.p.m.; 4 °C) and placed in frozen storage until the time of assay.16 Batches of frozen samples were sent out for duplicate assay of each sample within 3–6 months of collection and tested using cortisol enzyme immunoassay (Salimetrics®, Carlsbad CA; serum-saliva correlation 0.91, sensitivity <0.007 µg/dl).
Statistics
Statistical calculations were performed using commercially available software (SPSS version 25, Chicago, IL). Non-parametric analyses were used for analysis of data sets. Kruskal–Wallis one-way analysis of variance was used to compare likelihood of adequate sample volume among the buccal swab durations. Bonferroni adjustment is reported for post hoc tests with multiple comparisons. Spearman’s rank tests were used to establish associations between cortisol levels, swab duration, and behavioral state. Wilcoxon’s rank-sum test was used to compare matched samples (pre and post swab behavioral states; morning and evening cortisol levels). Mann–Whitney U test was used to compare distributions over the course of the week between infants who were subsequently pharmacologically managed (Pre Treatment) and those who were not (No Treatment). Values are expressed as median and interquartile range (IQR). P values <0.05 were considered statistically significant.
Missing data
Cortisol was collected within the first week of life among infants. Reasons for missing samples include varying entry times into the study (impacting the total number of samples collected per subject in the first 48 h of life), shorter nursery stay due to earlier discharge home or start of pharmacotherapy, insufficient quantity of saliva obtained (samples in which one or both assays were inadequate), and inability to obtain sample within allotted morning or evening collection period.
Results
Subject demographics and clinical characteristics
Pertinent demographic, prenatal, and postnatal characteristics are listed in Table 1. A total of 41 mothers were approached to participate in the study. Seven mothers declined. Three subjects who consented prenatally were subsequently excluded at birth prior to the start of salivary sample collection because one mother opted to withdraw post partum, one infant whose mother consented prenatally was not delivered at UMMHC, and one infant was <37 weeks of gestation. Six subjects were withdrawn after the start of salivary sample collection: two subjects were withdrawn from the study on the first day of data collection because the infants were irritable and their mothers chose to withdraw from the study, two subjects entered into a separate study within 30 h of birth and received an intervention that would confound results, and two subjects were placed in state custodial care within the first days of life.
Sample collection duration to achieve adequate saliva sample
For the 25 subjects who completed participation in the study, only cortisol samples in which duplicate assay results were obtained were included in analysis. The mean cortisol level of the duplicate assay collection was used. A total of 179 salivary cortisol samples were collected; 59 samples did not have adequate volume (i.e., were <25 µl) for duplicate assay, including three infants who did not have adequate amount of saliva in any of their samples to obtain cortisol levels. Increasing the duration of the buccal/sublingual swab collection (range 2–25 min) increased the likelihood of obtaining the minimum volume needed to perform the assay (P < 0.001). Post-hoc pairwise comparisons among five intervals [2 min (>1 ≤ 2 min); 5 min (>2 ≤ 5 min); 10 min (>5 ≤ 10 min); 15 min (>10 ≤ 15 min) and 25 min (>15 ≤ 25 min)] revealed a significant increase in collection rate with longer collection duration among all intervals (P < 0.03), except between 2 and 5 min and between 15 and 25 min (see Fig. 1).
Increasing saliva collection duration improves sample rate. Longer saliva collection times [duration range: 2 min (>1 ≤ 2 min); 5 min (>2 ≤ 5 min); 10 min (>5 ≤ 10 min); 15 min (>10 ≤ 15 min); and 25 min (>15 ≤ 25 min)] significantly increased rate of obtaining salivary cortisol levels (P < 0.001), except between 2 and 5 min and between 15 and 25 min (NS, not significant)
There was no change in behavioral state between the start and end of salivary swab collection in 53% of subjects, with 43% infants remaining at 0 distress (Sleeping) throughout the sampling period. In 42% of subjects distress increased and in 5% of subjects distress decreased over the sampling period. The increase in infant distress between the start and end of saliva collection was observed for both the Pre-Treatment group (P = 0.001) and No Treatment group (P < 0.001). At the start of the salivary swab, the Pre-Treatment group had a higher behavioral state score than the No Treatment group (P = 0.002). There was no difference in behavioral state scores between groups at the end of salivary collection (P = 0.101). There was no correlation between cortisol level and observed infant behavioral state for either the Pre-Treatment or No Treatment group, or the start or end of saliva collection.
