Abstract
Background
Inflammation is a major cause of preterm birth and often results in a fetal inflammatory response syndrome (FIRS). Preterm infants with FIRS have a higher childhood incidence of neurodevelopmental disability than preterm infants without FIRS. The mechanisms connecting FIRS to neurodevelopmental disability in formerly preterm infants are not fully understood, but the effect on premature gray matter may have an important role.
Methods
Fetal rats were exposed to intra-amniotic (i.a.) LPS 2 days prior to birth to model FIRS. On postnatal day 7, expression of inflammatory mediators was measured in the liver, lung, and brain. Activation of microglia and expression of glutamatergic receptor subunits and transporters were measured in the hippocampus and cortex.
Results
LPS caused persistent systemic inflammatory mediators gene expression. In the brain, there was corresponding activation of microglia in the hippocampus and cortex. Expression of inflammatory mediators persisted in the hippocampus, but not the cortex, and was associated with altered glutamatergic receptor subunits and transporters.
Conclusion
Hippocampal inflammation and dysregulation of glutamate metabolism persisted well into the postnatal period following i.a. LPS. Poor neurodevelopmental outcomes after FIRS in preterm infants may result in part through glutamatergically driven gray matter injury to the neonatal hippocampus.
Similar content being viewed by others
Introduction
Inflammation is a major cause of preterm birth especially for infants born at <28 weeks when histologic chorioamnionitis is present in over 50% of pregnancies1. Fetal inflammatory response syndrome (FIRS) occurs in many of these infants, which is characterized by umbilical cord inflammation (funisitis) and increased levels of circulating pro-inflammatory cytokines2. Infants with FIRS have worse overall outcomes, both during the neonatal period and later development3,4. Importantly, preterm infants with funisitis have a higher incidence of moderate-to-severe neurodevelopmental disability at 2 years of age5. Inflammation rather than actual infection appears to be the important mediator of infant neurologic morbidity: despite the large percentage of preterm infants exposed to chorioamnionitis and FIRS, <2% of very preterm infants have culture-proven early-onset sepsis, much less meningitis6.
Chorioamnionitis is the infection and consequent inflammatory response of the fetal membranes and amniotic fluid. Inflammatory stimuli within the amniotic fluid (bacterial products, toxins, and cytokines) in this condition come in contact with the fetus through multiple routes: the skin and umbilical cord directly and the lungs and gastrointestinal tract by breathing and swallowing of amniotic fluid. FIRS begins at these entry points and its magnitude is measureable in cord blood in humans and in the serum, liver, lung, and brain in preclinical models of chorioamnionitis2,7,8,9.
In the brain, acute or chronic fetal inflammation leads to increased inflammatory cytokines and microglial activation at the time of birth8,10,11,12,13. Several preclinical models have been used to measure inflammation in individual brain regions. In the rhesus macaque, mRNA expression of inflammatory cytokines IL-1β and MCP-1 were similar in the periventricular white matter, cerebellum, and thalamus at both 16 and 48 h after i.a. lipopolysaccharide (LPS)8. In sheep, IL-1β and IL-8 showed similar expression across several brain regions at birth after 2 (acute) and 14 days (chronic) post-inflammatory stimulus, however the pattern of TNFα expression differed by region11.
The persistence beyond birth of FIRS-induced brain inflammation and microglial activation has been less frequently studied. Zhang et al. described inflammation and microglial activation in white matter at 5 days of life in a rabbit model of prenatal LPS14. However, Jantzie et al. did not find increased microglia in white matter at 15 days of age in a rat model of intra-amniotic (i.a.) LPS given 4 days prior to birth15. In the setting of acute prenatal inflammation, it is unclear the extent to which systemic or gray matter inflammation persists through the first week of life when the neonate is no longer exposed to the inflammatory in utero environment. Moreover, it is also unclear whether gray matter regions are affected differently. The postnatal response of each region to inflammation likely determines the scope and specificity of neurodevelopmental abnormalities.
The effects of inflammation on the integrity of developing white matter have been extensively documented16,17. Far less literature has been dedicated to how gray matter is detrimentally affected by inflammation. We hypothesize that injury to developing gray matter resulting from persistent inflammation may have an impact on long-term neurodevelopment equal to that of white matter. To illustrate, former preterm infants (<28 weeks) at school age have significant cognitive, language, hyperactivity, and relationship difficulties at 4 years of age at a much higher rate than term infants (37% vs 11%). However, the combined rate of periventricular leukomalacia (PVL) and intraventricular hemorrhage (IVH), which are mostly associated with white matter injury, is only 16% in the preterm group18. This difference suggests that at least 11% of former preterm infants have neurodevelopmental disease not explained by PVL and IVH, but is more likely due to gray matter injury.
