Abstract
Background
We investigated ‘rare’ bile acids (BA) as potential markers in septic neonates.
Methods
‘Rare’ (C-6 hydroxylated BA) and ‘classical’ BA were determined in 102 neonates using high-performance liquid chromatography—high-resolution mass spectrometry (HPLC-HRMS). Four groups according to maturity (full term, FT vs. preterm, PT) and septic status (early-onset neonatal sepsis, EOS vs. CTR; non-septic controls) were formed: FT-CTR; (n = 47), PT-CTR (n = 22), FT-EOS (n = 20), PT-EOS (n = 13).
Results
Firstly, FT-CTR had a significant higher amount of ‘rare’ BA than PT (FT-CTR: 0.5 µmol/L, IQR: 0.3–1.3 vs. PT-CTR: 0.01 µmol/L, IQR 0.01–0.2; p < 0.01). The most common ‘rare’ BA in FT-CTR were tauro-γ- (TGMCA) and tauro-α-muricholic acid (TAMCA). Secondly, in EOS, absolute ‘rare’ BA levels were comparable in both gestational age groups (FT-EOS: 0.6 µmol/L, IQR: 0.1–1.6 and PT-EOS: 0.6 µmol/L, IQR: 0.2–1.5). Therefore, EOS had significantly higher median ‘rare’ BA values than non-septic PT neonates (p < 0.01). In PT and term neonates, the relative amount of tauro-ω-muricholic acid (TOMCA) within the ‘rare’ BA pool was significantly higher in EOS than in controls (FT-CTR vs. "FT-EOS and PT-CTR vs. PT-EOS; p < 0.01). It was hence the predominant ‘rare’ BA in EOS.
Conclusion
TOMCA is an independent factor associated with EOS. It has diagnostic potential.
Similar content being viewed by others
Introduction
Bile acids (BA) differ in quantity—total serum BA levels—and quality—BA composition (‘BA profile’)—between adults and neonates.1,2 In both adults and neonates, the ‘typical’ primary BA cholic (CA) and chenodeoxycholic acid (CDCA) are the predominant BA species. However, in neonates, ‘rare’ tri-hydroxylated BA like C-6 hydroxylated primary BA α-(AMCA) and β-muricholic acid (BMCA) or the secondary BA γ-(GMCA), ω-muricholic (OMCA) acid, and hyodeoxycholic acid (HDCA) also are synthesized (Fig. 1).3,4 Like ‘classical’ human BA, C-6 hydroxylated BA undergo conjugation with either glycine (G; predominant in human adults) or taurine (T; predominant in mice and neonates), eventually creating glyco-, tauro-, or unconjugated BA species, among them tauro-OMCA (TOMCA). In mice, ‘rare’, C-6 hydroxylated BA are mainly found, and are the predominant BA species. Why C-6 hydroxylated BA are rarely found in humans is not yet known. They are encountered, however, as conjugates in umbilical cord blood and amniotic fluid.4,5 No published values exist for C-6 hydroxylated BA levels in neonatal serum as determined by modern measuring methods including high-performance liquid chromatography—high-resolution mass spectrometry (HPLC-HRMS).4,6
BA synthesis process: primary bile acids (BA; CA and CDCA in humans and CA, AMCA and BMCA in mice) reach the intestinal lumen after gallbladder contraction via the biliary tract. The diversity of the BA pool is expanded by secondary BA formed by the intestinal microbiota (DCA, UDCA and LCA in humans and GMCA, OMCA acid and HDCA in mice). AMCA α-muricholic acid, BMCA β-muricholic acid, CA cholic acid, CDCA chenodeoxycholic acid, GMCA γ-muricholic acid, OMCA ω-muricholic acid, DCA deoxycholic acid, HDCA hyodeoxycholic acid, LCA lithocholic acid, UDCA ursodeoxycholic acid
Early-onset sepsis (EOS) is a severe illness with a mortality rate ranging from 2 to 3% in full term (FT) infants to 20–30% in preterm (PT) infants.7 On the basis of the timing of the infection, neonatal sepsis has been classified into EOS (≤72 h) and late-onset sepsis (>72 h).8 EOS may originate from both the mother and the child. Maternal risks can arise before labor including invasive procedures during pregnancy, or during birth due to prolonged rupture of membranes, fever, or vaginal colonization with group B streptococcus.9,10 Diagnosis consists of obtaining a complete white blood cell count with a single blood culture. Additionally, cytokines have been tested as laboratory biomarkers including C-reactive protein (CRP), interleukin-6 (IL-6), and procalcitonin (PCT)11,12; however, all lack sensitivity or specificity.13
In a previous study, we reported that serum levels of typical BA in both FT and PT neonates are markedly lower than in older children and adults. So far, it is unclear how EOS affects C-6 hydroxylated BA metabolism. This study aimed, using HPLC-HRMS, (i) to determine reference values of serum C-6 hydroxylated BA levels in non-septic neonates born FT or PT and (ii) to investigate possible BA changes due to EOS.
