Abstract
The bladder supports a diversity of macrophage populations with functional roles related to homeostasis and host defense, including clearance of cell debris from tissue, immune surveillance, and inflammatory responses. This review examines these roles with particular attention given to macrophage origins, differentiation, recruitment, and engagement in host defense against urinary tract infections (UTIs), where these cells recognize uropathogens through a combination of receptor-mediated responses. Time is an important variable that is often overlooked in many clinical and biological studies, including in relation to macrophages and UTIs. Given that ageing is a significant factor in urinary tract infection pathogenesis and macrophages have been shown to harbor their own circadian system, this review also explores the influence of age on macrophage functions and the role of diurnal variations in macrophage functions in host defense and inflammation during UTIs. We provide a conceptual framework for future studies that address these key knowledge gaps.
Similar content being viewed by others
Introduction
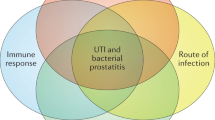
Macrophages have important roles during urinary tract infections (UTIs), influencing host colonization, pathology, and disease outcomes. As innate immune sentinels, these cells detect pathogen- and host-derived danger signals associated with immunological perturbations during UTIs, triggering host-protective inflammation, coordinating the recruitment of neutrophils for antimicrobial defense, and directly destroying uropathogenic Escherichia coli (UPEC) and other pathogens that cause UTIs. In contrast to these beneficial effects, macrophages can, in some circumstances, provide an intracellular niche for bacterial survival during UTIs and can also drive pathology through dysregulated inflammatory responses. There is, therefore, much to be gained from studying macrophage phenotypes and functions in the context of UTIs.
Developmental processes, ageing, and circadian rhythm can all profoundly influence macrophage functions. In this review, we consider how time influences macrophage biology and the implications of this for UTIs. We discuss how developmental processes influence macrophage ontogeny in the context of the bladder, as well as the impacts of circadian rhythm and ageing on the functions of macrophages and the urinary tract. We aim to provide a conceptual framework for future studies that address key knowledge gaps in these emerging research areas in relation to UTIs. The majority of studies referenced herein were performed in mice, but those carried out with human cells or tissues are specifically described as such. We begin with a broad overview of macrophage phenotypes, functions, and heterogeneity, particularly in relation to those in the bladder.
Phenotypes, functions, and heterogeneity of macrophages
Tissue-resident macrophages are phenotypically and functionally diverse. In the past, immunologists and cell biologists often simplified macrophage populations into two broad categories for convenience, namely pro-inflammatory (M1) and anti-inflammatory (M2) macrophages. The classical definition of M1 macrophages posits these as being derived in the presence of interferon-γ and lipopolysaccharide (LPS)1, whereas M2 macrophages are generated in the presence of Th2-associated cytokines such as IL-4 and/or IL-13 that suppress inflammation and promote tissue repair2,3. The M1/M2 paradigm is now widely regarded by many innate immunologists as being overly simplistic4, as exemplified by a transcriptome-based study that identified a spectrum of human macrophage activation states, depending on the precise nature of the stimulus5. Instead, we now appreciate that tissue-resident macrophages are protean cells that are able to modify their precise phenotypes and functions according to numerous factors in the local microenvironment6. These include cell–cell interactions, microbial products, extracellular matrix components, cytokines, chemokines, and other soluble factors6,7. Additional factors that influence heterogeneity of bladder macrophage populations include the developmental age and the inflammatory status. As expanded on below, tissue macrophages, including bladder macrophages, originate from three distinct sources, namely the yolk-sac, the fetal liver, and the bone marrow, throughout the lifespan of the mouse8,9. The longevity, self-renewal and/or replacement of fetal-derived macrophages with monocyte-derived macrophages varies between tissues, with each organ having its own dynamic. In the case of the bladder, infection also influences this dynamic and thus the heterogeneity of bladder macrophages. For example, alterations in bladder macrophage populations occur during infections, as demonstrated in UTIs10 and schistosomiasis11, with the death of some resident macrophages resulting in the recruitment of monocyte-derived macrophages to replace these cells. A plethora of factors including genetics, macrophage ontogeny, age, microbiome, and infectious agents encountered will undoubtedly influence the phenotypes and functions of bladder-resident macrophage populations during UTIs. This heterogeneity could potentially enable the diversification of macrophage functions in the bladder during homeostasis and UTIs, a concept that is beginning to be explored as described below.
In adult mice, the heterogeneity of macrophage populations in the bladder has been demonstrated through the use of transcriptomic and flow cytometric analyses9,12. On the basis of differential cell surface CX3CR1 expression, two bladder macrophage populations residing in the muscle (MacM, CX3CR1low) and the lamina propria (MacL, CX3CR1high) were identified9 (Table 1, kidney macrophage populations shown for comparison). Transcriptomic analysis demonstrated three populations, including the two populations identified by flow cytometry, as well as a third population expressing CXCL13 in older mice12. Each of these macrophage populations respond to immunological stimuli differently. In response to a UTI, Lacerda Mariano et al.9 showed that MacM macrophages had the capacity to phagocytose bacteria with a high efficiency and transitioned to an anti-inflammatory phenotype, whereas MacL macrophages died. Technological developments in single-cell sequencing approaches, along with the increased capacity of multiparameter flow cytometry, and simultaneous phenotypic and transcriptomic measurements, will likely reveal additional sub-populations of macrophages within the previously described populations and potential differences in their functional capacities, as has been observed in other tissues including the lung, liver and the kidney13,14,15.
Prenatal origins, recruitment, and replenishment of tissue-resident macrophages in the bladder
Tissue-resident macrophages are seeded during embryonic development and have the capacity to self-maintain independently of bone marrow-derived macrophages in adulthood7. Prenatal macrophages are initially derived from the yolk-sac independently of the transcription factor c-Myb16, and later during embryogenesis from early erythro-myeloid progenitors dependent on c-Myb that initially seed the fetal liver17, giving rise to adult macrophage populations. Fate mapping studies have demonstrated that microglia and Langerhans cells are embryonically-derived, and subsequent fate mapping studies have demonstrated yolk sac-derived macrophages are present in the kidney, liver (Kupffer cells), pancreas, lung, and spleen16. This demonstrated a clear prenatal contribution to these populations in young adult mice under homeostatic conditions16,18. Each of the macrophage populations have unique tissue-specific transcription factors instructing or associated with their development (Table 2); however, at this time there have been no unique transcription factors identified for bladder macrophages.
Recent studies have revealed that bladder macrophages in adult mice are derived from hematopoietic stem cells (HSC), rather than the self-renewing macrophage populations derived from the yolk-sac. Lacerda Mariano et al. utilized Cdh5-CreERT2 Rosa26tdTomato transgenic mice to identify the contribution of each stage of the hemopoietic progenitor cell development by labeling the yolk-sac progenitors and the HSC9,19. Yolk sac-derived macrophages were found in the embryos (E16.5) and newborn mice, however this specific macrophage population was reduced in the bladder and was almost absent in mice older than 12 weeks. The kinetics of this replacement have not been clearly defined for many tissues and this is even less clear for the bladder, both prenatally and postnatally. During the final stages of embryonic development and in newborn mice, HSC-derived macrophages are increased and these cells contribute to the adult MacM and MacL bladder macrophage populations9. These findings were confirmed using the Flk2/Flt3 mouse model, where HSC-derived macrophages and monocytes, but not yolk sac-derived macrophages, were labeled20. The bladder macrophage population included fetal HSC-derived macrophages and bone marrow monocyte-derived macrophages (Fig. 1), but functional differences between macrophages from the two different origins remain to be elucidated.
A schematic view of macrophage populations in the mouse through development from embryo to an aged mouse. Yolk sac-derived macrophages that are initially present in the bladder are replaced by macrophages derived from the fetal liver during the latter stages of embryogenesis, then bone marrow-derived macrophages after birth. Additional macrophage sub-populations are present in the bladders of aged mice.
Tissue maintenance and clearance of debris
One key role of tissue-resident macrophages is the clearance of debris and apoptotic cells, either for the maintenance of tissue homeostasis or following inflammation and the resolution of infection21,22. The clearance of debris derived from the different tissues or circulation is strictly controlled and facilitated by a distinct repertoire of receptors, opsonins, and transcription factors in macrophages that are unique to each tissue and that have been well documented (www.immgen.org) in tissues such as the spleen, bone marrow, intestine, liver, and lungs23. Analysis of macrophages in these different tissues revealed an increased expression of CD206 and CD163 in the steady state, as well as an anti-inflammatory transcriptomic profile23. Apoptotic cells have been shown to promote their own clearance and induce immune tolerance through the activation of the nuclear receptor LXR (NR1H3), a mechanism that limits inflammation24,25.
Similar to other tissues, the bladder includes a macrophage population (MacM subset) that has been shown by transcriptomics to have increased expression of the gene Mcr1 that encodes CD2069,23. The role of MacM and MacL macrophages in tissue development, homeostasis, and repair, as well as clearance of apoptotic cells such as damaged uroepithelial cells after exposure to infectious agents, toxins, and/or carcinogens26, still needs to be fully explored in the bladder. The MacM macrophage gene expression profiles are linked to pathways that are more homeostatic including endocytosis and phagocytosis, mineral absorption and iron metabolism9. As noted above, the subset of macrophages referred to as MacL has been shown to reside in sub-urothelial space9. Although the homeostatic functions of these macrophages are unclear, one of the roles could be supporting the integrity of the urothelium. The urothelial environment can be influenced by IL-6 that promotes the relocation of macrophages via CX3CL1. This pathway can help protect and potentially regenerate the urothelium following immunological injury caused by UTIs27, and it is possible that MacL macrophages are involved in this process. Resident macrophages in the kidney play important roles in tissue homeostasis and development, supporting ureteric bud branching and vascular development, as well as removing dead cells28,29. Alveolar macrophages help maintain the health of the lung, playing critical roles in immunosurveillance and lipid surfactant catabolism to prevent abnormal lipid accumulation that can induce oxidized lipid lung inflammation30. In other tissues such as the spleen and liver, a sub-population of macrophages clear cellular debris and material derived from the blood to maintain tissue homeostasis via CD206 and CD16323. Since these cell surface receptors are also expressed by MacM macrophages in the bladder9, it is possible that this sub-population of bladder macrophages play a similar role in the clearance of debris.
