Abstract
Background
Bronchopulmonary dysplasia (BPD) is an orphan disease and advances in prevention and treatment are lacking. The clinical efficacy of systemic corticosteroid therapy to reduce the severity of lung disease and BPD is highly variable. Our objective was to assess whether candidate SNPs in corticosteroid metabolism and response genes are associated with short-term phenotypic response to systemic corticosteroids in infants at high risk for BPD.
Methods
Pharmacogenetic analysis of data from a large randomized controlled trial (TOLSURF) in infants treated with dexamethasone or hydrocortisone using multivariate linear regression. The primary outcome was a change in respiratory severity score (RSS, mean airway pressure x FiO2) at day 7 of corticosteroid treatment.
Results
rs7225082 in the intron of CRHR1 is significantly associated with the magnitude of decrease in RSS 7 days after starting treatment with systemic corticosteroid (meta-analysis P = 2.8 × 10−4). Each T allele at rs7225082 is associated with a smaller absolute change in RSS at day 7, i.e., less response to systemic corticosteroids.
Conclusions
Genetic variability is associated with corticosteroid responsiveness with regard to respiratory status in preterm infants. Identification of genetic markers of corticosteroid responsiveness may allow for therapeutic individualization, with the goal of optimizing the risk-to-benefit ratio for an individual child.
Similar content being viewed by others
Introduction
Bronchopulmonary dysplasia (BPD) is the most frequent complication of extreme prematurity. With increasing survival of the most immature infants, rates of BPD are increasing. Among a large cohort of infants less than 1500g at birth, the incidence of BPD increased between 2009 and 2012, up to 55% in infants born at 26 weeks and 40% in infants born at 27 weeks.1 Preventive therapies for BPD are limited, but postnatal treatment with systemic corticosteroids is a common practice grounded in studies that show improved pulmonary outcomes.2,3 Corticosteroid treatment is highly variable among centers,4 in part due to concern regarding historic associations of high-dose dexamethasone with central nervous system injury.5,6,7 In order for corticosteroid use to be optimized, the risk-to-benefit ratio must be improved such that a given infant is more likely to be benefited than harmed. Precision therapeutics is a burgeoning field that utilizes genetic information to individualize therapy, and this approach can be used to investigate target populations for optimal corticosteroid benefit. A long-term goal of pharmacogenetic studies in BPD is to preemptively delineate likely responders and non-responders and treat accordingly, and to delineate the biology of differential drug response.
In the original Trial of Surfactant Treatment (TOLSURF) study, many infants received systemic corticosteroids to decrease the severity of lung disease and facilitate weaning from mechanical ventilation. In both dexamethasone- and hydrocortisone-treated infants, there is a known large range in phenotypic response to corticosteroid treatment. Many factors can contribute to this variability, including the severity of lung disease, variation among centers in management of respiratory support, and individual patient co-morbidities such as infections, etc. Genetic variation may also be an important and understudied contributor to differential corticosteroid response.
Genetic variation contributes to the risk of BPD.8,9 Although yet unstudied in the BPD population, there is a high probability that genetic variability also contributes to variability in drug response. Variant alleles can influence drug metabolism, disposition, and drug target sensitivity, and explain some of the heterogeneity in efficacy and toxicity that is observed within a patient population. A recent study10 links neonatal genetic variation to respiratory phenotype at birth after maternal treatment with antenatal corticosteroids. In asthma, multiple single-nucleotide polymorphisms (SNPs) in corticosteroid metabolism and response genes modify the clinical response to inhaled corticosteroids.11,12,13,14,15,16,17 Though asthma and BPD are separate clinical entities, significant overlap occurs in their pathophysiology (inflammation, pulmonary architecture, remodeling, bronchospasm, and air trapping). Genes which are implicated in prenatal corticosteroid response and asthma corticosteroid response are potentially relevant to clinical corticosteroid response for BPD.
Given this background, our objective was to identify pharmacogenetic variants from pediatric asthma and perinatal corticosteroid treatment literature, and test these genes and variants for an association with clinical response to systemic corticosteroids in infants at high risk for BPD. Our hypothesis states that variants associated with corticosteroid metabolism and response will correlate with short-term improvement in respiratory phenotype among a clinically homogeneous cohort of preterm infants.
Methods
Our investigation was a secondary analysis of existing data collected during a large multicenter, randomized, controlled trial of late surfactant therapy (TOLSURF study).18,19 The parent clinical trial was IRB-approved and parental consent was obtained, including collection and study of biospecimens (tracheal aspirate, urine, and DNA). The Children’s Mercy Hospital IRB deferred review of this secondary study as non-human subjects research (use of de-identified historical data). The source population from the TOLSURF study included preterm infants receiving inhaled nitric oxide, birth weight 701 ± 164 g, and gestational age 25.2 ± 1.2 weeks. There were no differences found in the primary outcome of survival without BPD at 36 weeks between surfactant-treated and placebo groups. Thus, the groups were combined for secondary analyses.
