Abstract
Background
Nutrient deficiencies limit the growth and turnover of intestinal mucosa, but studies assessing whether specific nutrients protect against or improve environmental enteric dysfunction (EED) are scarce. We aimed to investigate associations between nutrient intake and EED assessed by lactulose:mannitol (L:M) ratio, anti-1-antitrypsin, myeloperoxidase (MPO), and neopterin (NEO) among children 9–24 months in Bhaktapur, Nepal.
Methods
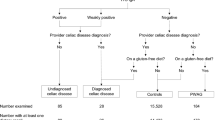
Among 231 included children, nutrient intake was assessed monthly by 24 h recalls, and 3-month usual intake was estimated using Multiple Source Method. Associations between nutrient intake and L:M ratio (measured at 15 months) were assessed using multiple linear regression, while associations between nutrient intake and fecal markers (measured quarterly) were assessed using Generalized Estimating Equations (GEE) models.
Results
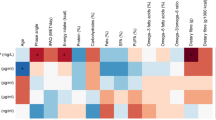
We found that associations between nutrient intake from complementary food and L:M ratio, alpha-1-antitrypsin (AAT), MPO and NEO were generally negative but weak. The only significant associations between nutrient intake (potassium, magnesium, phosphorous, folate, and vitamin C) and markers for intestinal inflammation were found for MPO.
Conclusion
Negative but weak associations between nutrient intake and markers of intestinal inflammation were found. Significant associations between several nutrients and MPO might merit further investigation.
Similar content being viewed by others
Introduction
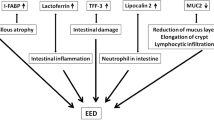
Environmental enteric dysfunction (EED) refers to a highly prevalent condition affecting populations in low- and middle-income countries (LMICs) with increased gut inflammation, increased intestinal permeability, and reduced absorption of nutrients due to villous atrophy1 and loss of enzymatic activity.2 EED is established during infancy and is associated with poor sanitation, gut infections, home births, micronutrient deficiencies, and breastfeeding practices.3 Possible consequences include infectious disease, stunting, impaired cognitive development, and reduced vaccine efficacy.4
The biomarker most commonly used to diagnose EED in previous studies is the lactulose:mannitol (L:M) ratio. While mannitol is passively absorbed proportional to intestinal absorptive capacity, lactulose is a disaccharide which is not absorbed by the healthy intestine. Increased L:M ratio thus indicates intestinal damage demonstrated by reduced absorptive capacity and increased permeability.2 Among newer, less-invasive biomarkers used to assess EED are the fecal markers alpha-1-antitrypsin (AAT) measuring intestinal permeability, myeloperoxidase (MPO) measuring neutrophil activity, and neopterin (NEO) representing Th-1 immune stimulation.5
Increased dietary diversity may enhance gut microbiota,1 which reduces the risk of intestinal inflammation.6 Further, generalized malnutrition, protein depletion, and deficiencies of specific nutrients including essential fatty acids, folate, zinc, vitamin A, and vitamin B12 have been shown to inhibit the growth and turnover of the intestinal mucosa.7 Meanwhile, studies assessing improvements in EED with micronutrient supplementation either alone8 or in combination with other interventions9 show mixed results. For specific nutrients, zinc10 and vitamin A11 have been associated with reduced L:M ratio in children, and alanyl-glutamin intake improved trans-mucosal resistance in mice.12 However, studies assessing whether specific nutrients protect against or improve EED are scarce. Also, studies investigating associations between nutrient intake and fecal markers for EED are mainly lacking.
The population of Bhaktapur, Nepal, has high socioeconomic status compared to national averages.13 Meanwhile, micronutrient adequacy, especially for iron, zinc, vitamin A, and niacin, among children in the MAL-ED Nepal cohort was very low,14 and the prevalence of anemia and zinc deficiency at 24 months was 29% and 23%, respectively.15 National governmental programs to improve micronutrient status are ready-to-use therapeutic food (RUTF) to children with severe malnutrition,16 a biannual vitamin A supplementation program for children 6–59 months and zinc supplementation to children with diarrhea.17 Finally, the main enteric pathogens causing diarrhea after 12 months of age in the MAL-ED Nepal cohort were campylobacter and enterohaemorrhagic E. coli (EHEC), norovirus GII, and rotavirus.18
The aim of this study was to investigate by exploratory analysis associations between nutrient intake and environmental enteric dysfunction assessed by L:M ratio, anti-1-antitrypsin, myeloperoxidase, and neopterin among children 9–24 months in Bhaktapur, Nepal.
