Abstract
Objective
We aimed to correlate photoplethysmographic parameters with stroke volume in infants with PDA. Photoplethysmography constitutes the optical signal in pulse oximetry.
Study design
Stroke volume was determined echocardiographically. Pulse transit time, right hand to foot arrival time difference, and relative amplitude were measured from pulse oximeter and ECG waveforms. Photoplethysmographic parameters before and after PDA closure were compared with stroke volume.
Results
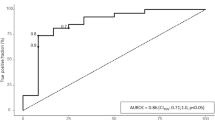
After PDA closure, pulse transit time to the hand and to the foot were prolonged (54.7 ± 6.7 vs 65.5 ± 9.8 ms, p < 0.001, 82.5 ± 12.8 vs 88.6 ± 10.6 ms, p = 0.03), arrival time difference decreased (27.7 ± 7.6 vs 23.1 ± 5.6 ms, p = 0.021), and relative amplitude decreased (from 2.1 ± 0.7% to 1.5 ± 0.5%, p = 0.003). The time-based photoplethysmographic parameters correlated with stroke volume.
Conclusions
Photoplethysmographic waveform parameters are significantly different before and after PDA closure and the time-based parameters correlate well with stroke volume. Monitoring pulse transit time may assist in evaluation for spontaneous PDA closure or response to therapy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
McNamara PJ, Sehgal A. Towards rational management of the patent ductus arteriosus: the need for disease staging. Arch Dis Child Fetal Neonatal Ed. 2007;92:F424–7.
Ngo S, Profit J, Gould JB, Lee HC. Trends in patent ductus arteriosus diagnosis and management for very low birth weight infants. Pediatrics. 2017;139:e20162390.
Sehgal A, McNamara PJ. The ductus arteriosus: a refined approach! Semin Perinatol. 2012;36:105–13.
Lemmers PMA, Benders MJNL, D’Ascenzo R, Zethof J, Alderliesten T, Kersbergen KJ, et al. Patent ductus arteriosus and brain volume. Pediatrics. 2016;137:e20153090.
Roze JC, Cambonie G, Marchand-Martin L, Gournay V, Durmeyer X, Durox M, et al. Association between early screening for patent ductus arteriosus and in-hospital mortality among extremely preterm infants. JAMA. 2015;313:2441–8.
Noori S. Patent ductus arteriosus in the preterm infant: to treat or not to treat? J Perinatol. 2010;30:S31–7.
Evans N. Diagnosis of the preterm patent ductus arteriosus: clinical signs, biomarkers, or ultrasound? Semin Perinatol. 2012;36:114–22.
Skelton R, Evans N, Smythe J. A blinded comparison of clinical and echocardiographic evaluation of the preterm infant for patent ductus arteriosus. J Paediatr Child Health. 1994;30:406–11.
Fink D, El-Khuffash A, McNamara PJ, Nitzan I, Hammerman C. Tale of two ductus arteriosus severity scores: similarities and differences. Am J Perinatol. 2018;35:55–8.
Allen J. Photoplethysmography and its application in clinical physiological measurement. Physiol Meas. 2007;28:R1–39.
Sinha IP, Mayell SJ, Halfhide C. Pulse oximetry in children. Arch Dis Child Educ Pract. 2014;99:117–8.
Nitzan M, Engelberg S. Three-wavelength technique for the measurement of oxygen saturation in arterial blood and in venous blood. J Biomed Opt. 2009;14:024046.
Lundell BP. Pulse wave patterns in patent ductus arteriosus. Arch Dis Child. 1983;58:682–5.
Noori S, Seri I. The very low birth weight neonate with a hemodynamically significant ductus arteriosus during the first postnatal week. In: Kleinman CS, Seri I, editors. Questions and controversies: cardiovascular. Philadelphia: Saunders; 2008. p. 178–94.
Babchenko A, Davidson E, Ginosar Y, Kurtz V, Feib I, Adler D, et al. Photoplethysmographic measurement of changes in total and pulsatile tissue blood volume following sympathetic blockade. Physiol Meas. 2001;22:389–96.
Geddes LA, Voelz MH, Babbs CF, Bourland JD, Tacker WA. Pulse transit time as an indicator of arterial blood pressure. Psychophysiology. 1981;18:71–4.