The role of macrophages in immune surveillance and inflammation during UTIs
Irrespective of their developmental pathway, macrophages play multifaceted roles in both host defense and colonization during UTIs. These cells are sentinels, recognizing invading uropathogens through families of pattern recognition receptors (PRRs), such as toll-like receptors (TLRs), C-type lectin receptors and inflammasome-forming nod-like receptors (NLRs), that detect both pathogen-associated molecular patterns (PAMPs) and danger-associated molecular patterns (DAMPs)31,32,33. TLR4, which detects LPS from Gram-negative bacteria, is required for innate defense to UPEC34, as is CD14 that presents LPS to TLR435. UPEC recognition by macrophages can also occur via interactions between FimH (an attachment protein) and TLR436, enabling antimicrobial and inflammatory responses to be engaged. For example, inducible secretion of IL-6 by macrophages results in both an increase in antimicrobial peptide production and alterations to iron homeostasis to facilitate UPEC clearance10,37.
Other inflammatory mediators released by macrophages contribute to leukocyte recruitment for host defense during UTIs. IL-8 plays an important role in neutrophil trafficking and transepithelial neutrophil migration in the urothelium38, with urine IL-8 levels correlating with pyuria in UTIs39,40. A seminal study in the field also revealed how crosstalk between different bladder macrophage subsets orchestrates recruitment of host-protective neutrophils to the infected bladder in a mouse model of UTI38. During UPEC infection, Ly6C−ve resident bladder macrophages recruit both neutrophils and Ly6C+ve monocytes by secreting the chemokines CXCL1 and CCL238. The newly recruited monocyte-derived macrophages secrete TNF, which induces resident Ly6C−ve macrophages to secrete CXCL2, causing neutrophils to produce matrix metalloproteinase 9 (MMP9) and facilitate bacterial clearance41,42. Macrophages can subsequently temper neutrophil responses by phagocytosing apoptotic neutrophils to enable the early resolution of inflammation43. Bladder macrophages have central roles in initiation of inflammation, neutrophil recruitment, and inflammation resolution during UTIs. The recruitment of monocytes that will become resident inflammatory macrophages38,44,45,46 can dominate the areas of inflammatory insults9,46. These recruited cells have the potential to become the majority of the resident macrophage population, either by continued recruitment or by self-renewal.
The interaction between bladder macrophages and UPEC is extremely complex. Previous studies showed that removal of the bladder-resident macrophage population prior to an experimental UTI infection altered the distribution of UPEC but did not impact the clearance of a primary UPEC infection46. UTIs induce an inflammatory response in bladder macrophages47,48, but UPEC are genetically and phenotypically diverse; this diversity profoundly impacts the types of innate immune responses that are generated, as well as UPEC clearance versus colonization. For example, UPEC strains that produce the α-hemolysin toxin trigger activation of the NLRP3 inflammasome49,50, a PRR that engages inflammatory caspases to initiate both the processing and secretion of IL-1β, as well as pro-inflammatory pyroptotic cell death51. Inflammasome-dependent IL-1β release facilitates UPEC clearance48, although variation in α-hemolysin expression between different UPEC strains can influence inflammasome-dependent and -independent responses, as well as host protection and susceptibility52,53. Whereas α-hemolysin-producing UPEC strains kill macrophages, some UPEC strains lacking this toxin can actually survive within these cells via mechanisms that avoid zinc poisoning (see below)54, or by subverting intracellular trafficking pathways that are poorly understood55. This diversity in UPEC and its interactions with innate immune cells highlights that the role of tissue-resident macrophages in the generation of an inflammatory response to a specific immunological insult will depend on the precise nature56 and the extent57 of the challenge.
Macrophages in the lamina propria of the bladder are particularly prone to cell death, as a significant reduction in the numbers of macrophages was observed during UTI in an experimental model9. Cells of the urothelium, including uroepithelial cells, can produce cytokines of the IL-6 family, IL-8 families, and IL-10 families, in response to UTIs58,59,60,61. Although IL-6 has been shown to promote macrophage survival and activity in other models of injury62,63,64, disruptions in the cytokine microenvironment caused by exfoliation may have an influence on macrophage survival. Studies in other tissue injury models have shown that macrophage populations may be replenished either by self-renewal of tissue-resident macrophages or by recruitment of bone marrow-derived monocytes, which then differentiate into tissue-resident macrophages65,66. Whether this is the case in the bladder mucosa following a UTI is currently under investigation.
Relocation of tissue macrophages to lymphatic tissues is an alternative fate of activated macrophages. This has been suggested for macrophages from the peritoneal cavity during peritonitis67, and for the disappearance of alveolar macrophages from bronchoalveolar fluid during influenza infection68,69. Analysis of the selective expression of markers, including Siglec-F, supports the view that alveolar macrophages migrate from the lung to the draining lymph node, potentially carrying antigens for priming of the host’s adaptive immune response69. At this time, it is unclear if bladder macrophages relocate to the local draining lymph nodes following a UTI, upon phagocytosing bacteria, or in response to other immunological insults. The fate of bladder macrophages in response to either an immunological or metabolic challenge will need to be addressed experimentally using specific fate mapping approaches and the labeling of highly purified cells. Studies designed to determine whether macrophages traffic antigens from the inflamed bladder to lymph nodes will also present significant challenges, as macrophages degrade antigens much more rapidly than dendritic cells70.
Autophagic regulation in macrophages upon UPEC infection
Bacterial proteins influence the macrophage response and early studies showed that FimH-positive E. coli are found in different compartments to FimH-negative E. coli71,72. Baorto et al. found that compartments containing FimH-positive E. coli were not acidified as quickly, did not contain as many reactive oxygen species, and were smaller than those compartments that contained FimH-negative E. coli72. This suggested that FimH-dependent phagocytosis results in an altered initial compartment. Subsequently, Amer et al. showed that FimH-positive E. coli entered into cells and were found in vacuoles that colocalized with lipid raft markers and quickly recruited two autophagy proteins, first ATG7 and then ATG8 (LC3)71. Thus, autophagy proteins appear to be recruited to compartments containing UPEC that have entered macrophages through FimH-dependent phagocytosis and may represent LC3-associated phagocytosis (LAP) or a similar process73. This may be a conserved method to protect the host cell from pathogens that avoid canonical phagocytosis, by targeting bacteria that enter the cell in other ways for degradation. That said, some UPEC strains can survive in macrophages54,55. Of note, most studies examining the uptake of FimH-positive or -negative E. coli and intersection with autophagy were performed in bone marrow-derived macrophages (BMDM) and not bladder macrophages. Since bladder-resident macrophages have been exposed to a specific milieu that will not be preserved in BMDM generated in vitro, studies using macrophages isolated from the bladder are now required to better understand their roles during UTIs.
Autophagy represents one host pathway for controlling macrophage responses to UPEC. Studies using BMDM demonstrated that autophagy pathway components can affect how UPEC is taken up by macrophages, as well as how macrophages respond to this pathogen. For example, the autophagy protein, ATG16L1, following recognition of UPEC, upregulates the NLRP3 inflammasome response in macrophages. Loss of ATG16L1 in macrophages enables rapid clearance of UPEC infections via an IL-1β-mediated hyperinflammatory response48. ATG16L1 appears to limit IL-1β signaling by controlling autophagosomal and proteasomal degradation of p6274. This implicates lysosomal degradation and autophagy in constraining the IL-1β response and thus the clearance of UPEC (Fig. 2). Given the detrimental effect on tissue integrity of excessive inflammation, there may be a delicate balance wherein macrophages attempt to degrade intracellular UPEC and secrete IL-1β into the local environment, with autophagic regulation limiting the extent of inflammatory response. Such a controlled orchestration has recently been shown in uroepithelial cells in response to UPEC infection, wherein infection-induced oxidative stress activates autophagic flux and inflammatory responses transiently to expel bacteria and induce an antioxidant response75. Macrophage responses may be similarly regulated by UPEC50 or the host76. Macrophage hyperactivation could result from disturbance of the balance between inflammasome activation, autophagy, and IL-1β secretion. As noted above, macrophage migration to the site of injury is, in part, designed to limit tissue damage and phagocytose cell debris. Autophagy-mediated intrinsic fine tuning of macrophage responses to infection and/or injury may be essential for macrophages to perform their functions in a tissue-specific manner.
Some of the key events initiated in macrophages upon UPEC infection and/or phagocytosis are shown. ATG16L1 is recruited to internalized UPEC, with bacteria being engulfed into autophagosomes via autophagy. TLR4 homodimers recognize UPEC and trigger pro-inflammatory signaling, including NF-κB activation. TLR signaling upregulates inflammasome components, with α-hemolysin-positive UPEC strains triggering inflammasome activation and caspase-1-dependent processing of pro-IL-1β. This enables secretion of mature IL-1β via membrane pores. TLR signaling also turns on the zinc toxicity response in macrophages, likely via regulated expression of both SLC30A zinc exporters and SLC39A zinc importers, with UPEC strains that survive in macrophages effectively evading this antimicrobial pathway. NF-κB activation increases the production of the pro-inflammatory cytokine IL-6, which modulates intracellular iron levels by increasing the production of the ferritin-iron intracellular complex and regulating levels of LCN-2 and ferroportin. Ferritin and iron form an intracellular complex, and LCN-2 maintains optimal iron levels in the cell by exporting excess iron out. An intrinsic clock controls the capacity of macrophages to sense and respond to UPEC, with circadian control of IL-6 production likely to be particularly important in macrophage/UPEC interactions and host defense.
Macrophage control of iron metabolism during infections
Physiological iron levels must be maintained for homeostasis and immune response upon infection, and macrophages play key roles in this control77,78, both via iron uptake and intracellular storage of “free” iron. Macrophages limit the release of free iron when exposed to hepcidin, a peptide hormone produced by hepatocytes in response to a range of stimuli including bacterial infection79,80. This would appear to be a feedback loop as macrophage-derived pro-inflammatory cytokines such as interleukin 6 (IL-6) drive hepcidin expression in hepatocytes thus further reducing iron availability81,82,83,84. Furthermore, hepcidin is a negative regulator of ferroportin85,86,87, aiding in preventing the release of iron by macrophages. Finally, the release of free iron by macrophages in response to an infection is supported by the decreased surface expression of CD16378 and TFR178,86,88. Macrophages produce IL-6 as a first response to UPEC89,90,91, and the IL-6—hepcidin feedback loop is particularly important in the host response to UPEC, since IL-6 signaling is necessary for macrophages to limit the growth of UPEC in the presence of excess iron10. Consistent with this, UPEC has developed mechanisms to limit innate immune cell-mediated IL-6 production as a host evasion strategy92,93. However, the role of hepcidin in UPEC infections, as well as the molecular and cellular mechanisms underlying IL-6 modulation of iron responses in the bladder, remain to be elucidated.
