Abstract
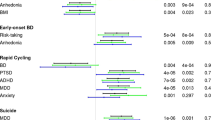
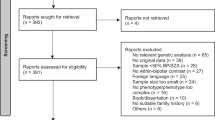
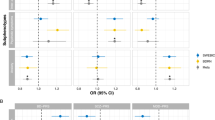
Bipolar disorder is a chronic and complex polygenic disease with high rates of comorbidity. However, the independent contribution of either diagnosis or genetic risk of bipolar disorder to the medical comorbidity profile of individuals with the disease remains unresolved. Here, we conducted a multi-step phenome-wide association study (PheWAS) of bipolar disorder using phenomes derived from the electronic health records of participants enrolled in the Mayo Clinic Biobank and the Mayo Clinic Bipolar Disorder Biobank. First, we explored the conditions associated with a diagnosis of bipolar disorder by conducting a phenotype-based PheWAS followed by LASSO-penalized regression to account for correlations within the phenome. Then, we explored the conditions associated with bipolar disorder polygenic risk score (BD-PRS) using a PRS-based PheWAS with a sequential exclusion approach to account for the possibility that diagnosis, instead of genetic risk, may drive such associations. 53,386 participants (58.7% women) with a mean age at analysis of 67.8 years (SD = 15.6) were included. A bipolar disorder diagnosis (n = 1479) was associated with higher rates of psychiatric conditions, injuries and poisonings, endocrine/metabolic and neurological conditions, viral hepatitis C, and asthma. BD-PRS was associated with psychiatric comorbidities but, in contrast, had no positive associations with general medical conditions. While our findings warrant confirmation with longitudinal-prospective studies, the limited associations between bipolar disorder genetics and medical conditions suggest that shared environmental effects or environmental consequences of diagnosis may have a greater impact on the general medical comorbidity profile of individuals with bipolar disorder than its genetic risk.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
No data were generated as part of this study. We analyzed electronic health record data as well as genetic data from Project Generation, and the authors do not have permissions to publicly share these datasets.
References
Cross-Disorder Group of the Psychiatric Genomics Consortium. Genetic relationship between five psychiatric disorders estimated from genome-wide SNPs. Nat Genet. 2013;45:984–94.
Mullins N, Forstner AJ, O’Connell KS, Coombes B, Coleman JRI, Qiao Z, et al. Genome-wide association study of more than 40,000 bipolar disorder cases provides new insights into the underlying biology. Nat Genet. 2021;53:817–29.
McIntyre RS, Berk M, Brietzke E, Goldstein BI, López-Jaramillo C, Kessing LV, et al. Bipolar disorders. Lancet. 2020;396:1841–56.
Forty L, Ulanova A, Jones L, Jones I, Gordon-Smith K, Fraser C, et al. Comorbid medical illness in bipolar disorder. Br J Psychiatry. 2014;205:465–72.
McElroy SL, Altshuler LL, Suppes T, Keck PE, Frye MA, Denicoff KD, et al. Axis I psychiatric comorbidity and its relationship to historical illness variables in 288 patients with bipolar disorder. AJP. 2001;158:420–6.
Soreca I, Fagiolini A, Frank E, Houck PR, Thompson WK, Kupfer DJ. Relationship of general medical burden, duration of illness and age in patients with bipolar I disorder. J Psychiatr Res. 2008;42:956–61.
He H, Hu C, Ren Z, Bai L, Gao F, Lyu J. Trends in the incidence and DALYs of bipolar disorder at global, regional, and national levels: Results from the global burden of Disease Study 2017. J Psychiatr Res. 2020;125:96–105.
Kilbourne AM, Perron BE, Mezuk B, Welsh D, Ilgen M, Bauer MS. Co-occurring conditions and health-related quality of life in patients with bipolar disorder. Psychosom Med. 2009;71:894–900.
Fullerton JM, Nurnberger JI. Polygenic risk scores in psychiatry: Will they be useful for clinicians? F1000Research. 2019;8:1293.
Lopes FL, Zhu K, Purves KL, Song C, Ahn K, Hou L, et al. Polygenic risk for anxiety influences anxiety comorbidity and suicidal behavior in bipolar disorder. Transl Psychiatry. 2020;10:298.
