Abstract
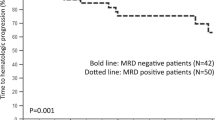
Organ recovery following anti-plasma cell therapy is associated with improved outcome in patients with AL amyloidosis. Current organ response criteria do not consider the depth of response. Newly diagnosed AL amyloidosis patients who had involvement of at least one evaluable organ and documentation of organ response were included. Cardiac response was seen in 182 patients. Time to cardiac response was 9.4 months. Renal response was seen in 278 patients, at a median time to response of 6 months. Hepatic response was seen in 70 patients, with a median time to response of 6.1 months. In all organs, the deeper the organ response achieved, the longer the survival. This led to four organ response criteria: complete organ response (nadir NT-proBNP ≤400 pg/mL; nadir proteinuria ≤200 mg per 24 h; nadir alkaline phosphatase ≤×2 lower limit of normal); very good partial organ response (>60% reduction in parameter not meeting complete organ response definition); partial organ response (31–60% reduction in parameter); and non-responder (≤30% reduction in organ response parameter). Cardiac and renal progression were associated with baseline organ impairment and inversely associated with the depth of organ response. Grading the depth of organ response provides additional valuable prognostic information for newly diagnosed AL amyloidosis patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Merlini G, Bellotti V. Molecular mechanisms of amyloidosis. N Engl J Med. 2003;349:583–96.
Dispenzieri A, Lacy MQ, Katzmann JA, Rajkumar SV, Abraham RS, Hayman SR, et al. Absolute values of immunoglobulin free light chains are prognostic in patients with primary systemic amyloidosis undergoing peripheral blood stem cell transplantation. Blood. 2006;107:3378–83.
Gertz MA, Kyle RA, Greipp PR. Response rates and survival in primary systemic amyloidosis. Blood. 1991;77:257–62.
Kaufman GP, Dispenzieri A, Gertz MA, Lacy MQ, Buadi FK, Hayman SR, et al. Kinetics of organ response and survival following normalization of the serum free light chain ratio in AL amyloidosis. Am J Hematol. 2015;90:181–6.
Palladini G, Hegenbart U, Milani P, Kimmich C, Foli A, Ho AD, et al. A staging system for renal outcome and early markers of renal response to chemotherapy in AL amyloidosis. Blood. 2014;124:2325–32.
Palladini G, Dispenzieri A, Gertz MA, Kumar S, Wechalekar A, Hawkins PN, et al. New criteria for response to treatment in immunoglobulin light chain amyloidosis based on free light chain measurement and cardiac biomarkers: impact on survival outcomes. J Clin Oncol. 2012;30:4541–9.
Gertz MA, Comenzo R, Falk RH, Fermand JP, Hazenberg BP, Hawkins PN, et al. Definition of organ involvement and treatment response in immunoglobulin light chain amyloidosis (AL): a consensus opinion from the 10th International Symposium on Amyloid and Amyloidosis, Tours, France, 18-22 April 2004. Am J Hematol. 2005;79:319–28.
Palladini G, Merlini G. What is new in diagnosis and management of light chain amyloidosis? Blood. 2016;128:159–68.
Muchtar E, Gertz MA, Kumar SK, Lacy MQ, Dingli D, Buadi FK, et al. Improved outcomes for newly diagnosed AL amyloidosis over the years 2000-14: cracking the glass ceiling of early death. Blood. 2017;129:2111–2119.
Cibeira MT, Sanchorawala V, Seldin DC, Quillen K, Berk JL, Dember LM, et al. Outcome of AL amyloidosis after high-dose melphalan and autologous stem cell transplantation: long-term results in a series of 421 patients. Blood. 2011;118:4346–52.
Gertz MA, Lacy MQ, Dispenzieri A, Hayman SR, Kumar SK, Dingli D, et al. Autologous stem cell transplant for immunoglobulin light chain amyloidosis: a status report. Leuk Lymphoma. 2010;51:2181–7.
Leung N, Glavey SV, Kumar S, Dispenzieri A, Buadi FK, Dingli D, et al. A detailed evaluation of the current renal response criteria in AL amyloidosis: is it time for a revision? Haematologica. 2013;98:988–92.
Michael M, Kastritis E, Delimpassi S, Michalis E, Repoussis P, Kyrtsonis MC, et al. Clinical characteristics and outcome of primary systemic light-chain amyloidosis in Greece. Clin Lymphoma Myeloma Leuk. 2010;10:56–61.