Materials and methods
Study design and patient characteristics
We conducted a prospective study at the Department of Pediatrics and Adolescent Medicine of the Medical University of Graz and collected serum samples of 102 neonates (aged 1–3 days; FT and PT) between January and December 2016. The study was approved by the Medical University of Graz ethics committee (28–173 ex 15/16). Prematurity was diagnosed when neonates were born at <37 weeks’ gestation. EOS was confirmed by complete white blood cell count with a positive blood culture and CRP concentrations above 5 mg/L. All neonates with primary liver or biliary-tract disorders or asphyxia were excluded and EOS was excluded in controls. Fasting blood sampling in non-septic and EOS neonates was performed during routine screening for phenylketonuria or routine measurements, respectively. Blood sampling was within 48 h after starting antibiotics. Neonates not fed within 2 h were considered ‘fasted’. Overnight fasting blood sample collection was not possible since newborn infants are fed at least every 4 h. Finally, serum samples were stored at −80°C until assays.
Laboratory analysis
Analyses including concentrations of CRP, IL-6, PCT, and bilirubin were measured by standard laboratory methods. In addition, C-6 hydroxylated BA levels were measured by HPLC-HRMS, including unconjugated and taurine (T)- and glycine (G)-conjugated species (Table 1). Individual BA were separated by HPLC using a reversed-phase C18 column (Macherey-Nagel, Düren, Germany) and a kinetex pentafluorophenyl column (Phenomenex, Aschaffenburg, Germany). Quantification and characterization was achieved using a mass spectrometer Q Exactive™ MS/MS (Thermo Fisher Scientific, Waltham, MA) and a high-performance quadrupole precursor selection with high-resolution and accurate-mass (HR/AM) Orbitrap™ detection according to the method published by Amplatz 2017.14
Statistical analysis
Each patient characteristic is presented as median and interquartile range (IQR). For statistical analysis, continuous variables were analyzed by Mann–Whitney U-testing. Correlations were analyzed by Spearman’s rank correlation test. Statistical significance was defined as a p-value < 0.05. Statistical analysis was performed with IBM SPSS Statistics software 23.0.0 (IBM SPSS, Armonk, NY).
Results
FT neonates without sepsis showed detectable levels of tauro-GMCA- (TGMCA) and tauro-AMCA (TAMCA)
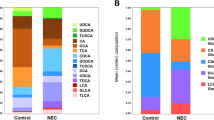
Reference values of C-6-hydroxylated ‘rare’ BA included tauro-, glyco-, and unconjugated α-(AMCA), β-(BMCA), and γ-(GMCA), ω-muricholic (OMCA) acid, and hyodeoxycholic acid (HDCA). In non-septic FT neonates (n = 47), the median BA level was 0.5 µmol/L (IQR: 0.3–1.3; Fig. 2; Table 2). In FT controls, TGMCA and TAMCA were the predominant C-6-hydroxylated BA species, although GMCA, BMCA, and GGMCA were also present (Fig. 3a). HDCA and its conjugates were below the detection limit. Looking at the total BA pool ‘typical’ primary BA were the dominant BA in all four groups (Supplemental Figure S1a–d).
Prematurity significantly influenced ‘rare’ BA levels
The influence of prematurity on ‘rare’ BA metabolism was investigated in a group of 22 non-septic PT neonates. In summary, C-6-hydroxylated BA levels in PT neonates were below the detection limit except for TAMCA, whose median concentration was 0.1 µmol/L (IQR: 0–0.2). In total, C-6-hydroxylated BA levels were significantly higher in non-septic FT neonates than in non-septic PT neonates (Fig. 2; p < 0.01). Interestingly, TAMCA was the only ‘rare’ BA found in healthy PT neonates (Fig. 3b). Unlike in non-septic FT neonates, GMCA, TGMCA, TOMCA, GGMCA, and BMCA were absent in non-septic PT neonates.