Methods
Design and subjects
The MAL-ED Nepal site provided data for the analyses. The data collection took place in Bhaktapur, a peri-urban, agriculture-based community located 15 km east of Kathmandu. Children were enrolled within 17 days from birth and followed at least until 24 months. The data collection period for age 9–24 months was February 2011 to November 2012. Out of 240 enrolled children, 229 had complete nutrition data at 24 months, the number of urine samples (collected at 15 months) was 218, while the number of fecal samples varied throughout follow-up. Data were divided into five time slots (9–12, 12–15, 15–18, 18–21, and 21–24 months, respectively). The study received ethical approval from Nepal Health Research Council (NHRC) and the Walter Reed Institute of Research (Silver Springs, MD) and all caregivers signed informed consent forms. Further details on design and methodology are reported elsewhere.4
Dietary intake and socioeconomic status
Trained local fieldworkers conducted monthly 24-h recall interviews to collect data on foods and amounts consumed the previous day. A separate form was used to collect details about recipes. Amounts were estimated using household utensils, portion size booklets, and play dough. The FAO International Network of Food Data Systems (INFOODS) database for Asia19 was the main food composition database, but supplementary nutrient values from other databases were also used.
The Multiple Source Method20 was used to calculate individuals’ usual intake of energy, animal source protein, fiber, poly-unsaturated fatty acids (PUFA), iron, zinc, calcium, sodium, potassium, magnesium, phosphorous, thiamin, riboflavin, niacin, pantothenic acid, vitamin B6, folate, vitamin B12, A, C, and E. Usual intake was calculated based on three 24 h recalls in each time slot or four recalls in time slots with secondary recalls. Socioeconomic status was assessed by questionnaire at 12 months by a WAMI (Water, Assets, Maternal education and Income) index, with scores ranging from 0 to 1.21 The 8 assets included were separate room for a kitchen, household bank account, mattress, refrigerator, TV, people per room (mean), table, and chair or bench.
Nutrient density adequacy
The nutrient density (ND) was defined as the amount of nutrient consumed per 100 kcal of complementary food and calculated for 10 micronutrients: thiamin, riboflavin, niacin, vitamin B6, folate, vitamin C, vitamin A, calcium, iron, and zinc. Context-specific desired nutrient density (DND) and nutrient density adequacy (NDA) of complementary foods was calculated based on methodology by Dewey and Brown22 for the same micronutrients. For each time slot and for each nutrient, context specific DNDs were calculated in the following way:
[Recommended nutrient intake (RNI) of nutrient χ − (concentration of nutrient χ in breastmilk × median breast milk intake in time slot)]/median energy intake from complementary food in time slot × 100.
For iron, FAO/WHO micronutrient requirements corresponding to low absorption (5%), while for zinc low or middle absorption23 (depending on the phytate:zinc ratio measured) was used. For nutrients where the levels in breast milk are negatively affected by maternal status (thiamin, riboflavin, vitamin B6, and vitamin A), we used concentrations based on studies conducted among women in low income countries.24, 25 Otherwise, WHO values based on breast milk from western women26 were used. Breast milk intake was not assessed, but calculated the following way:
[Total energy requirements (body weight measured monthly × FAO energy requirement per kg body weight for the appropriate age)27 − energy intake from complementary food] /energy density of breast milk (LMICs)26
For non-breastfed children, desired nutrient densities were calculated as FAO/WHO micronutrient requirements23 divided by median energy intake in the non-breastfed group.
NDA was calculated for each nutrient and for each observation as the ND as percentage of the DND. Finally, mean nutrient density adequacy (MNDA) was calculated as the mean of individual NDAs for all ten micronutrients each capped at 100%. Mean MNDA based on 3 months measurements (i.e., measured at 9, 10, and 11 months for time slot 1) was used in the analysis. A more detailed description of calculations of MNDA are reported elsewhere.14
L:M ratio and fecal markers for EED
Children were instructed to fast 2 h prior to and 30 m after the L:M test and recommended to void before administration of the sugar dose. The L:M ratio was assessed in urine collected during voiding (5 h follow-up period) following the administration of 250 mg/mL lactulose and 50 mg/mL mannitol at a dose of 2 mL/kg to a maximum administered dose of 20 mL at a concentration of 1002 mOsm/L. Aliquots were stored at −70 °C until testing and concentrations of lactulose and mannitol measured by high-performance liquid chromatography (HPLC) and either pulsed amperometric detection or iron chromatography. Results were presented as molar ratio of lactulose to mannitol.5 During our follow-up period L:M ratio was only measured at 15 months. Due to skewed values, the variable was log-transformed.