Rosengren S, Mellqvist UH, Nahi H, Forsberg K, Lenhoff S, Stromberg O, et al. Outcome of AL amyloidosis after high-dose melphalan and autologous stem cell transplantation in Sweden, long-term results from all patients treated in 1994-2009. Bone Marrow Transplant. 2016;51:1569–72.
Dittrich T, Bochtler T, Kimmich C, Becker N, Jauch A, Goldschmidt H, et al. AL amyloidosis patients with low amyloidogenic free light chain levels at first diagnosis have an excellent prognosis. Blood. 2017;130:632–42.
Milani P, Basset M, Russo F, Foli A, Merlini G, Palladini G. Patients with light-chain amyloidosis and low free light-chain burden have distinct clinical features and outcome. Blood. 2017;130:625–31.
Sidana S, Tandon N, Dispenzieri A, Gertz MA, Buadi FK, Lacy MQ, et al. Clinical presentation and outcomes in light chain amyloidosis patients with non-evaluable serum free light chains. Leukemia. 2017. doi: 10.1038/leu.2017.286. [Epub ahead of print].
Edwards CV, Gould J, Langer AL, Mapara M, Radhakrishnan J, Maurer MS. et al. Analysis of the phase 1a/b study of chimeric fibril-reactive monoclonal antibody 11-1F4 in patients with AL amyloidosis. Blood. 2016;128:643
Gertz MA, Landau H, Comenzo RL, Seldin D, Weiss B, Zonder J, et al. First-in-human phase I/II study of NEOD001 in patients with light chain amyloidosis and persistent organ dysfunction. J Clin Oncol. 2016;34:1097–103.
Gertz MA, Landau HJ, Weiss BM. Organ response in patients with AL amyloidosis treated with NEOD001, an amyloid-directed monoclonal antibody. Am J Hematol. 2016;91:E506–8.
Pepys MB, Herbert J, Hutchinson WL, Tennent GA, Lachmann HJ, Gallimore JR, et al. Targeted pharmacological depletion of serum amyloid P component for treatment of human amyloidosis. Nature. 2002;417:254–9.
Comenzo RL, Reece D, Palladini G, Seldin D, Sanchorawala V, Landau H, et al. Consensus guidelines for the conduct and reporting of clinical trials in systemic light-chain amyloidosis. Leukemia. 2012;26:2317–25.
Acknowledgements
The study was supported in part by the Jabbs Foundation (Birmingham, UK), the Henry J. Predolin Foundation (USA), and National Institutes of Health National Cancer Institute grant P50 CA186781.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A.D. received research funding from Celgene, Millennium, Pfizer, and Janssen and travel grant from Pfizer. M.Q.L. received research funding from Celgene. D.D. received research funding from Karyopharm Therapeutics, Amgen, and Millenium Pharmaceuticals. P.K. received research funding from Takeda, Celgene, and Amgen. S.K.K. received consultancy from Celgene, Millennium, Onyx, Janssen, and BMS, and research funding from Celgene, Millennium, Novartis, Onyx AbbVie, Janssen, and BMS. M.A.G. received consultancy from Millenium and honoraria from Celgene, Millenium, Onyx, Novartis, Smith Kline, Prothena, Ionis, and Amgen. The remaining authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Muchtar, E., Dispenzieri, A., Leung, N. et al. Depth of organ response in AL amyloidosis is associated with improved survival: grading the organ response criteria. Leukemia 32, 2240–2249 (2018). https://doi.org/10.1038/s41375-018-0060-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-018-0060-x
This article is cited by
-
Pathway for Development and Validation of Multi-domain Endpoints for Amyloid Light Chain (AL) Amyloidosis
Therapeutic Innovation & Regulatory Science (2024)
-
Value of repeat renal biopsy in the evaluation of AL amyloidosis patients lacking renal response despite of complete hematologic remission: a case report and literature review
BMC Nephrology (2022)
-
Depth of response prior to autologous stem cell transplantation predicts survival in light chain amyloidosis
Bone Marrow Transplantation (2021)
-
Systemic amyloidosis: moving into the spotlight
Leukemia (2020)
-
Updates in the Diagnosis and Management of AL Amyloidosis
Current Hematologic Malignancy Reports (2020)