EOS FT neonates show alterations in ‘rare’ BA’ composition but not in levels
C-6-hydroxylated BA levels were determined in 20 FT neonates with diagnosed EOS. Interestingly, levels were comparable in FT neonates with EOS and in FT controls with 0.5 µmol/L (IQR: 0.3–1.3) and 0.6 µmol/L (IQR: 0.1–1.6), respectively. However, the ‘rare’ BA profile in EOS term neonates differed from that in healthy FT neonates: TOMCA was significantly higher in EOS (p < 0.01) and accounted for 95% of all C-6-hydroxylated BA (Fig. 3c). TAMCA was significantly lower in EOS (p < 0.01). TGMCA, GMCA, BMCA, and GGMCA, which were—in addition to TAMCA—the most abundant ‘rare’ BA in FT controls, were below the detection limit in EOS.
EOS in PT infants was marked by significantly increased ‘rare’ BA levels caused by a rise of TOMCA
The influence of EOS was investigated since ‘classical’ human BA levels were found to be significantly decreased in EOS.1 C-6-hydroxylated BA levels were determined significantly higher in 13 EOS PT neonates compared to PT controls (0.6 µmol/L [IQR: 0.2–1.5] vs. 0 µmol/L [IQR: 0.0–0.2]; p < 0.01). As in EOS FT neonates, the BA profile in EOS PT neonates included a significantly higher amount of TOMCA (p < 0.01) than did that of PT controls. Overall, TOMCA accounted for 72% of all ‘rare’ BA, followed by GBMCA (17%), TAMCA (8%), and BMCA (3%; Fig. 3d). TAMCA values—the only C-6-hydroxylated BA in PT controls—were significantly lower in EOS (p < 0.01).
TOMCA levels are independently associated with EOS
Last, we evaluated the autonomous potential of TOMCA as a biomarker in EOS. EOS biomarker are listed in Table 3. Multivariate regression analysis revealed that TOMCA levels were independent of EOS biomarkers CRP, PCT, IL-6, and bilirubin (r = 0.75, p = 0.85).
Discussion
In this study, we determined reference ranges of ‘rare’ C-6-hydroxylated BA for non-septic full term and PT neonates using highly sensitive HPLC-HRMS. We found that, in general, C-6-hydroxylated BA levels are higher in full term neonates than in neonates born PT. In addition, we sought to investigate whether EOS affects C-6-hydroxylated BA metabolism, as ‘classical’ human BA concentrations decrease in septic neonates.1 ‘Rare’ BA levels were found to be higher in EOS PT neonates than in controls. This was due to an increase in TOMCA.
In mice, C-6-hydroxylated BA are the common BA species. In human, their appearance is ‘rare’, but significant amounts have been isolated from materials obtained from patients with hepatobiliary diseases and from foetuses and neonates, especially from umbilical cord blood and amniotic fluid.4,5 In neonatal serum, data are missing. As our first aim, we studied non-septic full term neonates who presented with mean C-6-hydroxylated BA amounts of 0.5 µmol/L. These quantities, accounting for ~10% of classical human BA,1 served as reference values. The microbiome strongly influences BA pool size and composition. Studies of our ‘rare’ BA pool revealed TAMCA and TGMCA, both products of CDCA hydroxylation, as the major BA in non-septic full term neonates. CDCA is the main product of the ‘alternative’ pathway of BA synthesis, whereas the ‘classic’ pathway primarily produces CA. Although the alternative pathway is not the major route for human BA synthesis in human adults, it is the main pathway in the neonate. This is evident in the neonatal lack of CYP7A1, the rate-limiting enzyme of BA synthesis in the ‘classic’ pathway, or in the finding that severe neonatal cholestasis develops in infants with deficiency of CYP7B1, a key enzyme in the ‘alternative’ synthesis pathway (Setchell, 199815; Bove, 200016). Hence, CDCA synthesis via CYP7B1 might be the predominant pathway in our study group. This is in accord with the earlier studies in the fetus which showed that the predominant BA species is CDCA conjugated with T.17 Hence, this seems a likely origin for the T-conjugated CDCA derivatives TAMCA and TGMCA. Interestingly, TAMCA is a so-called ‘primary’ BA since synthesized in the liver. This accords to current literature since primary BA are the predominant BA in neonates, whereas classical human secondary BA are only found in small amounts.1 GMCA, however, is a secondary BA generated by the intestinal microbiota. A revolution in knowledge about the neonatal microbiome has included demonstration that gut colonization by bacteria starts in intrauterine life, well before delivery, increasing during birth and the first days of life.18,19 This microflora is essential for the generation of secondary BA and henceforward GMCA. Additionally, Back et al.6, reporting high amounts of GMCA in the meconium, suggested that the fetal pathway persists throughout early infancy. Hence, the presence of GCM probably reflects the existence of further pathways for ‘rare’ secondary BA synthesis in the fetal and neonatal period.
