Abstract
An intrinsic feature of the developing brain is high susceptibility to environmental influence—known as plasticity. Research indicates cascading disruption to neurological development following preterm (PT) birth; yet, the interactive effects of PT birth and plasticity remain unclear. It is possible that, with regard to neuropsychological outcomes in the PT population, plasticity is a double-edged sword. On one side, high plasticity of rapidly developing neural tissue makes the PT brain more vulnerable to injury resulting from events, including inflammation, hypoxia, and ischemia. On the other side, plasticity may be a mechanism through which positive experience can normalize neurological development for PT children. Much of the available literature on PT neurological development is clinically weighted and focused on diagnostic utility for predicting long-term outcomes. Although diagnostic utility is valuable, research establishing neuroprotective factors is equally beneficial. This review will: (1) detail specific mechanisms through which plasticity is adaptive or maladaptive depending on the experience; (2) integrate research from neuroimaging, intervention, and clinical science fields in a summary of findings suggesting inherent plasticity of the PT brain as a mechanism to improve child outcomes; and (3) summarize how responsive caregiving experiences situate parents as agents of change in normalizing PT infant brain development.
Similar content being viewed by others
Introduction
Despite medical advances increasing survival of preterm infants (<37 gestational weeks (PT)), they remain at high risk for brain injury and long-term neurodevelopmental problems. An increasing body of research targeting the consequences of PT birth indicates cascading disruption to neurological development,1,2,3,4,5,6 with the degree of deficits correlating with degree of prematurity.7,8,9,10,11,12,13,14 Specifically, converging findings from animal models along with human neuroimaging investigations indicate that early disruption to white and gray matter development resulting from PT birth is largely responsible for inducing disruption of cognitive development15,16,17,18,19 and psychopathologies.20,21,22
Brain plasticity—the way experiences shape neural wiring of the brain—is thought to be one of the primary mechanisms through which humans adapt to environmental change and demonstrate resilience to adverse events.23 With regard to neuropsychological outcomes in the PT population, brain plasticity might be a double-edged sword.6,24 On one side, high plasticity of rapidly developing neural tissue makes the PT brain more vulnerable to injury resulting from various noxious events (e.g., inflammation, hypoxia, ischemia), evidenced by reduced gray matter volumes, disrupted white matter proliferation, and alterations in synaptic pruning in PT infants.21,25,26,27,28 On the other side, plasticity is the mechanism through which enriching experiences, such as optimal nutrition and highly responsive caregiving, might be leveraged as potential neuroprotective factors. There is emerging evidence suggesting that prematurity might be best characterized as a plasticity factor—such that, compared to those born full term, infants born preterm are potentially more vulnerable to negative environmental experiences but also stand to benefit more from positive environmental conditions.29,30,31,32,33 Although an area of active debate, awareness of prematurity as a potential plasticity factor is clinically relevant for expanding treatment from remediation of negative environmental factors to inclusion of preventative treatments that increase positive environmental experiences, such as quality of caregiving, to improve developmental outcomes.
Broadly, this review is centered on plasticity following PT birth. First, we provide an abridged overview of normative brain development in late gestation through early childhood. Then, we summarize current understanding of the extent to which PT birth disrupts normative brain development and provide an overview of common neurodevelopmental outcomes in the preterm population. The final section includes a discussion of prevailing theoretical perspectives on developmental plasticity with a focus on specific mechanisms through which plasticity is adaptive or maladaptive depending on the experience.
Normative brain development
Development of the human brain occurs over a longer period of time compared to other mammals, including non-human primates,34,35 and our relatively protracted period of brain development is largely considered to be adaptive for the human species.36,37 Maturational processes of the human brain begin in the third gestational week, when the neural tube forms, and continue for the next three decades of life. The initial architecture of the brain is primarily established in the first six prenatal months when neuronal production (neurogenesis) is most active.37 At 22 weeks, neuronal production is for the most part complete, but the process of neural migration of cells remains active.38,39 As neurons continue to migrate to different brain regions, neurons branch and form new neuronal connections (i.e., synaptogenesis), and dendrites and dendritic spines are generated to allow communication with other neurons, ultimately contributing to the integration of complex neural networks.39 Synaptic density rapidly increases in the perinatal period as a result of the processes of synaptogenesis, synaptic reorganization, and the formation of dendrites and dendritic spines40,41 (see Fig. 1a, b). The primarily genetically driven overproduction of dendrites, dendritic spines, and axons occurs resulting in an excess of synapses throughout the brain at this stage of life.42,43,44
The overabundance of synaptic connections and resultant hyper-connectivity of the brain in the perinatal period is followed by neural network refinement through pruning. Selection of synaptic connections to retain versus prune is, to some extent, genetically defined through mediated apoptosis (i.e., programmed cell death). Of note, the pruning process also represents one of several mechanisms through which the environment shapes neurological development because synapses that are rarely engaged are targeted for removal.45 Elimination of dendrites and reshaping of axons increases the brain’s efficiency and allows the brain to develop in response to environmental demands. Known as ‘experience-based synaptic pruning’, this process is limited prenatally and most active in childhood and adolescence46 (see Fig. 1a).
Onset and rate of development is not homogenous throughout the brain; rather, the onset and attenuation of primary maturational processes (i.e., neuronal differentiation and synaptogenesis) show regionally specific temporal windows. Integrating findings from several postmortem histological studies in humans, Fig. 1 demonstrates that unlike primary sensory regions (e.g., visual and auditory cortex), which reach a peak in synaptic density during the first months of life (Fig. 1b), prefrontal cortical synaptic production peaks only after 15 months of age, and some prefrontal regions do not reach the maximum number of synapses until later in childhood (Fig. 1a).44,47 The timing of experience-based synaptic pruning also varies regionally throughout the brain, remaining active in complex brain structures such as the prefrontal cortex and hippocampus beyond early childhood.45,48
The final and most protracted process of neurodevelopment is myelination, when a fatty-white sheath (myelin) forms to surround certain axons. Myelination of axons is fundamental to mature brain function and supports neuronal communication by increasing the speed and temporal precision of axonal signaling (i.e., efficiency). Similar to other neurodevelopmental processes, the temporal window of myelination varies widely between brain structures and progresses in a caudal to rostral direction. Myelination of the neurocircuitry regulating basic functions such as sensory processing is limited after early childhood. In contrast, myelination of circuits central to cognition, such as the prefrontal cortex and some limbic structures, continues beyond adolescence.49,50 Often referred to as sensitive periods, the window of time when brain development is most responsive to environment is clearly defined for some behaviors such as language acquisition. Although less well delineated, this is also evident for other cognitive behaviors.45
A relative advantage of the human brain’s protracted and multifaceted periods of plasticity is that it allows the developing brain to dynamically adapt in response to important environmental cues. There is increasing evidence that positive environmental factors, such as warm and highly responsive caregiving, support healthy brain development.51,52,53 Unfortunately, the advantage of plasticity also renders developing neural circuitry more vulnerable to adverse pre- and post-natal events.24 Moreover, the effect of adverse events, including inflammation and chronic environmental stress, is most disruptive to neurocircuitry when neural structures and neural networks are actively developing.54,55,56 Importantly, the neurocircuitry mediating cognitive and emotional processing, specifically prefrontal and limbic networks, has some of the longest developmental periods.57 Due to its protracted developmental time course, fronto-limbic circuitry is heavily influenced by postnatal environment and positive experience, particularly experiences with caregivers, but is also highly sensitive to injury throughout childhood.58 This idea will be further explored in the final section of this review.