Study cohort
Five hundred eleven infants enrolled in the TOLSURF study were screened for eligibility. One hundred twenty-six infants met the following criteria: received systemic dexamethasone (DEX) or hydrocortisone (HC) at >14 days of life for a minimum of 7 days of treatment and on invasive ventilation at corticosteroids start. These criteria were selected to exclude corticosteroid exposure for blood pressure support and brief courses to treat airway edema for extubation. Of these 126, 39 were excluded due to (1) no DNA collected/isolated or failed early sample quality control during genome-wide SNP genotyping (n = 26), (2) genotype call rates <95% (n = 3), and (3) sibling from a multiple gestation (n = 10, only one sibling was included to account for genetic relatedness). Ten were excluded for no primary outcome data; these infants were extubated to low-flow NC and mean airway pressure (MAP) was not measurable.
Use of systemic corticosteroids was not prescribed by the study protocol, but guidelines for their use were established by trial investigators. Approximately 75% of the source population were treated with postnatal corticosteroids, for various indications, one being BPD. For corticosteroid treatment for BPD, guidelines for use included withholding treatment until at least 2 weeks of age and only for infants with respiratory severity scores (RSS, FIO2 x mean airway pressure) of ≥7. Biologically equivalent doses of either hydrocortisone (15 mg/kg over 9 days) or dexamethasone (0.89 mg/kg over 10 days), based on doses and durations used in prior clinical trials, were recommended as per TOLSURF study guidelines.20 BPD at 36 and 40 weeks was defined in the original study with the following criteria: infants discharged in room air before 36 weeks were designated “No BPD.” Infants requiring ventilatory support and any level of supplemental oxygen, or with an effective FiO2 > 30% by nasal cannula, were diagnosed with BPD (“severe” BPD by the NIH workshop definition21). Infants receiving mechanical ventilation, NCPAP, or >4 L of nasal cannula flow in room air were designated “Yes BPD.” Infants at 36 weeks receiving ≤0.3 effective FiO2 at < 2 L of flow or on nasal flow <4 L with room air were evaluated for their requirement for respiratory support, determined by an oxygen/flow reduction (room air) challenge test.22
Corticosteroid response phenotyping
In order to measure short-term phenotypic response to systemic corticosteroids, the change in RSS was used as a phenotypic marker. In order to evaluate the response to corticosteroids, we went back to the original TOLSURF data and obtained mean airway pressure (MAP) and FiO2 to calculate RSS at pertinent time points. RSS values for the day were averaged for a 24-h period and recorded on day 0 (day before treatment), day 4 of treatment, and day 7 of corticosteroid treatment. The mode of ventilation was not taken into account in the RSS calculation, but MAP is reliably recorded from conventional ventilators, high-frequency ventilators, and BiPAP/SiPAP and CPAP modes. Only one infant in the analysis cohort was weaned to HFNC and his average RSS corresponded to a MAP of 2-cm H2O. The absolute change in RSS at day 7 is the primary outcome because this is a clinically meaningful time point and allows time for genetic effects to be assessed with respect to drug response.
Genotyping and imputation methods
DNA was isolated from cells in tracheal aspirates using an AutoGeneprep 965 instrument (Autogen, Holliston, MA) as per the manufacturer’s recommended protocols. When protein contamination was evident, DNA was re-precipitated using three volumes of 100% ethanol and 3 M ammonium acetate at a 3:1 ratio after incubation at –80 °C overnight. DNA was quantified by Nanodrop (Thermofisher Scientific, Inc., Waltman MA) and quality was assessed using the Agilent 2100 Bioanalyzer (Agilent, Santa Clara, CA). Genotyping was performed on the Affymetrix Axiom LAT1 array (WorldArray 4, >800,000 SNPs). SNPs were filtered based on call rates <95%, and Hardy–Weinberg equilibrium P-values < 10−6 using PLINK.23 Subjects were evaluated for call rates, consistency between genetic and reported sex, autosomal heterozygosity, and cryptic relatedness/genetic identity using IBD/IBS estimates in PLINK.23 In the case of multiples, one individual was selected at random to be included in the study.
Using the complete set of ~800,000 markers, genomic levels of African and European ancestry were evaluated using ADMIXTURE24 assuming three ancestral populations (K = 3). Individuals from the HapMap CEU and YRI were genotyped on the same array and included as reference populations for European and African ancestry, respectively. Windows were offset by a factor of 0.2, the cutoff for linkage was set to 0.1, and a constant recombination rate was set to 10−8 (bp)−1. Genome-wide SNP genotypes were further used to impute candidate variants in the phase 3 1000 Genomes populations using the Michigan Imputation Server (https://imputationserver.sph.umich.edu/index.html). Variants were then filtered for imputation quality scores >0.3.