Glutamate is a major neurotransmitter that is affected by inflammation19. In the developing brain, glutamate excitotoxicity is commonly implicated as a mechanism of injury caused by hypoxic ischemia and its resulting inflammatory processes20. Following prenatal inflammatory challenge to rodents, glutamate dysregulation occurs in periventricular regions21. In developing gray matter, excitotoxicity and altered postnatal glutamate metabolism are potential mechanisms of injury caused by prenatal inflammation and should be considered as contributors to poor long-term neurodevelopmental outcomes.
In this study, we hypothesized that prenatal inflammation would result in persistent postnatal systemic and brain inflammation in multiple predominantly gray matter regions that would ultimately affect glutamatergic receptor and transporter expression. We also hypothesized that the hippocampus and cerebral cortex could differ in severity of inflammation and glutamate homeostasis due to developmental timing and inherent differences of glutamate metabolism between the two regions22,23.
Methods
Animals
Animals were studied with the approval of the Institutional Animal Care and Use Committee at the University of Minnesota. Timed-pregnant Sprague-Dawley rats were purchased (Envigo, Madison, WI) and housed for 5 days before interventions and 1 week before birth of pups. Rats were housed in a temperature and humidity-controlled animal care facility with 12 h:12 h light:dark cycle and allowed food and water ad libitum.
Model of fetal inflammation
On gestational day 20 (term = 22 days), dams underwent laparotomy to facilitate i.a. injections as previously reported24. Briefly, dams were premedicated with long-acting buprenorphine (1.2 mg/kg) 4 h prior to surgery. Under general anesthesia with isoflurane (3% for induction and 1.5% for maintenance) via face mask, a laparotomy was performed. Each dam was randomly assigned to receive doses of 1 μg of LPS (Escherichia coli O155:B5, Sigma, St. Louis, MO) dissolved in 50 μL normal saline (NS) or an equivalent volume of NS to each amniotic sac. After uterine horns were exposed, every amniotic sac was injected with assigned treatment. Abdominal incision was closed in two layers with nylon sutures, staples, and tissue glue. The incision was treated along its length with bupivacaine (2 mg/kg subcutaneously). The dams woke within 5–10 min, recovered in the cage, and welfare was monitored until delivery. Pups did not deliver prematurely, however we found that the laparotomy 48 h prior to delivery impaired pup survival during spontaneous birth. Therefore delivery was performed operatively on gestational day 22 as reported;24 dams were under general anesthesia with isoflurane. Following delivery, dams were killed using an overdose of sodium pentobarbital (100 mg/kg, i.p.). Each pup was removed from the amniotic sac and resuscitated by clamping the umbilical cord, drying with gauze, and placing on a warming pad. Mouths of pups were gently opened repeatedly to stimulate breathing until skin color became pink. Once pink, pups were placed in the nest of foster dam. Weights were obtained at postnatal days (P) 0 (birth) and 5.
Tissue preparation
Tissue was collected from equal numbers of male and female pups at P7 after overdose of sodium pentobarbital (100 mg/kg, i.p.). For pups used for qPCR and protein analysis, the brain was removed and the cortex and hippocampus were quickly dissected on ice, flash-frozen in liquid nitrogen, and stored at −80 °C until analysis. Rats used for immunohistochemistry underwent transcardial perfusion-fixation before removal of brain as previously described25.
Quantitative RT-PCR
qPCR experiments were performed as previously described (n = 6–8)25. Total RNA was isolated with an RNA extraction kit (Thermo Fischer Scientific, Waltham, MA) and cDNA was obtained using 500 ng of RNA in a high capacity RNA to cDNA kit (Applied Biosystems, Foster City, CA). The qPCR experiments were performed using 4 μL of diluted cDNA and 0.5 μL 20X Taqman primer/probe (Applied Biosystems, Supplementary Table 1). Each sample was assayed in duplicate and normalized against ribosomal protein S18.
