Abstract
Background
Neonatal encephalopathy following perinatal asphyxia is a leading cause for neonatal death and disability, despite treatment with therapeutic hypothermia. 2-Iminobiotin is a promising neuroprotective agent additional to therapeutic hypothermia to improve the outcome of these neonates.
Methods
In an open-label study, pharmacokinetics and short-term safety of 2-iminobiotin were investigated in neonates treated with therapeutic hypothermia. Group A (n = 6) received four doses of 0.16 mg/kg intravenously q6h. Blood sampling for pharmacokinetic analysis and monitoring of vital signs for short-term safety analysis were performed. Data from group A was used to determine the dose for group B, aiming at an AUC0–48 h of 4800 ng*h/mL.
Results
Exposure in group A was higher than targeted (median AUC0–48 h 9522 ng*h/mL); subsequently, group B (n = 6) received eight doses of 0.08 mg/kg q6h (median AUC0–48 h 4465 ng*h/mL). No changes in vital signs were observed and no adverse events related to 2-iminobiotin occurred.
Conclusion
This study indicates that 2-iminobiotin is well tolerated and not associated with any adverse events in neonates treated with therapeutic hypothermia after perinatal asphyxia. Target exposure was achieved with eight doses of 0.08 mg/kg q6h. Optimal duration of therapy for clinical efficacy needs to be determined in future clinical trials.
Similar content being viewed by others
Background
Neonatal encephalopathy (NE) after perinatal asphyxia remains one of the leading causes for neonatal death and other adverse outcomes in term and near-term neonates, affecting between 0.5 and 2 of every 1000 live born children in high-income countries.1,2,3 Currently, the only established strategy to reduce brain injury following perinatal asphyxia is therapeutic hypothermia (TH), i.e., lowering the core temperature of the infant to 33–34 °C for 72 h by whole-body cooling.1 TH has reduced the composite adverse outcome of death and disability such as cerebral palsy, hearing loss and neurodevelopmental disorders from approximately 60% to 45%.2,3 Combining TH with additional neuroprotective strategies is, however, urgently needed in order to further improve the outcome of these neonates.4
Molecular pathways contributing to NE have been partly unraveled during the past decades.5 An excessive production of excitatory neurotransmitters promotes the activation of N-methyl d-aspartate and the opening of voltage-regulated ion channels. This results in an increase of intracellular calcium in neuronal cells causing mitochondrial failure, production of pro-radicals, and accumulation of xanthine. Further steps lead to reaction of superoxide free radical with nitric oxide (NO) to form peroxynitrite.4 End products of this process such as nitrotyrosine have been demonstrated postmortem in brain and spinal cord tissue of neonates who died after severe NE.6,7
Production of NO is catalyzed by the enzyme nitric oxide synthase (NOS, enzyme commission number 1.14.13.39). Three isoforms of NOS have been identified: endothelial (eNOS), neuronal (nNOS), and inducible NOS (iNOS). All three isoforms are upregulated after NE; both nNOS and eNOS immediately after reperfusion, iNOS from approximately 12 h onwards.8 Excessive production of nNOS and iNOS has shown to be deleterious to the brain in several animal models for NE.9,10,11 Selective inhibition of nNOS and iNOS is therefore a potential target for additional neuroprotection.4,12
2-Iminobiotin is a biotin analog and has been identified as a selective inhibitor of nNOS and iNOS. 2-Iminobiotin has shown favorable results in several preclinical studies regarding safety and efficacy and is available in a stable, inexpensive formulation suitable for human use. Therefore, it is a likely candidate to advance to clinical studies.12,13,14,15,16,17 Based on a piglet model for NE, target exposure to 2-iminobiotin was determined as an area under the concentration time curve from 0 to 24 h (AUC0–24 h) of 2400 ng*h/mL as higher exposure in that study did not result in additional neuroprotection.18 However, iNOS is assumed to be upregulated for up to 48 h after birth, indicating a longer time frame for potential benefit from treatment with 2-iminobioton.19,20,21 Therefore, the desired treatment duration in human neonates was set at 48 h, with a target AUC0–48 h of 4800 ng*h/ml.