Candidate SNP identification
Multiple PubMed queries using search terms “steroid, corticosteroid, pharmacogenetics, asthma, response” were performed. Of the papers that discussed pharmacogenetics of corticosteroids, we chose to only include statistically significant SNPs from papers with an objective and measurable phenotype (e.g., FEV1). Manuscripts reporting genetic associations of prenatal corticosteroid response and neonatal respiratory outcomes were included. The references of pertinent review articles were also reviewed for candidate results.
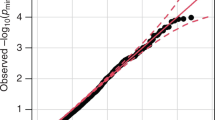
Statistical analysis
Continuous variables are presented as mean and standard deviation. Genetic association testing was performed at individual candidate SNPs, and at a collection of pooled SNPs within 50 kb of candidate genes. Infants of maternal self-reported African-American (AA) and non-Hispanic White (NHW) race/ethnicity were analyzed separately, and then combined in a meta-analysis using Fisher’s method. Genetic associations with respiratory phenotypic response were tested at candidate SNPs within each racial/ethnic group using linear regression in PLINK,23 adjusting for gestational age, sex, birth weight, multiple gestation, baseline RSS, and African genetic ancestry (for infants of maternal AA race). Gene-based association testing was performed using VEGAS2 v.02 by combining P-values across genotyped variants within each candidate gene, and including those within 50 kb of the transcription start/stop site. Demographic differences between ethnic groups were assessed using Fisher’s exact t- tests. Associations between change in RSS at day 7 and long-term diagnosis of BPD at 36 and 40 weeks were tested with univariate binomial logistic regression. Two post hoc exploratory analyses were performed, one including infants with missing data at day 7 of treatment (those weaned to low-flow nasal cannula), and one with a small-for-gestational-age (SGA) variable instead of birthweight, as birthweight and gestational age are highly correlated. P-values less than 0.05 were considered statistically significant for these comparisons.
Results
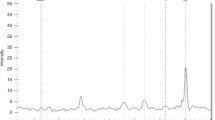
Figure 1 depicts the selection of the final pharmacogenetic cohort. The final analysis cohort consisted of 34 AA and 36 NHW infants (Table 1), and the seven Hispanic White infants were excluded from the initial analysis due to lack of sufficient sample size and power for genetic conclusions in this ethnic subgroup. There was a wide phenotypic range in response to systemic corticosteroids (Fig. 2). Because the hydrocortisone- and dexamethasone-treated groups were similar in clinical characteristics and clinical response variability, they were combined. Of all Table 1 variables tested for an association with the primary outcome, only baseline RSS (day 0 before steroid treatment) was significant, so this was adjusted for in all subsequent analyses. Day 7 change in RSS was not predictive of BPD status at 36 or 40 weeks of gestational age (P-value 0.614 and 0.831, respectively), suggesting that the final diagnosis of BPD is multi-factorial and short-term response to steroids is one of many important contributors.
Distribution of short-term phenotypic steroid response at day 7. Each bar represents an infant treated with systemic dexamethasone (black bars) or hydrocortisone (gray bars). Negative values indicate a decrease in the respiratory severity score (a more positive response to steroids). a Absolute change in RSS at day 7 of treatment. b Percent change in RSS at day 7
The list of candidate SNPs tested for an association with phenotypic response are provided in Supplemental Table S1. We examined 21 SNPs in the proximity of ten genes for associations with the primary outcome. Analyses were run within a racial/ethnic group and then combined in a meta-analysis to avoid confounding due to population structure, differences in the distribution of steroid response, and differences in environmental exposures. Because of the small number of Hispanic infants, we limited our primary analysis to the AA and NHW infants. For the primary outcome of absolute change in RSS at day 7, the entire cohort had an average change of −3.07 with standard deviation of 2.76. Genetic associations between candidate SNPs and absolute change in RSS at day 7 are listed in Table 2.
We identified a significant association between rs7225082 in the intron of CRHR1 and absolute change in RSS at day 7 following Bonferroni correction for 36 tests (meta-analysis P= 2.8 × 10−4). In both AA and NHW infants, the T allele at rs7225082 was associated with a smaller absolute change in RSS at day 7, i.e., lower response to systemic corticosteroids (AA: average decrease in absolute change in RSS = 1.2, P = 0.017; NHW: average decrease in absolute change in RSS = 1.74, P = 0.016; meta P-value = 2.8 × 10–4) (Table 2, Fig. 3a, b). Rs7225082 was also significantly associated with % change at day 7 (meta P-value = 1.8 × 10–4), as displayed in Fig. 4. Compared to the average change in RSS of –3.07 for the entire cohort, the difference in absolute change in RSS between genetic groups of –1.2 and –1.74 is relatively large. The T allele was at a frequency of 36% in AA infants, and 64% in NHW infants, consistent with observations from African and European continental frequencies from the 1000 Genomes Project (Fig. 3c). The results were similar when all infants were pooled, including the ten Hispanic white infants (total N = 87), and adjusted by genomic ancestry (Table 2).