In addition to iron retention, macrophages can limit bacterial access to extracellular free iron through the production of lipocalin-2 (LCN-2), a molecule that binds to both host iron-bound siderophores and bacterial iron-bound siderophores. LCN-2 can also limit bacterial survival by inhibiting macrophage iron retention as has been demonstrated with pathogenic E. coli and Salmonella enterica serovar Typhimurium (S. Typhimurium) within the host94,95,96, and it particularly reduces survival of bacteria within macrophages88,97,98. In addition to limiting bacterial access to iron, LCN-2 can promote bacterial clearance through a number of other mechanisms. These mechanisms include increasing the recruitment of innate immune cells in response to infection, promoting inflammation, promoting macrophage activation, and inhibiting the expression of anti-inflammatory cytokines that can support bacterial growth98,99,100 (Fig. 2). LCN-2-mediated cytokine regulation and iron regulation may significantly affect host response and recovery from a UTI, since LCN-2 and hepcidin have been shown to be produced during the pathogenesis of upper UTIs101,102. Furthermore, UPEC is known to access iron within bladder epithelial cells103,104 by using LCN-2-resistant siderophores96,99,105. However, it remains unclear what role macrophage iron regulation might play in the host response to UPEC.
Macrophage-mediated zinc poisoning
In addition to iron, zinc also has a critical role during infections. It controls inflammation and host defense96, and innate immune cells can both sequester essential zinc to limit microbial growth106,107 and deliver toxic levels of zinc to intracellular bacteria as part of their antimicrobial arsenal108. These opposing mechanisms of zinc utilization by the innate immune system appear to apply to UPEC, with this pathogen requiring both zinc acquisition systems for bladder and kidney colonization109, as well as resistance to zinc toxicity for dissemination in an intraperitoneal challenge model54. One of the first studies to characterize macrophage-mediated zinc poisoning showed that the professional intramacrophage pathogen Mycobacterium tuberculosis resists this antimicrobial response in human macrophages110. Subsequent studies have revealed that both S. Typhimurium111, as well as a UPEC strain that can survive in macrophages54, evade macrophage-mediated zinc toxicity. The mechanisms by which UPEC does so are unknown and will require a better understanding of molecular processes used by macrophages to engage this pathway. Although these mechanisms are currently not well understood, TLR-inducible expression of the zinc transporter SLC30A1 appears to be involved in mediating the macrophage zinc toxicity response112.
Circadian dynamics in macrophages during infection
Circadian rhythms are 24-hour (h) cycles of physiological activities orchestrated by the intrinsic property of the circadian clock. These circadian rhythms contribute to changes in organismal behavior, metabolism and immune functions to enable an anticipatory adaptation to changes in the environment, including the day/night cycle. In mammals, light signals activate receptors in the retina, which then transmit this information to the central clock residing in the suprachiasmatic nuclei (SCN) in the hypothalamus (Fig. 3a)113. Subsequently, the central clock helps to synchronize cells in the periphery including macrophages, which also exhibit robust cell-autonomous circadian rhythms114. These rhythms are entrained by various signals and stimuli that act via a combination of neural circuits and humoral cues115, including hormones such as glucocorticoids.
a Zeitgebers such as light, temperature and food synchronize the central clock in the suprachiasmatic nucleus (SCN), which in turn synchronizes all peripheral clocks present in the body. The clock comprises of interconnected transcriptional feedback loops, with heterodimers of the transcription factors brain and muscle ARNT-like 1 (BMAL1) and circadian locomotor output cycles protein kaput (CLOCK) activating the expression of period (Per) and cryptochrome (Cry) genes. PER and CRY represent the negative arm of circadian control, whereby they form complexes to inhibit the activity of BMAL1–CLOCK and hence their own expression (loop 1). REV-ERBα/β and retinoid-related orphan receptor (ROR) α/β/γ alternatively regulate RORE promoter elements, which includes Bmal1 and Nfil3 (loop 2). NFIL3 and DBP can alternatively regulate-D-box promoter elements such as retinoid-related orphan receptor (ROR) α/β/γ (loop 3). All clock products from each of the loops can translocate back into the nucleus to either activate or repress these loops. b In mice, circadian rhythm influences susceptibility to various pathogens, cytokine secretion and immune cell trafficking. When mice transition into the active phase, the immune system is primed to respond to infection. In contrast, during the resting phase, immune functions are dampened and susceptibility to infections is increased. c Disrupted host circadian rhythm can interrupt both host immune system and urinary tract functions (i.e., increased voiding and impaired ability to concentrate urine). This is predicted to provide an environment that favors host colonization by UPEC. UPEC, in turn, may also reciprocally influence host circadian rhythms.
At the molecular level, the circadian rhythm is generated from interlocked rhythmic transcription-translation feedback loops comprised of several core clock components (Fig. 3a). Central to this process are the transcription factors circadian locomotor cycles protein kaput (CLOCK), brain and muscle ARNT-like 1 (BMAL1), and neuronal PAS domain-containing 2 (NPAS2)116. These proteins form heterodimers (CLOCK-BMAL1 and NPAS2-BMAL1) and act on E-box elements on clock-controlled genes (CCGs), namely Period (Per1, Per2, Per3)117 and Cryptochrome (Cry1, Cry2) genes118. Within the nucleus, PER-CRY complexes repress the activity of BMAL1 heterodimers and remove it from the E-box119. As PER and CRY proteins become degraded through ubiquitin-dependent pathways, BMAL1 activity is restored and the cycle starts again. In a second feedback loop, BMAL1 activates the transcription of the nuclear receptors REV-ERB(α/β), which compete with the retinoic acid-related orphan receptors (ROR) (α/β/γ) for binding to a ROR response element (RORE) within the Bmal1 promoter region120,121. REV-ERBs inhibit, while RORs activate, Bmal1 transcription. The clock regulates circadian clock-controlled transcription factors like the PAR-domain basic leucine zipper (PARbZip) transcription factors, namely D-box binding protein (DBP), thyrotroph embryonic factor (TEF) and hepatic leukemia factor (HLF)122. These compete with the nuclear factor, interleukin 3 regulated (NFIL3) to bind to D-box containing promoters. PARbZip proteins activate circadian clock-regulated gene expression, whereas NFIL3 has the reverse effect123. PARbZip transcription factors regulate important physiological functions through the regulation of the expression level of rhythmic genes124,125. Together, this tripartite system, involving CLOCK, REV-ERB(α/β), and PARbZip transcription factors, regulates the transcription of most circadian clock-controlled genes (Fig. 3a).
This molecular circuitry is cell-autonomous and drives the cyclic gene expression program in most cells of the organism, including many immune cells like T cells, B cells, natural killer cells, and macrophages114. In particular, the rhythmic transcriptional outputs generated by the cell intrinsic clock regulates ~8% of the macrophage transcriptome, including the expression of pattern recognition receptors, inflammatory mediators, and regulators of cell trafficking126. In the next part of the review, we evaluate the existing literature on diurnal variations in macrophage functions such as engagement of pathogen-sensing systems and cytokine secretion. We also discuss how the circadian system influences host responses to infection and normal urinary tract function. Our goal is to provide a broad overview on aspects of circadian biology that are likely relevant to UPEC infections. This is an area that is yet to be explored in detail experimentally but is likely to be important for host protection versus host colonization during UTIs.
Circadian rhythm and pathogen sensing by macrophages
For experimental studies, the time at which the synchronizing signal from light turns on and off is defined as zeitgeber time (ZT), with ZT0-12 (light on) and ZT12-24 (light off) denoted as the inactive and active phase in nocturnal animals, respectively. As noted above, macrophages detect pathogens through families of PRRs, including TLRs. UPEC can be recognized by several TLRs, including TLR2, TLR4, TLR5, TLR11, and likely also TLR9127. For example, genetic deletion of Tlr4, Tlr5 and Tlr11 increases host susceptibility to UTIs128,129,130. Interestingly, Silver et al. showed that mRNA levels of Tlr4 in splenic macrophages display rhythmic oscillations, peaking at ZT15. Tlr2 and Tlr6 mRNA levels were also rhythmically regulated in splenic macrophages, peaking at ZT14131. Thus, it is likely that a macrophage-intrinsic circadian clock influences pathogen sensing by innate immune cells. Furthermore, although Tlr5 mRNA expression did not oscillate in splenic macrophages, significant daily variations in Il6 and Il1b expression were observed after challenge with the TLR5 agonist flagellin131. This suggests that circadian control may influence TLR signaling responses. TLR9, an endolysomal receptor that senses bacterial and viral DNA, is also directly impacted by the circadian clock. In a TLR9-dependent mouse cecal ligation and puncture (CLP) model of sepsis, mice that underwent CLP at the peak of TLR9 expression (ZT19) displayed exacerbated inflammation and a sepsis-like phenotype by comparison to mice that underwent CLP at ZT7 (TLR9 nadir)132. Given that several of these TLRs are tasked with sensing UPEC, it is likely that circadian rhythm influences host inflammatory responses and colonization during UTI. Studies in other bacterial infection models support this view (Fig. 3b).
As highlighted above, some UPEC strains trigger inflammasome activation in macrophages and other cell types. The most widely studied inflammasome is NLRP3133, which has important roles in inflammatory responses during experimental UTI48. UPEC-mediated inflammasome activation, IL-1β processing and release, and pyroptotic cell death can all be triggered by the toxin α-hemolysin50,53. However, many UPEC strains do not encode this toxin in their genome134, so the involvement of the NLRP3 inflammasome pathway in inflammation and host colonization during UPEC infection is likely to depend on whether the strain in question produces this toxin. It was recently demonstrated that Nlrp3 expression oscillates in a daily manner under the control of REV-ERBα in peritoneal mouse macrophages in vivo135. Similar oscillations were observed in primary mouse bone marrow-derived and human monocyte-derived macrophages synchronized in vitro, with circadian oscillations in Nlrp3 mRNA being lost upon Rev-erbα ablation. Given the importance of NLRP3 in influencing outcomes of UTI caused by α-hemolysin-positive UPEC strains, such rhythmic control of this PRR is likely to influence susceptibility and severity of UTI.