A phase I dose-escalating safety and tolerability study in healthy male volunteers showed mild adverse events (AEs) such as dizziness and headache at a dose of 12 mg/kg every 4 h (six doses) that resolved quickly after discontinuation. No difference in AEs was observed compared to placebo at the lower 2-iminobiotin doses (0.6–6 mg/kg). No serious adverse events (SAEs) have been reported.22
No studies combining 2-iminobiotin with TH in neonates have been performed to date. The objective of this study was to investigate the pharmacokinetics (PKs) and short-term safety of 2-iminobiotin in asphyxiated neonates treated with TH. Results from this study will be used to determine the dose required in future clinical trials to achieve the target AUC0–48 h associated with neuroprotection in animal models for NE.
Methods
Setting and study design
A single-center, open-label, phase II, prospective study was conducted at the level III Neonatal Intensive Care Unit of the University Medical Center Utrecht, the Netherlands. (Near-)term neonates treated with TH after perinatal asphyxia and with the ability to receive the first dose of 2-iminobiotin within 12 h after birth were eligible for inclusion. Exclusion criteria were major congenital malformations and inability to insert an indwelling catheter for administration of 2-iminobiotin or blood sampling. The study enrolled two groups (groups A and B) of six evaluable patients each.
Dosing regimen
In group A, patients received four intravenous 1-min bolus infusions of 0.16 mg/kg 2-iminobiotin at 6-h intervals. This dose was expected to yield the target AUC0–48 h of 4800 ng*h/mL when administered eight times at 6-h intervals, based on simulations using data from preclinical and clinical studies.18,22 A dose-escalation study in moderate and severely asphyxiated newborn piglets demonstrated efficacy using 2-iminobiotin with doses of 0.1, 0.2, and 1.0 mg/kg every 4 h. Although the highest 2-iminobiotin dose was still significantly neuroprotective compared to placebo, a trend was seen toward less neuroprotection compared to the dose of 0.2 mg/kg, which was selected as the most promising for future clinical trials.18 When combining PK data obtained from both animal models and adult humans, clearance appeared to increase linearly with body weight and a constant mg/kg dose achieved similar exposure across different species. Therefore, a dose of 0.2 mg/kg every 4 h was predicted to be the optimal dose in normothermic neonates.23 In a newborn piglet study investigating 2-iminobiotin during normothermia and hypothermia, clearance during hypothermia was estimated to be 2.2-fold lower compared to normothermic conditions (personal communication H. Tjabbes, Neurophyxia BV). Using simulations, the dosing regimen of 0.2 mg/kg under normothermic conditions was compared to different dosing regimens under hypothermic conditions, aiming for an equal AUC0–24 h. The dosing regimen of 0.16 mg/kg/dose every 6 h under hypothermia was predicted to achieve the desired target AUC0–24 h of approximately 2400 ng*h/mL (Supplementary Table S1). Upregulation of iNOS can be present for up to 48 h after birth.19,20,21 Therefore, the desired dosing period was set to 48 h with an AUC0–24 h of 2400 ng*h/mL for each 24-h period, which translates to an AUC0–48 h for the entire treatment period of 4800 ng*h/mL. However, owing to uncertainties regarding PK and safety in this extremely vulnerable population, 2-iminobiotin administration was limited to four doses in group A, after which an interim analysis was conducted by an independent Data and Safety Monitoring Board (DSMB) assessing both PK and short-term safety (for flowchart, see Fig. 1). In group B, 2-iminobiotin was increased to eight doses at 6-h intervals.
This study was approved by the ethics committee of the University Medical Center Utrecht (16/471) and was registered in the European Clinical Trials Database (www.clinicaltrialsregister.eu: 2014-004265-25) and the Netherlands Trial Register (www.trialregister.nl: NTR5221). Written informed consent was obtained from both parents.
Study drug
2-Iminobiotin was supplied as a 0.75 mg/mL solution for infusion in ready-to-administer vials containing NaCl 0.9% and a citrate buffer as vehicle to ensure solubility at pH 3.8–4.2 (Neurophyxia BV, ‘s-Hertogenbosch, the Netherlands).
PK analysis
From each included neonate, five blood samples of 0.5 mL were drawn at the following scheduled times for PK evaluation: one peak sample 5 min after the first administration, two trough samples (one before the second administration and one before the last administration) and two samples at 1 and 3 h after the last administration. 2-Iminobiotin plasma concentrations were measured using a liquid chromatography tandem mass spectrometry method validated in compliance with the Organisation for Economic Co-operation and Development Good Laboratory Practice guidelines. The lower limit of quantification (LLQ) was 5 ng/ml and the calibration curves were linear from 5 to 5000 ng/ml. Between-run and within-run coefficients of variation were <20%. Samples were stored at −80 °C until analyses.