Cortisol levels and pharmacological treatment
Of the 22 subjects in whom reliable cortisol samples were obtained, 11 subjects were subsequently treated pharmacologically for symptoms of severe withdrawal and 11 subjects were discharged home without pharmacologic intervention. As indicated in Table 1 more infants in the Pre-Treatment group had prenatal exposure to buprenorphine (n = 10) than infants in the No Treatment group (n = 4; P = 0.028). In the Pre-Treatment group, maternal buprenorphine dose at the time of delivery was ≥8 mg/day in 9/10 subjects, and 4/10 buprenorphine-exposed subjects had poly-drug exposure including one whose mother was on low-dose buprenorphine (<8 mg/day) at the time of delivery. The No Treatment group included four buprenorphine-exposed infants (maternal dose at time of delivery was ≥8 mg/day in 3/4 subjects; 1 with unknown dose), including two who had poly-drug exposure.
Diurnal cortisol
Of the 120 reliable cortisol samples, there were 42 “paired” samples in which a morning and evening sample were obtained on the same day. There was no statistically significant difference in salivary cortisol levels between morning (median 0.89 µg/dl, IQR 0.38–1.52 µg/dl) and evening (median 0.75 µg/dl, IQR 0.32–2.33 µg/dl; P = 0.425). There was also no difference between the morning and evening cortisol levels for pharmacologically treated infants (n = 16 pairs; median 1.45 µg/dl, IQR 0.43–2.18 µg/dl; 1.74 µg/dl, IQR 0.38–2.67 µg/dl, respectively; P = 0.581) or for infants who were not treated with medication (n = 26 pairs; median 0.78 µg/dl, IQR 0.31–1.17; 0.75 µg/dl 0.25–1.36, respectively; P = 0.679).
Cortisol in the first week of life
Given that there were no differences in the diurnal cortisol levels among subjects in the Pre-Treatment or No Treatment group, for weighting purposes a single daily value was obtained for each subject on a given day, that is, morning and evening values were averaged if both samples were obtained (n = 42), or only the morning (n = 17) or evening (n = 19) values were included in analysis if both cortisol samples were not obtained on the same day. Accordingly, there were 32 cortisol values in the Pre-Treatment group (23 samples ≤72 h post birth; 9 samples >72 h post birth), and 46 cortisol values in the No Treatment group (24 samples ≤72 h post birth; 22 samples >72 h post birth).
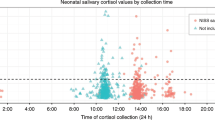
Figure 2 shows individual daily cortisol levels within the first week of life among the 22 subjects in whom reliable cortisol samples were obtained, based on hours from birth. On average, cortisol levels were significantly higher for infants who subsequently received pharmacological management for NAS (median 1.74 µg/dl, IQR 0.78–3.23 µg/dl) compared to infants who were not pharmacologically treated (median 0.72 µg/dl, 0.37–1.64 µg/dl; P = 0.003). Analysis adjusting for when no cortisol levels were obtained in the Pre-Treatment group due to the start of pharmacotherapy (i.e., exclude values >138 h post birth) showed over equivalent time periods cortisol levels remained significantly higher in the Pre-Treatment cohort (median 1.74 µg/dl, IQR 0.78–3.23 µg/dl) compared to the No Treatment cohort (median 0.86 µg/dl, IQR 0.40–1.75 µg/dl; P = 0.010).