Circadian rhythm and leukocyte recruitment
The appropriate migration of immune cells into tissues is critical for effective host defense during infection, as exemplified by neutrophil recruitment during UTI42. In mice, total-blood leukocyte numbers peak at rest phase (ZT5), whereas the trafficking of monocytes into bone marrow and organs peaks during the active phase (ZT13)136. The circadian variation in chemokine receptor CXCR4 can regulate the release of monocytes from the bone marrow and affects their homing ability to peripheral organs such as the liver and lung137,138. In parallel, the recruitment of inflammatory monocytes is dependent on the chemokine CCL2. In mice, Bmal1 deficiency disrupted this CCL2 oscillation, which impaired the daily trafficking of monocytes139. The movement of inflammatory monocytes to peripheral tissues from the blood is dependent on leukocyte adhesion. This process involves the expression and engagement of adhesion molecules on circulating monocytes to enable their trans-endothelial migration. This regulation is controlled by the molecular clock in monocytes. Bmal1 deletion in monocytes disrupts the rhythmic expression of the chemokine receptor CCR2, the transmembrane receptor CD18 integrin that facilitates extracellular matrix adhesion, and L-selectin that enables monocyte binding to endothelial cells138. This evidence suggests that disruption of Bmal1 may also cause dysfunctional monocyte/macrophage trafficking into target organs such as the bladder and kidney which are common infection sites of UTI. Thus, circadian control of these adhesion molecules and chemokines would be predicted to have an impact on UTI outcomes.
Circadian rhythm and inflammatory responses
In mice and humans, UPEC infection elicits the secretion of several inflammatory cytokines from resident and recruited immune cells. These include TNF, CCL2, IL-1β, and IL-6140. Cytokine secretion rhythms have been observed in vivo where serum levels of LPS-induced IL-6, IL-12, CCL5, CXCL1, and CCL2 were all elevated in wild type mice at the time of transition to the dark phase, by comparison to light phase141. Since glucocorticoids can dampen LPS-inducible inflammatory mediator production in macrophages142,143 and are under circadian clock control142, one possibility is that rhythmic cytokine production relates to regulation by this stress hormone. However, this seems unlikely, as the rhythms of IL-6 and TNF persisted in adrenalectomized mice144. It is therefore quite likely that a macrophage-intrinsic circadian clock governs these oscillations. Gibbs et al. showed that the temporal variations in serum levels of LPS-inducible IL-6 were absent in mice with myeloid-specific Bmal1 deletion. This study also investigated if REV-ERBα links the circadian and inflammatory pathways, given that expression of the transcription factor REV-ERBα was temporally regulated in peritoneal macrophages and this effect was abolished by Bmal1 deletion. Indeed, rhythmic immune responses to LPS were absent in REV-ERBα-deficient mice, suggesting a link between BMAL1, REV-ERBα and IL-6 production in macrophages141. Rhythmic control of IL-6 may be particularly important during UPEC infection, since this cytokine controls iron homeostasis and host defense during UPEC infection.
Other cytokines linked to both circadian control and UTI outcomes include IL-1β and TNF. As noted above, anti-IL-1β treatment can limit and control UPEC colonization of the urinary tract48, while TNF secreted by macrophages can regulate neutrophil migration into the infected uroepithelium and facilitate antibacterial defense38. At a basal state and upon LPS stimulation, mice lacking Per1 and Per2 show increased Il1b and Tnf expression145. In the absence of Per1, both Ccr2 expression and the migratory activity of macrophages increases146. Deletion of Per2 in peritoneal macrophages resulted in augmented TLR9 activation and increased TNF and IL-12 production132. Deletion of the clock genes Cry1 and Cry2 also causes a constitutive increase in Il6, Tnf, and Nos2 expression147. These studies suggest that the susceptibility of the host to UPEC infection may partly be dependent on the temporal gating of cytokine responses that is regulated by intrinsic circadian clock components in macrophages.
Circadian control of urinary tract function
Circadian rhythms exist in both the upper and lower urinary tract. Existing literature has focused mainly on the role of circadian rhythm in bladder and kidney functions, such as water and electrolyte excretion, urine volume, uroflow, micturition frequency and volume per void148. Ihara et al. showed that Clock∆19 mice display a nocturia phenotype, with a loss of their diurnal pattern of urine volume per void, characterized by increased voiding frequency and reduced bladder function149. Such phenotypes have also been explored at a molecular level. For example, Negoro et al. reported that 184 bladder genes exhibit circadian rhythmicity150. More recent studies show that mucosal and urothelial-expressed genes also exhibit rhythmic diurnal oscillations. This is likely to influence physiological processes in the urinary tract and, potentially, host responses during UTI. For example, both ex vivo and in vitro studies have revealed that clock genes regulate mechanosensor genes such as Piezo1 and Trpv4, as well as connexin-family gene Gja1 that encodes Connexin 43, a gap junction protein, in a rhythmic fashion in the mouse bladder urothelium150,151,152. This may be important because bladder fullness is sensed by the TRPV4 and Piezo1 mechanosensors, and Connexin 43 is also required for the micturition reflex150,153,154. Interestingly, LPS treatment can increase intracellular Ca2+ concentrations in mouse urothelial cells via TRPV4155. Given that TRPV4 is regulated by the circadian clock, disruption of TRPV4 rhythms may be linked to increased voiding, a common symptom of UTI. Such evidence suggests that circadian rhythm may influence susceptibility to UTI and that UTIs may dysregulate normal functions of the bladder in the host (Fig. 3c).
Impact of immune stimuli and infection on circadian rhythm
There is a clear diurnal variation in the host immune response to infection and immune stimuli. However, this can also occur in a reciprocal manner, whereby host circadian rhythms can also be altered upon infection and immune stimuli. LPS intraperitoneal administration to rats transiently suppressed Per2 and Dbp mRNA levels and decreased the amplitude of clock genes in the SCN156. These gene expression changes may explain the 40 min phase delay in circadian activity and abolished locomotor activity for 3 days in LPS-challenged mice157,158. Such studies suggest direct effects of immune stimuli on the central clock. However, it is unclear as to how these bacterial products influence the SCN at a molecular level.
Circadian rhythms also regulate kidney functions, including renal plasma flow, excretion of water and urinary solutes, and glomerular filtration rate148,159,160. Patients with acute pyelonephritis from UPEC infections develop an impaired ability to concentrate urine161. A similar phenotype is also apparent in Clock knockout mice162, so it is tempting to speculate that UPEC infection may interfere with circadian rhythm. The ability to concentrate urine relies on the water permeability of the collecting duct and the renal sodium gradient. The water permeability of the collecting duct epithelium is increased by arginine vasopressin (AVP), which stimulates the vasopressin type 2 receptor (V2R) in the basolateral plasma membrane and induces the trafficking of aquaporin-2 (AQP2) to the apical plasma membrane of the kidney collecting duct principal cells163. Hara et al. have reported that Aqp2 and V2R display diurnal variations in the inner medulla164. Furthermore, transcriptome analysis of Clock knockout mice revealed substantial changes in the expression levels and/or in the circadian expression patterns of V2R and Aqp2165. This suggests that disrupting the rhythmic expression of vasopressin receptors and AQP2 may lead to an impaired ability to concentrate urine, as is seen in UTI patients. Regional hyper-salinity in the kidney medulla is also required for the kidney’s urine concentrating ability166. Interestingly, Berry et al. showed that the secretion of chemokines by renal epithelial cells can be stimulated by sodium and is further enhanced by the presence of E. coli LPS. Pharmacological inhibition of the renal sodium gradient in mice abolished the intrarenal Ccl2 expression gradient, leading to a reduction in the number of medullary CD14+ monocytes and increased bacterial growth in the kidney167. Though not investigated, it is possible that a dysregulated renal sodium gradient via a disrupted circadian clockwork can negatively impact immune cell migration, which would be predicted to facilitate and exacerbate UPEC-induced pyelonephritis.
Clinical implications of circadian biology
Understanding the relationship between chronobiology and immunology may lead to novel strategies to combat bacterial and viral infections. Direct pharmacological manipulation of circadian clock components using SR9009, a REV-ERB agonist that inhibits Bmal1 expression168, inhibits the cellular entry and replication of many viruses such as HCV169, HBV169, and HIV-1170. The timing of therapeutic intervention, often referred to as chronotherapy, may play a role in modulating antibacterial and antiviral responses. For example, a four-fold higher dose of the antiviral agent acyclovir was required to reduce morbidity and mortality of mice infected with HSV-2 at ZT18 versus those infected at ZT6171. Furthermore, a randomized controlled trial showed that influenza vaccination in the morning led to higher antibody titers than those who were vaccinated in the afternoon172. Hosokawa et al. also demonstrated temporal variations in the effectiveness of a single dose of the aminoglycoside antibiotic amikacin in an intraperitoneal infection model with Pseudomonas aeruginosa. The authors showed that amikacin administration to Institute of Cancer Research (ICR) mice at mid-dark phase (active) was more effective at reducing bacterial loads than its administration at mid-light phase (inactive)173. With respect to UPEC, the efficacy of antibiotics (gentamicin) in treating experimental E. coli-induced pyelonephritis was also shown to be time dependent174. This study showed that kidney colonization was reduced when this drug was injected during the active period of animals. This may be because immune responses such as leukocyte recruitment and cytokine secretion by macrophages are strongest immediately before or during the active phase. The limited circadian literature in animals thus supports the view that administration of antibiotics during the early active phase (presumably occurring in the morning in humans) of UTI patients, where macrophage functions such as pathogen recognition and cytokine secretion peak, may enhance bacterial clearance. However, as with other drugs175, it is also important to consider the chronopharmokinetics and chronotoxicology of antibiotics. For example, in a prospective study involving 179 patients with serious infection, Prins et al. showed that nephrotoxicity was significantly greater when gentamicin or tobramycin were administered to patients between midnight and 7:30 a.m. than at any other time of the day176. Therefore, administering antibiotics at a time synchronized with the timing of optimal host immune response may be beneficial, but the chronopharmacokinetics and toxicity of antimicrobial agents and the impact of pathogens on circadian rhythm should also be considered.
