Abstract
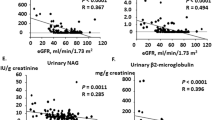
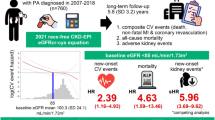
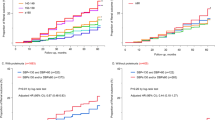
Little is known regarding the association of blood pressure (BP) after treatment for primary aldosteronism (PA) (i.e., adrenalectomy and mineralocorticoid receptor antagonists) with long-term renal outcomes, and whether the association is independent of BP before treatment. Using a dataset from a nationwide registry of PA in Japan, we assessed whether achieved BP levels 6 months after treatment for PA are associated with annual changes in estimated glomerular filtration rate (eGFR), rapid eGFR decline, and incident chronic kidney disease (CKD) during the 5-year follow-up period. The cohort included 1266 PA patients. In multivariable linear regression including systolic BP (SBP) levels before treatment for PA, estimates (95% confidence interval [CI]) for annual changes in eGFR after month 6 associated with one-standard deviation (1-SD) higher SBP at month 6 were –0.08 (–0.15, –0.02) mL/min/1.73 m2/year. After multivariable adjustment, the estimate (95% CI) for annual changes in eGFR after month 6 was –0.12 (–0.21, –0.02) for SBP ≥ 130 mmHg vs. SBP < 130 mmHg at month 6. Among 537 participants without CKD at baseline, a 1-SD higher SBP was associated with a higher risk for incident CKD events (hazard ratio [95% CI]: 1.40 [1.00, 1.94]). Higher SBP after treatment for PA was associated with a higher risk for kidney dysfunction over time, independently of BP levels before treatment. Achieving SBP lower than 130 mmHg after treatment for PA may be linked to better kidney outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Nishikawa T, Omura M, Satoh F, Shibata H, Takahashi K, Tamura N, et al. Guidelines for the diagnosis and treatment of primary aldosteronism—the Japan Endocrine Society 2009. Endocr J. 2011;58:711–21.
Monticone S, Burrello J, Tizzani D, Bertello C, Viola A, Buffolo F, et al. Prevalence and clinical manifestations of primary aldosteronism encountered in primary care practice. J Am Coll Cardiol. 2017;69:1811–20.
Brown NJ. Contribution of aldosterone to cardiovascular and renal inflammation and fibrosis. Nat Rev Nephrol. 2013;9:459–69.
Hundemer GL, Curhan GC, Yozamp N, Wang M, Vaidya A. Renal outcomes in medically and surgically treated primary aldosteronism. Hypertension. 2018;72:658–66.
Monticone S, Sconfienza E, D'ascenzo F, Buffolo F, Satoh F, Sechi LA, et al. Renal damage in primary aldosteronism: a systematic review and meta-analysis. J Hypertens. 2020;38:3–12.
Sechi LA, Novello M, Lapenna R, Baroselli S, Nadalini E, Colussi GL, et al. Long-term renal outcomes in patients with primary aldosteronism. JAMA. 2006;295:2638–45.
Iwakura Y, Morimoto R, Kudo M, Ono Y, Takase K, Seiji K, et al. Predictors of decreasing glomerular filtration rate and prevalence of chronic kidney disease after treatment of primary aldosteronism: renal outcome of 213 cases. J Clin Endocrinol Metab. 2014;99:1593–8.
Haze T, Hirawa N, Yano Y, Tamura K, Kurihara I, Kobayashi H, et al. Association of aldosterone and blood pressure with the risk for cardiovascular events after treatments in primary aldosteronism. Atherosclerosis. 2021;324:84–90.
Kobayashi Y, Haze T, Yano Y, Tamura K, Kurihara I, Ichijo T, et al. Associations between changes in plasma renin activity and aldosterone concentrations and changes in kidney function after treatment for primary aldosteronism. Kidney Int Rep. 2020;5:1291–7.
Kobayashi H, Abe M, Nakamura Y, Takahashi K, Fujita M, Takeda Y, et al. Association between acute fall in estimated glomerular filtration rate after treatment for primary aldosteronism and long-term decline in renal function. Hypertension. 2019;74:630–8.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2014). Hypertens Res. 2014;37:253–390.
Moriya A, Yamamoto M, Kobayashi S, Nagamine T, Takeichi-Hattori N, Nagao M, et al. ACTH stimulation test and computed tomography are useful for differentiating the subtype of primary aldosteronism. Endocr J. 2017;64:65–73.
Kempers MJ, Lenders JW, van Outheusden L, van der Wilt GJ, Schultze Kool LJ, Hermus AR, et al. Systematic review: diagnostic procedures to differentiate unilateral from bilateral adrenal abnormality in primary aldosteronism. Ann Intern Med. 2009;151:329–37.
Committee of the Japan Diabetes Society on the Diagnostic Criteria of Diabetes Mellitus, Seino Y, Nanjo K, Tajima N, Kadowaki T, Kashiwagi A, et al. Report of the committee on the classification and diagnostic criteria of diabetes mellitus. J Diabetes Investig. 2010;1:212–28.