In an exploratory analysis, we included the ten children who were originally excluded because they missed outcome data at day 7 of treatment (Fig. 1). We presume that these children were all weaned to low-flow NC because they had no mean airway pressure recorded in the TOLSURF dataset. In order to analyze these children, we set the RSS at day 7 to 0.5 for all ten infants, and repeated the regression analysis. The direction of effect of the T allele at rs7225082 was the same (P-values: AA 0.04; NHW 0.006). Since the T allele maintained its association with less corticosteroid response in a larger cohort, including ten more extremely good responders, it adds further support that rs7225082 has some influence on variability in corticosteroid response. In the second exploratory analysis, we included a binary SGA variable instead of birthweight. The direction of effect for the T allele at rs7225082 was the same (P-values: AA 0.03; NHW 0.02).
Four infants displayed continued worsening of their lung disease despite systemic corticosteroids, and all were TT homozygotes at rs7225082. When these four outliers whose lung disease continued to worsen despite treatment with corticosteroids (increase in RSS > 1) were excluded, the association with rs7225082 is in the same direction, but does not reach statistical significance. This suggests that the underlying trend is the same direction within infants showing either no change in RSS, or an improvement in RSS over time. The loss of significance could be from a smaller sample size or a “pushing-over” effect of these four infants, but our goal in this study was to assess the complete range of clinical response to corticosteroids, and this includes those infants who continue to get worse despite therapy. None of the other candidate SNP association tests met Bonferroni-corrected significance levels.
A gene-based analysis was performed for two sets of candidate genes, those associated with corticosteroid response in asthma (seven genes) and those associated with perinatal corticosteroid response (three genes) (Supplemental Table S1). Within each racial/ethnic group, none of the candidate genes were significantly associated with phenotypic response to corticosteroids following Bonferroni correction for multiple comparisons (Table 3). However, genetic variation in T showed an association at P = 0.02 in infants of maternal AA race/ethnicity, and variation in SERPINA6 showed an association at P = 0.03 in infants of maternal self-reported NHW race/ethnicity.
Discussion
To our knowledge, this is the first study to assess pharmacogenetic influences on drug response in premature infants at high risk for BPD. We capitalized on published literature to formulate a list of candidate genes and SNPs, and used an existing dataset containing both phenotypic data and genetic data for this proof-of-principle analysis. Our study is an important first step in bringing concepts of precision therapeutics to a very heterogeneous and difficult-to-treat population of preterm infants with respiratory failure. It is of paramount importance to develop predictive biomarkers of drug response in order to spare predicted “non-responders” the unwarranted risk of systemic corticosteroid therapy. This is especially important for a medication such as dexamethasone which has the potential to significantly help a subset of infants with developing BPD. The risk-to-benefit ratio of systemic steroids varies with your risk of developing BPD,25 as both “exposures” can lead to brain injury. And while a calculator that estimates BPD risk26 may be useful in determining which infants to treat, genetic markers of likely responders could strengthen patient selection for steroid treatment.
We identified SNP rs7225082 in CRHR1 as associated with corticosteroid responsiveness and we also present gene and SNP results that do not meet Bonferroni adjustment for significance. We present all of the results because we also hope that this paper is hypothesis-generating, and that these genetic variations may become significant in larger prospective cohorts. Although the effect size of SNP rs7225082 is small, the genetic variation in CRHR1 may be important because of the prevalence of this variant. All ethnic populations have a relatively large proportion of individuals carrying the T allele at rs7225082 (Fig. 3c), potentially contributing to partial or nonresponse to systemic corticosteroid treatment.
The most significant genetic association was between rs7225082 in the intron of CRHR1 and absolute change in RSS at day 7, whereby individuals that carried the T allele had a smaller improvement in RSS scores. This was true for infants of both maternal Black/AA and NHW race, and given our study design, we indeed had the most power to identify genetic associations that are shared among the two racial/ethnic groups. Interestingly, while the variant is common in both African and European populations, the allele associated with greater improvements in RSS scores is at higher frequency in populations with African ancestry. Genotypes were imputed at this variant and passed quality thresholds (Rsq = 0.89). However, another variant in CRHR1 that was directly genotyped and in linkage disequilibrium with the imputed variant at R-squared = 0.70 showed a similar trend (rs242941, P = 5.9 × 10−3). This suggests that our results are not driven by errors in genotype imputation, and strengthens our findings that genetic variation in CRHR1 contributes to drug response.
The difference in absolute change of RSS between the genetic groups must be interpreted within a clinical context. Absolute change in RSS is not a variable commonly used in clinical practice, so ventilator settings which correspond to this genetic difference are provided as an example of the clinical significance. If an infant starts on a MAP of 11 and FiO2 of 0.5, the baseline RSS is 5.5. An infant with the GG genotype at rs7225082 would have on average a decrease in RSS of 3.1 in response to systemic steroids, corresponding to, for example, a decrease in MAP to 8 and FiO2 to 0.3, a clinically significant improvement in respiratory status. For each copy of the T allele, the change in RSS would likely be less. So a GT genotype infant might have a corresponding decrease in MAP to 10 and FiO2 to 0.4, an RSS of 4, and absolute change of 1.5, a less robust response. A TT genotype infant would respond even less. Depending on the size of the infant, this difference in steroid response may mean an ability to wean from high- frequency ventilation to conventional ventilation, or the decrease in overall toxic oxygen exposure to the developing lung. The variability in response to steroids is multi-factorial, and this SNP in CRHR1 explains a portion of this variability.