A population PK model was developed from 2-iminobiotin using non-linear mixed-effects modeling (NONMEM, version 7.3.; ICON, Ellicott City MD). In the interim analyses, PK data from group A was used to calculate the AUC0–48 h if the current dose were to be extended to eight administrations at 6-h intervals. Subsequently, the dose required to achieve the target AUC0–48 h with a dosing regimen of eight administrations at 6-h intervals was determined. Based on the PK data from the interim analyses, the DSMB advised on the dose for group B.
Short-term safety analysis
Safety was assessed by close monitoring of vital signs such as heart rate, arterial blood pressure, transcutaneous oxygen saturation, rectal temperature, continuous neuromonitoring using 2-channel amplitude-integrated electroencephalography (aEEG) and near-infrared spectroscopy (NIRS), and recording of AEs and SAEs. Safety assessment included trend analysis of vital functions and an intrapatient comparison of vital functions in the 15 min before compared to the 30 min after each administration of 2-iminobiotin. In group A (n = 6), 4 administration per patient led to a total of 24 evaluations of each vital sign. In group B (n = 6), 8 administrations yielded a total of 48 evaluations. With this data, a clinically relevant change of >10% could be detected with a power of 80% for each variable. For each test, a p value <0.05 was considered statistically significant. A paired t test was performed to investigate any difference between the pre- and post-administration time frames of 2-iminobiotin. When the parameter was not normally distributed (based on Shapiro–Wilk test), Wilcoxon rank test was performed. Statistical analyses was performed using SPSS (version 21.0.0, IBM Corp, Armonk NY). All SAEs and AEs were recorded and discussed by the study team and reported to the ethics committee according to national policy. Based on the short-term safety data from the interim analyses, the DSMB advised on continuation of the study.
Results
Six patients were included in group A and six in group B. All patients concluded all study activities. All patients were treated with TH for 72 h following perinatal asphyxia and ensuing NE according to the national protocol.2 All administrations of 2-iminobiotin and all blood sampling took place during TH. Patient characteristics are presented in Table 1.
Pharmacokinetics
2-Iminobiotin concentrations could be measured in all samples; no concentrations were below the LLQ. A preliminary population PK model was developed based on data obtained from patients in group A. A two-compartment structural PK model was superior to a one-compartment model (objective function value 559.8 vs 602.3, decrease of 42.5) and provided an adequate fit for the data. Estimation method was first-order conditional estimation with interaction option in NONMEM. Interindividual variability (IIV) could be detected on clearance; residual variability was proportional. Only body weight was considered as a potential covariate, which was not found to have a significant effect on clearance (p > 0.05) and was therefore excluded from the model. The estimated clearance was used to compute the model-predicted AUC0–48 h for group A when treatment would be extended to eight administrations every 6 h through integration of the predicted time curve over the 48 h time interval. Consecutively, the dose required to achieve the target AUC0–48 h with a dosing regimen of eight administrations at 6-h intervals was determined. The median AUC0–48 h for group A was 9522 ng*h/mL (range 5176–22615 ng*h/mL), 198% of the target AUC0–48 h of 4800 ng*h/mL. Simulations using the individual estimates based on this preliminary model predicted that eight administrations of 0.08 mg/kg every 6 h would result in a median AUC0–48 h of 4772 ng*h/mL (range 2588–11,307). Therefore, this dosing regimen was applied in group B. The resulting median AUC0–48 h for group B was 4465 ng*h/mL (range 2926–13,816 ng*h/mL), close to the target AUC0–48 h.
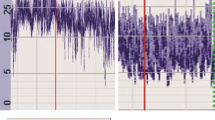
Data from both groups was used to expand the preliminary model into the final population PK model. No structural changes to the preliminary model were required. The population estimate for clearance was 0.380 L/h; PK parameter estimates for the final model are shown in Table 2; Fig. 2 illustrates the poor correlation between clearance and body weight. Exposure metrics were determined through high-density simulation of the individual predictions; individual PK metrics are shown in Table 3. Figure 3 shows that the developed model provides an adequate individual and population fit for the PK data, albeit with considerable interpatient variability. Figure 4 shows the goodness-of-fit plots for the complete dataset and Fig. 5 shows the combined visual predictive check for both treatment groups where the observations have been adequately captured by the model predictions.