Atypical brain development following preterm birth
Causes and types of brain injury
PT birth is associated with atypical brain development, with extent of brain injury correlating with the degree of prematurity.4,59,60 The PT brain is vulnerable to damage via both impaired maturation and specific injury,61 as the brain must continue rapid and active developmental processes such as myelogenesis, angiogenesis, and axonal growth outside of the normal supportive uterine environment. Evidence suggests that preterm birth is associated with suppression of the cerebral neurogenesis that normally continues through the third trimester.60 The vulnerability of the preterm brain to damage is heightened by a lack of long chain fatty acids and fatty acid transporters necessary for normal central nervous system growth,62 lack of availability of necessary growth factors, overly intense inflammatory response from activation of an immature immune system, reduction in the blood–brain barrier as a result of inflammation, and exposure to harmful external factors.63 Exposures to multiple harmful external factors including maternal fetal infection and chorioamnionitis, postnatal sepsis, drug exposure, malnutrition, hemodynamic changes, hypoxia, ischemia, and mechanical ventilation may cause or worsen brain injury.61 In addition, there can be a complex interplay between these factors. Chorioamnionitis—inflammation of the placenta and the placental membranes—complicates 40–70% of PT births,64 and preterm infants are at higher risk for infection, with 25–60% of extremely PT infants (<28 weeks of gestation at birth) having at least one invasive bacterial infection during their hospitalization.65 The resulting inflammation increases the likelihood of damage to the developing brain, including intraventricular hemorrhage (IVH) and the diffuse white matter injury seen so commonly in the preterm population.66,67 Hypoxia induces a profound inflammatory response in the PT brain that is paralleled by mobilization of the peripheral immune system, resulting in direct axonal injury and impaired differentiation into mature myelinating oligodendrocytes, which leads to overall hypomyelination of the premature brain and functional loss.68,69 There is evidence that by term equivalent age (i.e., predicted due date based on a term pregnancy of 40 weeks), PT infants with a history of at least one hypoxic–ischemic event are at high risk for widespread white matter abnormalities and localized damage to the basal ganglia.52 Animal models have demonstrated significant decreases in dendrite arborization and spine density from disrupted maturation following ischemia.70 Though the cause underlying it may be variable, severe inflammation leads to pro-inflammatory cytokines crossing the blood–brain barrier, increasing leakiness, and worsening the neuroinflammatory response by activating microglia and astrocytes.64 Pro-inflammatory cytokines in the fetal brain disrupt normal maturation in vulnerable cell populations, altering white matter development in particular.64
Though prematurity has now been associated with reduced cerebral cortex volume and altered microstructural development of the subcortical gray matter including the thalamus and basal ganglia,61 white matter injury is the hallmark of preterm brain injury clinically. White matter injury is caused by insult to immature oligodendrocytes. The most common nonhemorrhagic neuropathology in the white matter of PT infants is periventricular leukomalacia (PVL).71 PVL is comprised of two principal constituents: (1) focal necroses located periventricularly that result in complete loss of all cellular elements, and (2) disruption of early differentiating preoligodendrocytes along with microgliosis and astrogliosis found more diffusely in the white matter. Acutely, preoligodendrocyte disruption occurs via cell death which is followed by failure of appropriate preoligodendrocyte differentiation, which results in hypomyelination.71 Pathologically, PVL may consist of damage ranging from large focal necroses with cystic changes (cystic PVL) at the most severe end to small focal necroses with focal gliosis but no cystic changes, and at the least severe end of microscopic focal necroses with gliosis.71 In addition, white matter injury may consist of diffuse white matter gliosis without any focal necrosis (e.g., without ‘leukomalacia’). Though cystic PVL predominated in previous decades, the majority of PT brain injury now consists of non-necrotic, non-cystic, diffuse white matter injury.72 Diffuse white injury is identified by the presence of multifocal lesions on magnetic resonance imaging (MRI) and is found in roughly one-third of infants born at 24 to 32 weeks of gestational age.72 Long-term, cystic PVL is associated with the spastic diplegic type of cerebral palsy due to injury of the deeper and more medial white matter tracts controlling function of the lower extremities. If white matter damage is extensive, quadriplegia may result.73 Visual impairment may be an important consequence of PVL if the optic radiations are involved.73 Though the adverse motor outcomes associated with PVL have been well demonstrated, predicting other neurodevelopmental deficits is more difficult.73
Children born preterm are also at risk of brain injury secondary to IVH. IVH is characterized by bleeding into a region of the immature brain. Though the pathogenesis underlying IVH is complex, it is believed to result from immature vasoregulation and variable blood flow hemodynamics in the germinal matrix, coupled with an increase in cerebral arterial pressure following PT birth. IVH is categorized by a graded severity rating ranging from grade I to grade IV. In the most mild grade (grade I), bleeding is confined within the germinal matrix. In more moderate grades, bleeding extends into the ventricles (grade II), which can result in ventricular enlargement (grade III). When most severe, bleeding is evident outside of the ventricle (grade IV), resulting in damage to surrounding brain tissue.74 Severe IVH represents a major cause of both short- and long-term morbidity and mortality in children born PT.75 Roughly 6% of very low birth weight (VLBW; <1500 g at birth) and 15% of extremely PT infants suffer severe IVH which confers a greater than 75% chance of neurodevelopmental impairment and or cerebral palsy.75
Finally, other morbidities associated with PT birth such as necrotizing enterocolitis, bronchopulmonary dysplasia, and retinopathy of prematurity73 are also associated with a several-fold increase in neurodevelopmental impairment in infants born at extremely low birth weights.76,77
Biological adversity
PT infants also experience biological adversity from factors that are shown to disrupt neurological development including malnutrition, prenatal and postnatal infections, and toxins from repeated anesthesia.78,79 Additionally, medically necessary treatments often result in deprivation of caregiver contact, limiting the physical and social–emotional contact that is increasingly suggested as central for healthy brain development.80,81 Biological adversity and deprivation of caregiver interaction might disrupt neurological development by limiting experience-expectant brain plasticity that occurs as a result of environmental input that is expected to be available across early life. For example, in gestation there is an expectation of a nutrient-rich intrauterine environment which insulates the infant from harmful toxins and muffles visual and auditory stimuli. In addition, immediately following birth there is an expectation of nearly continuous tactile contact with a primary caregiver which is shown to regulate both PT and term-born infant physiological response to moment-to-moment environmental fluctuations (e.g., changes in temperature and heart rate).82,83 In the months following birth, PT infants requiring more extended neonatal intensive care unit (NICU) stays often have reduced opportunity for social caregiver–infant interactions characterized by sustained eye gaze, frequent warm-responsive interactions, and responsive touch. Although limited, there is emerging evidence suggesting that social caregiver–infant interactions (and social interactions with caregivers more generally) provide environmental stimulation that is central for healthy development of the neural circuitry underlying later language and emotion regulation functioning.58
Brain development following PT birth
Considering these known adversities facing PT infants in their first months of life, it is not surprising that neural circuits with protracted developmental trajectories show long-lasting disruption.84 Specifically, when measured at term equivalent age, frontostriatal (FrS; including thalamocortical) and prefrontal-limbic systems (PrLS) have been shown to be different in PT infants compared to those born at term.85,86,87 For example, investigations of long-term outcomes of prematurity on brain development show that compared to full-term peers, children and adolescents born PT can have decreased subcortical-limbic gray matter volume of the hippocampus and amygdala.88 Disrupted brain development in PT children has been characterized as a maturational delay that might diminish as age increases.3,89 However, a very recent investigation provides evidence that regional differences in subcortical volumes, including limbic structures, are evident into adulthood for individuals born less than 33 weeks of gestation.6
In addition to differences in regional brain volume, there is strong evidence of delayed myelination of the white matter connecting brain networks in children born PT.85,86,90,91 Diffusion tensor imaging has been used to determine maturational increase of white matter in the first year of life in full-term and PT infants. Figure 2 integrates findings from several of these longitudinal investigations showing rate of increase in fractional anisotropy (FA; indicating white matter integrity). Anisotropy refers to directional dependence, and FA describes the degree to which water diffuses in a constrained fashion in a certain direction.92 Well-aligned white matter fibers with a high degree of structural integrity and myelination will constrain the diffusion of water directionally, increasing the anisotropy. Findings indicate that although white matter tract integrity increases in the weeks following PT birth, at term equivalent age PT infant white matter integrity is lower than healthy term-born infants and shows attenuated maturational increase (see Fig. 2). Moreover, recent research indicated less developed white matter at term equivalent age for PT infants born before 30 gestational weeks compared to PT infants born closer to term.93
A graph theory framework uses advanced statistical modeling to demonstrate brain connectivity as a network of nodes (brain regions) and links (connections between regions) and describes patterns of network connectivity, including the direction and strength of modeled connections.5,94,95 These studies provide converging evidence suggesting specialized structural network topology associated with prematurity that is characterized by reduced network integration (also referred to as efficiency) when compared to term-born equivalents.5,94,95 Considering that network integration is tightly linked to higher-order cognition, this finding is consistent with cognitive behavioral problems (e.g., lower executive functioning) facing children born PT, which will be discussed in detail in the next section. Moreover, findings indicate those with higher gestational ages showed increased network integration, which further underscores the benefits of structural connectivity associated with longer gestation.95 In contrast to disruption of network integration, findings also show normality of brain network topography such that functionally specialized subnetwork modules within the brain (also referred to as network modularity) appear unaffected.5 Together, these findings suggest that in response to PT birth, the developmental processes of neural reorganization might prioritize a tight, functionally specific modular structure at the cost of integration of the neural network as a whole. One hypothesis of specialized PT infant structural network topology is that when perinatal development occurs outside the intrauterine environment, more modular, life-sustaining brain circuitry is strengthened at the cost of the neural circuitry maturation required for subsequent cognitive aptitude and higher-order socioemotional function.