The synthesis of tri-hydroxylated BA TAMCA and TGMCA might be, besides the microbial influence, also based on a hepato-protective mechanism since hydroxylation enhances the polarity of BA, which both facilitates their elimination via the kidneys and lowers their cytotoxic potential.17 In fact, serum studies in adult patients with cholestatic liver disease revealed higher tri-hydroxylated BA levels than in controls, with BA profiles resembling those of sd neonates.3,4 Therefore, it is speculated that there are common metabolic pathways in neonatal and cholestatic liver; however, the exact pathways are still unclear.
As our second aim, we profiled BA in non-septic neonates born PT. TAMCA was the only C-6-hydroxylated BA found in small amounts, whereas TGMCA was absent. First, that C-6-hydroxylated BA levels were lower in PT neonates than in controls might be due to differences in BA metabolism, with a possible shift to the synthesis of other ‘rare’ BA. For instance, Wahlen et al.20 measured high amounts of tetrahydroxylated and ketonic BA in the urine of healthy term and PT infants. However, these BA species were not included in our study. Secondly, the absence of TGMCA might be explained by differences in the microbiota between full and PT neonates. Studies in neonatal fecal specimens showed that gut-related bacterial diversity is less in PT neonates than in those born at term.21 As foetuses mature, they swallow large amounts of amniotic fluid, particularly during the third trimester of pregnancy. It seems likely that reduced microbial diversity in a PT neonate’s gut microbiota yields fewer ‘rare’ secondary BA.22 Additionally, nutrition has a major role in early colonization of the neonatal gut microbiota. Milk of PT mothers differs from that of full term mothers. For example, PT milk seems to have a different mix of oligosaccharides; this could influence microbial growth.23 In our study, we also investigated possible differences between breast milk- and formula-fed infants; however, none was detected (data not shown).
As a third aim, we investigated the influence of EOS on ‘rare’ BA metabolism. It is well known that BA levels rise in septic adults due to a cholestatic effect of cytokines.24 We aimed to examine the influence of sepsis, in our case EOS, and of cytokines in excess on BA metabolism in the very young infant. We have earlier shown that classical human BA in FT and PT neonates with EOS were significantly lower than in age-matched controls, possibly due to endotoxin suppression of de novo BA synthesis. In our study, levels of the C-6-hydroxylated BA TOMCA significantly increased in all septic neonates independent of prematurity or maturity status. Additionally, EOS PT neonates presented with a more miscellaneous BA profile than that of PT controls with TOMCA as the clearly predominant ‘rare’ BA species. Hence, TOMCA may represent an important BA in EOS. Studies in rats showed that OMCA might be a result of the 6-isomerase conversion of BMCA, a primary BA, and thus might be considered a secondary BA.25 Other authors suggest that rat hepatocytes contain a 7-β-hydroxylase that can convert HDCA, a bacterial metabolite and hence a secondary BA, into OMCA, which is then often referred as a ‘tertiary’ BA.25 Our results let us speculate that EOS may enhance the conversion of either BMCA or HDCA into OMCA. However, these assumptions await further investigation in future studies. Although the major pathway for formation of TOMCA and the purpose of its rise in EOS is still unknown, TOMCA was identified as an independent factor associated with EOS. In this patient group assessments of TOMCA may be of clinical value in the future.
In summary, our study describes ‘rare’, C-6 hydroxylated BA in serum of neonates. Differences among the BA pools of non-septic or septic neonates, born full term or PT, might be explained by variations in microbiome diversity, nutrition, and expression of enzymes for BA synthesis. In EOS, TOMCA seems to be a prominent BA. Future studies need to clarify underlying physiology and diagnostic potential.
References
Zohrer, E. et al. Serum bile acids in term and preterm neonates: a case-control study determining reference values and the influence of early-onset sepsis. Medicine 95, e5219 (2016).
Tagliacozzi, D. et al. Quantitative analysis of bile acids in human plasma by liquid chromatography-electrospray tandem mass spectrometry: a simple and rapid one-step method. Clin. Chem. Lab. Med. 41, 1633–1641 (2003).
Batta, A. K. et al. Characterization of serum and urinary bile acids in patients with primary biliary cirrhosis by gas-liquid chromatography-mass spectrometry: effect of ursodeoxycholic acid treatment. J. Lipid Res. 30, 1953–1962 (1989).