Macrophages in the ageing bladder
Postmenopausal and elderly women are particularly susceptible to recurrent UTI (rUTIs), with 53% of women over age 55 having at least one UTI recurrence within a year177. Thus, ageing is associated with increased incidence of rUTIs. Recent work has identified inflamm-aging as a possible mechanism through formation of tertiary lymphoid tissue (bTLT) in the bladder12. bTLT contains bone fide germinal centers with distinct B and T cell zones. It forms primarily in female bladders, and it develops and matures after reproductive senescence (approximately >12 months of age) in mice. Interestingly, bTLT contain a unique population of macrophages expressing CXCL13 in aged mice12. These are not observed in bladders from young mice. This finding differs from most other models of lymphoid neogenesis, in which a stromal cell secretes CXCL13 to develop and maintain the organization of the tertiary lymphoid tissue. There are a few other reports of macrophages producing CXCL13, such as subsets of peritoneal macrophages, M2-like macrophages during resolution of inflammation, within atherosclerotic plaques (that often contain artery TLTs), and in macrophages from patients with idiopathic pulmonary fibrosis. Single-cell analysis and bulk transcriptomics of macrophage populations revealed a subset of markers of murine peritoneal macrophages and highlights macrophage dynamics in the experimental Staphylococcus aureus peritonitis and zymosan-induced peritonitis models178,179. The expression of CXCL13 in human macrophage populations is controlled by cytokines including TNF and IL-10180, and the increased expression of CXCL13 may play a role in plaque stabilization in human atherosclerosis181. In systemic sclerosis it has been reported that the increased expression of CXCL13 by macrophages is due to Fli1 deficiency, with this having the potential to contribute to the development of tissue fibrosis and tissue-specific immune activation182.
In murine models, macrophages expressing CXCL13 have been shown to have an important role in protecting the host, and recently, CXCL13+CX3CR1+ resident intestinal macrophages were shown to induce IgA-producing bTLT in response to Salmonella infection183. Thus, our work and that of others may be changing the paradigm of which cells typically produce CXCL13 to promote bTLT formation. The reason why aged bladder macrophages begin to express CXCL13 remains to be determined. In ageing, tissue macrophages maintain tissue homeostasis by clearing debris as cells die, become senescent, or accumulate damaged proteins184. Impaired clearance of these cells by macrophages contributes to age-related pathologies and inflammation. One possibility is that CXCL13 production by macrophages could increase due to phagocytosis of these senescent cells, leading to subsequent bTLT formation. If senescent cells contribute to macrophage-derived CXCL13, that mechanism may explain why multiple organs form bTLTs during ageing and why germ-free mice still form bTLTs.
Conclusions and final perspectives
Presently, it remains unclear if there are functional differences between yolk sac-, fetal liver-, and hematopoietic-derived macrophages in response to ageing, infection, metabolic challenges, and other environmental changes such as circadian rhythm, even though these macrophage populations may show similar phenotypes. To further elucidate the functional biology and the influence of genetic variation on resident bladder macrophage populations in response to infection, cancer metabolic stress and homeostasis, spatial and temporal compartmentalization of these cells will need to be characterized through single-cell transcriptomics and epigenetic studies on different stains of inbred mice, including the collaborative cross mice. Additional fate mapping studies on the macrophage populations should be undertaken in genetically diverse mice to further characterize the phenotypes and functions of resident bladder macrophage populations during homeostasis, as well as in response to immunological and metabolic challenges, as the majority of studies to date have been performed in C57BL/6 mice.
Macrophages in the bladder play in important roles in host defense and immune response during UTIs. These include the cooperation of macrophage subsets that leads to the recruitment of protective neutrophils during UTIs, as well as their involvement in the IL-6/hepcidin feedback loop and LCN-2 production that regulates iron levels during UPEC infections. Interactions between macrophages and UPEC result in a diverse array of immune responses due to the genetic and phenotypic diversity of UPEC strains. This complexity raises additional questions about the role and fate of macrophages during a UTI that have not yet been fully investigated. The role of ageing in the macrophage response adds another dimension of complexity, as illustrated by recent work showing increased expression of CXCL13+ macrophages in aged mice. Discovering mechanisms behind this response will fill an important gap in knowledge leading to a broader understanding of how bTLT formation is promoted by macrophages in the bladder.
Circadian rhythms play a role in urinary tract function, as well as in inflammatory responses and leukocyte recruitment. Evidence that circadian processes are also inherent in macrophage biology has significant implications for related macrophage functions, such as pathogen recognition and cytokine secretion, which peak during the early active phase. A better understanding of these processes in humans could lead to improved treatment regimens for UTI patients that take into consideration chronopharmacokinetics and chronotoxicology of antibiotics and strive to synchronize clinical interventions with the optimal time of day for the desired host immune response.
References
Orecchioni, M., Ghosheh, Y., Pramod, A. B. & Ley, K. Macrophage polarization: different gene signatures in M1(LPS+) vs. classically and M2(LPS−) vs. alternatively activated macrophages. Front. Immunol. 10, 1084 (2019).
Van Dyken, S. J. & Locksley, R. M. Interleukin-4- and interleukin-13-mediated alternatively activated macrophages: roles in homeostasis and disease. Annu. Rev. Immunol. 31, 317–343 (2013).
Wynn, T. A. & Vannella, K. M. Macrophages in tissue repair, regeneration, and fibrosis. Immunity 44, 450–462 (2016).
Murray, P. J. et al. Macrophage activation and polarization: nomenclature and experimental guidelines. Immunity 41, 14–20 (2014).
Xue, J. et al. Transcriptome-based network analysis reveals a spectrum model of human macrophage activation. Immunity 40, 274–288 (2014).
Blériot, C., Chakarov, S. & Ginhoux, F. Determinants of resident tissue macrophage identity and function. Immunity 52, 957–970 (2020).
Ginhoux, F. & Guilliams, M. Tissue-resident macrophage ontogeny and homeostasis. Immunity 44, 439–449 (2016).
Mass, E. et al. Specification of tissue-resident macrophages during organogenesis. Science 353, aaf4238 (2016).
Lacerda Mariano, L. et al. Functionally distinct resident macrophage subsets differentially shape responses to infection in the bladder. Sci. Adv. 6, eabc5739 (2020).
Owusu-Boaitey, N., Bauckman, K. A., Zhang, T. & Mysorekar, I. U. Macrophagic control of the response to uropathogenic E. coli infection by regulation of iron retention in an IL-6-dependent manner. Immun. Inflamm. Dis. 4, 413–426 (2016).
Fu, C. L., Odegaard, J. I. & Hsieh, M. H. Macrophages are required for host survival in experimental urogenital schistosomiasis. Faseb J. 29, 193–207 (2015).
Ligon, M. M. et al. Single cell and tissue-transcriptomic analysis of murine bladders reveals age- and TNFα-dependent but microbiota-independent tertiary lymphoid tissue formation. Mucosal Immunol. 13, 908–918 (2020).
Mould, K. J., Jackson, N. D., Henson, P. M., Seibold, M. & Janssen, W. J. Single cell RNA sequencing identifies unique inflammatory airspace macrophage subsets. JCI Insight 4, e126556 (2019).
Zimmerman, K. A. et al. Single-Cell RNA sequencing identifies candidate renal resident macrophage gene expression signatures across species. J. Am. Soc. Nephrol. 30, 767–781 (2019).
Guilliams, M. et al. Spatial proteogenomics reveals distinct and evolutionarily conserved hepatic macrophage niches. Cell 185, 379–396 (2022).
Schulz, C. et al. A lineage of myeloid cells independent of Myb and hematopoietic stem cells. Science 336, 86–90 (2012).
Hoeffel, G. et al. C-Myb(+) erythro-myeloid progenitor-derived fetal monocytes give rise to adult tissue-resident macrophages. Immunity 42, 665–678 (2015).
Gomez Perdiguero, E. et al. Tissue-resident macrophages originate from yolk-sac-derived erythro-myeloid progenitors. Nature 518, 547–551 (2015).
Gentek, R. et al. Hemogenic endothelial fate mapping reveals dual developmental origin of mast cells. Immunity 48, 1160–1171 (2018).
Boyer, S. W., Schroeder, A. V., Smith-Berdan, S. & Forsberg, E. C. All hematopoietic cells develop from hematopoietic stem cells through Flk2/Flt3-positive progenitor cells. Cell Stem Cell 9, 64–73 (2011).
Arandjelovic, S. & Ravichandran, K. S. Phagocytosis of apoptotic cells in homeostasis. Nat. Immunol. 16, 907–917 (2015).
Henson, P. M. & Hume, D. A. Apoptotic cell removal in development and tissue homeostasis. Trends Immunol. 27, 244–250 (2006).
A-Gonzalez, N. et al. Phagocytosis imprints heterogeneity in tissue-resident macrophages. J. Exp. Med. 214, 1281–1296 (2017).
A-Gonzalez, N. et al. Apoptotic cells promote their own clearance and immune tolerance through activation of the nuclear receptor LXR. Immunity 31, 45–258 (2009).
Fadok, V. A. et al. Macrophages that have ingested apoptotic cells in vitro inhibit proinflammatory cytokine production through autocrine/paracrine mechanisms involving TGF-beta, PGE2, and PAF. J. Clin. Investig. 101, 890–898 (1998).
Joseph, D. B. et al. In vivo replacement of damaged bladder urothelium by Wolffian duct epithelial cells. Proc. Natl Acad. Sci. U.S.A. 115, 8394–8399 (2018).
Bottek, J. et al. Spatial proteomics revealed a CX(3)CL1-dependent crosstalk between the urothelium and relocated macrophages through IL-6 during an acute bacterial infection in the urinary bladder. Mucosal Immunol. 13, 702–714 (2020).
Munro, D. A. D. & Hughes, J. The origins and functions of tissue-resident macrophages in kidney development. Front. Physiol. 8, 837 (2017).