Immunohistochemistry
CD11b immunohistochemistry was performed to identify microglia as previously described (n = 6)25. Sections were incubated with mouse monoclonal anti-rat CD11b (1:1000; Abcam) followed by anti-mouse biotinylated secondary antibody and avidin-horseradish peroxidase conjugate solution (Vector Laboratories, Burlingame, CA). The protein/antibody complex was visualized using DAB (Vector Laboratories). Images were obtained at 20×. Activation of microglia was measured by areal coverage percentage in the cortex and hippocampus as has been reported26,27. At equivalent sites for each animal, four cortical and two CA1 hippocampal images were obtained bilaterally from a single section for each brain region. Using set intensity thresholds, the area of CD11b positive cells was calculated by subtracting non-stained pixels from total pixel area (Photoshop, Adobe, San Jose, CA). The scorer was blinded to group assignment. The mean was calculated for each animal in each brain region and then each treatment group mean was established. Areal coverage ratio was measured by dividing CD11b positive area by total area of the section.
Western analysis
Protein levels in the hippocampus were determined as previously reported (n = 6)25. Individual frozen hippocampi were sonicated in ice-cold homogenizing buffer (10 mM Tris, 0.1% Tween, pH 8.0) containing complete protease inhibitor cocktail tablets (Roche, Indianapolis, IN). Protein concentration was determined by performing a Bradford assay (Bioworld, St. Louis Park, MN) followed by the addition of reducing agent (Thermo Scientific, Waltham, MA) and LDS (Thermo) to prepare the protein for gel separation. 15 µg of protein per sample was separated on NuPage 4–12% Bis-Tris Gels (Thermo) and then transferred to a PVDF membrane (Millipore, Burlington, MA). The membranes were blocked in Rockland (Pottstown, PA) Blocking Buffer for Fluorescent Western Blotting for 1 h at room temperature and incubated overnight at 4 °C with primary antibodies. After incubation with the secondary antibodies for 45 min at room temperature, the membranes were imaged and analyzed with Odyssey infrared scanning (LiCor Bioscience, Lincoln, NE). Target proteins were standardized to β-actin. Primary antibodies were purchased from Abcam (Boston, MA) against: MMP9 (ab38898, 1:1000), p-NR1 (Ser890, ab195002, 1:500), NR1 (ab109182, 1:500), p-NR2A (Tyr1325, ab16646, 1:1000), NR2A (ab133265, 1:1000), p-NR2B (Tyr1472, ab3856, 1:500), NR2B (ab183942, 1:1000). Secondary antibodies: Alexa Fluor 680 conjugated anti-mouse IgG (1:12,500, Jackson Laboratory, Bar Harbor, ME), Alexa Fluor 790 conjugated anti-rabbit IgG (1:12,500, Jackson). Mouse β-actin (1–10,000 R&D Systems, Minneapolis, MN) was used as standard.
Statistical analysis
Data are reported as mean ± SEM. All comparisons were specified a priori. Unpaired t-tests were used to compare control and LPS treated groups (GraphPad Prism v6, La Jolla, CA). Statistical significance was accepted at p < 0.05.
Results
Effect of i.a. LPS on neonatal health
Pup survival and growth were assessed following birth. The percentage of survivors from each prenatal treatment litter was calculated; pups placed with foster dams were considered birth survivors. Prenatal injections of LPS did not alter pup survival from control levels (Fig. 1a, Controls 78.4% vs LPS 78.7%, p = 0.98). Survival past fostering to P5 was also similar between groups (Controls 91.0% vs LPS 86.5%, p = 0.43). Birth weight and growth differed slightly between treatment groups (Fig. 1b). Following i.a. LPS treatment pups had a slight decrease in birth weight compared to controls (Controls 5.9 ± 0.08 vs LPS 5.6 ± 0.05 g, p < 0.05). LPS-treated pups continued to have lower weight at P5 (Controls 13.4 ± 0.20 vs LPS 12.0 ± 0.23 g, p < 0.05)
Effect of i.a. LPS on pup health. a The percentage of pups from each litter surviving at birth and 5 days following fostering is depicted (n = 14 control litters, 13 LPS litters). There were no significant differences between the control group (black bars) or LPS group (white bars) at either time point. b Weights of pups following i.a. LPS were slightly decreased on postnatal (P) day 0 (birth) and P5 compared to control pups (*p < 0.05). Data are presented as mean ± SEM
Effect of i.a. LPS on persistent systemic inflammation
To determine whether neonatal systemic inflammation persists following i.a. LPS injection, we measured mRNA expression of inflammatory markers in the liver and lung at P7 (Fig. 2). In the liver, expression of cytokines TNFα (1.5-fold), IL-1β (1.7-fold), and IL-6 (2.1-fold) was increased compared to controls. Expression of matrix metalloproteinase 9 (MMP9), an endopeptidase involved in extracellular matrix breakdown and an effector of infection and inflammation28, was also increased (2.6-fold). Similarly, in the lung, expression of TNFα (1.3-fold), IL-1β (1.6-fold), and MMP9 (1.5-fold) was increased. There were no significant differences measured in the expression of monocyte chemoattractant protein-1 (MCP-1) in either liver or lung.