Stool samples were collected monthly for children <12 months, then quarterly up to 36 months age.4 Samples collected at 12, 15, 18, 21, and 24 months were used in the analysis. The samples were stored for processing at −70 °C without fixative.5 The concentrations of AAT, MPO, and NEO were measured by ELISA tests at Walter Reed/AFRIMS Research Unit Nepal (WARUN) with initial dilutions of 1:500 ng/mL for MPO (ALPCO, Salem, NH), AAT (BioVendor, Candler, NC) and NEO (GenWay Biotech, San Diego, CA). Tests showing out of range values were run again at a two-fold higher or lower (as appropriate) concentration.5 To avoid overly diluting the samples, stool samples collected either during or ≤7 days after a diarrheal episode (three semi-liquid stools in a 24 h period separated by ≥2 days without diarrhea) or at the same time as the urine sample for the L:M test of intestinal permeability inherent in MAL-ED protocol4 were excluded. Due to skewed distributions, the variables were log-transformed to obtain normality and ease interpretation of results.
Statistical analysis
Continuous data are presented as mean and standard deviation (SD) if normally distributed, and as median and interquartile range (IQR) if not normally distributed. Variables to be included in regression models were selected based on a theory-based approach. Models for associations between nutrient intake and MNDA and L:M ratio, AAT, MPO, and NEO, respectively, are presented. Models for nutrient intake and L:M ratio and fecal markers were adjusted for energy intake from complementary food, WAMI, gender, season, and age (only for fecal markers), while models with MNDA were not adjusted for energy intake. We also tried adjusting for stool consistency, but due to very little variation this made no changes to the estimates and was excluded. Models describing associations between nutrient intake and L:M ratio were assessed with multiple linear regression analysis. All other analysis was performed using GEE with autoregressive (AR-1) covariance structure. Season was coded according to the date when the fecal sample was taken as pre-monsoon (March–May), monsoon (June–August), post monsoon (September–November), and winter (December–January). Apart from season and gender, all variables were continuous. The statistical package for the social sciences (SPSS) version 24.0 was used for data analysis.
Results
The baseline characteristics of mother and child pairs are presented in Table 1. The mean (SD) age of mothers was 274 years and 11% had 3 children or more. The median (IQR) number of assets (out of 8 assessed) was 6.5, 7 Median (IQR) WAMI score was 0.7 (0.6, 0.8), where all participants had access to improved water and sanitation. The majority of participants (53%) were male.
L:M ratio, fecal markers for EED, nutrient intake, nutrient adequacy, and information about breast feeding is presented in Table 2. All outcome variables were skewed with some very high values. The median (IQR) L:M ratio was 0.07 (0.05, 0.12), where 26% had values above the reference (0.12).28 All fecal markers decreased gradually with age. The largest reductions between the first and the last time slot were seen for MPO (74%) and NEO (72%).
Associations between intake of individual nutrients and MNDA and L:M ratio, AAT, MPO, and NEO are presented in Table 3. Associations were generally negative and weak with few significant findings in view of the number of models presented. Significant negative associations were found between intake of potassium (−0.33, CI −0.61, −0.05), magnesium (−2.81, CI −5.36, −0.26), phosphorous (−0.58, CI −1.14, −0.02), folate (−2.08, CI −3.90, −0.25), vitamin C (−0.01, CI −0.001, 0), and MNDA (−0.01, CI −0.01, 0) and log MPO. Weak but significant negative associations were also found between intake of zinc, calcium, potassium, magnesium, phosphorous, and lactulose (data not shown), while for L:M ratio, AAT, NEO, and mannitol no significant associations were found.
Discussion
We found that associations between nutrient intake from complementary food and L:M ratio, AAT, MPO, and NEO were generally negative but weak and few reached statistical significance. The only significant associations between nutrient intake and markers for intestinal inflammation were found for MPO.