Sanchez Ruiz JA, Coombes BJ, Pendegraft RS, Ozerdem A, McElroy SL, Cuellar-Barboza AB, et al. Pharmacotherapy exposure as a marker of disease complexity in bipolar disorder: associations with clinical & genetic risk factors. Psychiatry Res. 2023;323:115174.
Coombes BJ, Millischer V, Batzler A, Larrabee B, Hou L, Papiol S, et al. Association of attention-deficit/hyperactivity disorder and depression polygenic scores with lithium response: a Consortium for Lithium Genetics Study. Complex Psychiatry. 2021;7:80–89.
Coombes BJ, Markota M, Mann JJ, Colby C, Stahl E, Talati A, et al. Dissecting clinical heterogeneity of bipolar disorder using multiple polygenic risk scores. Transl Psychiatry. 2020;10:314.
Schubert KO, Thalamuthu A, Amare AT, Frank J, Streit F, Adl M, et al. Combining schizophrenia and depression polygenic risk scores improves the genetic prediction of lithium response in bipolar disorder patients. Transl Psychiatry. 2021;11:606.
Denny JC, Ritchie MD, Basford MA, Pulley JM, Bastarache L, Brown-Gentry K, et al. PheWAS: demonstrating the feasibility of a phenome-wide scan to discover gene-disease associations. Bioinformatics. 2010;26:1205–10.
Linder JE, Bastarache L, Hughey JJ, Peterson JF. The role of electronic health records in advancing genomic medicine. Annu Rev Genom Hum Genet. 2021;22:219–38.
Smoller JW. The use of electronic health records for psychiatric phenotyping and genomics. Am J Med Genet Part B: Neuropsychiatr Genet. 2018;177:601–12.
Bastarache L. Using phecodes for research with the electronic health record: from PheWAS to PheRS. Annu Rev Biomed Data Sci. 2021;4:1–19.
Kember RL, Merikangas AK, Verma SS, Verma A, Judy R, Damrauer SM, et al. Polygenic risk of psychiatric disorders exhibits cross-trait associations in electronic health record data from european ancestry individuals. Biol Psychiatry. 2021;89:236–45.
Fang Y, Fritsche LG, Mukherjee B, Sen S, Richmond-Rakerd LS. Polygenic liability to depression is associated with multiple medical conditions in the electronic health record: phenome-wide association study of 46,782 individuals. Biol Psychiatry. 2022;92:923–31.
Olson JE, Ryu E, Hathcock MA, Gupta R, Bublitz JT, Takahashi PY, et al. Characteristics and utilisation of the Mayo Clinic Biobank, a clinic-based prospective collection in the USA: cohort profile. BMJ Open. 2019;9:e032707.
Frye MA, McElroy SL, Fuentes M, Sutor B, Schak KM, Galardy CW, et al. Development of a bipolar disorder biobank: differential phenotyping for subsequent biomarker analyses. Int J Bipolar Disord. 2015;3:14.
Denny JC, Bastarache L, Ritchie MD, Carroll RJ, Zink R, Mosley JD, et al. Systematic comparison of phenome-wide association study of electronic medical record data and genome-wide association study data. Nat Biotechnol. 2013;31:1102–11.
Wei W-Q, Bastarache LA, Carroll RJ, Marlo JE, Osterman TJ, Gamazon ER, et al. Evaluating phecodes, clinical classification software, and ICD-9-CM codes for phenome-wide association studies in the electronic health record. PLoS ONE. 2017;12:e0175508.
Wu P, Gifford A, Meng X, Li X, Campbell H, Varley T, et al. Mapping ICD-10 and ICD-10-CM codes to Phecodes: workflow development and initial evaluation. JMIR Med Inf. 2019;7:e14325.
Das S, Forer L, Schönherr S, Sidore C, Locke AE, Kwong A, et al. Next-generation genotype imputation service and methods. Nat Genet. 2016;48:1284–7.
Fuchsberger C, Abecasis GR, Hinds DA. minimac2: faster genotype imputation. Bioinformatics. 2015;31:782–4.
Privé F, Arbel J, Vilhjálmsson BJ. LDpred2: better, faster, stronger. Bioinformatics. 2021;36:5424–31.