Effect of i.a. LPS on systemic inflammatory mediator expression at P7. In the liver, mRNA expression of TNFα, IL-1β, IL-6, and MMP9 are significantly increased in the LPS group (white bars) compared to the control group (black bars) (*p < 0.05). Lung mRNA expression of TNFα, IL-1β, and MMP9 are significantly increased after LPS. Data are presented as mean ± SEM
Effect of i.a. LPS on persistent microglial activation
To determine how persistent systemic inflammation affected microglia in the hippocampus and cortex, we assessed activation at P7 (Fig. 3). Microglial activation is a change in function that can both protect and harm the brain and occurs following environmental perturbations;29 it can be measured by changes in their density and morphology. To account for the complexity of microglia, we measured cross-sectional areal coverage of CD11b positive cells as a ratio of the total section area. The area of microglia in the hippocampus (1.3-fold) and cortex (2.2-fold) were both increased after i.a. LPS compared to controls. Between regions, there was increased density in the hippocampus compared to cortex in control (2.5-fold) and LPS (1.5-fold) groups.
Effect of i.a. LPS on persistent regional activation of microglia. The areal coverage of CD11 + microglial cells was significantly increased in the hippocampus and cortex after LPS (white bars) compared to the control group (black bars) (*p < 0.05, #p = 0.05). Representative photomicrographs at 20× of hippocampus and cortex of control and LPS groups are shown. Scale bars represent 100 μm. Data are presented as mean ± SEM
Effect of i.a. LPS on persistent gray matter inflammation
Due to the presence of microglial activation at P7, we measured mRNA expression of inflammatory markers in the hippocampus and cortex to determine persistence and as a further measure of activation (Fig. 4a). A regional effect was found in the hippocampus where there was increased expression of IL-1β (1.4-fold) and IL-6 (1.8-fold) after i.a. LPS. Neither of these effects was seen in the cortex. Similarly, gene expression of MMP9 was increased only in the hippocampus (1.5-fold, Fig. 4b). To corroborate mRNA findings, the active form of MMP9 protein was measured in the hippocampus and also found to be increased (2.3-fold). Despite increased systemic expression of inflammatory markers at P7, we found decreased expression of TNFα in both brain regions and MCP-1 in the hippocampus (Fig. 4a).
Effect of i.a. LPS on regional brain inflammatory mediator expression at P7. a Hippocampal mRNA expression of the inflammatory markers IL-1β and IL-6 was increased at P7 after LPS (white bars) compared to the control group (black bars) (*p < 0.05); TNFα and MCP-1 expression were decreased. Cortical mRNA expression of TNFα was also decreased after LPS. b Hippocampal mRNA expression and protein level of MMP9 were increased following i.a. LPS (*p < 0.05, #p = 0.05). Cortical MMP mRNA expression did not change. Data are presented as mean ± SEM
Effect of i.a. LPS on glutamatergic dysregulation
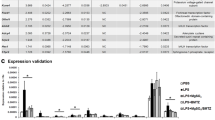
To determine whether the increased expression of inflammatory markers and microglial activation are associated with changes in the potentially excitotoxic glutamatergic system, we measured the mRNA expression for NMDA and AMPA receptor subunits, metabotropic glutamate receptors, and glutamate transporters GLT-1 and GLAST. As with inflammatory markers, a regional effect was noted. In the hippocampus, there was increased expression of AMPA receptor subunit GluR1 (1.2-fold), and NMDA receptor subunits NR1 (1.3-fold) and NR2B (1.1-fold) (Fig. 5a). In contrast, there were no differences of AMPA or NMDA receptors in the cortex. Expression of the glutamate transporter GLT-1 was increased 1.6-fold in the hippocampus (Fig. 5b). There were minimal changes in expression of metabotropic receptors (mGluR), but type 2 (mGluR2) was decreased in the hippocampus (Table 1).