Salivary cortisol levels in the first week of life. Panel A Pre-Treatment Cohort. Closed circles indicate individual salivary cortisol levels among subjects who subsequently received pharmacological treatment for withdrawal. Panel B No Treatment Cohort. Open circles indicate individual salivary cortisol levels among subjects who did not need pharmacotherapy. Sun symbol (¤) indicates two overlapping values at time point (closed and open, respective panels). Dotted lines indicate median salivary cortisol level over the course of the study period. Solid lines indicate median salivary cortisol levels for time intervals ≤72 h post birth and >72 h post birth
There was no difference in cortisol levels between opioid-only and opioid-poly-drug exposure for either the Pre-Treatment cohort (P = 0.25) or the no Treatment cohort (P = 0.51). Among the opioid-only exposed infants (n = 16), cortisol levels were higher in the Pre-Treatment than No Treatment cohort (P = 0.037). Of note, cortisol values were not affected by circumcision; among the 11 males studied, cortisol values were obtained in only one infant pre- and post circumcision, and the post-circumcision cortisol level was lower than the cortisol pre-circumcision.
As illustrated in Fig. 2, for subjects who did not receive pharmacologic treatment, cortisol levels were twice as high within the first 72 h of birth (median 1.25 µg/dl, IQR 0.47–1.97 µg/dl) compared to the latter part of the week (median 0.58 µg/dl, IQR 0.27–1.08 µg/dl; P = 0.022), whereas cortisol levels remained elevated throughout this study period (respectively, ≤72 h median 2.06 µg/dl, IQR 0.49–3.75 µg/dl; >72 h median 1.47 µg/dl, IQR 0.96–2.18 µg/dl; P = 0.536) for infants who were subsequently treated for severe withdrawal symptoms.
Traditional measures of NAS severity
Finnegan scores nearest the salivary sampling period were higher in the first week of life among infants who were subsequently treated (median 5.0, IQR 2–7) than among infants who were discharged without pharmacological management (median 4.0, IQR 2–5; P = 0.021). Infants who were subsequently treated pharmacologically (median days on morphine 23.0, IQR 11–36 days) had a significantly longer length of hospitalization (median 26.0 days, IQR 16–42 days) than infants discharged without pharmacotherapy (median 6.0 days, IQR 5–7 days; P < 0.001).
Discussion
This study describes a novel approach to examine salivary cortisol levels as a biomarker for severity of withdrawal in opioid-exposed newborns. Salivary cortisol levels within the first week of life were higher in infants who subsequently received pharmacologic treatment to manage their withdrawal symptoms compared to infants who were discharged home without the need for pharmacotherapy. As is typically observed in healthy infants, we found cortisol levels decreased a few days after birth in our cohort of infants who were not treated with pharmacotherapy.17,18 In contrast, cortisol levels remained elevated after 72 h of life in study infants who subsequently were admitted to the NICU to treat their withdrawal. These findings support our hypothesis that salivary cortisol may provide an index of underlying autonomic dysregulation and help identify infants who will have more severe withdrawal.
We found that a 2 min buccal/sublingual swab collection period, common protocol for obtaining salivary cortisol,16 resulted in inadequate aliquot for obtaining reliable cortisol levels in nearly 70% of samples. Increasing saliva collection duration significantly improved sample rates. Durations <5 min resulted in inadequate volumes to obtain reliable cortisol levels in half the samples, whereas durations >10 min increased sample rates to 80%; 100% adequate volumes were obtained for swab durations between 15 and 25 min. These data suggest that a minimum of 10 min collection period with a buccal/sublingual swab should be used to help ensure adequate salivary aliquot necessary for a reliable cortisol assay in opioid-exposed newborns.
Consistent with Francis et al.19 who found no relationship between state of arousal and adrenal activity, we observed no significant relationship between behavioral state during the collection period and salivary cortisol levels. It is possible salivary swab collection served as a stressor in some infants (i.e., increased arousal/distress). However, studies suggest that cortisol levels peak 20–25 min after initiation of an acute stressor.20 Because nearly all swab durations in this study lasted under 20 min (two swabs were 20 min, one swab was 25 min), we feel salivary swab collection did not likely affect cortisol levels within the sampling period. Rather, the cortisol levels obtained in this study reflected the infant’s underlying “resting” postprandial stress state.