Common neurodevelopmental outcomes in the preterm population
Sensory motor problems
Muscle and movement deficits are usually the first neurodevelopmental impairments recognized in children born preterm.96 Abnormalities of extensor movements, hypotonia, and muscle asymmetries may even be recognized prior to term equivalent age.77,97 Cerebral palsy (CP) is the most common childhood physical disability.98 Between 9 and 20% of extremely preterm children have CP, with the largest proportion presenting with milder forms.76,99 The severity of CP is difficult to accurately define prior to 2 years, in part due to the fact that this period is one of incredibly rapid brain growth and experience/use-dependent neuronal reorganization in response to the environment, including interventions and therapy.100 Milder motor disorders are very common. Developmental coordination disorder (DCD) includes difficulties with balance, manual dexterity, and ball skills, and is present in approximately one-third of PT children101; however, the association of DCD with cognitive or neurosensory impairments is unclear.102 Minor neuromotor dysfunction (MND) is subtler than other more severe motor deficits including CP and indicates coordination difficulties, learning deficits, and deficits in fine motor function.101 MND does not generally occur alone, but in association with other subtle deficits which, taken together, cause significant academic struggles.101 Such minor motor disorders are associated with overall functional deficits and cognitive and behavioral abnormalities at school age in PT children.103
Language problems
Speech-language deficits are also common in preterm children. These deficits include abnormalities in speech articulation as well as expressive and receptive language.104,105,106,107,108,109,110 As with other neurodevelopmental impairments, language deficits are often associated with other deficits including hearing loss, cognitive deficits, behavioral abnormalities, and CP in PT children.110,111,112 Exposure to language is a critical environmental factor that is necessary for healthy development in the first 2 years of life.113 Further consideration of how medical and parental caregiving shapes language development in the PT population will be presented in the final section of this review.
Executive function
In addition to motor and language delays, PT birth is associated with many delays in higher-level domains of cognitive and social–emotional development. Beyond general delays in cognitive functioning,114 more specific delays have been documented in executive functioning.30,115 Problematically, these deficits are linked to increased risk for school failure, special education needs, and teacher reports of behavioral and general academic delays.116,117 Children born preterm are also at high risk of attention and information processing speed deficits, and these abnormalities are associated with early white matter injury.118 In children born preterm, processing speed abnormalities have been noted as early as 5 months of age and persist into later childhood.118,119,120 These processing speed and attention abnormalities may have a large and lasting impact on the development of higher cognitive skills that depend on these processes.
Executive functioning (EF) is an umbrella term referring to higher-order cognitive abilities, encompassing multiple skills such as aspects of attentional shifting, working memory, and inhibitory control.121 In recent years, EF has further been differentiated into ‘cool’ and ‘hot’ EF. Investigations of cool EF are focused on how aspects of working memory, attention, and inhibition support higher-order planning, flexible cognition, decision making, reasoning, and cognitive aspects of theory of mind, particularly in affective neutral environments. Hot EF reflects the larger construct of emotional regulation and is commonly engaged in situations that require affective processing, or within environments that include ‘emotion-laden’ stimuli.122
Supported by largely overlapping neural circuitry, hot and cool EF are mediated by healthy development of the FrS and PrLS.123 The neurocircuitry mediating EF can also be loosely dissociated into cool and hot functioning. This distinction is helpful to better understand the link between atypical neurological development and EF deficits in the larger PT population. Cool EF dysfunction in children born PT is broadly associated with disrupted PrLS system development with atypical prefrontal connections to cingulate and hippocampal brain regions linked to lower performance.124,125,126,127 Though less well understood, disruption in hot EF capacities have also been reported in children born PT.128 Specifically, atypicality of neurocircuitry mediating social–emotional processing is commonly reported in the PT population, including regional volume differences in the medial orbitofrontal cortex and amygdala as well as disruption to structural and functional connections within FrS.91
Clinical pathology
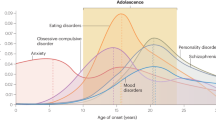
The cascading effects of PT birth that are described above can set these children on a path for more complex clinical pathologies. Although the majority of findings linking prematurity to disrupted EF and emotion regulation in childhood and adolescence indicate deficits just beyond the normal range of function, there is increasing awareness that PT birth is linked to psychopathologies that are highly disruptive to daily functioning. This includes clinical levels of some internalizing and externalizing behaviors and increased risk for attention deficit hyperactivity disorder.129,130,131,132 Adolescence is a phase of development during which many affective problems emerge.133 Not surprisingly, clinicians frequently report PT birth in association with increased risk for psychopathologies such as anxiety, depression, and attention deficit hyperactivity disorder in older children and adolescents.129 This also converges with parental reports of increased affective symptomatology.129,132
Plasticity and PT infant brain development
Traditionally, relations between risk factors and outcome following PT birth have been characterized by the diathesis stress model.134 In a diathesis stress framework, in identical poor rearing environments (e.g., low-quality parenting) children born PT are predicted to show vulnerability resulting in an increase in negative outcomes compared to those born full term. In recent years, however, several researchers have considered the differential susceptibility model as an alternative characterization of the interplay between prematurity and subsequent PT child outcome. Originated by Belsky and colleagues,135 the differential susceptibility model re-conceptualizes vulnerability factors as plasticity factors that modulate an individual’s environmental susceptibility for the better in high-quality environments and for the worse in poor-quality environments. Both the diathesis stress model and the differential susceptibility model propose that PT birth increases risk for negative outcome in rearing environments with lower quality of care; however, the differential susceptibility model also predicts that in rearing environments with higher quality of care, PT birth increases the probability of positive outcome.135
Two studies have directly tested diathesis stress compared to differential susceptibility models to determine a framework that characterizes how prematurity interacts with environmental susceptibility.29,136 In this line of research, Hadfield et al.136 found effect of maternal factors, including attachment and maternal distress, were similar between full-term and PT children; however, paternal distress effect on child cognitive and social development were moderated by prematurity. Since adversity of parental distress (but not the presence of positive emotional factors) drove the interaction between birth status and outcome, Hadfield et al.136 tentatively interpret paternal distress effects within a diathesis stress framework. Gueron-Sela et al.29 also compared effects of caregiving environment on PT child outcomes relative to a full-term comparison group with results more consistent with a differential susceptibility hypothesis. Specifically, compared to children born full term, in environments with high maternal distress and/or lower quality of caregiver interaction, PT infants showed reduced social outcomes, whereas PT infants showed increased social competence in environments with low distress and high-quality caregiver interaction.29
Although the weight of scientific evidence does not fully support a differential susceptibility account of prematurity effects on developmental outcomes, the differential susceptibility hypothesis of prematurity is also supported by findings of several studies showing that infants born PT or at VLBW are more susceptible to both negative and positive environmental influences.29,30,31,32,33 Moreover, a more theoretical basis for how positive environmental experiences in caregiving might benefit preterm infants more than infants born at term is available. Broadly, it is proposed that unlike term-born infants, PT infants are susceptible to overstimulation and need support in regulating their motor, autonomic, and state systems while minimizing stress in their environment.137 In the neonatal period, parenting that supports and improves the parent–child bond while parents learn how to effectively become the child’s “co-regulator” will gradually help the child self-regulate as they mature.83,138 Later in the infant period and beyond, responsive parenting behaviors, in which parents attend to their child’s communicative signals, appropriately interpret them, and respond sensitively and contingently, facilitates children’s positive development.138