Denny JC, Bastarache L, Roden DM. Phenome-wide association studies as a tool to advance precision medicine. Annu Rev Genom Hum Genet. 2016;17:353–73.
P. Vatcheva K, Lee M. Multicollinearity in regression analyses conducted in epidemiologic studies. Epidemiology. 2016;06:227 https://doi.org/10.4172/2161-1165.1000227
Low YS, Gallego B, Shah NH. Comparing high-dimensional confounder control methods for rapid cohort studies from electronic health records. J Comp Eff Res. 2016;5:179–92.
Ahuja Y, Kim N, Liang L, Cai T, Dahal K, Seyok T, et al. Leveraging electronic health records data to predict multiple sclerosis disease activity. Ann Clin Transl Neurol. 2021;8:800–10.
Dyas AR, Zhuang Y, Meguid RA, Henderson WG, Madsen HJ, Bronsert MR, et al. Development and validation of a model for surveillance of postoperative bleeding complications using structured electronic health records data. Surgery. 2022;172:1728–32.
Wu Y, Fan J, Peissig P, Berg R, Tafti AP, Yin J, et al. Quantifying predictive capability of electronic health records for the most harmful breast cancer. Proc SPIE Int Soc Opt Eng. 2018;10577:105770J.
Fritsche LG, Gruber SB, Wu Z, Schmidt EM, Zawistowski M, Moser SE, et al. Association of polygenic risk scores for multiple cancers in a phenome-wide study: results from the michigan genomics initiative. Am J Hum Genet. 2018;102:1048–61.
Andreassen OA, Hindley GFL, Frei O, Smeland OB. New insights from the last decade of research in psychiatric genetics: discoveries, challenges and clinical implications. World Psychiatry. 2023;22:4–24.
Carroll RJ, Bastarache L, Denny JC. R PheWAS: data analysis and plotting tools for phenome-wide association studies in the R environment. Bioinformatics. 2014;30:2375–6.
Friedman J, Hastie T, Tibshirani R. Regularization paths for generalized linear models via coordinate descent. J Stat Softw. 2010;33:1–22.
Lenzenweger MF, Lane MC, Loranger AW, Kessler RC. DSM-IV personality disorders in the national comorbidity survey replication. Biol Psychiatry. 2007;62:553–64.
Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RMAA, Petukhova M, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the national comorbidity survey replication. Arch Gen Psychiatry. 2007;64:543–52.
Merikangas KR, Jin R, He J-P, Kessler RC, Lee S, Sampson NA, et al. Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Arch Gen Psychiatry. 2011;68:241.
Schaffer A, Isometsä ET, Tondo L, Moreno DH, Sinyor M, Kessing LV, et al. Epidemiology, neurobiology and pharmacological interventions related to suicide deaths and suicide attempts in bipolar disorder: Part I of a report of the International Society for Bipolar Disorders Task Force on Suicide in Bipolar Disorder. Aust N. Z J Psychiatry. 2015;49:785–802.
Pearlson GD. Etiologic, Phenomenologic, and endophenotypic overlap of schizophrenia and bipolar disorder. Annu Rev Clin Psychol. 2015;11:251–81.
Bowie CR, Best MW, Depp C, Mausbach BT, Patterson TL, Pulver AE, et al. Cognitive and functional deficits in bipolar disorder and schizophrenia as a function of the presence and history of psychosis. Bipolar Disord. 2018;20:604–13.
Van Rheenen TE, Lewandowski KE, Bauer IE, Kapczinski F, Miskowiak K, Burdick KE, et al. Current understandings of the trajectory and emerging correlates of cognitive impairment in bipolar disorder: an overview of evidence. Bipolar Disord. 2020;22:13–27.
Dominiak M, Jażdżyk P, Antosik-Wójcińska AZ, Konopko M, Bieńkowski P, Świȩcicki Ł, et al. The impact of bipolar spectrum disorders on professional functioning: a systematic review. Front Psychiatry. 2022;13:951008.
Sinha A, Shariq A, Said K, Sharma A, Jeffrey Newport D, Salloum IM. Medical comorbidities in bipolar disorder. Curr Psychiatry Rep. 2018;20:36.
