Abstract
Objective
Test sustainability of Web-based Implementation for the Science of Enhancing Resilience (WISER) intervention efficacy in reducing healthcare worker (HCW) emotional exhaustion (EE), a key component of burnout.
Design
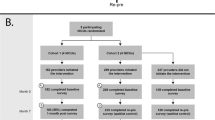
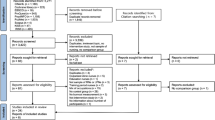
One-year follow-up of WISER RCT using two cohorts (one waitlist control with shortened intervention period) of HCWs of four NICUs each, to improve HCW well-being (primary outcome: EE).
Results
In Cohorts 1 and 2, 194 and 312 WISER initiators were identified by 1-year, and 99 and 80 completed 1-year follow-up, respectively. Combined cohort results showed that relative to baseline, at 1-year WISER decreased EE (−7.07 (95%CI: −10.22, −3.92), p < 0.001), depression (−4.49 (−6.81, −2.16), p = <0.001), and improved work-life integration (6.08 (4.25, 7.90), p = <0.001). EE continued to decline between 6-month and 1-year follow-up (p = 0.022). The percentage of HCWs reporting concerning outcomes was significantly decreased for EE (−10.9% (95%CI: −17.9%, −4.9%); p < 0.001), and secondary outcomes depression and work-life integration.
Conclusion
WISER improves HCW well-being for at least 1 year.
Clinical Trials Number
NCT02603133; https://clinicaltrials.gov/ct2/show/NCT02603133
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The authors will share survey data from the study upon reasonable request to the corresponding author.
References
Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136:358–67.
Cimiotti JP, Aiken LH, Sloane DM, Wu ES. Nurse staffing, burnout, and health care-associated infection. Am J Infect Control. 2012;40:486–90.
Tawfik DS, Profit J, Morgenthaler TI, Satele CA, Sinsky CA, Dyrbye LN, et al. Physician Burnout, Well-being, and Work Unit Safety Grades in Relationship to Reported Medical Errors. Mayo Clin Proc. 2018;93:1571–80.
Fibuch E, Ahmed A. Physician turnover: a costly problem. Physician Leadersh J. 2015;2:22–5.
Schloss EP, Flanagan DM, Culler CL, Wright AL. Some hidden costs of faculty turnover in clinical departments in one academic medical center. Acad Med. 2009;84:32–6.
Shanafelt TD, Mungo M, Schmitgen J, Storz KA, Reeves D, Hayes SN, et al. Longitudinal Study Evaluating the Association Between Physician Burnout and Changes in Professional Work Effort. Mayo Clin Proc Mayo Clin. 2016;91:422–31.
Profit J, Adair KC, Cui X, Mitchell B, Brandon D, Tawfik DS, et al. Randomized controlled trial of the “WISER” intervention to reduce healthcare worker burnout. J Perinatol. 2021;41:2225–34.
Sexton JB, Adair KC, Proulx J, Profit J, Cui X, Bae J, et al. Emotional Exhaustion Among US Health Care Workers Before and During the COVID-19 Pandemic, 2019-2021. Jama Netw Open. 2022;5:e2232748. https://doi.org/10.1001/jamanetworkopen.2022.32748.
Sexton JB, Adair KC, Leonard MW, Frankel TC, Proulx J, Watson SR, et al. Providing feedback following Leadership WalkRounds is associated with better patient safety culture, higher employee engagement and lower burnout. BMJ Qual Saf. 2018;27:261–70. https://doi.org/10.1136/bmjqs-2016-006399.
Schwartz SP, Adair KC, Bae J, Rehder KJ, Shanafelt TD, Profit J, et al. Work-life balance behaviours cluster in work settings and relate to burnout and safety culture: a cross-sectional survey analysis. BMJ Qual Saf. 2019;28:142–50. https://doi.org/10.1136/bmjqs-2018-007933.
Sexton JB, Schwartz SP, Chadwick WA, Rehder KJ, Bae J, Bokovoy J, et al. The associations between work-life balance behaviours, teamwork climate and safety climate: cross-sectional survey introducing the work-life climate scale, psychometric properties, benchmarking data and future directions. BMJ Qual Saf. 2017;26:632–40.
Adair KC, Kennedy LA, Sexton JB. Three Good Tools: Positively reflecting backwards and forward is associated with robust improvements in well-being across three distinct interventions. J Posit Psychol. 2020;15:613–22.
Sexton JB, Adair KC. Forty-five good things: a prospective pilot study of the Three Good Things well-being intervention in the USA for healthcare worker emotional exhaustion, depression, work-life balance and happiness. BMJ Open. 2019;9:e022695.
Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994;10:77–84.
Lyubomirsky S, Ross L. Changes in attractiveness of elected, rejected, and precluded alternatives: a comparison of happy and unhappy individuals. J Pers Soc Psychol. 1999;76:988–1007.
Howell RT, Rodzon KS, Kurai M, Sanchez AH. A validation of well-being and happiness surveys for administration via the Internet. Behav Res Methods. 2010;42:775–84.
West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388:2272–81.
Han S, Shanafelt TD, Sinsky CA, Awad KM, Dyrbye LN, Fiscus LC, et al. Estimating the Attributable Cost of Physician Burnout in the United States. Ann Intern Med. 2019;170:784–90.
Sexton JB, Adair KC, Cui X, Tawfik DS, Profit J. Effectiveness of a bite-sized web-based intervention to improve healthcare worker wellbeing: A randomized clinical trial of WISER. Front Public Health. 2022;10:1016407.
Acknowledgements
We would like to thank the HCWs at the participating institutions: it is their time, thoughtfulness, meaningful contributions, and steadfast dedication to patient-centered care that taught us so much about how to adapt and improve this intervention. In addition, we would like to thank the site principal investigators: Wendy L. Timpson, Martin J. McCaffrey, Alexis S. Davis, Mohan Pammi, Melissa Mathews, Ann R. Stark, LuAnn Papile, Eric Thomas, Michael Cotten, Amir Khan. Finally, we are grateful to the site nurse leads who helped with the intervention: Debra Brendon, Florence Chow, Marlee Crankshaw, Lisa Criscoe, Melissa DeColo, Nicole Francis, Kim Jacobs, Belinda Mathis, Nancy Morris, Krista Moses, Rebecca Schiff, Amy Toronto, and Karen Waldo.
Funding
This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development [R01 HD084679-01, Co-PI: Sexton and Profit].
Author information
Authors and Affiliations
Contributions
Dr. Profit conceptualized and designed the study, assisted in data analysis and interpretation, critically reviewed the manuscript, and approved the final manuscript as submitted. Dr. Adair assisted in analysis and interpretation of the data, critically reviewed the manuscript, and approved the final manuscript as submitted. Dr. Tawfik assisted in analysis and interpretation of the data, critically reviewed the manuscript, and approved the final manuscript as submitted. Dr. Cui coordinated the data management and carried out the initial data analyses, critically reviewed the manuscript, and approved the final manuscript as submitted. Dr. Sexton created WISER, conceptualized and designed the study, assisted in data analysis and interpretation, critically reviewed the manuscript, and approved the final manuscript as submitted. All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study was approved by Duke University and Stanford University.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Profit, J., Cui, X., Tawfik, D. et al. “WISER” intervention to reduce healthcare worker burnout – 1 year follow up. J Perinatol (2024). https://doi.org/10.1038/s41372-024-01993-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41372-024-01993-5