In addition to prematurity related vulnerability, a disproportionate benefit of high-quality environments for PT compared to full-term children is a fundamental tenet of differential susceptibility theory139—that is yet to be fully addressed in the neuroimaging literature. Findings indicate that increasing maternal engagement during the NICU stay results in increased PT infant frontal brain activity during sleep, although intervention effects were equally beneficial for PT infants born prior to 31 gestational weeks compared to PT infants born later in gestation.128 Emerging results also indicate that supportive NICU experiences such as skin-to-skin contact are associated with stronger brain responses, whereas painful experiences such as breathing tube insertions and skin punctures are associated with reduced brain responses to the same touch stimuli.140 In light of the rapid prefrontal and limbic development in the first year of life (see Figs. 1 and 2), it is not surprising that there are converging results indicating that successful clinical implementation of practices to reduce stress during NICU care benefits frontal-limbic connectivity and neurodevelopmental outcomes in infants and children born PT, even when measured at age 8 years.141,142,143,144
Consistent with the idea that neural circuitry is most responsive to experience-dependent plasticity when it is rapidly developing, the protracted developmental course of frontal-striatal and frontal-limbic circuitries make these networks heavily influenced by experience, and early in life, experiences will primarily stem from interactions with caregivers.80,145,146 Evidence from animal studies shows that specific maternal nurturing maternal behaviors (e.g., licking/grooming) issued to offspring early in life results in experience-driven synaptic reorganization in frontal-limbic circuitries.147,148,149,150 Moreover, these nurturing maternal behaviors in rodents were found to have protective effects in PT pups who were exposed to pain shortly after birth.151,152 Consistent with animal literature, intervention research in humans, targeting early maternal sensitivity, has shown improved white matter development in PT neonates assigned to the intervention at term equivalent age.153 Finally, and perhaps the most convincing evidence suggesting a differential susceptibility hypothesis of prematurity within the context of brain development, is a single longitudinal study investigating the effects of maternal responsiveness on brain development in PT and full-term adolescents.52 Findings indicated differences in cortical thickness and cortical symmetry between term-born and preterm groups, possibly reflecting atypicality in synaptic production and pruning related to prematurity (see Fig. 1). Of note, cortical thickness in the PT group, but not the full-term group, was moderated by maternal responsiveness such that increased cortical thickness and greater cortical asymmetry were evident for adolescents with mothers who were inconsistently responsive or unresponsive during childhood.52 Findings from this longitudinal study are consistent with a differential susceptibility hypothesis of prematurity because, compared to children born full term, brain development of PT children was more susceptible to positive environmental events (i.e., consistent responsive parenting).
The role of intervention
Previous findings indicate that forming relationships with infants and supporting caregiver–infant co-regulation are key factors for healthy brain maturation (for reviews on this topic see Bick and Nelson58). Thus, there are clinically relevant implications for shifting characterization of prematurity from a factor reflecting vulnerability (i.e., diathesis stress model) to a plasticity factor which is susceptible to influence of both positive and negative environmental experiences. Most notably, prematurity characterized as a plasticity factor expands clinical treatment from remediation of negative environmental factors that are largely difficult to mitigate (e.g., NICU stress and parental distress) to inclusion of interventions that capitalize on positive environmental experiences (e.g., highly responsive caregiving). Specifically, interventions that target increased parental responsiveness to infant signals can provide parents the opportunity to learn to co-regulate with their preterm infants and to appreciate them as capable of communicating and being active social partners.
The last decade has seen a promising shift in the extent to which PT infant neonatal care facilities incorporate parental involvement in care during a NICU stay (e.g., family nurture interventions to increase skin-to-skin contact, sustained shared eye-contact, and quiet talk).83,154,155,156,157 Although substantially fewer preventative services target effects of parental characteristics on PT child outcome beyond the first months of life, the limited available literature indicates that parental characteristics such as low parental stress and high quality of parent–child interactions are environmental factors that facilitate resilient neurodevelopment following PT birth.32,138,158,159,160,161,162 Given that the first 3 years of life represent the most sensitive period of brain development,163,164 it is surprising that use of preventative programs that target increase in parental responsiveness, positive play, and use of rich language are not common practice. One reason that such parenting programs are not ubiquitously offered may be that the majority of early intervention services (i.e., physical and occupational therapy) are traditionally centered on the physical needs of the child. Although such early intervention is helpful for remediating some PT deficits,165 the addition of preventive parenting programs may be advantageous for empowering parents to be agents of change capable of improving their child’s long-term psychological health outcomes through nurturing of their child’s emotional and cognitive development. Results of parenting intervention studies administered in the first year of life and in early childhood show improvement to cognitive, language, and emotional outcomes in PT populations.32,138,165,166,167 Moreover, a recent follow-up study on a group of children born PT found increased cognitive, motor, and language scores for children assigned to parental invention group compared to a control group 7 years following the intervention; although intervention effects were only evident for families with elevated social risk (e.g., low family income).168
Of course, interventions targeting improved caregiving are one of many behavioral treatment programs that successfully leverage neural plasticity to improve PT child outcomes. To illustrate this point, consider CP, the most common childhood physical disability.98 Several investigations have reported success using CP-specific early intervention programs, targeting improved motor function, that capitalize on experience/use-dependent neuronal reorganization in response to the environment.100 Neuroscientific research indicates that motor cortex activity drives continued postnatal development of the motor system. Further, an infant’s motor interaction with the environment contributes to appropriate muscle, ligament, and bone growth in addition to driving the refinement of the motor system. This likely underlies the success of interventions for CP that maximize functional outcomes via neuroplasticity while minimizing the debilitating complications that can arise from detrimental adaptations in muscle and bone growth that may result from CP.
Conclusions
A promising approach to prevent and treat neurological and psychiatric diseases in PT populations is to leverage plasticity to support healthy developmental outcomes. Previous findings link quality of parenting to child brain development, suggesting the possibility that intervening to improve parenting might in turn improve child neurodevelopmental outcomes. Indeed, improving environmental factors through intervention have proven useful for mitigating motor, language, EF, and self-regulation deficits, especially for children born PT.58,81,169,170 However, additional neuroimaging investigations are urgently needed to develop a mechanistic understanding of the link between environmental susceptibility and neurodevelopment outcome following PT birth. Such work will enable better characterization of neurodevelopment outcomes in PT children and inform innovation of treatment to better leverage neuronal plasticity to promote healthy physical, emotional, and cognitive development in the preterm population.
References
Nagy, Z. et al. Structural correlates of preterm birth in the adolescent brain. Pediatrics 124, e964–e972 (2009).
Nagy, Z. & Jonsson, B. Cerebral MRI findings in a cohort of ex-preterm and control adolescents. Acta Paediatr. 98, 996–1001 (2009).
Nosarti, C. et al. Preterm birth and structural brain alterations in early adulthood. Neuroimage Clin. 6, 180–191 (2014).
Monson, B. B. et al. Examination of the pattern of growth of cerebral tissue volumes from hospital discharge to early childhood in very preterm infants. JAMA Pediatr. 170, 772–779 (2016).
Batalle, D. et al. Early development of structural networks and the impact of prematurity on brain connectivity. Neuroimage 149, 379–392 (2017).
Karolis, V. R. et al. Volumetric grey matter alterations in adolescents and adults born very preterm suggest accelerated brain maturation. Neuroimage 163, 379–389 (2017).
Bolk, J. et al. National population-based cohort study found that visual-motor integration was commonly affected in extremely preterm born children at six-and-a-half years. Acta Paediatr. 107, 831–837 (2018).
Bolk, J. et al. Visual-motor integration and fine motor skills at 6(1/2) years of age and associations with neonatal brain volumes in children born extremely preterm in Sweden: a population-based cohort study. BMJ Open 8, e020478 (2018).