Unique to this study were findings that salivary cortisol levels were significantly higher within the first week of life in opioid-exposed infants who subsequently received pharmacologic treatment for withdrawal compared to infants whose withdrawal was not treated with pharmacotherapy. Cortisol levels within the first week of life among the No Treatment cohort (range 0.091–2.75 µg/dl, one outlier at 5.433 µg/dl) were nearly identical to those observed in healthy newborns (e.g., 0.09–2.08 µg/dl; 19) In contrast, cortisol levels in the Pre-Treatment group were significantly higher (range 0.273–5.433; nearly 50% of the samples >2.0 µg/dl). Moreover, there was a significant reduction in mean cortisol levels ~3 days after birth among infants who had minimal withdrawal signs and symptoms, consistent with adrenal function in healthy newborns, compared to infants who subsequently received pharmacologic treatment. This suggests newborns that were opioid exposed but not symptomatic enough to receive pharmacologic treatment are physiologically similar to non-exposed healthy newborns.
Subjects in this study presented with elevated cortisol levels over the first days of life consistent with physical and emotional stressors of labor and delivery. Higher cortisol levels are commonly observed with spontaneous parturition, prolonged labor, and delivery complications, whereas lower cortisol levels are observed with cesarean section deliveries.21,22,23 In the present study, very few infants were delivered via cesarean section (four Pre-Treatment, two No Treatment). Notably, cortisol levels in the Pre-Treatment group remained elevated throughout the study period. Acute pain associated with circumcision did not play a role in these findings as only one infant in the Treatment group had cortisol levels surrounding circumcision and these levels were lower post circumcision.
We speculate that cortisol differences between the Pre-Treatment and No Treatment cohorts may reflect inherent differences in the HPA axis response to stressors caused by withdrawal among opioid-exposed infants. It may be that in infants with more severe withdrawal, the capacity to respond to stressors and maintain homeostasis via the HPA axis is not functioning properly, resulting in an overstimulation of cortisol release. This is consistent with findings in adults where the HPA axis is activated during opioid withdrawal, resulting in increased cortisol production that is also associated with signs and symptoms of acute withdrawal.24,25,26 While responding to stressors may serve as a protective immediate response, continuously elevated cortisol levels may result in persistent changes in the HPA axis with detrimental long-term neurodevelopment consequences, including cognitive and memory impairments, affective disorders, depression, anxiety, as well as immune deficiencies, suppression of proper gonadal function, and increase in insulin resistance.27,28,29,30,31
Salivary cortisol concentrations did not vary between morning and evening samples, consistent with reports that healthy full-term newborns do not demonstrate a circadian rhythm of salivary cortisol until at least 1 month of age.32,33 Although the fetal HPA system responsible for cortisol release is functional by the second trimester of human gestation, cortisol circadian rhythms with a peak in the morning and nadir in the evening are not established until the first few months of life in healthy infants.32,33 It is unknown from the present study whether infants exposed to opioids develop typical cortisol circadian rhythms in later months, or if disrupted sleep and other physiologic stressors associated with drug withdrawal affect the HPA axis and impair the development of healthy cortisol-releasing responses. It is also possible that the constellation of dysregulated autonomic nervous system responses often observed in opioid-exposed newborns are due to an immature HPA system or early programming of stress response and overexposure to glucocorticoids in utero.34 Jansson et al.35 observed lower vagal tone and higher heart rate were associated with symptom severity in the first few days of life among methadone-exposed newborns, supporting the hypothesis that in utero programming may be responsible for withdrawal symptoms associated with dysregulated autonomic functioning post birth. Future studies that examine the development of cortisol circadian rhythm among opioid-exposed newborns are warranted to help delineate whether persistent stressors alter the infant’s HPA axis prenatally or post partum, or if opioid exposure in utero results in an immature HPA system that exacerbates autonomic system dysregulation that often characterizes prolonged withdrawal in newborns.