Horio M, Imai E, Yasuda Y, Watanabe T, Matsuo S. Modification of the CKD epidemiology collaboration (CKD-EPI) equation for Japanese: accuracy and use for population estimates. Am J Kidney Dis. 2010;56:32–38.
Perkins BA, Ficociello LH, Ostrander BE, Silva KH, Weinberg J, Warram JH, et al. Microalbuminuria and the risk for early progressive renal function decline in type 1 diabetes. JASN 2007;18:1353–61.
Krolewski AS, Niewczas MA, Skupien J, Gohda T, Smiles A, Eckfeldt JH, et al. Early progressive renal decline precedes the onset of microalbuminuria and its progression to macroalbuminuria. Diabetes Care. 2014;37:226–34.
Turin TC, Coresh J, Tonelli M, Stevens PE, de Jong PE, Farmer CK, et al. Change in the estimated glomerular filtration rate over time and risk of all-cause mortality. Kidney Int. 2013;83:684–91.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 2012;2013 (Suppl 3):1–150.
Irie F, Iso H, Sairenchi T, Fukasawa N, Yamagishi K, Ikehara S, et al. The relationships of proteinuria, serum creatinine, glomerular filtration rate with cardiovascular disease mortality in Japanese general population. Kidney Int. 2006;69:1264–71.
White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med. 2011;30:377–99.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:2199–269.
Williams TA, Lenders J, Mulatero P, Burrello J, Rottenkolber M, Adolf C, et al. Outcomes after adrenalectomy for unilateral primary aldosteronism: an international consensus on outcome measures and analysis of remission rates in an international cohort. Lancet Diabetes Endocrinol. 2017;5:689–99.
Inker LA, Astor BC, Fox CH, Isakova T, Lash JP, Peralta CA, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis. 2014;63:713–35.
Kim IY, Park IS, Kim MJ, Han M, Rhee H, Seong EY, et al. Change in kidney function after unilateral adrenalectomy in patients with primary aldosteronism: identification of risk factors for decreased kidney function. Int Urol Nephrol. 2018;50:1887–95.
Hundemer GL, Curhan GC, Yozamp N, Wang M, Vaidya A. Cardiometabolic outcomes and mortality in medically treated primary aldosteronism: a retrospective cohort study. Lancet Diabetes Endocrinol. 2018;6:51–59.
Holtkamp FA, de Zeeuw D, Thomas MC, Cooper ME, de Graeff PA, Hillege HJ, et al. An acute fall in estimated glomerular filtration rate during treatment with losartan predicts a slower decrease in long-term renal function. Kidney Int. 2011;80:282–7.
Letavernier E, Peyrard S, Amar L, Zinzindohoué F, Fiquet B, Plouin PF. Blood pressure outcome of adrenalectomy in patients with primary hyperaldosteronism with or without unilateral adenoma. J Hypertens. 2008;26:1816–23.
Sawka AM, Young WF Jr, Thompson GB, Grant CS, Farley DR, Leibson C, et al. Primary aldosteronism: factors associated with normalization of blood pressure after surgery. Ann Intern Med. 2001;135:258–61.
Catena C, Colussi G, Lapenna R, Nadalini E, Chiuch A, Gianfagna P, et al. Long-term cardiac effects of adrenalectomy or mineralocorticoid antagonists in patients with primary aldosteronism. Hypertension. 2007;50:911–8.
Yang W-Y, Melgarejo JD, Thijs L, Zhang Z-Y, Boggia J, Wei F-F, et al. Association of office and ambulatory blood pressure with mortality and cardiovascular outcomes. JAMA. 2019;322:409–20.
Schlueter WA, Batlle DC. Renal effects of antihypertensive drugs. Drugs. 1989;37:900–25.
Acknowledgements
We thank the JPAS/JRAS members for collecting the clinical data.
Funding
This study was conducted as a part of the JPAS and JRAS by a research grant from the Japan Agency for Medical Research and Development (grant numbers JP17ek0109122 and JP20ek0109352), and the National Center for Global Health and Medicine, Japan (27-1402, 30-1008).
Author information
Authors and Affiliations
Consortia
Contributions
TH, Y. Yano, KT and MN designed the study; TH carried out the analyses; TH and Y. Yano drafted the manuscript; and YH, KT, IK, HK, MT, TI, NW, T. Katabami, KY, SO, T. Kai, SI, Y. Yoshikawa, MY, YC, AT and MN revised the paper.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Haze, T., Yano, Y., Hatano, Y. et al. Association of achieved blood pressure after treatment for primary aldosteronism with long-term kidney function. J Hum Hypertens 36, 904–910 (2022). https://doi.org/10.1038/s41371-021-00595-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-021-00595-4
This article is cited by
-
Possible relationship between primary aldosteronism and small vessel disease
Hypertension Research (2023)
-
Effect of the interaction between the visceral-to-subcutaneous fat ratio and aldosterone on cardiac function in patients with primary aldosteronism
Hypertension Research (2023)
-
The potential of a new nomogram for the diagnosis of primary aldosteronism
Hypertension Research (2023)