Burnett, A. C. et al. Executive function in adolescents born<1000 g or <28 weeks: a prospective cohort study. Pediatrics 135, e826–e834 (2015).
Burnett, A. C. et al. Trends in executive functioning in extremely preterm children across 3 birth eras. Pediatrics 141, pii: e20171958 (2018).
Cheong, J. L. et al. Association between moderate and late preterm birth and neurodevelopment and social-emotional development at age 2 years. JAMA Pediatr. 171, e164805 (2017).
Cheong, J. L. Y. et al. Changing neurodevelopment at 8 years in children born extremely preterm since the 1990s. Pediatrics 139, pii: e20164086 (2017).
Witt, A. et al. Emotional and effortful control abilities in 42-month-old very preterm and full-term children. Early Hum. Dev. 90, 565–569 (2014).
Lejeune, F. et al. Social reasoning abilities in preterm and full-term children aged 5-7 years. Early Hum. Dev. 103, 49–54 (2016).
Kolb, B. & Gibb, R. Brain plasticity and recovery from early cortical injury. Dev. Psychobiol. 49, 107–118 (2007).
Kolb, B., Ladowski, R., Gibb, R. & Gorny, G. Does dendritic growth underly recovery from neonatal occipital lesions in rats. Behav. Brain Res. 77, 125–133 (1996).
Soria-Pastor, S. et al. Decreased regional brain volume and cognitive impairment in preterm children at low risk. Pediatrics 124, e1161–e1170 (2009).
Soria-Pastor, S. et al. Patterns of cerebral white matter damage and cognitive impairment in adolescents born very preterm. Int J. Dev. Neurosci. 26, 647–654 (2008).
Woodward, L. J., Clark, C. A., Pritchard, V. E., Anderson, P. J. & Inder, T. E. Neonatal white matter abnormalities predict global executive function impairment in children born very preterm. Dev. Neuropsychol. 36, 22–41 (2011).
Johnson, S. & Marlow, N. Growing up after extremely preterm birth: lifespan mental health outcomes. Semin. Fetal Neonatal Med. 19, 97–104 (2014).
Boardman, J. P. et al. Abnormal deep grey matter development following preterm birth detected using deformation-based morphometry. Neuroimage 32, 70–78 (2006).
Fenoglio, A., Georgieff, M. K. & Elison, J. T. Social brain circuitry and social cognition in infants born preterm. J. Neurodev. Disord. 9, 27 (2017).
Bennett, S. H., Kirby, A. J. & Finnerty, G. T. Rewiring the connectome: evidence and effects. Neurosci. Biobehav. Rev. 88, 51–62 (2018).
Luciana, M. Cognitive development in children born preterm: implications for theories of brain plasticity following early injury. Dev. Psychopathol. 15, 1017–1047 (2003).
Back, S. A. et al. Hypoxia-ischemia preferentially triggers glutamate depletion from oligodendroglia and axons in perinatal cerebral white matter. J. Cereb. Blood Flow. Metab. 27, 334–347 (2007).
Back, S. A., Riddle, A. & McClure, M. M. Maturation-dependent vulnerability of perinatal white matter in premature birth. Stroke 38, 724–730 (2007).
Degnan, A. J. et al. Altered structural and functional connectivity in late preterm preadolescence: an anatomic seed-based study of resting state networks related to the posteromedial and lateral parietal cortex. PLoS One 10, e0130686 (2015).
Hintz, S. R. et al. Neuroimaging and neurodevelopmental outcome in extremely preterm infants. Pediatrics 135, e32–e42 (2015).
Gueron-Sela, N., Atzaba-Poria, N., Meiri, G. & Marks, K. The caregiving environment and developmental outcomes of preterm infants: diathesis stress or differential susceptibility effects? Child Dev. 86, 1014–1030 (2015).
Camerota, M., Willoughby, M. T., Cox, M. & Greenberg, M. T. and the Family Life Project Investigators. Executive function in low birth weight preschoolers: the moderating effect of parenting. J. Abnorm. Child Psychol. 43, 1551–1562 (2015).
Landry, S. H., Smith, K. E., Swank, P. R., Assel, M. A. & Vellet, S. Does early responsive parenting have a special importance for children’s development or is consistency across early childhood necessary? Dev. Psychol. 37, 387–403 (2001).
Landry, S. H., Smith, K. E. & Swank, P. R. Responsive parenting: establishing early foundations for social, communication, and independent problem-solving skills. Dev. Psychol. 42, 627–642 (2006).
Jaekel, J., Pluess, M., Belsky, J. & Wolke, D. Effects of maternal sensitivity on low birth weight children’s academic achievement: a test of differential susceptibility versus diathesis stress. J. Child Psychol. Psychiatry 56, 693–701 (2015).
Thompson, J. L. & Nelson, A. J. Middle childhood and modern human origins. Hum. Nat. 22, 249–280 (2011).
Watson, R. E., Desesso, J. M., Hurtt, M. E. & Cappon, G. D. Postnatal growth and morphological development of the brain: a species comparison. Birth Defects Res. B Dev. Reprod. Toxicol. 77, 471–484 (2006).
Bjorklund, D. F. The role of immaturity in human development. Psychol. Bull. 122, 153–169 (1997).
Tottenham, N. The importance of early experiences for neuro-affective development. Curr. Top. Behav. Neurosci. 16, 109–129 (2014).
Paredes, M. F. et al. Extensive migration of young neurons into the infant human frontal lobe. Science 354, pii: aaf7073 (2016).
Stiles, J. & Jernigan, T. L. The basics of brain development. Neuropsychol. Rev. 20, 327–348 (2010).
Kostovic, I. & Jovanov-Milosevic, N. The development of cerebral connections during the first 20-45 weeks’ gestation. Semin. Fetal Neonatal Med. 11, 415–422 (2006).
Kostovic, I. & Judas, M. Prolonged coexistence of transient and permanent circuitry elements in the developing cerebral cortex of fetuses and preterm infants. Dev. Med Child Neurol. 48, 388–393 (2006).
Huttenlocher, P. R., de Courten, C., Garey, L. J. & Van der Loos, H. Synaptogenesis in human visual cortex--evidence for synapse elimination during normal development. Neurosci. Lett. 33, 247–252 (1982).
LaMantia, A. S. & Rakic, P. Axon overproduction and elimination in the anterior commissure of the developing rhesus monkey. J. Comp. Neurol. 340, 328–336 (1994).
Petanjek, Z., Judas, M., Kostovic, I. & Uylings, H. B. Lifespan alterations of basal dendritic trees of pyramidal neurons in the human prefrontal cortex: a layer-specific pattern. Cereb. Cortex 18, 915–929 (2008).
Hodel, A. S. Rapid infant prefrontal cortex development and sensitivity to early environmental experience. Dev. Rev. 48, 113–144 (2018).
Semple, B. D., Blomgren, K., Gimlin, K., Ferriero, D. M. & Noble-Haeusslein, L. J. Brain development in rodents and humans: Identifying benchmarks of maturation and vulnerability to injury across species. Prog. Neurobiol. 106-107, 1–16 (2013).
Huttenlocher, P. R. & Dabholkar, A. S. Regional differences in synaptogenesis in human cerebral cortex. J. Comp. Neurol. 387, 167–178 (1997).
Gogtay, N. et al. Dynamic mapping of normal human hippocampal development. Hippocampus 16, 664–672 (2006).
Brody, B. A., Kinney, H. C., Kloman, A. S. & Gilles, F. H. Sequence of central nervous system myelination in human infancy. I. An autopsy study of myelination. J. Neuropathol. Exp. Neurol. 46, 283–301 (1987).
Jabès, A. & Nelson, C. A. 20 years after “The ontogeny of human memory: a cognitive neuroscience perspective,” where are we? Int. J. Behav. Dev. 39, 293–303 (2015).
Whittle, S. et al. Positive parenting predicts the development of adolescent brain structure: a longitudinal study. Dev. Cogn. Neurosci. 8, 7–17 (2014).
Frye, R. E., Malmberg, B., Swank, P., Smith, K. & Landry, S. Preterm birth and maternal responsiveness during childhood are associated with brain morphology in adolescence. J. Int. Neuropsychol. Soc. 16, 784–794 (2010).