Most infants in our study cohort were exposed prenatally to buprenorphine (72%; 14/22). Infants of mothers who are treated with buprenorphine for substance use disorder have comparable risk for NAS that warrants pharmacologic treatment to those infants prenatally exposed to methadone.36,37 Consistent with this literature, half the subjects in our study cohort developed symptoms that subsequently warranted treatment, whereas half were discharged without pharmacotherapy.38 In our study 10/14 buprenorphine-exposed infants were subsequently treated; this is not extraordinary, although the higher treatment rate may reflect other exposure confounds. Nine buprenorphine-exposed infants in the Pre-Treatment group had mothers whose dose was ≥8 mg/day at the time of delivery, including three infants with poly-exposure; the 10th infant whose dose was <8 mg also had poly-exposure. Higher buprenorphine exposure doses (≥8 mg/day), polysubstance use, and exposures to medications such as antidepressants may contribute to exacerbated symptoms and increased risk for prolonged treatment.36,39 However, it remains unclear why some infants develop symptoms that warrant pharmacotherapy, whereas others do not. This challenge is in part due to scoring tools that are complicated to use and prone to subjective interpretation of withdrawal.9 Salivary cortisol levels may prove to be a useful objective marker of withdrawal severity.
In the present study, birth weight was significantly higher among infants who were subsequently treated for severity of withdrawal than infants whose symptoms did not warrant pharmacotherapy, corroborating findings that higher infant birth weight increases likelihood of pharmacological management of NAS.38 However, others have found no relationship between birth weight and severity of NAS symptoms.4 Birth weight is likely dependent on other factors that may also contribute to severity of symptoms, such as gestational period, drugs of exposure, timing and duration of drug exposure in utero, and genetics.2,11,38 Larger studies examining these covariates and other factors, as well as biomarkers such as salivary cortisol, are needed to identify infants at risk for severity of withdrawal.
Limitations to this study are small sample and incomplete results from all time points limiting extrapolation of findings. We were not able to obtain salivary cortisol samples daily in every subject in the study. Our initial sampling time was based on standard guidelines,16 but this was an inadequate duration for obtaining adequate volume of saliva for analysis resulting in no data points for several of the initial samples. Although we corrected this problem by adjusting saliva collection duration, we had fewer values to analyze for the first several infants in the study, reducing power to assess repeated measures over time. Furthermore, once an infant was treated with medication or discharged home, we did not obtain cortisol levels, limiting the number of samples towards the end of the first week.
Trials with a larger cohort that include multiple exposures and a control group with no exposures will serve to determine whether infants with elevated salivary cortisol levels in the first week of life are at risk for more severe and prolonged withdrawal. Studies designed to minimize missing samples will also help confirm this risk. Studying newborns receiving pharmacologic treatment will help determine if salivary cortisol levels can also be a marker of medication capture of withdrawal symptoms. Further, continuing collection past the “observation” period (e.g., for entirety of treatment; after discharge from hospital) will help determine if opioid-exposed newborns with elevated salivary cortisol levels during first weeks of life have the capacity to respond to stressors and maintain homeostasis via the HPA axis over time.
Conclusion
In this cohort of opioid-exposed newborns, salivary cortisol levels were significantly higher within the first week of life in infants who were subsequently managed with pharmacotherapy compared to infants who were discharged home without medication to treat withdrawal. This is noteworthy because levels were twice as high in the Pre-Treatment cohort in the first few days of life, even prior to being symptomatic enough to warrant treatment. This suggests that salivary cortisol in opioid-exposed newborns may provide an index of stress levels and help identify infants who will have more severe withdrawal. Such a biomarker would allow risk stratification for early treatment and/or discharge decisions. Larger prospective studies are needed to validate salivary cortisol as a clinical biomarker of withdrawal before it can be used as a monitoring tool for withdrawal in opioid-exposed neonates.
References
Patrick, S. W., Davis, M. M., Lehmann, C. U., Lehman, C. U. & Cooper, W. O. Increasing incidence and geographic distribution of neonatal abstinence syndrome: United States 2009 to 2012. J. Perinatol. 35, 650–655 (2015).
Kocherlakota, P. Neonatal abstinence syndrome. Pediatrics 134, 547–561 (2014).
Hudak, M. L. & Tan, R. C. Neonatal drug withdrawal. Pediatrics 129, 540–560 (2012).