The weak associations found between nutrient intake and intestinal inflammation are comparable to a cross-sectional study among 18 months old children in Bangladesh,29 and likely has several explanations. Firstly, associations between nutrient intake and EED are hard to assess since they are bidirectional or cyclical in nature, with malnutrition being both a cause and a consequence of EED. The level of severity of EED in our population might also be questioned since most participants had L:M ratios below the reference standard. Intestinal permeability is mediated by inflammation,30 and effects of enteroaggressive pathogens on fecal markers are cumulative.31 Meanwhile, a murine study by Brown et al. showed that increased permeability due to enteropathogens was only present in mice who had consumed a malnourished (in energy and protein) diet.6 Although the severity of intestinal lesions associated with elevated MPO, to our knowledge, is unknown, our data suggest that in this population, EED may be moderate and the demand (additional to daily requirements) for typical “repair nutrients”, such as folate, zinc, and vitamin B12,7 relatively limited. Further, nutrient intake in our study was assessed only from complementary food, whereas estimates of breast milk intake performed in a previous study suggested that this population were high breast milk consumers.14 Adjusting for energy intake from complementary food in our analysis did not account for the favorable absorption of many nutrients (i.e., zinc and iron)32 from breast milk compared to complementary food with low bioavailability.14 As a result, associations between nutrient intake, vitamin status, and EED may be distorted.
Other important aspects likely to weaken associations between nutrient intake and EED in our study is the length of follow-up and the age of the included children (9–24 months). The gut microbiota matures and becomes more stable during the first 3 years of life.33 This process is negatively influenced by malnutrition and frequent use of antibiotics15 and likely positively influenced by increased dietary diversity.34 Improved microbiota maturity is in turn associated with increased resistance to pathogens.34 In addition, it is hypothesized that increased levels of the biomarkers assessed may be side-effects of self-limiting natural processes (intestinal immune maturation) up to a certain “turning-point” where after elevated levels indicate EED.30 If this turning point occurs within our period of follow-up but at different time points for each participant, it could further complicate interpretation of results. In the end, dividing the data into 3-month time slots may not be sufficiently refined to assess the complex temporal interplay between nutrient intake, pathogen exposure and markers of EED in our age group. Finally, correlations between the fecal markers assessed and between the fecal markers and L:M ratio are low,35 indicating that they reflect different biological processes. For this reason, more comprehensive scores may be needed to adequately describe EED and assess risk factors associated with EED.31
Although the number of models performed in our study suggests that some significant associations likely are spurious, those found between several nutrients, MNDA, and MPO may still be of importance. MPO is the fecal marker most strongly affected by the most prevalent enteroaggressive pathogen (Campylobacter) in this population and in MAL-ED overall.18 It was the only fecal marker out of the three assessed here which was significantly associated with length velocity among children in the Bhaktapur cohort36 and may thus be the marker most indicative of EED in our population. The usefulness of MPO as a biomarker for inflammatory bowel disease (IBD) is currently being investigated, and has been shown to increase both with onset and severity of the disease.37 Although studies assessing associations between nutrient intake and MPO are lacking, both magnesium, vitamin C, potassium and fruit and vegetable intake have been associated with decreased risk of IBD.38 Although the pathways at present seem unclear, these foods and nutrients may protect against intestinal inflammation, which supports our findings. However, potential associations between intake of specific nutrients and MPO need to be corroborated by future studies.
The main strength of the study is the longitudinal design with monthly measurements of nutrient intake enabling calculations of within- and between-subject variance and likely more valid assessment of nutrient intake than in a cross-sectional study. The level of detail of nutrient data collected was high and included estimation of amounts. Fecal markers were assessed from asymptomatic stool samples. Frequent assessment of diarrhea incidence (several times per week) was a major advantage that improved the quality of data for fecal marker concentrations. Both L:M ratio and fecal markers were assessed according to strict guidelines in laboratories undergoing regular quality checks and standardization of tests between MAL-ED sites.5 The sample was drawn from a relatively homogenous population. Finally, retention was favorable (85% in the final time slot) in the MAL-ED Nepal cohort.
The main limitation of our study was uncertainty about the reliability of the outcome variables assessed. The L:M ratio may be affected by mannitol believed to be present naturally in urine, and HPLC may lack sensitivity for determining low concentrations of lactulose35 while both MPO and NEO are non-specific markers of intestinal immunity.2 Also, assessing only nutrient intake from complementary food in this group who are high breast milk consumers,14 weakens the strength of the inferences made from our study. Further, since all participants had access to improved water and sanitation, it was impossible to assess differences between exposed and unexposed participants regarding water, sanitation, and hygiene believed to be of major importance in the development of EED.31 The vast number of regression models increases the likelihood of spurious significant associations. Meanwhile, correction for multiple comparisons is not required in explorative studies.39 Finally, the lack of international reference standards for biomarkers for EED, complicates the interpretation of results.