Individual PK plots of patient in group A (left) and in group B (right). Gray dashed lines indicate the nominal dosing times; red dots are the observed 2-iminobiotin plasma concentrations; blue solid lines represent the individual model fit; black dashed lines represent the population model fit. PK pharmacokinetics
GoF plots for the final model. 1 = observed vs population predicted 2-iminobiotin plasma concentrations; 2 = observed vs individual predicted 2-iminobiotin plasma concentrations; 3 = conditional weighted residuals vs population predicted 2-iminobiotin plasma concentrations; 4 = conditional weighted residuals vs time after first administration. GoF goodness of fit
VPC plot for all administrations. Purple dots represent the individual observations; dashed lines represent the 5th, 50th, and 95th percentiles of the observations. Solid lines represent the 5th, 50th, and 95th percentiles of the predictions; red shaded area represents the predicted 90% confidence interval around the 50th percentile, blue shaded areas represent the predicted 90% confidence intervals around the 5th and 95th percentiles. All predictions and observations have been normalized for a 0.16 mg/kg dose. T = 0 represents the last administration preceding each observation. VPC visual predictive check
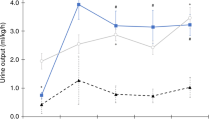
Safety
The trends of heart rate, mean arterial blood pressure, and rectal temperature during and after 2-iminobiotin administration are presented in Fig. 6. No statistically significant or clinically relevant change in any vital sign (heart rate; blood pressure; ventilation rate; arterial oxygen saturation; cerebral oxygenation using NIRS; and mean, minimum, and maximum aEEG background activity) was observed in the 15 min before compared to the 30 min after 2-iminobiotin administration in either group.
Two SAEs were reported, both in group A. One patient (A4) died on day 3 after redirecting of care because of irreversible cerebral injury, and one patient (A5) had an abnormal magnetic resonance imaging on day 5 demonstrating injury to the deep gray matter. Both were considered related to severe perinatal asphyxia and not to the study medication. AEs reported were hyperkalemia (two patients), hypokalemia (three patients), elevated serum creatinine (SCr) and serum urea concentrations (one patient), elevated serum alanine transaminase and aspartate transaminase concentrations (eight patients), and elevated C-reactive protein concentrations (six patients). None were considered to be related to the study medication. As no concerns regarding short-term safety arose in group A, no additional safety measures or protocol amendments were necessary for group B according to DSMB.
Discussion
This is the first study to describe the short-term safety and PK of 2-iminobiotin in (near-)term neonates treated with TH for moderate-to-severe NE. 2-Iminobiotin exposure in terms of AUC0–48 h in group A was much higher than anticipated. The dose for group A was determined with the best available evidence, using a predicted clearance in neonates with data derived from adult human volunteers as well as animal models translational for NE.18,22 However, the animal models used to study 2-iminobiotin are considered translational for NE based on brain development and pattern of hypoxic–ischemic injury but may not accurately reflect maturation of other organs.24,25 Therefore, immaturity of renal function in human neonates may not have been captured adequately in this prediction. The exponent describing the relationship between body weight and 2-iminobiotin clearance was estimated to be 1 based on interspecies scaling.23 Using adult human data alone with a generally more accepted allometric exponent of 0.75 and accounting for immaturity of renal function would have predicted a neonatal clearance much closer to the value estimated in this study.26
Treatment with TH has the potential to influence PK.27 2-Iminobiotin does not undergo hepatic metabolism and is excreted renally in unchanged form. Clearance of predominantly renally excreted drugs were found to be impaired during TH compared to normothermia, most likely due to diminished kidney perfusion.28 Although a potential effect of TH on 2-iminobiotin clearance was anticipated when selecting the dose for group A, underestimation of the effect of TH on 2-iminobiotin clearance may have contributed to the overexposure in group A. Additionally, renal clearance in asphyxiated neonates can be lower compared to non-asphyxiated neonates regardless of TH.29
Neonatal renal function is impaired compared to older children and adults but increases steadily over the first few weeks after birth.30 However, as 2-iminobiotin was administered in this study during the first 2 days after birth only, it is unlikely that maturation of kidney function will significantly impact 2-iminobiotin clearance in this time frame. However, impaired kidney function as a result of perinatal asphyxia could also influence clearance and may contribute to the observed variation in clearance.31 Figure 3 shows accumulation of 2-iminobiotin in patients A5 and B2. Patient B2 suffered from acute kidney injury (AKI) indicated by low urinary output, elevated SCr, and urea concentrations until 7 days after birth. Patient A5 had elevated SCr on day 1 after birth that normalized within 24 h. The same situation was observed in patients A2, A3, and B5 who did not show 2-iminobiotin accumulation. As SCr concentrations during the first few days of life are confounded by maternal transfer, determination of individual renal function based on SCr is subject to a high degree of uncertainty in neonates. Although a 2-iminobiotin dose reduction might be necessary in patients with renal impairment to achieve the desired AUC0–48 h, the lack of a robust tool to accurately predict neonatal renal function on the first day after birth makes this clinically unfeasible. In addition, data from this study suggest that other factors besides AKI may be responsible for 2-iminobiotin accumulation and that elevated SCr concentration on the first day of life will not always predict impaired 2-iminobiotin clearance.