Effect of i.a. LPS on regional glutamatergic receptors and transporters at P7. a AMPA subunit GluR1 and NMDA receptor subunits NR1 and NR2B expression was increased on P7 in the hippocampus after LPS (white bars) compared to controls (black bars). No differences were measured in the cortex. b Expression of the glutamate transporter GLT-1 was increased on postnatal day 7 in the hippocampus after LPS compared to controls. The transporter GLAST was not different. No differences were measured in the cortex. c Phosphorylated fraction and total protein levels of NMDA receptor subunits NR1 (first row), NR2A (second row), and NR2B (last row) were measured in the hippocampus and phosphorylated/total ratio calculated. Phosphorylation was decreased for NR2A and increased for NR2B after i.a. LPS. Data are presented as mean ± SEM. *p < 0.05
NMDA receptor subunits NR2A and NR2B undergo an important functional transition during early development30. Based on our gene expression findings, we wanted to determine if i.a LPS would alter protein levels of these subunits. Therefore, we measured phosphorylated and total protein levels of NR1, NR2A, and NR2B and calculated phosphorylated-to-total protein ratios (Fig. 5c). We found increased phosphorylated NR1 (1.3-fold) in LPS-treated animals and a trend in total NR1 (p = 0.07), but no difference was observed in the ratio of phosphorylated-to-total NR1. Phosphorylated NR2A was decreased (50%) following i.a. LPS treatment, but total NR2A was increased (2-fold). This caused a 70% decrease in the phosphorylated-to-total NR2A ratio. In contrast to NR2A, phosphorylated NR2B was increased (3.7-fold) following i.a. LPS without a change in total NR2B. The ratio of phosphorylated-to-total NR2B was increased 3-fold in the i.a. LPS group.
Discussion
Chorioamnionitis and FIRS cause significant life-long morbidity for infants born prematurely. The goal of this study was to determine whether inflammatory and glutamate metabolism alterations persisted in the gray matter regions, hippocampus and cortex, at 7 days of life and whether there were regional differences in the responses. Our model of prenatal inflammation caused a persistent postnatal increase of inflammatory mediator gene expression systemically in the liver and lungs. The brain was relatively protected compared to the systemic organs, but nevertheless demonstrated signs of persistent gray matter inflammation that varied in spectrum and intensity by brain region. Microglial activation was found in both the hippocampus and cortex, but between the two regions, was greater in the hippocampus. Despite microglial activation across both regions, IL-1β, IL-6, and MMP9 gene expression was elevated only in the hippocampus, possibly as a result of more intense microglial activation in the hippocampus. Prenatal LPS exposure resulted in changes in gene expression of multiple glutamate receptor types and transporters only in the hippocampus where expression of AMPA subunit 1, NMDA subunits NR1 and NR2B, and the transporter GLT-1 were increased. Upregulation of gene expression correlated with altered protein levels of phosphorylated, total, and phosphorylated/total ratio of NMDA receptor subunits.
Systemic inflammation is present in the liver and lungs at birth following acute or chronic prenatal inflammatory challenge7. Our data suggest that FIRS, which is defined by an increased plasma level of the cytokine IL-62, persists through 7 days of life and is accompanied by upregulation of several other inflammatory markers. Microglial activation at 7 days is likely a consequence of persistent systemic inflammation and is consistent with previous studies showing that microglial activation occurs at birth following a prenatal inflammatory stimulus8,13,14.
Persistent microglial activation led us to hypothesize that inflammatory marker expression would also persist in hippocampus and cortex. There is a well-described connection between systemic and brain cytokine concentrations11,12,31. Rodent models of prenatal systemic inflammation have shown increased inflammation measured in the whole brain at birth12. In sheep and non-human primate models, inflammation is similarly increased across individual brain regions at birth8,11. However, after 7 days we found that inflammatory gene expression persisted in the hippocampus, but not the cortex. During this important neonatal timeframe, the hippocampus especially is developing rapidly through critical periods. Therefore, persistent inflammation is likely to span multiple critical periods and impair important events which may cause long-term disability in functions that are hippocampally dependent.