Matthews AM, Huckans MS, Blackwell AD, Hauser P. Hepatitis C testing and infection rates in bipolar patients with and without comorbid substance use disorders. Bipolar Disord. 2008;10:266–70.
Henriques F, Ferreira AR, Gonçalves-Pinho M, Freitas A, Fernandes L. Bipolar disorder and medical comorbidities: A Portuguese population-based observational retrospective study (2008–2015). J Affect Disord. 2022;298:232–8.
Huhn M, Nikolakopoulou A, Schneider-Thoma J, Krause M, Samara M, Peter N, et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and network meta-analysis. Lancet. 2019;394:939–51.
Zhang J-P, Gallego JA, Robinson DG, Malhotra AK, Kane JM, Correll CU. Efficacy and safety of individual second-generation vs. first-generation antipsychotics in first-episode psychosis: a systematic review and meta-analysis. Int J Neuropsychopharmacol. 2013;16:1205–18.
McKnight RF, Adida M, Budge K, Stockton S, Goodwin GM, Geddes JR. Lithium toxicity profile: a systematic review and meta-analysis. Lancet. 2012;379:721–8.
Gitlin M. Lithium side effects and toxicity: prevalence and management strategies. Int J Bipolar Disord. 2016;4:27.
Tabák AG, Jokela M, Akbaraly TN, Brunner EJ, Kivimäki M, Witte DR. Trajectories of glycaemia, insulin sensitivity, and insulin secretion before diagnosis of type 2 diabetes: an analysis from the Whitehall II study. Lancet. 2009;373:2215–21.
Fürtjes AE, Coleman JRI, Tyrrell J, Lewis CM, Hagenaars SP. Associations and limited shared genetic aetiology between bipolar disorder and cardiometabolic traits in the UK Biobank. Psychol Med. 2021;52:1–10.
Lindekilde N, Scheuer SH, Rutters F, Knudsen L, Lasgaard M, Rubin KH, et al. Prevalence of type 2 diabetes in psychiatric disorders: an umbrella review with meta-analysis of 245 observational studies from 32 systematic reviews. Diabetologia. 2022;65:440–56.
Vancampfort D, Mitchell AJ, De Hert M, Sienaert P, Probst M, Buys R, et al. Prevalence and predictors of type 2 diabetes mellitus in people with bipolar disorder: a systematic review and meta-analysis. J Clin Psychiatry. 2015;76:1490–9.
Liu YK, Ling S, Lui LMW, Ceban F, Vinberg M, Kessing LV, et al. Prevalence of type 2 diabetes mellitus, impaired fasting glucose, general obesity, and abdominal obesity in patients with bipolar disorder: a systematic review and meta-analysis. J Affect Disord. 2022;300:449–61.
Miola A, Alvarez-Villalobos NA, Ruiz-Hernandez FG, De Filippis E, Veldic M, Prieto ML, et al. Insulin resistance in bipolar disorder: A systematic review of illness course and clinical correlates. J Affect Disord. 2023;334:1–11.
McIntyre RS, Soczynska JK, Woldeyohannes HO, Miranda A, Vaccarino A, MacQueen G, et al. A randomized, double-blind, controlled trial evaluating the effect of intranasal insulin on neurocognitive function in euthymic patients with bipolar disorder: Intranasal insulin in bipolar disorder. Bipolar Disord. 2012;14:697–706.
Miola A, De Filippis E, Veldic M, Ho AM-C, Winham SJ, Mendoza M, et al. The genetics of bipolar disorder with obesity and type 2 diabetes. J Affect Disord. 2022;313:222–31.
Sabé M, Pallis K, Solmi M, Crippa A, Sentissi O, Kaiser S. Comparative effects of 11 antipsychotics on weight gain and metabolic function in patients with acute schizophrenia: a dose-response meta-analysis. J Clin Psychiatry. 2023;84:22r14490 https://doi.org/10.4088/JCP.22r14490
MDD Working Group of the Psychiatric Genomics Consortium, Cai N, Revez JA, Adams MJ, Andlauer TFM, Breen G, et al. Minimal phenotyping yields genome-wide association signals of low specificity for major depression. Nat Genet. 2020;52:437–47.