Puranik, A. S. et al. Kidney-resident macrophages promote a proangiogenic environment in the normal and chronically ischemic mouse kidney. Sci. Rep. 8, 13948 (2018).
Dong, Y. et al. CD44 loss disrupts lung lipid surfactant homeostasis and exacerbates oxidized lipid-induced lung inflammation. Front. Immunol. 11, 29 (2020).
Taylor, P. R. et al. Macrophage receptors and immune recognition. Annu. Rev. Immunol. 23, 901–944 (2005).
Akira, S., Takeda, K. & Kaisho, T. Toll-like receptors: critical proteins linking innate and acquired immunity. Nat. Immunol. 2, 675–680 (2001).
Inohara, N. & Nuñez, G. NODs: intracellular proteins involved in inflammation and apoptosis. Nat. Rev. Immunol. 3, 371–382 (2003).
Schilling, J. D., Martin, S. M., Hung, C. S., Lorenz, R. G. & Hultgren, S. J. Toll-like receptor 4 on stromal and hematopoietic cells mediates innate resistance to uropathogenic Escherichia coli. Proc. Natl Acad. Sci. USA 100, 4203–4208 (2003).
Carey, A. J. et al. Uropathogenic Escherichia coli engages CD14-dependent signaling to enable bladder-macrophage-dependent control of acute urinary tract infection. J. Infect. Dis. 213, 659–668 (2016).
Mossman, K. L. et al. Cutting edge: FimH adhesin of type 1 fimbriae is a novel TLR4 ligand. J. Immunol. 181, 6702–6706 (2008).
Ching, C. B. et al. Interleukin-6/Stat3 signaling has an essential role in the host antimicrobial response to urinary tract infection. Kidney Int. 93, 1320–1329 (2018).
Schiwon, M. et al. Crosstalk between sentinel and helper macrophages permits neutrophil migration into infected uroepithelium. Cell 56, 456–468 (2014).
Ko, Y. C. et al. Elevated interleukin-8 levels in the urine of patients with urinary tract infections. Infect. Immun. 61, 1307–1314 (1993).
Zaki Mel, S. Interleukin 8 is a surrogate marker for rapid diagnosis of bacteriuria. Immunol. Investig. 37, 694–703 (2008).
Haraoka, M. et al. Neutrophil recruitment and resistance to urinary tract infection. J. Infect. Dis. 180, 1220–1229 (1999).
Abraham, S. N. & Miao, Y. The nature of immune responses to urinary tract infections. Nat. Rev. Immunol. 15, 655–663 (2015).
Michlewska, S., Dransfield, I., Megson, I. L. & Rossi, A. G. Macrophage phagocytosis of apoptotic neutrophils is critically regulated by the opposing actions of pro-inflammatory and anti-inflammatory agents: key role for TNF-alpha. Faseb J. 23, 844–854 (2009).
Mittal, R., Chhibber, S., Sharma, S. & Harjai, K. Macrophage inflammatory protein-2, neutrophil recruitment and bacterial persistence in an experimental mouse model of urinary tract infection. Microbes Infect. 6, 1326–1332 (2004).
Yu, Y. et al. Characterization of early-phase neutrophil extracellular traps in urinary tract infections. PLoS Pathog. 13, e1006151 (2017).
Mora-Bau, G. et al. Macrophages subvert adaptive immunity to urinary tract infection. PLoS Pathog. 11, e1005044 (2015).
Lacerda Mariano, L. & Ingersoll, M. A. Bladder resident macrophages: mucosal sentinels. Cell Immunol. 330, 136–141 (2018).
Symington, J. W. et al. ATG16L1 deficiency in macrophages drives clearance of uropathogenic E. coli in an IL-1β-dependent manner. Mucosal Immunol. 8, 1388–1399 (2015).
Demirel, I. et al. Activation of the NLRP3 inflammasome pathway by uropathogenic Escherichia coli is virulence factor-dependent and influences colonization of bladder epithelial cells. Front. Cell. Infect. Microbiol. 8, 81 (2018).
Murthy, A. M. V. et al. Regulation of hemolysin in uropathogenic Escherichia coli fine-tunes killing of human macrophages. Virulence 9, 967–980 (2018).
Schroder, K. & Tschopp, J. The inflammasomes. Cell 140, 821–832 (2010).
Nagamatsu, K. et al. Dysregulation of Escherichia coli α-hemolysin expression alters the course of acute and persistent urinary tract infection. Proc. Natl Acad. Sci. U.S.A. 112, e871–e880 (2015).
Murthy, A. M. V. et al. Variation in hemolysin A expression between uropathogenic Escherichia coli isolates determines NLRP3-dependent vs. -independent macrophage cell death and host colonization. Faseb J. 33, 7437–7450 (2019).
Stocks, C. J. et al. Uropathogenic Escherichia coli employs both evasion and resistance to subvert innate immune-mediated zinc toxicity for dissemination. Proc. Natl Acad. Sci. USA. 116, 6341–6350 (2019).
Bokil, N. J. et al. Intramacrophage survival of uropathogenic Escherichia coli: differences between diverse clinical isolates and between mouse and human macrophages. Immunobiology 216, 1164–1171 (2011).
Ajuebor, M. N. et al. Role of resident peritoneal macrophages and mast cells in chemokine production and neutrophil migration in acute inflammation: evidence for an inhibitory loop involving endogenous IL-10. J. Immunol. 162, 1685–1691 (1999).
Rosas, M. et al. The induction of inflammation by dectin-1 in vivo is dependent on myeloid cell programming and the progression of phagocytosis. J. Immunol. 181, 3549–3557 (2008).
Hedges, S. & Svanborg, C. The mucosal cytokine response to urinary tract infections. Int. J. Antimicrob. Agents 4, 89–93 (1994).
Ching, C., Schwartz, L., Spencer, J. D. & Becknell, B. Innate immunity and urinary tract infection. Pediatr. Nephrol. 35, 1183–1192 (2020).
Acharya, D. et al. Rapid bladder interleukin-10 synthesis in response to uropathogenic Escherichia coli is part of a defense strategy triggered by the major bacterial flagellar filament FliC and contingent on TLR5. mSphere 4, e00545–19 (2019).
Duell, B. L., Carey, A. J., Dando, S. J., Schembri, M. & Ulett, G. C. Human bladder uroepithelial cells synergize with monocytes to promote IL-10 synthesis and other cytokine responses to uropathogenic Escherichia coli. PLoS ONE 8, e78013 (2013).
Roca, H. et al. CCL2 and interleukin-6 promote survival of human CD11b+ peripheral blood mononuclear cells and induce M2-type macrophage polarization. J. Biol. Chem. 284, 34342–34354 (2009).
Gou, X. et al. IL-6 prevents lung macrophage death and lung inflammation injury by inhibiting GSDME- and GSDMD-mediated pyroptosis during pneumococcal pneumosepsis. Microbiol. Spectr. 10, e0204921 (2022).
Frisdal, E. et al. Interleukin-6 protects human macrophages from cellular cholesterol accumulation and attenuates the proinflammatory response. J. Biol. Chem. 286, 30926–30936 (2011).
Yona, S. et al. Fate mapping reveals origins and dynamics of monocytes and tissue macrophages under homeostasis. Immunity 38, 79–91 (2013).
Hashimoto, D. et al. Tissue-resident macrophages self-maintain locally throughout adult life with minimal contribution from circulating monocytes. Immunity 38, 792–804 (2013).
Bellingan, G. J. et al. Adhesion molecule-dependent mechanisms regulate the rate of macrophage clearance during the resolution of peritoneal inflammation. J. Exp. Med. 196, 1515–1521 (2002).
Lauder, S. N. et al. Paracetamol reduces influenza-induced immunopathology in a mouse model of infection without compromising virus clearance or the generation of protective immunity. Thorax 66, 368–374 (2011).
Kirby, A. C., Coles, M. C. & Kaye, P. M. Alveolar macrophages transport pathogens to lung draining lymph nodes. J. Immunol. 183, 1983–1989 (2009).
Delamarre, L., Pack, M., Chang, H., Mellman, I. & Trombetta, E. S. Differential lysosomal proteolysis in antigen-presenting cells determines antigen fate. Science 307, 1630–1634 (2005).
Amer, A. O., Byrne, B. G. & Swanson, M. S. Macrophages rapidly transfer pathogens from lipid raft vacuoles to autophagosomes. Autophagy 1, 53–58 (2005).
Baorto, D. M. et al. Survival of FimH-expressing enterobacteria in macrophages relies on glycolipid traffic. Nature 389, 636–639 (1997).
Sanjuan, M. A. et al. Toll-like receptor signalling in macrophages links the autophagy pathway to phagocytosis. Nature 450, 1253–1257 (2007).
Lee, J. et al. Autophagy suppresses interleukin-1β (IL-1β) signaling by activation of p62 degradation via lysosomal and proteasomal pathways. J. Biol. Chem. 287, 4033–4040 (2012).
Joshi, C. S., Mora, A., Felder, P. A. & Mysorekar, I. U. NRF2 promotes urothelial cell response to bacterial infection by regulating reactive oxygen species and RAB27B expression. Cell Rep. 37, 109856 (2021).
Schaale, K. et al. Strain- and host species-specific inflammasome activation, IL-1β release, and cell death in macrophages infected with uropathogenic Escherichia coli. Mucosal Immunol. 9, 124–136 (2016).
Gordon, O. et al. Silver coordination polymers for prevention of implant infection: thiol interaction, impact on respiratory chain enzymes, and hydroxyl radical induction. Antimicrob. Agents Chemother. 54, 4208–4218 (2010).
Cairo, G., Recalcati, S., Mantovani, A. & Locati, M. Iron trafficking and metabolism in macrophages: contribution to the polarized phenotype. Trends Immunol. 32, 241–247 (2011).
Subashchandrabose, S. & Mobley, H. L. T. Virulence and fitness determinants of uropathogenic Escherichia coli. Microbiol. Spectr. https://doi.org/10.1128/microbiolspec.UTI-0015-2012 (2015).
Michels, K., Nemeth, E., Ganz, T. & Mehrad, B. Hepcidin and host defense against infectious diseases. PLoS Pathog. 11, e1004998 (2015).