Corticotrophin-releasing hormone receptor 1 (CRHR1) modulates inflammation through control of ACTH-induced cortisol production. SNPs in this gene may affect baseline endogenous corticosteroid levels and baseline airway inflammation, leading to variation in response to exogenous administration of systemic corticosteroids. The importance of genetic variation in CRHR1 to corticosteroid response has been described in chronic obstructive pulmonary disease (COPD)27 asthma12 and persistent pulmonary hypertension of the newborn.28 Genetic variation in the ligand for CRHR1, corticotropin-releasing hormone (CRH), is associated with neonatal respiratory response to maternal prenatal corticosteroid therapy.10 Fetuses who carry the risk allele at rs7225082 are more likely to require CPAP/ventilator postnatally (poor response to maternal corticosteroids) and correspondingly in our study, preterm infants who carry the risk allele have a poorer response to postnatal corticosteroids. Given the importance of this gene in other patient populations, the biologic plausibility, and the same directionality of effect in two patient populations, we feel confident that genetic variation in CRHR1 is important for corticosteroid response in premature infants.
In the gene-based analysis, we identified two genes associated with absolute change in RSS at day 7 at P < 0.05 that warrant additional investigation—SERPINA6 that was previously implicated in perinatal corticosteroid response, and the T gene that was previously implicated in corticosteroid response in asthma. SERPINA6 encodes an alpha-globulin protein with corticosteroid-binding properties. This is the major transport protein for endogenous glucocorticoids and progestins in the blood of most vertebrates. SERPINA6 transcript number and protein function could regulate systemic bioavailability of endogenous glucocorticoids, as the protein sequesters up to 80% of circulating cortisol in an inactive complex.29 Increased levels of SERPINA6, genetically determined, could reduce unbound and biologically active levels of cortisol and influence tissue response to treatment. It is biologically plausible that alterations in SERPINA6 expression could modulate response to corticosteroid therapy in BPD.
The T gene encodes a mesodermal developmental transcription factor and contributes to regulation in lung development. Alterations in the T gene could alter the temporal pattern of lung development, and thus affect lung maturity and responsiveness to corticosteroids. The T gene is expressed in adult lung,30 but the abundance in neonatal lung is not known. The importance of the T gene in corticosteroid response among patients with asthma was first reported in a large GWAS study, in which the significant two SNPs were found in a transcription factor located 50 kb downstream of the gene.11 The SNP rs6456042 (intronic) is in tight linkage disequilibrium with three other SNPs with known functional implications: rs3099266 (promoter region), rs1134481 (3′ UTR), and rs2305089 (nonsynonymous within the coding region). Thus, although the top SNP in AA infants in our study is not in a coding region, it is likely a marker of carriage of other tightly linked functionally significant genetic changes.
Use of respiratory severity score (RSS) as the phenotypic biomarker provided an objective measure of pulmonary dysfunction at baseline and served as an index of improvement. The RSS allows latitude among individuals treating physician philosophy in choosing the perceived least harmful combination of oxygen and positive airway pressure to achieve the patient’s ventilation goals. The RSS has been validated as a close correlate of oxygenation index.31 In addition, RSS is used extensively in studies of preterm infants beyond the first week of life when paO2 is unavailable.32,33,34,35 RSS at day of life 30 is predictive of clinically important outcomes of preterm infants needing protracted ventilation.36 While the change in RSS may be exaggerated when an infant weans from high-frequency ventilation to conventional ventilation because often this includes a drop in the mean airway pressure, we believe that this improved RSS represents a change in lung pathology which is still valid to measure using this phenotypic marker. Our cohort did not have sufficient size to analyze genetic associations among infants only treated with one modality of invasive ventilation.
Many placebo-controlled studies have documented a short-term pulmonary response to corticosteroids using endpoints such as the respiratory acuity score37 peak inspiratory pressure (PIP) and oxygen need.38,39,40 More recently, McEvoy et al.41 compared short-term effects of lower dose dexamethasone and demonstrated improved lung mechanics at 3 and 5 days. Our study adds to the published literature by assessing contributors to variability in clinical response to steroids, moving the field from a population-based approach toward a more personalized medicine approach.
Our study has some weaknesses, including a small sample size, and no PCR validation of the significant SNP in CRHR1. These are common weaknesses among secondary analysis studies which use data collected for alternative scientific purposes. We believe that the question of steroid pharmacogenetics in BPD is important enough that working within these initial limitations is worthwhile. Additionally, we lack a validation cohort for the pharmacogenetic finding. Because of the challenges in making and reproducing gene–disease (or gene–drug response) conclusions in complex disease based on small sample sizes,42 the research team is collaborating in a multisite consortium and prospectively enrolling preterm infants at risk for BPD who are being treated clinically with systemic corticosteroids in order to recruit a larger patient cohort and further study steroid pharmacogenetics.