Flint J. The genetic basis of major depressive disorder. Mol Psychiatry. 2023;28:2254–65. https://doi.org/10.1038/s41380-023-01957-9
Wolford BN, Willer CJ, Surakka I. Electronic health records: the next wave of complex disease genetics. Hum Mol Genet. 2018;27:R14–R21.
Gianfrancesco MA, Goldstein ND. A narrative review on the validity of electronic health record-based research in epidemiology. BMC Med Res Methodol. 2021;21:234.
Davis K, Ballreich J. Equitable access to care — how the united states ranks internationally. N Engl J Med. 2014;371:1567–70.
Zhao L, Chang H, Zhou D-S, Cai J, Fan W, Tang W, et al. Replicated associations of FADS1, MAD1L1, and a rare variant at 10q26.13 with bipolar disorder in Chinese population. Transl Psychiatry. 2018;8:270.
Schultz LM, Merikangas AK, Ruparel K, Jacquemont S, Glahn DC, Gur RE, et al. Stability of polygenic scores across discovery genome-wide association studies. HGG Adv. 2022;3:100091.
Acknowledgements
The Mayo Clinic Bipolar Disorder Biobank was supported by the Marriott Foundation, and this study was supported by the Thomas and Elizabeth Grainger Fund in Bipolar Functional Genomics and Drug Development, and National Institute of Mental Health grant R01MH121924. The Mayo Clinic Biobank and Project Generation were supported in part by Mayo Clinic Center for Individualized Medicine. We acknowledge Regeneron Genetics Center for providing the genetic data for Mayo Clinic Biobank participants, and a subset of participants in the Bipolar Biobank. We also acknowledge the Mayo Clinic Biobank and Mayo Clinic Bipolar Biobank research teams as well as the patient-participants who consented to participate in these research programs.
Author information
Authors and Affiliations
Contributions
Jorge A. Sanchez-Ruiz: Conceptualization, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. Brandon J. Coombes: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Writing – original draft, Writing – review & editing. Vanessa M. Pazdernik: Conceptualization, Data curation, Formal analysis, Methodology, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. Lindsay M. Melhuish Beaupre: Conceptualization, Validation, Writing – original draft, Writing – review & editing. Greg D. Jenkins and Richard S. Pendegraft: Conceptualization, Data curation, Software, Validation. Anthony Batzler: Conceptualization, Data curation, Software. Aysegul Ozerdem: Conceptualization, Methodology, Supervision, Writing – review & editing. Susan L. McElroy, Manuel A. Gardea-Resendez, Alfredo B. Cuellar-Barboza, and Miguel L. Prieto: Conceptualization, Investigation, Resources, Writing – review & editing. Regeneron Genetics Center: Investigation. Mark A. Frye: Conceptualization, Funding acquisition, Investigation, Project administration, Resources, Supervision, Validation, Writing – review & editing. Joanna M. Biernacka: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing. All authors have contributed to and approved the final manuscript. This manuscript has not been published elsewhere nor submitted for publication to another journal.
Corresponding author
Ethics declarations
Competing interests
SLM reports receiving personal fees for advisory boards and/or consultation from Idorsia, Levo, Novo Nordisk, Otsuka, Sunovion, and Takeda; receiving grant support from Idorsia, Janssen, Marriott Foundation, Myriad, National Institute of Mental Health, Novo Nordisk, Otsuka, and Sunovion; and receiving payments from Johnson & Johnson for being an inventor on US Patent No. 6,323,236 B2. ABCB has received lecture and consulting fees from Asofarma and Exeltis. MLP has served on an advisory board for Janssen and has received grant support from ANID FONDECYT Regular 1181365, FONDEF ID19I10116 and Basal Funding for Scientific and Technological Center of Excellence, IMPACT, #FB210024. MAF reports the following conflicts of interest: grant support from Assurex Health and Mayo Foundation; CME/travel/honoraria from Carnot Laboratories, American Physician Institute; and financial interest/stock ownership/royalties in Chymia LLC. All other authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sanchez-Ruiz, J.A., Coombes, B.J., Pazdernik, V.M. et al. Clinical and genetic contributions to medical comorbidity in bipolar disorder: a study using electronic health records-linked biobank data. Mol Psychiatry (2024). https://doi.org/10.1038/s41380-024-02530-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41380-024-02530-8