Even though the PK analysis was performed in a small group of neonates with sparse sampling, the population and consequently individual PK parameters could be determined with an adequate precision. An exception is the IIV on clearance, which could not be estimated reliably as the 95% confidence interval of the estimate includes zero (Table 2). However, addition of this random effect was necessary to obtain adequate individual fits. In this small dataset, no relationship between body weight and clearance was detected. Current understanding of PKs would imply that clearance is dependent on body weight and post-conception age.26 All neonates in this study were term or near term, therefore having a similar degree of maturation. The main aim of the population PK analysis was to describe the PKs of 2-iminobiotin in the individual neonates and to predict the dose required to achieve the target AUC0–48 h. As this study consists of only 12 neonates, little inference on the absence or presence of a body weight effect on the PK can be derived on the current data.
Based on the PK analyses of group A, the dose for group B was reduced to 0.08 mg/kg in order to achieve a median AUC0–48 h of approximately 4800 ng*h/mL. Even though this target was achieved, three patients in group B had a lower AUC0–48 h due to considerable interpatient variability in PK parameters. Choosing a higher dose for group B would have resulted in more patients above the predefined target AUC0–48 h. Because of the observation of less neuroprotection at a higher 2-iminobiotin dose in the piglet model, a higher median AUC0–48 h in neonates was deemed undesirable.
NOS promotes various physiological intracellular activities, such as vasodilation, long-term synaptic neurotransmission, and smooth muscle relaxation.32,33,34 eNOS is believed to be instrumental following perinatal asphyxia by maintaining pulmonary blood flow, preventing pulmonary hypertension, and ensuring adequate cerebral oxygenation.8,10 Inhibition of eNOS could therefore potentially be neurodegenerative.35 In our study, no effect on respiratory and cardiovascular parameters was observed after administration of 2-iminobiotin. Both nNOS and iNOS are associated with brain damage and are present in excessive amounts following birth asphyxia.8 Animal data suggest that both nNOS and iNOS are upregulated during TH after hypoxia–ischemia, although TH might attenuate NOS expression.36 In addition, in vitro data indicate that 2-iminobiotin in combination with hypothermia attenuates hypoxia-induced neuronal cell damage.37
The aim of this study was to investigate the PK and short-term safety of 2-iminobiotin when combined with TH. We therefore allowed a 12-h window between birth and first administration of 2-iminobiotin. As nNOS is upregulated immediately after reperfusion, start of 2-iminobiotin should preferentially be as soon as possible after birth.8 From animal studies, it has been shown that iNOS is upregulated until 48 h after hypoxia–ischemia,19,20,21 therefore in part B of the current study 2-iminobiotin was dosed for 48 h. 2-Iminobiotin has not been administered for >24 h in animal models for NE. The uncertainty regarding the optimal treatment duration is a limitation of the present study. However, no safety concerns arose when administration was prolonged to 48 h. Consequently, no evidence exist that treatment for 48 h is detrimental compared to treatment for 24 h while preclinical evidence suggests that it might be beneficial.19,20,21
All events recorded as AEs or SAEs are common complications of the underlying disease and did not occur more often in our group when compared to the overall population of neonates treated with TH for NE in our hospital.38 None of the complications were deemed related to 2-iminobiotin by the study team and DSMB. Although this study was not designed for efficacy, it is noteworthy that the incidence of SAEs (death and deep gray matter injury, both 1 out of 12 (8.3%)) is lower compared to the historical data in this population (around 30% mortality and 15% neurodevelopmental disorders).1,2,38