Overall, our results implicate genetic variation in CRHR1 in modifying the acute respiratory response to systemic corticosteroids in preterm infants treated for prevention of BPD. Although the identified significant SNP is likely not directly causal, these results add to the body of knowledge that endogenous steroid homeostasis may contribute to variability in response to treatment with exogenous corticosteroids. Additional studies are required to validate these associations and to identify the mechanistic effects of SNPs in CRHR1 on corticosteroid response.
Change history
07 February 2019
In the original version of this article, the Supplementary Information file contained incorrect reference numbers. ‘Supplemental Table S1’ has now been replaced with the corrected version, in which the correct reference numbers are cited. The authors would like to apologise for this error.
References
Stoll, B. J. et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA 314, 1039–1051 (2015).
Doyle, L. W., Cheong, J. L., Ehrenkranz, R. A. & Halliday, H. L. Late (>7 days) systemic postnatal corticosteroids for prevention of bronchopulmonary dysplasia in preterm infants. Cochrane Database Syst. Rev. 10, CD001145 (2017).
Halliday, H. L., Ehrenkranz, R. A. & Doyle, L. W. Moderately early (7-14 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants. Cochrane Database Syst. Rev. CD001144 (2003).
Yoder, B. A., Harrison, M. & Clark, R. H. Time-related changes in steroid use and bronchopulmonary dysplasia in preterm infants. Pediatrics 124, 673–679 (2009).
Shinwell, E. S. et al. Early postnatal dexamethasone treatment and increased incidence of cerebral palsy. Arch. Dis. Child. Fetal Neonatal Ed. 83, F177–F181 (2000).
Zhang, R., Bo, T., Shen, L., Luo, S. & Li, J. Effect of dexamethasone on intelligence and hearing in preterm infants: a meta-analysis. Neural Regen. Res. 9, 637–645 (2014).
Powell, K., Kerkering, K. W., Barker, G. & Rozycki, H. J. Dexamethasone dosing, mechanical ventilation and the risk of cerebral palsy. J. Matern. Fetal Neonatal. Med. 19, 43–48 (2006).
Bhandari, V. et al. Familial and genetic susceptibility to major neonatal morbidities in preterm twins. Pediatrics 117, 1901–1906 (2006).
Lavoie, P. M., Pham, C. & Jang, K. L. Heritability of bronchopulmonary dysplasia, defined according to the consensus statement of the National Institutes of Health. Pediatrics 122, 479–485 (2008).
Borowski, K. S. et al. Neonatal genetic variation in steroid metabolism and key respiratory function genes and perinatal outcomes in single and multiple courses of corticosteroids. Am. J. Perinatol. 32, 1126–1132 (2015).
Tantisira, K. G. et al. Genome-wide association identifies the T gene as a novel asthma pharmacogenetic locus. Am. J. Respir. Crit. Care Med. 185, 1286–1291 (2012).
Tantisira, K. G. et al. Corticosteroid pharmacogenetics: association of sequence variants in CRHR1 with improved lung function in asthmatics treated with inhaled corticosteroids. Hum. Mol. Genet. 13, 1353–1359 (2004).
Stockmann, C. et al. Fluticasone propionate pharmacogenetics: CYP3A4*22 polymorphism and pediatric asthma control. J. Pediatr. 162, 1222–1227.e1–2 (2013).
Park, T. J. et al. Genome-wide association study identifies ALLC polymorphisms correlated with FEV(1) change by corticosteroid. Clin. Chim. Acta 436, 20–26 (2014).
Tantisira, K. G. et al. Genomewide association between GLCCI1 and response to glucocorticoid therapy in asthma. N. Engl. J. Med. 365, 1173–1183 (2011).
Hawkins, G. A. et al. The glucocorticoid receptor heterocomplex gene STIP1 is associated with improved lung function in asthmatic subjects treated with inhaled corticosteroids. J. Allergy Clin. Immunol. 123, 1376–1383 (2009). e1377.
Dijkstra, A. et al. SERPINE1 -675 4G/5G polymorphism is associated with asthma severity and inhaled corticosteroid response. Eur. Respir. J. 38, 1036–1043 (2011).
Ballard, R. A. et al. Randomized trial of late surfactant treatment in ventilated preterm infants receiving inhaled nitric oxide. J. Pediatr. 168, 23–29 (2016). e24.
Keller, R. L. et al. The randomized, controlled trial of late surfactant: effects on respiratory outcomes at 1-year corrected age. J. Pediatr. 183, 19–25 (2017). e12.
Doyle, L. W. et al. Low-dose dexamethasone facilitates extubation among chronically ventilator-dependent infants: a multicenter, international, randomized, controlled trial. Pediatrics 117, 75–83 (2006).