Differences in developmental timing between brain regions might contribute to differences in intensity and persistence of inflammation. Microglia have multiple functions that support normal neurodevelopment (e.g. synaptic pruning, axon guidance, cell genesis) that are determined by local growth factors and other cells such as astrocytes32. The response of microglia to inflammation may vary depending on their phenotype at the time of inflammatory insult. One possible effect of local developmental factors and an explanation for the regional difference in persistence of inflammatory markers is that microglial density was greater in the hippocampus compared to the cortex in both experimental and control groups. Regional developmental differences in microglial density have also been shown between the cortex and amygdala without inflammatory insult33. In adult mice, microglial activation differs among regions following peripheral LPS challenge and correlates with differences in inflammatory markers34. In our experiment, although both regions demonstrated increased activation in treatment groups compared to controls, pre-treatment microglial density may have exacerbated a post-treatment activation sufficient to promote persistent inflammatory gene expression.
Similar to the inflammatory markers, we found that gene expression of AMPA and NMDA glutamate receptor subunits and the glutamate transporter GLT-1 were only affected in the hippocampus at 7 days. This may result from persistent inflammation in the hippocampus and be an adaptive response to increased extracellular glutamate that has been measured acutely following systemic prenatal inflammatory challenge21. It is also possible that upregulation of gene expression may result from a feedback mechanism following changes in receptor activity. NMDA receptors are typically formed from two NR1 subunits and two NR2 or NR3 subunits. NR2A and NR2B are the most important during development30. Previous studies have shown a link between inflammation and altered NR2 receptor metabolism, notably that IL-1β increased NMDA receptor function through phosphorylation of NR2A and NR2B subunits in a culture of rat hippocampal neurons18. We found in our in vivo study that prenatal LPS altered NR2A and NR2B protein levels and function in the hippocampus. Phosphorylation of NR2B was increased, but NR2A was decreased. Important to this finding is that NR2A and NR2B expression and protein levels undergo a programmed change during neonatal development. NR2B is more abundant in synapses following birth to maximize plasticity, but synapses transition to NR2A following the first 2 weeks in rodents30. Altered NR2A and NR2B activity that persists likely affects cell function during critical developmental windows and the timing of programmed transition of NR2B to NR2A. These gene expression and protein results may reflect glutamate homeostasis dysregulation that has significant long-term consequences for the developing gray matter35. Persistent changes suggest a recurrent cycle of neurotoxic injury; activation of microglia may also be a direct response to excitotoxicity that feeds the cycle36. Together this supports our proposed mechanism illustrating a connection between preterm fetal inflammation and long-term neurodevelopmental disability (Fig. 6).
Dysregulation of hippocampal gray matter function may have a particularly devastating long-term effect because of its important role in learning and memory. In preterm infants, the hippocampus is vulnerable to early insults resulting from injuries such as hypoxic ischemia or nutritional deficits37,38. In rodent models, Dada et al. showed a long-term reduction in hippocampal volume and decreased neuronal staining after prenatal treatment with LPS39. Smaller hippocampal volume is associated with poorer memory function in formerly preterm infants40. Because FIRS increases the risk for long-term neurodevelopmental deficits, the connection between fetal inflammation, persistent hippocampal inflammation, and altered glutamate metabolism should be considered as a potential mechanism.
FIRS may have an indirect effect on gray matter injury by causing lower birth weight and poorer growth. Although the difference in birth weight in our study was small (0.3 g), the gap increased between groups at P5. Poorer nutrition during a metabolically active period in the hippocampus could explain the differences we measured in NMDA subunit proteins. However, the persistence of inflammatory gene expression is unlikely to be attributed to growth.
In summary, we found that i.a. LPS as a model of FIRS in rats caused persistent systemic and hippocampal inflammation. This resulted in activation of microglia in the hippocampus and cortex, but dysregulation of glutamate metabolism only in the hippocampus. Inflammation and glutamatergic changes persisting through a critical developmental period of the hippocampus may be important mechanisms triggered by FIRS that result in worse neurodevelopmental outcomes for former preterm infants.
References
Lahra, M. M. & Jeffery, H. E. A fetal response to chorioamnionitis is associated with early survival after preterm birth. Am. J. Obstet. Gynecol. 190, 147–151 (2004).
Gomez, R. et al. The fetal inflammatory response syndrome. Am. J. Obstet. Gynecol. 179, 194–202 (1998).
Hofer, N., Kothari, R., Morris, N., Müller, W. & Resch, B. The fetal inflammatory response syndrome is a risk factor for morbidity in preterm neonates. Am. J. Obstet. Gynecol. 209, 542.e1–542.e11 (2013).