Since its introduction in 2008, TH has significantly improved the outcome of children with NE and has become the standard of care in western countries.1,2,3 However, additional neuroprotective strategies to augment TH have not been established in the past decade. Several promising pharmacological interventions such as melatonin, erythropoietin, and darbepoetin have recently made the transition from preclinical to explorative clinical studies32,33,34 but their effect has yet to be confirmed in randomized, phase III clinical trials (NCT02621944, NCT03079167, NCT03071861). Phase II studies investigating topiramate and allopurinol in addition to TH are currently underway (NCT01765218, NCT03162653). In addition, xenon ventilation in neonates is safe and feasible despite the need of closed-circuit ventilation to minimize the loss of this expensive noble gas but a recent efficacy study showed disappointing results.39 Argon, a much more abundant and less expensive noble gas, has also shown neuroprotective properties in animal models but has not (yet) progressed to trials in humans.40
Over the past two decades, studies have focused on safety and efficacy of 2-iminobiotin in cell cultures, animal models for NE, and humans. In the present study, 2-iminobiotin exposure known to be effective in animals has been achieved in human neonates with NE during treatment with TH, although the PK parameters are derived from a small dataset. An open-label efficacy trial with 2-iminobiotin in combination with TH is at risk for introducing bias as the standard of care continues to evolve and patients might not be adequately matched to historical controls. Therefore, it is our opinion that a placebo-controlled (phase II) trial in addition to TH with a 2-iminobiotin dose of 0.08 mg/kg/dose every 6 h is the logical next step to examine the neuroprotective potential of 2-iminobiotin. As the optimal duration of treatment has not been fully elucidated, a dose-escalating design regarding treatment duration should be incorporated. This trial should also include collection of PK data to further increase the knowledge of 2-iminobiotin PK in this vulnerable population. Allometric scaling and incorporation of maturation should be considered in future PK models.
Conclusion
Administration of 2-iminobiotin in (near-)term neonates treated with TH for NE is safe regarding short-term clinical parameters and occurrence of (S)AEs. Estimated clearance of 2-iminobiotin in this population is 0.380 L/h, and a dose of 0.08 mg/kg every 6 h is necessary to reach the desired median AUC0–48 h of approximately 4800 ng*h/mL. Optimal duration of therapy for clinical efficacy in combination with TH needs to be determined in future clinical trials.
References
Jacobs, S. E. et al. Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst. Rev. CD003311 (2013).
Groenendaal, F. et al. Introduction of hypothermia for neonates with perinatal asphyxia in the Netherlands and flanders and the dutch-flemish working group on neonatal neurology. Neonatology 104, 15–21 (2013).
Azzopardi, D. V. et al. Moderate hypothermia to treat perinatal asphyxial encephalopathy. N. Engl. J. Med 361, 1349–1358 (2009).
Van Bel, F. & Groenendaal, F. Drugs for neuroprotection after birth asphyxia: Pharmacologic adjuncts to hypothermia. Semin Perinatol. 40, 1–8 (2016).
Hagberg, H., David Edwards, A. & Groenendaal, F. Perinatal brain damage: the term infant. Neurobiol. Dis. 92, 102–112 (2016).
Groenendaal, F. et al. Nitrotyrosine in human neonatal spinal cord after perinatal asphyxia. Neonatology 93, 1–6 (2007).
Groenendaal, F., Lammers, H., Smit, D. & Nikkels, P. G. J. Nitrotyrosine in brain tissue of neonates after perinatal asphyxia. Arch. Dis. Child. Fetal Neonatal Ed. 91, F429–F433 (2006).
Liu, H. et al. Nitric oxide synthase in hypoxic or ischemic brain injury. Rev. Neurosci. 26, 105–117 (2015).
Drury, P. P. et al. NNOS inhibition during profound asphyxia reduces seizure burden and improves survival of striatal phenotypic neurons in preterm fetal sheep. Neuropharmacology 83, 62–70 (2014).
Fan, X., Kavelaars, A., Heijnen, C. J., Groenendaal, F. & van Bel, F. Pharmacological neuroprotection after perinatal hypoxic-ischemic brain injury. Curr. Neuropharmacol. 8, 324–334 (2010).
Peeters-Scholte, C. et al. Neuroprotection by selective nitric oxide synthase inhibition at 24 h after perinatal hypoxia-ischemia. Stroke 33, 2304–2310 (2002).
Favié, L. M. A. et al. Nitric oxide synthase inhibition as a neuroprotective strategy following hypoxic-ischemic encephalopathy: evidence from animal studies. Front. Neurol. 9, 258 (2018).
Sup, S. J., Green, B. G. & Grant, S. K. 2-Iminobiotin is an inhibitor of nitric oxide synthases. Biochem. Biophys. Res. Commun. 204, 962–968 (1994).