Ehrenkranz, R. A. et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics 116, 1353–1360 (2005).
Walsh, M. C., Wilson-Costello, D., Zadell, A., Newman, N. & Fanaroff, A. Safety, reliability, and validity of a physiologic definition of bronchopulmonary dysplasia. J. Perinatol. 23, 451 (2003).
Purcell, S. et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am. J. Hum. Genet. 81, 559–575 (2007).
Alexander, D. H., Novembre, J. & Lange, K. Fast model-based estimation of ancestry in unrelated individuals. Genome Res. 19, 1655–1664 (2009).
Doyle, L. W., Halliday, H. L., Ehrenkranz, R. A., Davis, P. G. & Sinclair, J. C. An update on the impact of postnatal systemic corticosteroids on mortality and cerebral palsy in preterm infants: effect modification by risk of bronchopulmonary dysplasia. J. Pediatr. 165, 1258–1260 (2014).
Laughon, M. M. et al. Prediction of bronchopulmonary dysplasia by postnatal age in extremely premature infants. Am. J. Respir. Crit. Care Med. 183, 1715–1722 (2011).
Kim, W. J. et al. Association between CRHR1 polymorphism and improved lung function in response to inhaled corticosteroid in patients with COPD. Respirology 14, 260–263 (2009).
Byers, H. M. et al. Variations in CRHR1 are associated with persistent pulmonary hypertension of the newborn. Pediatr. Res. 71, 162–167 (2012).
Moisan, M. P. et al. Role of corticosteroid binding globulin in the fast actions of glucocorticoids on the brain. Steroids 81, 109–115 (2014).
Park, J. C. et al. Epigenetic silencing of human T (brachyury homologue) gene in non-small-cell lung cancer. Biochem. Biophys. Res. Commun. 365, 221–226 (2008).
Iyer, N. P. & Mhanna, M. J. Non-invasively derived respiratory severity score and oxygenation index in ventilated newborn infants. Pediatr. Pulmonol. 48, 364–369 (2013).
Mercier, J. C. et al. Inhaled nitric oxide for prevention of bronchopulmonary dysplasia in premature babies (EUNO): a randomised controlled trial. Lancet 376, 346–354 (2010).
Laughon, M. et al. A pilot randomized, controlled trial of later treatment with a peptide-containing, synthetic surfactant for the prevention of bronchopulmonary dysplasia. Pediatrics 123, 89–96 (2009).
Ballard, R. A. et al. Inhaled nitric oxide in preterm infants undergoing mechanical ventilation. N. Engl. J. Med. 355, 343–353 (2006).
Katz, L. A. & Klein, J. M. Repeat surfactant therapy for postsurfactant slump. J. Perinatol. 26, 414–422 (2006).
Malkar, M. B. et al. Respiratory severity score on day of life 30 is predictive of mortality and the length of mechanical ventilation in premature infants with protracted ventilation. Pediatr. Pulmonol. 50, 363–369 (2015).
Scott, S. M., Backstrom, C. & Bessman, S. Effect of five days of dexamethasone therapy on ventilator dependence and adrenocorticotropic hormone-stimulated cortisol concentrations. J. Perinatol. 17, 24–28 (1997).
Yoder, M. C. Jr, Chua, R. & Tepper, R. Effect of dexamethasone on pulmonary inflammation and pulmonary function of ventilator-dependent infants with bronchopulmonary dysplasia. Am. Rev. Respir. Dis. 143, 1044–1048 (1991).
Durand, M., Sardesai, S. & McEvoy, C. Effects of early dexamethasone therapy on pulmonary mechanics and chronic lung disease in very low birth weight infants: a randomized, controlled trial. Pediatrics 95, 584–590 (1995).
Kari, M. A., Heinonen, K., Ikonen, R. S., Koivisto, M. & Raivio, K. O. Dexamethasone treatment in preterm infants at risk for bronchopulmonary dysplasia. Arch. Dis. Child. 68, 566–569 (1993).
McEvoy, C., Bowling, S., Williamson, K., McGaw, P. & Durand, M. Randomized, double-blinded trial of low-dose dexamethasone: II. Functional residual capacity and pulmonary outcome in very low birth weight infants at risk for bronchopulmonary dysplasia. Pediatr. Pulmonol. 38, 55–63 (2004).
Ioannidis, J. P., Trikalinos, T. A. & Khoury, M. J. Implications of small effect sizes of individual genetic variants on the design and interpretation of genetic association studies of complex diseases. Am. J. Epidemiol. 164, 609–614 (2006).
Acknowledgments
The TOLSURF study was funded by grants from the National Health, Lung, and Blood Institute (NHLBI, 5UO1HL094338M), and an Edward A. Dickson Emeritus Professorship Award (P.L.B.). Ikaria Inc./Mallinckrodt Pharmaceuticals funded the genetic analyses, including support for supplies, technical effort, and statistical analyses.