Salas, A. A. et al. Histological characteristics of the fetal inflammatory response associated with neurodevelopmental impairment and death in extremely preterm infants. J. Pediatr. 163, 652–657 (2013).
Rovira, N. et al. Impact of histological chorioamnionitis, funisitis and clinical chorioamnionitis on neurodevelopmental outcome of preterm infants. Early Hum. Dev. 87, 253–257 (2011).
Stoll, B. J. et al. Very low birth weight preterm infants with early onset neonatal sepsis: the predominance of gram-negative infections continues in the National Institute of Child Health and Human Development Neonatal Research Network, 2002-2003. Pediatr. Infect. Dis. J. 24, 635–639 (2005).
Gisslen, T. et al. Repeated exposure to intra-amniotic LPS partially protects against adverse effects of intravenous LPS in preterm lambs. Innate. Immun. 20, 214–224 (2014).
Schmidt, A. F. et al. Intra-amniotic LPS causes acute neuroinflammation in preterm rhesus macaques. J. Neuroinflamm. 13, 238 (2016).
Maxwell, J. R., Denson, J. L., Joste, N. E., Robinson, S. & Jantzie, L. L. Combined in utero hypoxia-ischemia and lipopolysaccharide administration in rats induces chorioamnionitis and a fetal inflammatory response syndrome. Placenta 36, 1378–1384 (2015).
Kuypers, E. et al. Effects of intra-amniotic lipopolysaccharide and maternal betamethasone on brain inflammation in fetal sheep. PLoS One 8, e81644 (2013).
Strackx, E. et al. Lipopolysaccharide-induced chorioamnionitis causes acute inflammatory changes in the ovine central nervous system. CNS Neurol. Disord. Drug. Targets 14, 77–84 (2015).
Beloosesky, R., Weiner, Z., Ginsberg, Y. & Ross, M. G. Maternal N-acetyl-cysteine (NAC) protects the rat fetal brain from inflammatory cytokine responses to lipopolysaccharide (LPS). J. Matern. Fetal Neonatal Med. 25, 1324–1328 (2012).
Kannan, S. et al. Microglial activation in perinatal rabbit brain induced by intrauterine inflammation: detection with 11C-(R)-PK11195 and small-animal PET. J. Nucl. Med. 48, 946–954 (2007).
Zhang, Z. et al. Trajectory of inflammatory and microglial activation markers in the postnatal rabbit brain following intrauterine endotoxin exposure. Neurobiol. Dis. 111, 153–162 (2018).
Jantzie, L. L. et al. Complex pattern of interaction between in utero hypoxia-ischemia and intra-amniotic inflammation disrupts brain development and motor function. J. Neuroinflamm. 11, 131 (2014).
Favrais, G. et al. Systemic inflammation disrupts the developmental program of white matter. Ann. Neurol. 70, 550–565 (2011).
Mallard, C., Welin, A. K., Peebles, D., Hagberg, H. & Kjellmer, I. White matter injury following systemic endotoxemia or asphyxia in the fetal sheep. Neurochem. Res. 28, 215–223 (2003).
Woodward, L. J. et al. Very preterm children show impairments across multiple neurodevelopmental domains by age 4 years. Arch. Dis. Child. Fetal Neonatal Ed. 94, F339–F344 (2009).
Viviani, B. et al. Interleukin-1beta enhances NMDA receptor-mediated intracellular calcium increase through activation of the Src family of kinases. J. Neurosci. 23, 8692–8700 (2003).
Vexler, Z. S. & Ferriero, D. M. Molecular and biochemical mechanisms of perinatal brain injury. Semin. Neonatol. 6, 99–108 (2001).
Zhang, Z. et al. Maternal inflammation leads to impaired glutamate homeostasis and up-regulation of glutamate carboxypeptidase II in activated microglia in the fetal/newborn rabbit brain. Neurobiol. Dis. 94, 116–128 (2016).
Lourenço, C. F. et al. The pattern of glutamate-induced nitric oxide dynamics in vivo and its correlation with nNOS expression in rat hippocampus, cerebral cortex and striatum. Brain Res. 1554, 1–11 (2014).
Fan X., et al. In situ real-time monitoring of glutamate and electrophysiology from cortex to hippocampus in mice based on a microelectrode array. Sensors 17, pii: E61 (2016).