Kopala-Sibley D. C. et al. Early childhood parenting predicts late childhood brain functional connectivity during emotion perception and reward processing. Child Dev. 1–19 (2018).
Birn, R. M. et al. Extreme early-life anxiety is associated with an evolutionarily conserved reduction in the strength of intrinsic functional connectivity between the dorsolateral prefrontal cortex and the central nucleus of the amygdala. Mol. Psychiatry 19, 853 (2014).
Birn, R. M. et al. Evolutionarily conserved prefrontal-amygdalar dysfunction in early-life anxiety. Mol. Psychiatry 19, 915–922 (2014).
Ewing-Cobbs, L. et al. Longitudinal diffusion tensor imaging after pediatric traumatic brain injury: impact of age at injury and time since injury on pathway integrity. Hum. Brain Mapp. 37, 3929–3945 (2016).
Lenroot, R. K. & Giedd, J. N. Brain development in children and adolescents: insights from anatomical magnetic resonance imaging. Neurosci. Biobehav. Rev. 30, 718–729 (2006).
Bick, J. & Nelson, C. A. Early adverse experiences and the developing brain. Neuropsychopharmacology 41, 177–196 (2016).
Kidokoro, H. et al. Brain injury and altered brain growth in preterm infants: predictors and prognosis. Pediatrics 134, e444–e453 (2014).
Malik, S. et al. Neurogenesis continues in the third trimester of pregnancy and is suppressed by premature birth. J. Neurosci. 33, 411–423 (2013).
Penn, A. A., Gressens, P., Fleiss, B., Back, S. A. & Gallo, V. Controversies in preterm brain injury. Neurobiol. Dis. 92, 90–101 (2016).
Moulle, V. S., Cansell, C., Luquet, S. & Cruciani-Guglielmacci, C. The multiple roles of fatty acid handling proteins in brain. Front. Physiol. 3, 385 (2012).
Gilles, F., Gressens, P., Dammann, O. & Leviton, A. Hypoxia-ischemia is not an antecedent of most preterm brain damage: the illusion of validity. Dev. Med. Child Neurol. 60, 120–125 (2018).
Paton, M. C. B. et al. Perinatal brain injury as a consequence of preterm birth and intrauterine inflammation: designing targeted stem cell therapies. Front Neurosci. 11, 200 (2017).
Strunk, T. et al. Infection-induced inflammation and cerebral injury in preterm infants. Lancet Infect. Dis. 14, 751–762 (2014).
Thompson D. K. et al. Early life predictors of brain development at term-equivalent age in infants born across the gestational age spectrum. Neuroimage 1–12 (2018).
Young, J. M. et al. Longitudinal study of white matter development and outcomes in children born very preterm. Cereb. Cortex 27, 4094–4105 (2016).
Jellema, R. K. et al. Cerebral inflammation and mobilization of the peripheral immune system following global hypoxia-ischemia in preterm sheep. J. Neuroinflamm. 10, 13 (2013).
Counsell, S. J. et al. Diffusion-weighted imaging of the brain in preterm infants with focal and diffuse white matter abnormality. Pediatrics 112, 1–7 (2003).
Dean, J. M. et al. Prenatal cerebral ischemia disrupts MRI-defined cortical microstructure through disturbances in neuronal arborization. Sci. Transl. Med. 5, 168ra7 (2013).
Volpe, J. J. Confusions in nomenclature: “periventricular leukomalacia” and “white matter injury”-identical, distinct, or overlapping? Pediatr. Neurol. 73, 3–6 (2017).
Back, S. A. & Miller, S. P. Brain injury in premature neonates: a primary cerebral dysmaturation disorder? Ann. Neurol. 75, 469–486 (2014).
Ahya, K. P. & Suryawanshi, P. Neonatal periventricular leukomalacia: current perspectives. Res. Rep. Neonatol. 8, 1–8 (2018).
Burstein, J., Papile, L. A. & Burstein, R. Intraventricular hemorrhage and hydrocephalus in premature newborns: a prospective study with CT. AJR Am. J. Roentgenol. 132, 631–635 (1979).
Roberts, J. C., Javed, M. J., Hocker, J. R., Wang, H. & Tarantino, M. D. Risk factors associated with intraventricular hemorrhage in extremely premature neonates. Blood Coagul. Fibrinolysis 29, 25–29 (2018).
Jarjour, I. T. Neurodevelopmental outcome after extreme prematurity: a review of the literature. Pediatr. Neurol. 52, 143–152 (2015).
Aylward, G. P. Neurodevelopmental outcomes of infants born prematurely. J. Dev. Behav. Pediatr. 35, 394–407 (2014).
Rand, K. M., Austin, N. C., Inder, T. E., Bora, S. & Woodward, L. J. Neonatal infection and later neurodevelopmental risk in the very preterm infant. J. Pediatr. 170, 97–104 (2016).
Duerden, E. G. et al. Midazolam dose correlates with abnormal hippocampal growth and neurodevelopmental outcome in preterm infants. Ann. Neurol. 79, 548–559 (2016).
Belsky, J. & de Haan, M. Annual Research Review: parenting and children’s brain development: the end of the beginning. J. Child Psychol. Psychiatry 52, 409–428 (2011).
Bick J., Nelson C. A. Early experience and brain development. Wiley Interdiscip. Rev. Cogn. Sci. 8, 1–7 (2017).
Feldman, R., Rosenthal, Z. & Eidelman, A. I. Maternal-preterm skin-to-skin contact enhances child physiologic organization and cognitive control across the first 10 years of life. Biol. Psychiatry 75, 56–64 (2014).
Welch, M. G. Calming cycle theory: the role of visceral/autonomic learning in early mother and infant/child behaviour and development. Acta Paediatr. 105, 1266–1274 (2016).
de Kieviet, J. F., Zoetebier, L., van Elburg, R. M., Vermeulen, R. J. & Oosterlaan, J. Brain development of very preterm and very low-birthweight children in childhood and adolescence: a meta-analysis. Dev. Med. Child Neurol. 54, 313–323 (2012).
Ball, G. et al. The effect of preterm birth on thalamic and cortical development. Cereb. Cortex 22, 1016–1024 (2012).
Ball, G. et al. The influence of preterm birth on the developing thalamocortical connectome. Cortex 49, 1711–1721 (2013).
Padilla, N., Alexandrou, G., Blennow, M., Lagercrantz, H. & Aden, U. Brain growth gains and losses in extremely preterm infants at term. Cereb. Cortex 25, 1897–1905 (2015).
Taylor, H. G. et al. Brain volumes in adolescents with very low birth weight: effects on brain structure and associations with neuropsychological outcomes. Dev. Neuropsychol. 36, 96–117 (2011).
Nam, K. W. et al. Alterations in cortical thickness development in preterm-born individuals: implications for high-order cognitive functions. Neuroimage 115, 64–75 (2015).
de Kieviet, J. F. et al. A crucial role for white matter alterations in interference control problems of very preterm children. Pediatr. Res. 75, 731–737 (2014).
Fischi-Gomez, E. et al. Structural brain connectivity in school-age preterm infants provides evidence for impaired networks relevant for higher order cognitive skills and social cognition. Cereb. Cortex 25, 2793–2805 (2015).
Li, K. et al. Fractional anisotropy alterations in individuals born preterm: a diffusion tensor imaging meta-analysis. Dev. Med. Child Neurol. 57, 328–338 (2015).
Knight, M. J., Smith-Collins, A., Newell, S., Denbow, M. & Kauppinen, R. A. Cerebral white matter maturation patterns in preterm infants: an MRI T2 relaxation anisotropy and diffusion tensor imaging study. J. Neuroimaging 28, 86–94 (2018).
Fischi-Gomez, E. et al. Brain network characterization of high-risk preterm-born school-age children. Neuroimage Clin. 11, 195–209 (2016).
Kim, D. J. et al. Longer gestation is associated with more efficient brain networks in preadolescent children. Neuroimage 100, 619–627 (2014).