Nemeth, E. et al. Hepcidin, a putative mediator of anemia of inflammation, is a type II acute-phase protein. Blood 101, 2461–2463 (2003).
Shanmugam, N. K. et al. Tumor necrosis factor α inhibits expression of the iron regulating hormone hepcidin in murine models of innate colitis. PLoS ONE 7, e38136 (2012).
Lee, P., Peng, H., Gelbart, T., Wang, L. & Beutler, E. Regulation of hepcidin transcription by interleukin-1 and interleukin-6. Proc. Natl Acad. Sci. USA 102, 1906–1910 (2005).
Armitage, A. E. et al. Hepcidin regulation by innate immune and infectious stimuli. Blood 118, 4129–4139 (2011).
Nairz, M., Schroll, A., Sonnweber, T. & Weiss, G. The struggle for iron—a metal at the host-pathogen interface. Cell Microbiol 12, 1691–1702 (2010).
Cassat, J. E. & Skaar, E. P. Iron in infection and immunity. Cell Host Microbe 13, 509–519 (2013).
Theurl, I. et al. Autocrine formation of hepcidin induces iron retention in human monocytes. Blood 111, 2392–2399 (2008).
Bellmann-Weiler, R. et al. Neutrophil gelatinase-associated lipocalin and interleukin-10 regulate intramacrophage Chlamydia pneumoniae replication by modulating intracellular iron homeostasis. Immunobiology 218, 969–978 (2013).
Schilling, J. D., Mulvey, M. A., Vincent, C. D., Lorenz, R. G. & Hultgren, S. J. Bacterial invasion augments epithelial cytokine responses to Escherichia coli through a lipopolysaccharide-dependent mechanism. J. Immunol. 166, 1148–1155 (2001).
Mysorekar, I. U., Mulvey, M. A., Hultgren, S. J. & Gordon, J. I. Molecular regulation of urothelial renewal and host defenses during infection with uropathogenic Escherichia coli. J. Biol. Chem. 277, 7412–7419 (2002).
Song, J. et al. A novel TLR4-mediated signaling pathway leading to IL-6 responses in human bladder epithelial cells. PLoS Pathog. 3, e60 (2007).
Bhushan, S. et al. Uropathogenic Escherichia coli block MyD88-dependent and activate MyD88-independent signaling pathways in rat testicular cells. J. Immunol. 180, 5537–5547 (2008).
Bhushan, S. et al. Uropathogenic E. coli induce different immune response in testicular and peritoneal macrophages: implications for testicular immune privilege. PLoS ONE 6, e28452 (2011).
Steigedal, M. et al. Lipocalin 2 imparts selective pressure on bacterial growth in the bladder and is elevated in women with urinary tract infection. J. Immunol. 193, 6081–6089 (2014).
Paragas, N. et al. α-Intercalated cells defend the urinary system from bacterial infection. J. Clin. Investig. 124, 2963–2976 (2014).
Shields-Cutler, R. R. et al. Human urinary composition controls antibacterial activity of siderocalin. J. Biol. Chem. 290, 15949–15960 (2015).
Johnson, A. C., Becker, K. & Zager, R. A. Parenteral iron formulations differentially affect MCP-1, HO-1, and NGAL gene expression and renal responses to injury. Am. J. Physiol. Ren. Physiol. 299, 426–435 (2010).
Nairz, M. et al. Lipocalin-2 ensures host defense against Salmonella Typhimurium by controlling macrophage iron homeostasis and immune response. Eur. J. Immunol. 45, 3073–3086 (2015).
Bachman, M. A., Miller, V. L. & Weiser, J. N. Mucosal lipocalin 2 has pro-inflammatory and iron-sequestering effects in response to bacterial enterobactin. PLoS Pathog. 5, e1000622 (2009).
Cheng, L. et al. Lipocalin-2 promotes m1 macrophages polarization in a mouse cardiac ischaemia-reperfusion injury model. Scand. J. Immunol. 81, 31–38 (2015).
Subashchandrabose, S. & Mobley, H. L. Back to the metal age: battle for metals at the host-pathogen interface during urinary tract infection. Metallomics 7, 935–942 (2015).
Choi, J. W., Fujii, T. & Fujii, N. Significance of neutrophil gelatinase-associated lipocalin level-to-serum creatinine ratio for assessing severity of inflammation in patients with renal dysfunction. Biomed. Res. Int. 2015, 791926–791926 (2015).
Dikshit, N. et al. Intracellular uropathogenic E. coli exploits host Rab35 for iron acquisition and survival within urinary bladder cells. PLoS Pathog. 11, e1005083 (2015).
Bauckman, K. A. & Mysorekar, I. U. Ferritinophagy drives uropathogenic Escherichia coli persistence in bladder epithelial cells. Autophagy 12, 850–863 (2016).
Henderson, J. P. et al. Quantitative metabolomics reveals an epigenetic blueprint for iron acquisition in uropathogenic Escherichia coli. PLoS Pathog. 5, e1000305 (2009).
Gammoh, N. Z. & Rink, L. Zinc in Infection and Inflammation. Nutrients 9, 6 (2017).
Jordan, M. R., Wang, J., Capdevila, D. A. & Giedroc, D. P. Multi-metal nutrient restriction and crosstalk in metallostasis systems in microbial pathogens. Curr. Opin. Microbiol. 55, 17–25 (2020).
von Pein, J. B., Stocks, C. J., Schembri, M. A., Kapetanovic, R. & Sweet, M. J. An alloy of zinc and innate immunity: Galvanising host defence against infection. Cell Microbiol. 23, e13268 (2021).
Sabri, M., Houle, S. & Dozois, C. M. Roles of the extraintestinal pathogenic Escherichia coli ZnuACB and ZupT zinc transporters during urinary tract infection. Infect. Immun. 77, 1155–1164 (2009).
Botella, H. et al. Mycobacterial p(1)-type ATPases mediate resistance to zinc poisoning in human macrophages. Cell Host Microbe 10, 248–259 (2011).
Kapetanovic, R. et al. Salmonella employs multiple mechanisms to subvert the TLR-inducible zinc-mediated antimicrobial response of human macrophages. Faseb J. 30, 1901–1912 (2016).
Stocks, C. J. et al. Frontline science: LPS-inducible SLC30A1 drives human macrophage-mediated zinc toxicity against intracellular Escherichia coli. J. Leukoc. Biol. 109, 287–297 (2021).
Hastings, M. H., Maywood, E. S. & Brancaccio, M. Generation of circadian rhythms in the suprachiasmatic nucleus. Nat. Rev. Neurosci. 19, 453–469 (2018).
Wang, C., Lutes, L. K., Barnoud, C. & Scheiermann, C. The circadian immune system. Sci. Immunol. 7, eabm2465 (2022).
Koronowski, K. B. & Sassone-Corsi, P. Communicating clocks shape circadian homeostasis. Science 371, eabd0951 (2021).
Patke, A., Young, M. W. & Axelrod, S. Molecular mechanisms and physiological importance of circadian rhythms. Nat. Rev. Mol. Cell. Biol. 21, 67–84 (2020).
Shearman, L. P., Zylka, M. J., Weaver, D. R., Kolakowski, L. F. Jr. & Reppert, S. M. Two period homologs: circadian expression and photic regulation in the suprachiasmatic nuclei. Neuron 19, 1261–1269 (1997).
Kume, K. et al. mCRY1 and mCRY2 are essential components of the negative limb of the circadian clock feedback loop. Cell 98, 193–205 (1999).
Cao, X., Yang, Y., Selby, C. P., Liu, Z. & Sancar, A. Molecular mechanism of the repressive phase of the mammalian circadian clock. Proc. Natl Acad. Sci. USA 118, e2021174118 (2021).
Preitner, N. et al. The orphan nuclear receptor REV-ERBalpha controls circadian transcription within the positive limb of the mammalian circadian oscillator. Cell 110, 251–260 (2002).
Sato, T. K. et al. A functional genomics strategy reveals Rora as a component of the mammalian circadian clock. Neuron 43, 527–537 (2004).
Gachon, F. Physiological function of PARbZip circadian clock-controlled transcription factors. Ann. Med. 39, 562–571 (2007).
Mitsui, S., Yamaguchi, S., Matsuo, T., Ishida, Y. & Okamura, H. Antagonistic role of E4BP4 and PAR proteins in the circadian oscillatory mechanism. Genes Dev. 15, 995–1006 (2001).
Weger, B. D. et al. Systematic analysis of differential rhythmic liver gene expression mediated by the circadian clock and feeding rhythms. Proc. Natl Acad. Sci. USA 118, e2015803118 (2021).
Yoshitane, H. et al. Functional D-box sequences reset the circadian clock and drive mRNA rhythms. Commun. Biol. 2, 300 (2019).
Collins, E. J. et al. Post-transcriptional circadian regulation in macrophages organizes temporally distinct immunometabolic states. Genome Res. 31, 171–185 (2021).
Behzadi, E. & Behzadi, P. The role of toll-like receptors (TLRs) in urinary tract infections (UTIs). Cent. Eur. J. Urol. 69, 404–410 (2016).
Patole, P. S. et al. Toll-like receptor-4: renal cells and bone marrow cells signal for neutrophil recruitment during pyelonephritis. Kidney Int. 68, 2582–2587 (2005).
Andersen-Nissen, E. et al. Cutting edge: Tlr5-/- mice are more susceptible to Escherichia coli urinary tract infection. J. Immunol. 178, 4717–4720 (2007).
Zhang, D. et al. A toll-like receptor that prevents infection by uropathogenic bacteria. Science 303, 1522–1526 (2004).
Silver, A. C. et al. Daily oscillations in expression and responsiveness of Toll-like receptors in splenic immune cells. Heliyon 4, e00579 (2018).
Silver, A. C., Arjona, A., Walker, W. E. & Fikrig, E. The circadian clock controls toll-like receptor 9-mediated innate and adaptive immunity. Immunity 36, 251–261 (2012).
Swanson, K. V., Deng, M. & Ting, J. P. The NLRP3 inflammasome: molecular activation and regulation to therapeutics. Nat. Rev. Immunol. 19, 477–489 (2019).
Welch, R. A. Uropathogenic Escherichia coli-associated exotoxins. Microbiol. Spectr. https://doi.org/10.1128/microbiolspec.UTI-0011-2012 (2016).