Tang, J. R. et al. Moderate postnatal hyperoxia accelerates lung growth and attenuates pulmonary hypertension in infant rats after exposure to intra-amniotic endotoxin. Am. J. Physiol. Lung Cell. Mol. Physiol. 299, L735–L748 (2010).
Gisslen, T., Ennis, K., Bhandari, V. & Rao, R. Recurrent hypoinsulinemic hyperglycemia in neonatal rats increases PARP-1 and NF-κB expression and leads to microglial activation in the cerebral cortex. Pediatr. Res. 78, 513–519 (2015).
Barton, S. K. et al. Differential short-term regional effects of early high dose erythropoietin on white matter in preterm lambs after mechanical ventilation. J. Physiol. 594, 1437–1449 (2016).
Kim, I. et al. A postnatal peak in microglial development in the mouse hippocampus is correlated with heightened sensitivity to seizure triggers. Brain Behav. 5, e00403 (2015).
Teng, L. et al. Matrix metalloproteinase-9 as new biomarkers of severity in multiple organ dysfunction syndrome caused by trauma and infection. Mol. Cell. Biochem. 360, 271–277 (2012).
Boche, D., Perry, V. H. & Nicoll, J. A. Review: activation patterns of microglia and their identification in the human brain. Neuropathol. Appl. Neurobiol. 39, 3–18 (2013).
Dumas, T. C. Developmental regulation of cognitive abilities: modified composition of a molecular switch turns on associative learning. Prog. Neurobiol. 76, 189–211 (2005).
Mallard, C. Innate immune regulation by toll-like receptors in the brain. ISRN Neurol. 2012, 701950 (2012).
Lenz, K. M. & Nelson, L. H. Microglia and beyond: innate immune cells as regulators of brain development and behavioral function. Front. Immunol. 9, 698 (2018).
Nelson, L. H. & Lenz, K. M. Microglia depletion in early life programs persistent changes in social, mood-related, and locomotor behavior in male and female rats. Behav. Brain Res. 64, 11–22 (2016).
Yang, T. T. et al. Differential distribution and activation of microglia in the brain of male C57BL/6J mice. Brain Struct. Funct. 218, 1051–1060 (2013).
Kaindl, A. M. et al. Activation of microglial N-methyl-D-aspartate receptors triggers inflammation and neuronal cell death in the developing and mature brain. Ann. Neurol. 72, 536–549 (2012).
Block, M. L. & Hong, J. S. Microglia and inflammation-mediated neurodegeneration: multiple triggers with a common mechanism. Prog. Neurobiol. 76, 77–98 (2005).
Nakamura, Y., Nakashima, T., Fukuda, S., Nakashima, H. & Hashimoto, T. Hypoxic-ischemic brain lesions found in asphyxiating neonates. Acta Pathol. Jpn. 36, 551–563 (1986 Apr).
Lodygensky, G. A. et al. Intrauterine growth restriction affects the preterm infant’s hippocampus. Pediatr. Res. 63, 438–443 (2008).
Dada, T. et al. Mouse model of intrauterine inflammation: sex-specific differences in long-term neurologic and immune sequelae. Brain Behav. Immun. 38, 142–150 (2014).
Beauchamp, M. H. et al. Preterm infant hippocampal volumes correlate with later working memory deficits. Brain 131, 2986–2994 (2008).
Acknowledgements
Funding for this project was provided by a grant from The National Institutes of Health (CHRCDA K12 HD068322; Bethesda, MD) and the Viking Children’s Fund, Department of Pediatrics, University of Minnesota, Minneapolis, MN.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Gisslen, T., Singh, G. & Georgieff, M.K. Fetal inflammation is associated with persistent systemic and hippocampal inflammation and dysregulation of hippocampal glutamatergic homeostasis. Pediatr Res 85, 703–710 (2019). https://doi.org/10.1038/s41390-019-0330-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0330-y
This article is cited by
-
Perinatal compromise affects development, form, and function of the hippocampus part two; preclinical studies
Pediatric Research (2024)
-
Chorioamnionitis and neonatal outcomes
Pediatric Research (2022)
-
N,N-Dimethylformamide Delays LPS-Induced Preterm Birth in a Murine Model by Suppressing the Inflammatory Response
Reproductive Sciences (2022)
-
Fetal inflammation induces acute immune tolerance in the neonatal rat hippocampus
Journal of Neuroinflammation (2021)