Spittle, A. J. & Orton, J. Cerebral palsy and developmental coordination disorder in children born preterm. Semin. Fetal Neonatal Med. 19, 84–89 (2014).
Allen, M. C., Cristofalo, E. A. & Kim, C. Outcomes of preterm infants: morbidity replaces mortality. Clin. Perinatol. 38, 441–454 (2011).
Novak, I., Hines, M., Goldsmith, S. & Barclay, R. Clinical prognostic messages from a systematic review on cerebral palsy. Pediatrics 130, e1285–e1312 (2012).
Hintz, S. R., Newman, J. E. & Vohr, B. R. Changing definitions of long-term follow-up: should “long term” be even longer? Semin. Perinatol. 40, 398–409 (2016).
Novak, I. et al. Early, accurate diagnosis and early intervention in cerebral palsy: advances in diagnosis and treatment. JAMA Pediatr. 171, 897–907 (2017).
Arnaud, C. et al. Prevalence and associated factors of minor neuromotor dysfunctions at age 5 years in prematurely born children: the EPIPAGE Study. Arch. Pediatr. Adolesc. Med. 161, 1053–1061 (2007).
Wilson, P. H., Ruddock, S., Smits-Engelsman, B., Polatajko, H. & Blank, R. Understanding performance deficits in developmental coordination disorder: a meta-analysis of recent research. Dev. Med. Child Neurol. 55, 217–228 (2013).
Ferrari, F. et al. Preterm birth and developmental problems in the preschool age. Part I: minor motor problems. J. Matern. Fetal Neonatal Med. 25, 2154–2159 (2012).
Marston, L., Peacock, J. L., Calvert, S. A., Greenough, A. & Marlow, N. Factors affecting vocabulary acquisition at age 2 in children born between 23 and 28 weeks’ gestation. Dev. Med. Child Neurol. 49, 591–596 (2007).
Ortiz-Mantilla, S., Choudhury, N., Leevers, H. & Benasich, A. A. Understanding language and cognitive deficits in very low birth weight children. Dev. Psychobiol. 50, 107–126 (2008).
Conrad, A. L., Richman, L., Lindgren, S. & Nopoulos, P. Biological and environmental predictors of behavioral sequelae in children born preterm. Pediatrics 125, e83–e89 (2010).
Foster-Cohen, S. H., Friesen, M. D., Champion, P. R. & Woodward, L. J. High prevalence/low severity language delay in preschool children born very preterm. J. Dev. Behav. Pediatr. 31, 658–667 (2010).
Barre, N., Morgan, A., Doyle, L. W. & Anderson, P. J. Language abilities in children who were very preterm and/or very low birth weight: a meta-analysis. J. Pediatr. 158, 766–74 e1 (2011).
Van Noort‐Van Der Spek, I. L., Franken, M. C. J., Wieringa, M. H. & Weisglas‐Kuperus, N. Phonological development in very‐low‐birthweight children: an exploratory study. Dev. Med. Child Neurol. 52, 541–546 (2010).
Vohr, B. Speech and language outcomes of very preterm infants. Semin. Fetal Neonatal Med. 19, 78–83 (2014).
Vohr, B. R., Topol, D., Watson, V., St Pierre, L. & Tucker, R. The importance of language in the home for school-age children with permanent hearing loss. Acta Paediatr. 103, 62–69 (2014).
Peralta-Carcelen, M., Bailey, K., Rector, R., Gantz, M. & Network, N. N. R. Behavioral and socioemotional competence problems of extremely low birth weight children. J. Perinatol. 33, 887–892 (2013).
McMahon, E., Wintermark, P. & Lahav, A. Auditory brain development in premature infants: the importance of early experience. Ann. N. Y. Acad. Sci. 1252, 17–24 (2012).
Anderson, P. J. & Doyle, L. W. Cognitive and educational deficits in children born extremely preterm. Semin. Perinatol. 32, 51–58 (2008).
Baron, I. S., Kerns, K. A., Muller, U., Ahronovich, M. D. & Litman, F. R. Executive functions in extremely low birth weight and late-preterm preschoolers: effects on working memory and response inhibition. Child Neuropsychol. 18, 586–599 (2012).
Best, J. R., Miller, P. H. & Naglieri, J. A. Relations between executive function and academic achievement from ages 5 to 17 in a large, representative national sample. Learn Individ Differ. 21, 327–336 (2011).
Johnson, S., Wolke, D., Hennessy, E. & Marlow, N. Educational outcomes in extremely preterm children: neuropsychological correlates and predictors of attainment. Dev. Neuropsychol. 36, 74–95 (2011).
Murray, A. L. et al. Neonatal brain pathology predicts adverse attention and processing speed outcomes in very preterm and/or very low birth weight children. Neuropsychology 28, 552–562 (2014).
Anderson, P. J. et al. Attention problems in a representative sample of extremely preterm/extremely low birth weight children. Dev. Neuropsychol. 36, 57–73 (2011).
Rose, S. A., Feldman, J. F. & Jankowski, J. J. Information processing in toddlers: continuity from infancy and persistence of preterm deficits. Intelligence 37, 311–320 (2009).
Miyake, A. et al. The unity and diversity of executive functions and their contributions to complex “Frontal Lobe” tasks: a latent variable analysis. Cogn. Psychol. 41, 49–100 (2000).
Mischel W., Ayduk O., Mendoza-Denton R. Sustaining Delay of Gratification Over Time: A Hot-Cool Systems Perspective (Russell Sage Foundation, New York, 2003).
Zelazo, P. D. & Carlson, S. M. Hot and cool executive function in childhood and adolescence: development and plasticity. child development. Perspectives 6, 354–360 (2012).
Caldinelli, C. et al. White matter alterations to cingulum and fornix following very preterm birth and their relationship with cognitive functions. Neuroimage 150, 373–382 (2017).
Nosarti, C. et al. Grey and white matter distribution in very preterm adolescents mediates neurodevelopmental outcome. Brain 131, 205–217 (2008).
Nosarti, C. et al. Impaired executive functioning in young adults born very preterm. J. Int. Neuropsychol. Soc. 13, 571–581 (2007).
Narberhaus, A. et al. Neural substrates of visual paired associates in young adults with a history of very preterm birth: alterations in fronto-parieto-occipital networks and caudate nucleus. Neuroimage 47, 1884–1893 (2009).
Montagna, A. & Nosarti, C. Socio-emotional development following very preterm birth: pathways to psychopathology. Front. Psychol. 7, 80 (2016).
Saigal, S., Pinelli, J., Hoult, L., Kim, M. M. & Boyle, M. Psychopathology and social competencies of adolescents who were extremely low birth weight. Pediatrics 111, 969–975 (2003).
Hack, M. et al. Behavioral outcomes and evidence of psychopathology among very low birth weight infants at age 20 years. Pediatrics 114, 932–940 (2004).
Bhutta, A. T., Cleves, M. A., Casey, P. H., Cradock, M. M. & Anand, K. J. Cognitive and behavioral outcomes of school-aged children who were born preterm: a meta-analysis. JAMA 288, 728–737 (2002).
Botting, N., Powls, A., Cooke, R. W. & Marlow, N. Attention deficit hyperactivity disorders and other psychiatric outcomes in very low birthweight children at 12 years. J. Child Psychol. Psychiatry 38, 931–941 (1997).
Cyranowski, J. M., Frank, E., Young, E. & Shear, M. K. Adolescent onset of the gender difference in lifetime rates of major depression: a theoretical model. Arch. Gen. Psychiatry 57, 21–27 (2000).
Monroe, S. M. & Simons, A. D. Diathesis-stress theories in the context of life stress research: implications for the depressive disorders. Psychol. Bull. 110, 406–425 (1991).
Belsky, J. The differential susceptibility hypothesis: sensitivity to the environment for better and for worse. JAMA Pediatr. 170, 321–322 (2016).
Hadfield, K., O’Brien, F. & Gerow, A. Is level of prematurity a risk/plasticity factor at three years of age? Infant Behav. Dev. 47, 27–39 (2017).
Vandenberg, K. A. State systems development in high-risk newborns in the neonatal intensive care unit: identification and management of sleep, alertness, and crying. J. Perinat. Neonatal Nurs. 21, 130–139 (2007).