Shoda, J. et al. Similarity of unusual bile acids in human umbilical cord blood and amniotic fluid from newborns and in sera and urine from adult patients with cholestatic liver diseases. J. Lipid Res. 29, 847–858 (1988).
Nakagawa, M. & Setchell, K. D. Bile acid metabolism in early life: studies of amniotic fluid. J. Lipid Res. 31, 1089–1098 (1990).
Back, P. & Walter, K. Developmental pattern of bile acid metabolism as revealed by bile acid analysis of meconium. Gastroenterology 78, 671–676 (1980).
Stoll, B. J. et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 126, 443–456 (2010).
Simonsen, K. A., Anderson-Berry, A. L., Delair, S. F. & Davies, H. D. Early-onset neonatal sepsis. Clin. Microbiol. Rev. 27, 21–47 (2014).
Koenig, J. M. & Keenan, W. J. Group B streptococcus and early-onset sepsis in the era of maternal prophylaxis. Pediatr. Clin. North. Am. 56, 689–708 (2009).
Stoll, B. J. et al. Early onset neonatal sepsis: the burden of group B Streptococcal and E. coli disease continues. Pediatrics 127, 817–826 (2011).
Srinivasan, L. & Harris, M. C. New technologies for the rapid diagnosis of neonatal sepsis. Curr. Opin. Pediatr. 24, 165–171 (2012).
Hofer, N., Muller, W. & Resch, B. Non-infectious conditions and gestational age influence C-reactive protein values in newborns during the first 3 days of life. Clin. Chem. Lab. Med. 49, 297–302 (2011).
Hornik, C. P. et al. Early and late onset sepsis in very-low-birth-weight infants from a large group of neonatal intensive care units. Early Hum. Dev. 88, S69–S74 (2012).
Amplatz, B. et al. Bile acid preparation and comprehensive analysis by high performance liquid chromatography-high-resolution mass spectrometry. Clin. Chim. Acta 464, 85–92 (2017).
Setchell KD, Schwarz M, O'Connell NC, et al. Identification of a new inborn error in bile acid synthesis: mutation of the oxysterol 7alpha-hydroxylase gene causes severe neonatal liver disease. J Clin Invest. 1998;102:1690-1703.
Bove KE, Daugherty CC, Tyson W, et al. Bile acid synthetic defects and liver disease. Pediatr Dev Pathol. 2000;3:1-16.19.
Colombo, C., Zuliani, G., Ronchi, M., Breidenstein, J. & Setchell, K. D. Biliary bile acid composition of the human fetus in early gestation. Pediatr. Res. 21, 197–200 (1987).
Jimenez, E. et al. Is meconium from healthy newborns actually sterile? Res. Microbiol. 159, 187–193 (2008).
DiGiulio, D. B. et al. Microbial prevalence, diversity and abundance in amniotic fluid during preterm labor: a molecular and culture-based investigation. PLoS ONE 3, e3056 (2008).
Wahlen, E. & Strandvik, B. Effects of different formula feeds on the developmental pattern of urinary bile acid excretion in infants. J. Pediatr. Gastroenterol. Nutr. 18, 9–19 (1994).
Madan, J. C. et al. Gut microbial colonisation in premature neonates predicts neonatal sepsis. Arch. Dis. Child. Fetal Neonatal Ed. 97, F456–F462 (2012).
Scholtens, P. A., Oozeer, R., Martin, R., Amor, K. B. & Knol, J. The early settlers: intestinal microbiology in early life. Annu Rev. Food Sci. Technol. 3, 425–447 (2012).
De Leoz, M. L. et al. Lacto-N-tetraose, fucosylation, and secretor status are highly variable in human milk oligosaccharides from women delivering preterm. J. Proteome Res. 11, 4662–4672 (2012).
Trauner, M., Fickert, P. & Stauber, R. E. Inflammation-induced cholestasis. J. Gastroenterol. Hepatol. 14, 946–959 (1999).
Sacquet, E. C. et al. Bacterial formation of omega-muricholic acid in rats. Appl. Environ. Microbiol. 37, 1127–1131 (1979).
Acknowledgements
The excellent technical assistance of Maria Schäffer is gratefully acknowledged. We thank A.S. Knisely for helpful comments on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Zöhrer, E., Meinel, K., Fauler, G. et al. Neonatal sepsis leads to early rise of rare serum bile acid tauro-omega-muricholic acid (TOMCA). Pediatr Res 84, 66–70 (2018). https://doi.org/10.1038/s41390-018-0007-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-018-0007-y