Jansson, L. M., Velez, M. & Harrow, C. The opioid-exposed newborn: assessment and pharmacologic management. J. Opioid Manag. 5, 47–55 (2009).
Trescot, A. M., Datta, S., Lee, M. & Hansen, H. Opioid pharmacology. Pain Physician 11, 133–153 (2008).
MacMullen, N. J., Dulski, L. A. & Blobaum, P. Evidence-based interventions for neonatal abstinence syndrome. Pediatr. Nurs. 40, 165–172 (2014). 203.
Sublett, J. Neonatal abstinence syndrome: therapeutic interventions. MCN Am. J. Matern. Nurs. 38, 102–107 (2013).
Finnegan, L. P., Connaughton, J. F., Kron, R. E. & Emich, J. P. Neonatal abstinence syndrome: assessment and management. Addict. Dis. 2, 141–158 (1975).
Timpson, W., Killoran, C., Maranda, L., Picarillo, A. & Bloch-Salisbury, E. A quality improvement initiative to increase scoring consistency and accuracy of the finnegan tool. Adv. Neonatal Care 18, 70–78 (2018).
Anand, K. J. S. et al. Tolerance and withdrawal from prolonged opioid use in critically ill children. Pediatrics 125, 1208–1225 (2010).
Kraft, W. K. & van den Anker, J. N. Pharmacologic management of the opioid neonatal abstinence syndrome. Pediatr. Clin. N. Am. 59, 1147–1165 (2012).
Kirschbaum, C. & Hellhammer, D. H. Salivary cortisol in psychobiological research: an overview. Neuropsychobiology 22, 150–169 (1989).
Tennant, F. The physiologic effects of pain on the endocrine system. Pain Ther. 2, 75–86 (2013).
Li, S. X. et al. Serum cortisol secretion during heroin abstinence is elevated only nocturnally. Am. J. Drug Alcohol Abus. 34, 321–328 (2008).
Magnano, C. L., Diamond, E. J. & Gardner, J. M. Use of salivary cortisol measurements in young infants: a note of caution. Child Dev. 60, 1099 (1989).
Salimetrics, L. L. C. Collection Methods: SalivaBio Infant’s Swab (SIS), Vols. C3-5001.08 (State College, 2018).
Rokicki, W., Forest, M. G., Loras, B., Bonnet, H. & Bertrand, J. Free cortisol of human plasma in the first three months of life. Biol. Neonate 57, 21–29 (1990).
Seshagiri, K. & Harischandra, Y. V. Cortisol levels in healthy term and preterm appropriate for gestation infants. Int. J. Contemp. Med. Res. 4, 1659–1664 (2017).
Francis, S. J. et al. Assessment of adrenocortical activity in term newborn infants using salivary cortisol determinations. J. Pediatr. 111, 129–133 (1987).
Ramsay, D. & Lewis, M. Reactivity and regulation in cortisol and behavioral responses to stress. Child Dev. 74, 456–464 (2003).
Mears, K., Mcauliffe, F., Grimes, H. & Morrison, J. J. Fetal cortisol in relation to labour, intrapartum events and mode of delivery. J. Obstet. Gynaecol. (Lahore) 24, 129–132 (2004).
Miller, N. M., Fisk, N. M., Modi, N. & Glover, V. Stress responses at birth: determinants of cord arterial cortisol and links with cortisol response in infancy. BJOG Int. J. Obstet. Gynaecol. 112, 921–926 (2005).
Vogl, S. E. et al. Mode of delivery is associated with maternal and fetal endocrine stress response. BJOG Int. J. Obstet. Gynaecol. 113, 441–445 (2006).
Bearn, J., Buntwal, N., Papadopoulos, A. & Checkley, S. Salivary cortisol during opiate dependence and withdrawal. Addict. Biol. 6, 157–162 (2001).
Kreek, M. J. & Koob, G. F. Drug dependence: stress and dysregulation of brain reward pathways. Drug Alcohol Depend. 51, 23–47 (1998).