Author information
Authors and Affiliations
Consortia
Contributions
T.L. conceived and designed the project, helped with acquisition of data, analysis, and interpretation of data, drafting the article and revising it critically for important intellectual content, and final approval of the version to be published. W.T. conceived and designed the project, helped with acquisition of data, analysis, and interpretation of data, drafting the article and revising it critically for important intellectual content, and final approval of the version to be published. M.N. helped to design the project, helped with acquisition of data, analysis, and interpretation of data, and revising the article critically for important intellectual content, and final approval of the version to be published. P.L.B. conceived and designed the project, helped with acquisition of data, analysis, and interpretation of data, drafting the article and revising it critically for important intellectual content, and final approval of the version to be published. D.T. conceived and designed the project, helped with acquisition of data, analysis, and interpretation of data, drafting the article and revising it critically for important intellectual content, and final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A list of members for TOLSURF Study Group is given in Appendix.
Electronic supplementary material
Appendix
Appendix
TOLSURF Study Group
TOLSURF investigators were:
University of California San Francisco – R.A. Ballard M.D., P.L. Ballard M.D. Ph.D., E.E. Rogers M.D., D.M. Black Ph.D., L. Palermo M.S., S. Hamilton Strong, J. Immamura-Ching, M. Orfanos-Villalobos, C. Williams
Alta Bates Summit Medical Center, Berkeley, CA and Children’s Hospital and Research Center Oakland, Oakland, CA – J.D. Merrill M.D., D.J. Durand M.D, J.M. Asselin R.T., D. Horton, L. Pacello, A. Willard
University of Texas Health Science Center- Houston, Houston, TX – E.C. Eichenwald M.D., C. Garcia M.D., G. McDavid, K. Burson, R. Hinojosa, C. Johnson, K. Miller, S. Rogers, S. Wright
Children’s Mercy Hospital, Kansas City, MO – W.E. Truog M.D., C. Gauldin, A. Holmes, P. Johnson, K. Meinert
Women and Children’s Hospital of Buffalo, Buffalo, NY – A.M. Reynolds M.D., J. Lucie, P. Conway, M.l. Sacilowski, M. Leadersdorff, P. Orbank, K. Wynn
Anne and Robert H. Lurie Children’s Hospital/Northwestern University, Chicago IL – R.H. Steinhorn M.D., N.F. Porta M.D., M. deUngria M.D., J. Khan M.D., K. Hamann, M. Schau, B. Hopkins, J. Jenson
Stonybrook University Hospital, Stonybrook, NY – J. Shariff, R. McGovern, J. Adelman, A. Combs, M. Tjersland
University of Washington, Seattle, WA – D.E. Mayock M.D., S. Walker, E. Howland, J. Longoria, H. Meo
University of Florida College of Medicine-Jacksonville, UF Jacksonville and Wolfson Children's Hospital, Jacksonville, FL – M.L. Hudak, M.D., K. Barnette, A. Kellum, M. Burke, C. Hayes, S. Chadwick, D. Howard, C. Kennedy, R. Prince
Wake Forest School of Medicine and Forsyth Medical Center, Winston Salem, NC – B. Stefanescu M.D., J. Helderman M.D., K. Warden, P. Brown, J. Griffin, L. Conley
University of Minnesota Children’s Hospital, Minneapolis, MN – C.M. Bendel M.D., M. Georgieff M.D., B. Davern, M. Mills, S. Ritter
Medical University of South Carolina, Charleston, SC – R.M. Ryan M.D., Frances R. Koch M.D., C. Wagner M.D., D. Fanning, J. Roberson
Children’s Hospitals and Clinics of Minnesota, St Paul, MN – M.C. Mammel M.D., A. Lampland M.D., P. Meyers, A. Brey
Children’s Hospitals and Clinics of Minnesota, Minneapolis, MN – E.M. Bendel-Stenzel M.D., C. Worwa, P. Dixon, G. Ebert, C. Hejl, M. Maxwell, K. McCullough
University of Tennessee Health Science Center, Memphis, TN – R. Dhanireddy M.D., M.T. El Abiad M.D., A. Talati M.D., S. Dempsey, K. Gammage, G. Gower, K. James, P. LeNoue
All Children’s Hospital, St Petersburg, FL – V.J. McKay M.D., S. Bell, D. Bruton, M. Beaulieu, R. Williams
Florida Hospital for Children, Orlando, FL – R. Wadhawan M.D., T.M. O’Shea M.D., R. Barron-Nelson, S. Taylor
Arkansas Children’s Hospital and University of Arkansas Medical Sciences Little Rock, AK – S.E. Courtney M.D., N.C. Sikes, G. Lowe, B. Proffitt.
Rights and permissions
About this article
Cite this article
Lewis, T., Truog, W., Norberg, M. et al. Genetic variation in CRHR1 is associated with short-term respiratory response to corticosteroids in preterm infants at risk for bronchopulmonary dysplasia. Pediatr Res 85, 625–633 (2019). https://doi.org/10.1038/s41390-018-0235-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-018-0235-1