Conclusions
We found that associations between nutrient intake from complementary food and L:M ratio, AAT, MPO, and NEO were generally negative but weak in this group of children aged 9–24 months in Bhaktapur, Nepal. The only significant associations were found for intake of potassium, magnesium, phosphorous, folate, vitamin C and MNDA and MPO. General approaches, such as improving dietary diversity, might have beneficial effects on microbiota and gut maturation and would likely be advantageous in reducing EED in our population and in similar settings.
References
Owino, V. et al. Environmental enteric dysfunction and growth failure/stunting in global child health. Pediatrics 138 pii: e2016064117 (2016).
Syed, S., Ali, A. & Duggan, C. Environmental enteric dysfunction in children. J. Pediatr. Gastroenterol. Nutr. 63, 6–14 (2016).
Crane, R. J., Jones, K. D. & Berkley, J. A. Environmental enteric dysfunction: an overview. Food Nutr. Bull. 36, S76–S87 (2015).
The MAL-ED Network Investigators. The MAL-ED study: a multinational and multidiciplinary approach to understand the relationship between enteric pathogens, malnutrition, gut physiology, physical growth, cognitive development, and immune responses in infants and children up to 2 years of age in resource-poor environments. Clin. Infect. Dis. 59(Suppl 4), S193–S206 (2014).
Kosek, M. et al. Assessment of environmental enteropathy in theMAL-ED cohort study: theoretical and analytic framework. Clin. Infect. Dis. 59(Suppl 4), S239–S247 (2014).
Brown, E. M. et al. Diet and specific microbial exposure trigger features of environmental enteropathy in a novel murine model. Nat. Commun. 6, 7806 (2015).
Ziegler, T. R. et al. Trophic and cytoprotective nutrition for intestinal adaptation, mucosal repair, and barrier function. Annu. Rev. Nutr. 23, 229–261 (2003).
Smith, H. E. et al. Multiple micronutrient supplementation transiently ameliorates environmental enteropathy in Malawian children aged 12-35 months in a randomized controlled clinical trial. J. Nutr. 144, 2059–2065 (2014).
Wang, A. Z. et al. A combined intervention of zinc, multiple micronutrients, and albendazole does not ameliorate environmental enteric dysfunction or stunting in rural malawian children in a double-blind randomized controlled trial. J. Nutr. 147, 97–103 (2017).
Manary, M. J. et al. Perturbed zinc homeostasis in rural 3-5-y-old Malawian children is associated with abnormalities in intestinal permeability attributed to tropical enteropathy. Pediatr. Res. 67, 671–675 (2010).
Thurnham, D. I. et al. Innate immunity, gut integrity, and vitamin A in Gambian and Indian infants. J. Infect. Dis. 182(Suppl 1), S23–S28 (2000).
Ueno, P. M. et al. Alanyl-glutamine promotes intestinal epithelial cell homeostasis in vitro and in a murine model of weanling undernutrition. Am. J. Physiol. Gastrointest. Liver Physiol. 301, G612–G622 (2011).
Shrestha, P. S. et al. Bhaktapur, Nepal: theMAL-ED birth cohort study in Nepal. Clin. Infect. Dis. 59(Suppl 4), S300–S303 (2014).
Morseth, M. S., et al. Severely inadequate micronutrient intake among children 9-24 months in Nepal-The MAL-ED birth cohort study. Matern. Child Nutr. 14, e12552, 2017.
Lang, D & MAL-ED Network Investigators. Opportunities to a ssess factors contributing to the development of the intestinal microbiota in infants living in developing countries. Microb. Ecol. Health Dis. 26, 28316 (2015).
Ministry of Health and Population, Government of Nepal. NEPAL Integrated Management of Acute Malnutrition (IMAM) Guideline Draft 7: 8 February 2017 (Ministry of Health and Population (MoHP), Government of Nepal, 2017)
Bhandari, S. & Banjara, M. R. Micronutrients deficiency, a hidden hunger in Nepal: prevalence, causes, consequences, and solutions. Int. Sch. Res. Notices 2015 276469 (2015).
Platts-Mills, J. A. et al. Pathogen-specific burdens of community diarrhoea in developing countries: a multisite birth cohort study (MAL-ED). Lancet Glob. Health 3, e564–e575 (2015).
FAO. International System of Food Data Systems (INFOODS). http://www.fao.org/infoods/infoods/tables-and-databases/faoinfoods-databases/en/.