Payne RA, Symeonides CN, Webb DJ, Maxwell SR. Pulse transit time measured from the ECG: an unreliable marker of beat-to-beat blood pressure. J Appl Physiol. 2006;100:136–41.
Nichols W, O’Rourke M, Vlachopoulos C. McDonald’s blood flow in arteries: theoretical, experimental and clinical principles. 6th ed. Boca Raton: CRC Press; 2011. p. 55–76.
Mahfouz RA, Alzaiat A, Gad M. Association of aortic stiffness to brain natriuretic peptide in children before and after device closure of patent ductus arteriosus. J Saudi Heart Assoc. 2015;27:23–30.
Terrin G, Conte F, Oncel MY, Scipione A, McNamara PJ, Simons S, et al. Paracetamol for the treatment of patent ductus arteriosus in preterm neonates: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2016;101:F127–6.
Benitz WE, Committee on Fetus and Newborn. Patent ductus arteriosus in preterm infants. Pediatrics. 2016;137:e20153730.
Semberova J, Sirc J, Miletin J, Kucera J, Berka I, Sebkova S, et al. Spontaneous closure of patent ductus arteriosus in infants <1500 g. Pediatrics. 2017;140:e20164258
Hamrick SEG, Hansmann G. Patent ductus arteriosus of the preterm infant. Pediatrics. 2010;125:1020.
Evans N. Preterm patent ductus arteriosus: a continuing conundrum for the neonatologist? Semin Fetal Neonatal Med. 2015;20:272–7.
El-Khuffash AF, Slevin M, McNamara PJ, Molloy EJ. Troponin T. N-terminal pro natriuretic peptide and a patent ductus arteriosus scoring system predict death before discharge or neurodevelopmental outcome at 2 years in preterm infants. Arch Dis Child Fetal Neonatal Ed. 2011;96:F133–7.
Khan SS, Sithisarn T, Bada HS, Vranicar M, Westgate PM, Hanna M. Urinary NT-proBNP levels and echocardiographic parameters for patent ductus arteriosus. J Perinatol. 2017;37:1319–24.
Gomez-Pomar E, Makhoul M, Westgate PM, Ibonia KT, Patwardhan A, Giannone PJ, et al. Relationship between perfusion index and patent ductus arteriosus in preterm infants. Pediatr Res. 2017;81:775–9.
Author contributions
C.A. helped design the study, performed the data collection, analyzed the clinical and echocardiographic data of study patients with P.D.A, drafted the initial manuscript, critically reviewed the manuscript, and approved the final manuscript as submitted. L.P. performed the data collection, drafted the initial manuscript, critically reviewed the manuscript, and approved the final manuscript as submitted. G.G. designed and performed the digital signal analysis, and approved the final manuscript as submitted. Y.A. designed and built the PPG device and the associated data acquisition system and approved the final manuscript as submitted. M.N. helped design the study, designed the technological aspects of the study, verified the signal analysis, helped in the interpretation of the results, critically reviewed the manuscript, and approved the final manuscript as submitted. A.B. helped design the study, critically reviewed the manuscript, and approved the final manuscript as submitted. D.M. performed the surgical ligations and reviewed and approved the final manuscript as submitted. E.K. analyzed the echocardiographic data of the study patients and approved the final manuscript as submitted. D.G. performed the data analysis, critically reviewed the manuscript, and approved the final manuscript as submitted. R.K. conceptualized and designed the study, supervised data collection, critically reviewed the manuscript, and approved the final manuscript as submitted. All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Amirtharaj, C.R., Palmeri, L.C., Gradwohl, G. et al. Photoplethysmographic assessment of pulse transit time correlates with echocardiographic measurement of stroke volume in preterm infants with patent ductus arteriosus. J Perinatol 38, 1220–1226 (2018). https://doi.org/10.1038/s41372-018-0165-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0165-0
This article is cited by
-
Assessing patent ductus arteriosus in preterm infants from standard neonatal intensive care monitoring
European Journal of Pediatrics (2022)
-
Using pulse oximetry waveforms to detect coarctation of the aorta
BioMedical Engineering OnLine (2020)