Nijboer, C. H., Kavelaars, A., Van Bel, F., Heijnen, C. J. & Groenendaal, F. Gender-dependent pathways of hypoxia-ischemia-induced cell death and neuroprotection in the immature P3 rat. Dev. Neurosci. 29, 385–392 (2007).
Peeters-Scholte, C., Van Den Tweel, E., Groenendaal, F. & Van Bel, F. Redox state of near infrared spectroscopy-measured cytochrome aa 3 correlates with delayed cerebral energy failure following perinatal hypoxia-ischaemia in the newborn pig. Exp. Brain Res. 156, 20–26 (2004).
Van Den Tweel, E. R. W., Peeters-Scholte, C. M. P. C. D., Van Bel, F., Heijnen, C. J. & Groenendaal, F. Inhibition of nNOS and iNOS following hypoxia-ischaemia improves long-term outcome but does not influence the inflammatory response in the neonatal rat brain. Dev. Neurosci. 24, 389–395 (2002).
Van den Tweel, E. R. W. et al. Long-term neuroprotection with 2-iminobiotin, an inhibitor of neuronal and inducible nitric oxide synthase, after cerebral hypoxia-ischemia in neonatal rats. J. Cereb. Blood Flow Metab. 25, 67–74 (2005).
Bjorkman, S. T. et al. Short-term dose-response characteristics of 2-iminobiotin immediately postinsult in the neonatal piglet after hypoxia-ischemia. Stroke 44, 809–811 (2013).
Ikeno, S. et al. Immature brain injury via peroxynitrite production induced by inducible nitric oxide synthase after hypoxia-ischemia in rats. J. Obstet. Gynaecol. Res. 26, 227–234 (2000).
Nogawa, S., Zhang, F., Ross, M. E. & Iadecola, C. Cyclo-oxygenase-2 gene expression in neurons contributes to ischemic brain damage. J. Neurosci. 17, 2746–2755 (1997).
Fernández, A. P. et al. Postnatal changes in the nitric oxide system of the rat cerebral cortex after hypoxia during delivery. Dev. Brain Res. 142, 177–192 (2003).
Neurophyxia B. V. Phase 1 clinical study: first-in-man 2-IB dose escalation study. https://www.neurophyxia.com/files/results-phase1-clinical-trial.pdf (2009) [cited 11 Mar 2019]
Neurophyxia B. V. Determination of target dose for Phase II study of 2-Iminobiotin (2-IB) in neonates with perinatal asphyxia https://www.neurophyxia.com/files/2012-01-18-Determination-of-target-dose-for-Phase-II.pdf (2012) [cited 11 Mar 2019]
Clancy, B., Finlay, B. L., Darlington, R. B. & Anand, K. J. S. Extrapolating brain development from experimental species to humans. Neurotoxicology 28, 931–937 (2007).
Pressler, R. & Auvin, S. Comparison of brain maturation among species: an example in translational research suggesting the possible use of bumetanide in newborn. Front. Neurol. 4, 36 (2013).
Holford, N., Heo, Y.-A. & Anderson, B. A pharmacokinetic standard for babies and adults. J. Pharm. Sci. 102, 2941–2952 (2013).
Van den Broek, M. P. H., Groenendaal, F., Egberts, A. C. G. & Rademaker, C. M. A. Effects of hypothermia on pharmacokinetics and pharmacodynamics. Clin. Pharmacokinet. 49, 277–294 (2010).
Bijleveld, Y. et al. Population pharmacokinetics of amoxicillin in term neonates undergoing moderate hypothermia. Clin. Pharm. Ther. 103, 458–467 (2018).
Liu, X., Borooah, M., Stone, J., Chakkarapani, E. & Thoresen, M. Serum gentamicin concentrations in encephalopathic infants are not affected by therapeutic hypothermia. Pediatrics 124, 310–315 (2009).
Kearns, G. L. et al. Developmental pharmacology — drug disposition, action, and therapy in infants and children. N. Engl. J. Med. 349, 1157–1167 (2003).
Karlo, J., Bhat, B. V., Koner, B. C. & Adhisivam, B. Evaluation of renal function in term babies with perinatal asphyxia. Indian J. Pediatr. 81, 243–247 (2014).
Aly, H. et al. Melatonin use for neuroprotection in perinatal asphyxia: a randomized controlled pilot study. J. Perinatol. 35, 186–191 (2015).