Pourcet, B. et al. Nuclear receptor subfamily 1 Group D member 1 regulates circadian activity of NLRP3 inflammasome to reduce the severity of fulminant hepatitis in mice. Gastroenterology 154, 1449–1464.e1420 (2018).
Scheiermann, C. et al. Adrenergic nerves govern circadian leukocyte recruitment to tissues. Immunity 37, 290–301 (2012).
Chong, S. Z. et al. CXCR4 identifies transitional bone marrow premonocytes that replenish the mature monocyte pool for peripheral responses. J. Exp. Med. 213, 2293–2314 (2016).
He, W. et al. Circadian expression of migratory factors establishes lineage-specific signatures that guide the homing of leukocyte subsets to tissues. Immunity 49, 1175–1190.e1177 (2018).
Nguyen, K. D. et al. Circadian gene Bmal1 regulates diurnal oscillations of Ly6C(hi) inflammatory monocytes. Science 341, 1483–1488 (2013).
Sundac, L. et al. Protein-based profiling of the immune response to uropathogenic Escherichia coli in adult patients immediately following hospital admission for acute cystitis. Pathog. Dis. 74, ftw062 (2016).
Gibbs, J. E. et al. The nuclear receptor REV-ERBα mediates circadian regulation of innate immunity through selective regulation of inflammatory cytokines. Proc. Natl Acad. Sci. USA 109, 582–587 (2012).
Chung, S., Son, G. H. & Kim, K. Circadian rhythm of adrenal glucocorticoid: its regulation and clinical implications. Biochim. Biophys. Acta 1812, 581–591 (2011).
Bhattacharyya, S., Brown, D. E., Brewer, J. A., Vogt, S. K. & Muglia, L. J. Macrophage glucocorticoid receptors regulate Toll-like receptor 4-mediated inflammatory responses by selective inhibition of p38 MAP kinase. Blood 109, 4313–4319 (2007).
Olejniczak, I., Oster, H. & Ray, D. W. Glucocorticoid circadian rhythms in immune function. Semin. Immunopathol. 44, 53–163 (2022).
Xu, H. et al. Myeloid cell-specific disruption of Period1 and Period2 exacerbates diet-induced inflammation and insulin resistance. J. Biol. Chem. 289, 16374–16388 (2014).
Wang, T. et al. PER1 prevents excessive innate immune response during endotoxin-induced liver injury through regulation of macrophage recruitment in mice. Cell Death Dis. 7, e2176 (2016).
Narasimamurthy, R. et al. Circadian clock protein cryptochrome regulates the expression of proinflammatory cytokines. Proc. Natl Acad. Sci. USA 109, 12662–12667 (2012).
Firsov, D. & Bonny, O. Circadian rhythms and the kidney. Nat. Rev. Nephrol. 14, 626–635 (2018).
Ihara, T. et al. The Clock mutant mouse is a novel experimental model for nocturia and nocturnal polyuria. Neurourol. Urodyn. 36, 1034–1038 (2017).
Negoro, H. et al. Involvement of urinary bladder Connexin43 and the circadian clock in coordination of diurnal micturition rhythm. Nat. Commun. 3, 809 (2012).
Ihara, T. et al. Clock genes regulate the circadian expression of Piezo1, TRPV4, Connexin26, and VNUT in an ex vivo mouse bladder mucosa. PLoS ONE 12, e0168234 (2017).
Ihara, T. et al. The Circadian expression of Piezo1, TRPV4, Connexin26, and VNUT, associated with the expression levels of the clock genes in mouse primary cultured urothelial cells. Neurourol. Urodyn. 37, 942–951 (2018).
Mochizuki, T. et al. The TRPV4 cation channel mediates stretch-evoked Ca2+ influx and ATP release in primary urothelial cell cultures. J. Biol. Chem. 284, 21257–21264 (2009).
Miyamoto, T. et al. Functional role for Piezo1 in stretch-evoked Ca2+ influx and ATP release in urothelial cell cultures. J. Biol. Chem. 289, 16565–16575 (2014).
Alpizar, Y. A. et al. TRPV4 mediates acute bladder responses to bacterial lipopolysaccharides. Front. Immunol. 11, 799 (2020).
Okada, K. et al. Injection of LPS causes transient suppression of biological clock genes in rats. J. Surg. Res. 145, 5–12 (2008).
Marpegán, L., Bekinschtein, T. A., Costas, M. A. & Golombek, D. A. Circadian responses to endotoxin treatment in mice. J. Neuroimmunol. 160, 102–109 (2005).
Marpegan, L. et al. Diurnal variation in endotoxin-induced mortality in mice: correlation with proinflammatory factors. Chronobiol. Int. 26, 1430–1442 (2009).
Gumz, M. L. Molecular basis of circadian rhythmicity in renal physiology and pathophysiology. Exp. Physiol. 101, 1025–1029 (2016).
Rakova, N. et al. Long-term space flight simulation reveals infradian rhythmicity in human Na(+) balance. Cell Metab. 17, 125–131 (2013).
Rodionova, E. A. et al. Urinary aquaporin-2 in children with acute pyelonephritis. Pediatr. Nephrol. 21, 361–367 (2006).
Zuber, A. M. et al. Molecular clock is involved in predictive circadian adjustment of renal function. Proc. Natl Acad. Sci. USA 106, 16523–16528 (2009).
Wilson, J. L., Miranda, C. A. & Knepper, M. A. Vasopressin and the regulation of aquaporin-2. Clin. Exp. Nephrol. 17, 751–764 (2013).
Hara, M. et al. Robust circadian clock oscillation and osmotic rhythms in inner medulla reflecting cortico-medullary osmotic gradient rhythm in rodent kidney. Sci. Rep. 7, 7306 (2017).
Nikolaeva, S. et al. The circadian clock modulates renal sodium handling. J. Am. Soc. Nephrol. 23, 1019–1026 (2012).
Knepper, M. A., Kwon, T. H. & Nielsen, S. Molecular physiology of water balance. N. Engl. J. Med. 372, 1349–1358 (2015).
Berry, M. R. et al. Renal sodium gradient orchestrates a dynamic antibacterial defense zone. Cell 170, 860–874.e819 (2017).
Solt, L. A. et al. Regulation of circadian behaviour and metabolism by synthetic REV-ERB agonists. Nature 485, 62–68 (2012).
Zhuang, X. et al. The circadian clock components BMAL1 and REV-ERBα regulate flavivirus replication. Nat. Commun. 10, 377 (2019).
Borrmann, H. et al. Pharmacological activation of the circadian component REV-ERB inhibits HIV-1 replication. Sci. Rep. 10, 13271 (2020).
Matsuzawa, T. et al. Differential day-night outcome to HSV-2 cutaneous infection. J. Investig. Dermatol. 138, 233–236 (2018).
Long, J. E. et al. Morning vaccination enhances antibody response over afternoon vaccination: a cluster-randomised trial. Vaccine 34, 2679–2685 (2016).
Hosokawa, H., Nyu, S., Nakamura, K., Mifune, K. & Nakano, S. Circadian variation in amikacin clearance and its effects on efficacy and toxicity in mice with and without immunosuppression. Chronobiol. Int. 10, 259–270 (1993).
LeBrun, M. et al. Effectiveness and toxicity of gentamicin in an experimental model of pyelonephritis: effect of the time of administration. Antimicrob. Agents Chemother. 43, 1020–1026 (1999).
Dallmann, R., Brown, S. A. & Gachon, F. Chronopharmacology: new insights and therapeutic implications. Annu. Rev. Pharmacol. Toxicol. 54, 339–361 (2014).
Prins, J. M., Weverling, G. J., van Ketel, R. J. & Speelman, P. Circadian variations in serum levels and the renal toxicity of aminoglycosides in patients. Clin. Pharmacol. Ther. 62, 106–111 (1997).
Ikäheimo, R. et al. Recurrence of urinary tract infection in a primary care setting: analysis of a 1-year follow-up of 179 women. Clin. Infect. Dis. 22, 91–99 (1996).
Accarias, S. et al. Single-cell analysis reveals new subset markers of murine peritoneal macrophages and highlights macrophage dynamics upon Staphylococcus aureus peritonitis. Innate Immun. 22, 382–392 (2016).
Stables, M. J. et al. Transcriptomic analyses of murine resolution-phase macrophages. Blood 118, e192–e208 (2011).
Bellamri, N. et al. TNF-α and IL-10 control CXCL13 expression in human macrophages. J. Immunol. 204, 2492–2502 (2020).
Smedbakken, L. M. et al. Increased levels of the homeostatic chemokine CXCL13 in human atherosclerosis—potential role in plaque stabilization. Atherosclerosis 224, 266–273 (2012).
Taniguchi, T. et al. CXCL13 produced by macrophages due to Fli1 deficiency may contribute to the development of tissue fibrosis, vasculopathy and immune activation in systemic sclerosis. Exp. Dermatol. 27, 1030–1037 (2018).
Koscsó, B. et al. Gut-resident CX3CR1(hi) macrophages induce tertiary lymphoid structures and IgA response in situ. Sci. Immunol. 5, eaax0062 (2020).
Ovadya, Y. et al. Impaired immune surveillance accelerates accumulation of senescent cells and aging. Nat. Commun. 9, 5435 (2018).
T’Jonck, W., Guilliams, M. & Bonnardel, J. Niche signals and transcription factors involved in tissue-resident macrophage development. Cell Immunol. 330, 43–53 (2018).
Acknowledgements
N.J.S. is supported by Columbia University O’Brien Center Opportunity Pool, U54DK104309-08. M.J.S. is supported by a National Health and Medical Research Council of Australia (NHMRC) Investigator Grant (APP1194406). I.U.M. is supported in part by NIH grants R01DK100644, R01AG052494, P20DK119840, and R56AG064634. We thank Dr. Robert Lawrence for editorial comments. Figures were created in part using BioRender®.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
IUM serves on the scientific advisory board of Luca Biologics.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, A.S., Steers, N.J., Parab, A.R. et al. Timing is everything: impact of development, ageing and circadian rhythm on macrophage functions in urinary tract infections. Mucosal Immunol 15, 1114–1126 (2022). https://doi.org/10.1038/s41385-022-00558-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41385-022-00558-z