Harttig, U. et al. The MSM program: web-based statistics package for estimating usual dietary intake using the Multiple Source Method. Eur. J. Clin. Nutr. 65 (Suppl 1), S87–S91 (2011).
Psaki, S. R. et al. Measuring socioeconomic status in multicountry studies: results from the eight-country MAL-ED study. Popul. Health Metr. 12, 8 (2014).
Working Group on Infant and Young Child Feeding Indicators. Developing and Validating Simple Indicators of Dietary Quality and Energy Intake of Infants and Young Children in Developing Countries: Summary of findings from analysis of 10 data sets. (Food and Nutrition Technical Assistance Project (FANTA), Washington DC, 2006).
FAO/WHO. Vitamin and Mineral Requirements in Human Nutrition (FAO/WHO, 2002)
Allen, L. H. B vitamins in breast milk: relative importance of maternal status and intake, and effects on infant status and function. Adv. Nutr. 3, 362–369 (2012).
Rice, A. L. et al. Maternal vitamin A or beta-carotene supplementation in lactating bangladeshi women benefits mothers and infants but does not prevent subclinical deficiency. J. Nutr. 129, 356–365 (1999).
WHO. Complementary Feeding of Young Children in Developing Countries: a Review of Current Scientific Knowledge (World Health Organization, Geneva, 1998).
FAO. Human Energy Requirements (FAO, Rome, 2004)
Lunn, P. G., Northrop-Clewes, C. A. & Downes, R. M. Intestinal permeability, mucosal injury, and growth faltering in Gambian infants. Lancet 338, 907–910 (1991).
Campbell, R. K. Environmental Enteric Dysfunction in Early Childhood: Bridging the Gap Between Diet and Stunting in a Randomized Trial of Complementary Food Supplementation in Rural Bangladesh. PhD thesis, John Hopkins University, Baltimore, MD (2016).
Colston, J. M. et al. A methodologic framework for modeling and assessing biomarkers of environmental enteropathy as predictors of growth in infants: an example from a Peruvian birth cohort. Am. J. Clin. Nutr. 106, 245–255 (2017).
McCormick, B. J. et al. Dynamics and trends in fecal biomarkers of gut function in children from 1-24 months in the MAL-ED study. Am. J. Trop. Med. Hyg. 96, 465–472 (2017).
Krebs, N. F. Bioavailability of dietary supplements and impact of physiologic state: infants, children and adolescents. J. Nutr. 131, 1351S–1354S (2001).
Yatsunenko, T. et al. Human gut microbiome viewed across age and geography. Nature 486, 222–227 (2012).
Velly, H., Britton, R. A. & Preidis, G. A. Mechanisms of cross-talk between the diet, the intestinal microbiome, and the undernourished host. Gut Microbes 8, 98–112 (2017).
Campbell, R. et al. Association between urinary biomarkers of total sugars intake and measures of obesity in a cross-sectional study. PLoS ONE 12, e0179508 (2017).
Morseth, M. S. et al. Environmental enteropathy, micronutrient adequacy and length velocity in Nepalese children - the MAL-ED Birth Cohort Study. J. Pediatr. Gastroenterol. Nutr. (2018) 10.1097/MPG.0000000000001990.
Hansberry, D. R. et al. Fecal myeloperoxidase as a biomarker for inflammatory bowel disease. Cureus 9, e1004 (2017).
Reif, S. et al. Pre-illness dietary factors in inflammatory bowel disease. Gut 40, 754–760 (1997).
Bender, R. & Lange, S. Adjusting for multiple testing--when and how? J. Clin. Epidemiol. 54, 343–349 (2001).
Dewey, K. G. & Brown, K. H. Update on technical issues concerning complementary feeding of young children in developing countries and implications for intervention programs. Food and Nutrition Bulletin 24, 5–28 (2003).
Acknowledgements
We thank the staff, children, and caregivers of the MAL-ED Bhaktapur site for their contributions. This work was supported by the Bill & Melinda Gates Foundation (grant number OPP47075); the Foundation for the NIH and the National Institutes of Health, Fogarty International Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Morseth, M.S., Strand, T.A., Torheim, L.E. et al. Nutrient intake and environmental enteric dysfunction among Nepalese children 9–24 months old—the MAL-ED birth cohort study. Pediatr Res 84, 509–515 (2018). https://doi.org/10.1038/s41390-018-0108-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-018-0108-7