Landry, S. H., Smith, K. E., Swank, P. R. & Guttentag, C. A responsive parenting intervention: the optimal timing across early childhood for impacting maternal behaviors and child outcomes. Dev. Psychol. 44, 1335–1353 (2008).
Belsky, J. & Pluess, M. Beyond diathesis stress: differential susceptibility to environmental influences. Psychol. Bull. 135, 885–908 (2009).
Maitre, N. L. et al. The dual nature of early-life experience on somatosensory processing in the human infant brain. Curr. Biol. 27, 1048–1054 (2017).
McAnulty, G. et al. School age effects of the newborn individualized developmental care and assessment program for medically low-risk preterm infants: preliminary findings. J. Clin. Neonatol. 1, 184–194 (2012).
McAnulty, G. et al. School-age effects of the newborn individualized developmental care and assessment program for preterm infants with intrauterine growth restriction: preliminary findings. BMC Pediatr. 13, 25 (2013).
Welch, M. G. et al. Family nurture intervention in preterm infants increases early development of cortical activity and independence of regional power trajectories. Acta Paediatr. 106, 1952–1960 (2017).
Welch, M. G. et al. Electroencephalographic activity of preterm infants is increased by Family Nurture Intervention: a randomized controlled trial in the NICU. Clin. Neurophysiol. 125, 675–684 (2014).
Luby, J. L., Belden, A., Harms, M. P., Tillman, R. & Barch, D. M. Preschool is a sensitive period for the influence of maternal support on the trajectory of hippocampal development. Proc. Natl. Acad. Sci. USA 113, 5742–5747 (2016).
Braun, K. The prefrontal-limbic system: development, neuroanatomy, function, and implications for socioemotional development. Clin. Perinatol. 38, 685–702 (2011).
Bock, J. & Braun, K. The impact of perinatal stress on the functional maturation of prefronto-cortical synaptic circuits: implications for the pathophysiology of ADHD? Prog. Brain Res. 189, 155–169 (2011).
Bock, J., Rether, K., Groger, N., Xie, L. & Braun, K. Perinatal programming of emotional brain circuits: an integrative view from systems to molecules. Front. Neurosci. 8, 11 (2014).
Liu, D., Diorio, J., Day, J. C., Francis, D. D. & Meaney, M. J. Maternal care, hippocampal synaptogenesis and cognitive development in rats. Nat. Neurosci. 3, 799 (2000).
Liu, D. et al. Maternal care, hippocampal glucocorticoid receptors, and hypothalamic-pituitary-adrenal responses to stress. Science 277, 1659–1662 (1997).
Francis, D. D., Diorio, J., Plotsky, P. M. & Meaney, M. J. Environmental enrichment reverses the effects of maternal separation on stress reactivity. J. Neurosci. 22, 7840–7843 (2002).
Walker, C. D., Xu, Z., Rochford, J. & Johnston, C. C. Naturally occurring variations in maternal care modulate the effects of repeated neonatal pain on behavioral sensitivity to thermal pain in the adult offspring. Pain 140, 167–176 (2008).
Milgrom, J. et al. Early sensitivity training for parents of preterm infants: impact on the developing brain. Pediatr. Res. 67, 330 (2010).
Welch, M. G. et al. Family nurture intervention (FNI): methods and treatment protocol of a randomized controlled trial in the NICU. BMC Pediatr. 12, 14 (2012).
Welch, M. G. et al. Randomized controlled trial of Family Nurture Intervention in the NICU: assessments of length of stay, feasibility and safety. BMC Pediatr. 13, 148 (2013).
Welch, M. G. et al. Family Nurture Intervention in the Neonatal Intensive Care Unit improves social-relatedness, attention, and neurodevelopment of preterm infants at 18 months in a randomized controlled trial. J. Child Psychol. Psychiatry 56, 1202–1211 (2015).
Welch, M. G. & Myers, M. M. Advances in family-based interventions in the neonatal ICU. Curr. Opin. Pediatr. 28, 163–169 (2016).
Grunau, R. E. et al. Neonatal pain, parenting stress and interaction, in relation to cognitive and motor development at 8 and 18 months in preterm infants. Pain 143, 138–146 (2009).
Tu, M. T. et al. Maternal stress and behavior modulate relationships between neonatal stress, attention, and basal cortisol at 8 months in preterm infants. Dev. Psychobiol. 49, 150–164 (2007).
Voigt, B. et al. Negative reactivity in toddlers born prematurely: indirect and moderated pathways considering self-regulation, neonatal distress and parenting stress. Infant Behav. Dev. 36, 124–138 (2013).
Landry, S. H., Smith, K. E., Miller-Loncar, C. L. & Swank, P. R. Predicting cognitive-language and social growth curves from early maternal behaviors in children at varying degrees of biological risk. Dev. Psychol. 33, 1040–1053 (1997).
Landry, S. H., Smith, K. E., Miller-Loncar, C. L. & Swank, P. R. The relation of change in maternal interactive styles to the developing social competence of full-term and preterm children. Child Dev. 69, 105–123 (1998).
Shonkoff, J. & Phillips, D. From Neurons to Neighbourhoods. The Science of Early Childhood Development (National Academy Press, Washington, 2000).
Shonkoff, J. P., Duncan, G. J., Fisher, P. A., Magnuson, K. & Raver, C. Building the Brain’s “Air Traffic Control” System: How Early Experiences Shape the Development of Executive Function. National Forum on Early Childhood Policy and Programs (Harvard University, Harvard, 2011).
Spittle, A. J., . & Orton, J. & Doyle, L. W. & Boyd, R. Early developmental intervention programs post hospital discharge to prevent motor and cognitive impairments in preterm infants. Cochrane Database Syst. Rev. 2, CD005495 (2007).
Spittle, A. J. et al. Preventive care at home for very preterm infants improves infant and caregiver outcomes at 2 years. Pediatrics 126, e171–e178 (2010).
Spittle A., Orton J., Anderson P. J., Boyd R., Doyle L. W. Early developmental intervention programmes provided post hospital discharge to prevent motor and cognitive impairment in preterm infants. Cochrane Database Syst. Rev. 11, CD005495 (2015).
Spittle, A. J., Treyvaud, K., Lee, K. J., Anderson, P. J. & Doyle, L. W. The role of social risk in an early preventative care programme for infants born very preterm: a randomized controlled trial. Dev. Med. Child Neurol. 60, 54–62 (2018).
Poehlmann, J. et al. Emerging self-regulation in toddlers born preterm or low birth weight: differential susceptibility to parenting? Dev. Psychopathol. 23, 177–193 (2011).
Merz, E. C., Landry, S. H., Montroy, J. J. & Williams, J. M. Bidirectional associations between parental responsiveness and executive function during early childhood. Soc. Dev. 26, 591–609 (2017).
Dubois, J., Hertz-Pannier, L., Dehaene-Lambertz, G., Cointepas, Y., Le Bihan, D. Assessment of the early organization and maturation of infants′ cerebral white matter fiber bundles: A feasibility study using quantitative diffusion tensor imaging and tractography. NeuroImage 30, 1121–1132 (2006).
Acknowledgments
We thank Bartlett D. Moore IV for assistance with graphical design of figures.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
DeMaster, D., Bick, J., Johnson, U. et al. Nurturing the preterm infant brain: leveraging neuroplasticity to improve neurobehavioral outcomes. Pediatr Res 85, 166–175 (2019). https://doi.org/10.1038/s41390-018-0203-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-018-0203-9
This article is cited by
-
Amygdala volumes and associations with socio-emotional competencies in preterm youth: cross-sectional and longitudinal data
Pediatric Research (2024)
-
Divergent neurodevelopmental profiles of very-low-birth-weight infants
Pediatric Research (2024)
-
Neuroprotective therapies in the NICU in preterm infants: present and future (Neonatal Neurocritical Care Series)
Pediatric Research (2024)
-
Parental cognitive stimulation in preterm-born children’s neurocognitive functioning during the preschool years: a systematic review
Pediatric Research (2023)
-
Parsing brain-behavior heterogeneity in very preterm born children using integrated similarity networks
Translational Psychiatry (2023)