Camí, J., Gilabert, M., San, L. & de la Torre, R. Hypercortisolism after opioid discontinuation in rapid detoxification of heroin addicts. Br. J. Addict. 87, 1145–1151 (1992).
Graham, Y. P., Heim, C., Goodman, S. H., Miller, A. H. & Nemeroff, C. B. The effects of neonatal stress on brain development: implications for psychopathology. Dev. Psychopathol. 11, 545–565 (1999).
McEwen, B. S. & Sapolsky, R. M. Stress and cognitive function. Curr. Opin. Neurobiol. 5, 205–216 (1995).
Sapolsky, R. M. & Meaney, M. J. Maturation of the adrenocortical stress response: neuroendocrine control mechanisms and the stress hyporesponsive period. Brain Res. Rev. 11, 65–76 (1986).
Whirledge, S. & Cidlowski, J. A. Glucocorticoids, stress, and fertility. Minerva Endocrinol. 35, 109–125 (2010).
Yehuda, R., Giller, E. L., Southwick, S. M., Lowy, M. T. & Mason, J. W. Hypothalamic-pituitary-adrenal dysfunction in posttraumatic stress disorder. Biol. Psychiatry 30, 1031–1048 (1991).
Ivars, K. et al. Development of salivary cortisol circadian rhythm and reference intervals in full-term infants. PLoS ONE 10, 1–13 (2015).
Castro, M. et al. Salivary cortisol as a tool for physiological studies and diagnostic strategies. Braz. J. Med. Biol. Res. 33, 1171–1175 (2000).
O’Connor, T. G., Bergman, K., Sarkar, P. & Glover, V. Prenatal cortisol exposure predicts infant cortisol response to acute stress. Dev. Psychobiol. 55, 145–155 (2013).
Jansson, L. M., DiPietro, J. A., Elko, A. & Velez, M. Infant autonomic functioning and neonatal abstinence syndrome. Drug Alcohol Depend. 109, 198–204 (2010).
Jansson, L. M. et al. Maternal buprenorphine treatment and fetal neurobehavioral development. Am. J. Obstet. Gynecol. 216, 1–529.e8 (2017). 529.
Jones, H. E. et al. Neonatal abstinence syndrome after methadone or buprenorphine exposure. N. Engl. J. Med. 363, 2320–2331 (2010).
Kaltenbach, K. et al. Predicting treatment for neonatal abstinence syndrome in infants born to women maintained on opioid agonist medication. Addiction 107, 45–52 (2012).
Wong, J. et al. Does maternal buprenorphine dose affect severity or incidence of neonatal abstinence syndrome? J. Addict. Med. 12, 435–441 (2018).
Acknowledgements
We thank Mrs. Barbara Glidden for assistance in data collection. We also thank Dr. Tiffany Moore Simas for laboratory support for the preparation and storage of the salivary cortisol samples. We gratefully acknowledge the infants and parents for participating in this study. We appreciate the cooperation of the staff nurses and attendings in the Mother-Baby Unit at UMass Memorial Healthcare on this project and their tireless and endless work to improve the care of all babies in the unit. This research did not receive any specific grant funding from agencies in the public, commercial, or not-for-profit sectors. This project was supported by the Neonatology Associates of Worcester and the University of Massachusetts Medical School, Department of Pediatrics.
Author information
Authors and Affiliations
Contributions
E.B.-S. conceived the study. E.B.-S. and NR made substantial contributions to study design, acquisition of data, and analysis. All authors made substantial contributions to interpretation of data, to drafting the article or revising it critically for important intellectual content, and approve the manuscript for submission to Pediatric Research.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rodriguez, N., Vining, M. & Bloch-Salisbury, E. Salivary cortisol levels as a biomarker for severity of withdrawal in opioid-exposed newborns. Pediatr Res 87, 1033–1038 (2020). https://doi.org/10.1038/s41390-019-0601-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0601-7
This article is cited by
-
Disarray in the perinatal management of neonatal abstinence syndrome
Pediatric Research (2022)
-
Commentary on salivary cortisol levels as a biomarker for severity of withdrawal in opioid-exposed newborns
Pediatric Research (2020)