Baserga, M. C. et al. Darbepoetin administration to neonates undergoing cooling for encephalopathy: a safety and pharmacokinetic trial. Pediatr. Res. 78, 315–322 (2015).
Wu, Y. W. et al. High-dose erythropoietin and hypothermia for hypoxic-ischemic encephalopathy: a phase II trial. Pediatrics 137, e20160191 (2016).
Huang, Z. et al. Enlarged infarcts in endothelial nitric oxide synthase knockout mice are attenuated by nitro-L-arginine. J. Cereb. Blood Flow Metab. 16, 981–987 (1996).
Karabiyikoglu, M., Han, H. S., Yenari, M. A. & Steinberg, G. K. Attenuation of nitric oxide synthase isoform expression by mild hypothermia after focal cerebral ischemia: variations depending on timing of cooling. J. Neurosurg. 98, 1271–1276 (2003).
Zitta, K. et al. 2-iminobiotin superimposed on hypothermia protects human neuronal cells from hypoxia-induced cell damage: an in vitro study. Front. Pharm. 8, 1–11 (2018).
Diederen, C. M. J., van Bel, F. & Groenendaal, F. Complications during therapeutic hypothermia after perinatal asphyxia: a comparison with trial data. Ther. Hypothermia Temp. Manag. https://doi.org/10.1089/ther.2017.0046 (2018).
Azzopardi, D. et al. Moderate hypothermia within 6 h of birth plus inhaled xenon versus moderate hypothermia alone after birth asphyxia (TOBY-Xe): a proof-of-concept, open-label, randomised controlled trial. Lancet Neurol. 15, 145–153 (2016).
Alderliesten, T. et al. Neuroprotection by argon ventilation after perinatal asphyxia: a safety study in newborn piglets. PLoS ONE 9, e113575 (2014).
Acknowledgements
The authors thank Alwin Huitema for his critical appraisal of the PK analysis and Petra Lemmers for her assistance in extracting the data for the safety analysis. This study was supported by Neurophyxia BV with an unrestricted grant.
Author information
Authors and Affiliations
Contributions
L.M.A.F.: conception and design, acquisition of data, analysis and interpretation of data, drafting the manuscript; C.M.P.C.D.P.-S.: conception and design, data analysis, and critical revision of the manuscript for important intellectual content; A.B.: analysis and interpretation of data, critical revision of the manuscript for important intellectual content; H.T., T.C.G.E., F.v.B., C.M.A.R.: conception and design, critical revision of the manuscript for important intellectual content; P.V.: analysis and interpretation of data, critical revision of the manuscript for important intellectual content; F.G.: conception and design, acquisition of data, analysis and interpretation of data, critical revision of the manuscript for important intellectual content. L.M.A.F., C.M.P.C.D.P.-S., H.T., C.M.A.R., F.G., T.C.G.E., and F.v.B. were involved in drafting the concept and design of the study and in drafting the final protocol. C.M.P.C.D.P.-S. and H.T. advised on the study protocol and supplied several other documents required for ethics committee approval. L.M.A.F. and F.G. were involved in patient inclusion and study management. P.V. performed the pharmacokinetic analysis and advised on the 2-IB dose used for this study. L.M.A.F., A.B., and F.G. performed the safety analysis. L.M.A.F. drafted the manuscript; the other authors provided critical revision of the intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
C.M.P.C.D.P.-S., F.v.B., and F.G. are the inventors of 2-iminobiotin as a neuroprotective agent in neonates with hypoxic–ischemic encephalopathy. C.M.P.C.D.P.-S. and H.T. are shareholders and consultants of Neurophyxia BV. P.V. is employed at LAP&P Consultants BV. The other authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Favié, L.M.A., Peeters-Scholte, C.M.P.C.D., Bakker, A. et al. Pharmacokinetics and short-term safety of the selective NOS inhibitor 2-iminobiotin in asphyxiated neonates treated with therapeutic hypothermia. Pediatr Res 87, 689–696 (2020). https://doi.org/10.1038/s41390-019-0587-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0587-1
This article is cited by
-
Emerging therapies and management for neonatal encephalopathy—controversies and current approaches
Journal of Perinatology (2021)
-
Translation from animal to clinical studies, choosing the optimal moment
Pediatric Research (2020)
-
When is a potential new neuroprotective treatment ready for translation?
Pediatric Research (2020)
-
A Phase IIa Clinical Trial of 2-Iminobiotin for the Treatment of Birth Asphyxia in DR Congo, a Low-Income Country
Pediatric Drugs (2020)