Abstract
Background/objectives
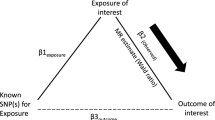
Obesity and asthma are common chronic diseases and have been reported to be mutually causative. We investigated the causal direction of the relationship between adiposity and asthma using genetic markers as instrumental variables (IVs) in bi-directional Mendelian randomization (MR) analysis.
Subjects/methods
We used data from the Taiwan Children Health Study with 24 body mass index (BMI)-single-nucleotide polymorphisms (SNPs, combined into a weighted allelic score) and 16 asthma-SNPs (combined into two weighted allelic scores, separately for asthma inflammatory and antioxidative genes) to yield genetic IVs for adiposity and asthma, respectively.
Results
The weighted allele score for BMI was strongly associated with adiposity (p = 2 × 10–16) and active asthma (p = 0.03). The two-stage least square regression risk ratio (RR) for the effect of BMI on asthma was 1.04 (95% confidence interval: 1.00–1.07, p = 0.03). Although the weighted asthma genetic scores were significantly associated with asthma (p = 8.4 × 10–3), no association was seen for genetically instrumented asthma with BMI using MR. Central obesity was the most accurate predictor of asthma. Adiposity showed higher causal effects on asthma in boys and children with non-atopic asthma. Sensitivity analysis for MR revealed no directional genetic pleiotropy effects. The causal effect RRs of BMI on asthma were 1.04, 1.08, and 1.03 for inverse-variance weighted, MR–Egger regression (slope), and weighted median methods, respectively, all in accordance with the MR estimates.
Conclusions
High adiposity may lead to asthma, whereas the effects of asthma on adiposity accumulation are likely to be small.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Chen YC, Dong GH, Lin KC, Lee YL. Gender difference of childhood overweight and obesity in predicting the risk of incident asthma: a systematic review and meta-analysis. Obes Rev. 2013;14:222–31.
Hasler G, Gergen PJ, Ajdacic V, Gamma A, Eich D, Rössler W, et al. Asthma and body weight change: a 20-year prospective community study of young adults. Int J Obes. 2006;30:1111–8.
Chen Z, Salam MT, Alderete TL, Habre R, Bastain TM, Berhane K, et al. Effects of childhood asthma on the development of obesity among school-aged children. Am J Respir Crit Care Med. 2017;195:1181–8.
Timpson NJ, Nordestgaard BG, Harbord RM, Zacho J, Frayling TM, Tybjærg-Hansen A, et al. C-reactive protein levels and body mass index: elucidating direction of causation through reciprocal Mendelian randomization. Int J Obes. 2011;35:300–8.
Vimaleswaran KS, Berry DJ, Lu C, Tikkanen E, Pilz S, Hiraki LT, et al. Causal relationship between obesity and vitamin D status: bi-directional Mendelian randomization analysis of multiple cohorts. PLoS Med. 2013;10:e1001383–e1001383.
Granell R, Henderson AJ, Evans DM, Smith GD, Ness AR, Lewis S, et al. Effects of BMI, fat mass, and lean mass on asthma in childhood: a Mendelian randomization study. PLoS Med. 2014;11:e1001669.
Melén E, Himes BE, Brehm JM, Boutaoui N, Klanderman BJ, Sylvia JS, et al. Analyses of shared genetic factors between asthma and obesity in children. J Allergy Clin Immunol. 2010;126:631–7, e631–8.
Chih AH, Chen YC, Tu YK, Huang KC, Chiu TY, Lee YL. Mediating pathways from central obesity to childhood asthma: a population-based longitudinal study. Eur Respir J. 2016;48:748–57.
Chen YC, Chih AH, Chen JR, Liou TH, Pan WH, Lee YL. Rapid adiposity growth increases risks of new-onset asthma and airway inflammation in children. Int J Obes. 2017;41:1035–41.
Group. WMGRS. WHO child growth standards: length/height-for-age, weight-for-age, weight-forlength, weight-for-height and body mass index-for-age: methods and development. Geneva: World Health Organization; 2006.
Chen YC, Tu YK, Huang KC, Chen PC, Chu DC, Lee YL. Pathway from central obesity to childhood asthma. Physical fitness and sedentary time are leading factors. Am J Respir Crit Care Med. 2014;189:1194–203.
Han YY, Forno E, Celedon JC. Adiposity fractional exhaled nitric oxide, and asthma in U.S. children. Am J Respir Crit Care Med. 2014;190:32–9.
Wen W, Zheng W, Okada Y, Takeuchi F, Tabara Y, Hwang JY, et al. Meta-analysis of genome-wide association studies in East Asian-ancestry populations identifies four new loci for body mass index. Hum Mol Genet. 2014;23:5492–504.
Wang J, Mei H, Chen W, Jiang Y, Sun W, Li F, et al. Study of eight GWAS-identified common variants for association with obesity-related indices in Chinese children at puberty. Int J Obes. 2012;36:542–7.
Wang HJ, Hinney A, Song JY, Scherag A, Meng X-R, Grallert H, et al. Association of common variants identified by recent genome-wide association studies with obesity in Chinese children: a case-control study. BMC Med Genet. 2016;17:7.
Zhu WF, Wang CL, Liang L, Shen Z, Fu JF, Liu PN, et al. Triglyceride-raising APOA5 genetic variants are associated with obesity and non-HDL-C in Chinese children and adolescents. Lipids Health Dis. 2014;13:93.
Akhabir L, Sandford AJ. Genome-wide association studies for discovery of genes involved in asthma. Respirology. 2011;16:396–406.
Hua L, Zuo XB, Bao YX, Liu QH, Li JY, Lv J, et al. Four-locus gene interaction between IL13, IL4, FCER1B, and ADRB2 for asthma in Chinese Han children. Pediatr Pulmonol. 2016;51:364–71.
Tsai CH, Tung KY, Su MW, Chiang BL, Chew FT, Kuo NW, et al. Interleukin-13 genetic variants, household carpet use and childhood asthma. PLoS ONE. 2013;8:e51970.
Tung KY, Tsai CH, Lee YL. Microsomal epoxide hydroxylase genotypes/diplotypes, traffic air pollution, and childhood asthma. Chest. 2011;139:839–48.
Liu YL, Wang SC, Hwu HG, Fann CS, Yang UC, Yang WC, et al. Haplotypes of the D-amino acid oxidase gene are significantly associated with schizophrenia and its neurocognitive deficits. PLoS ONE. 2016;11:e0150435.
Pedersen AB, Mikkelsen EM, Cronin-Fenton D, Kristensen NR, Pham TM, Pedersen L, et al. Missing data and multiple imputation in clinical epidemiological research. Clin Epidemiol. 2017;9:157–66.
Palmer TM, Sterne JA, Harbord RM, Lawlor DA, Sheehan NA, Meng S, et al. Instrumental variable estimation of causal risk ratios and causal odds ratios in Mendelian randomization analyses. Am J Epidemiol. 2011;173:1392–403.
Burgess S, Bowden J, Fall T, Ingelsson E, Thompson SG. Sensitivity analyses for robust causal inference from Mendelian randomization analyses with multiple genetic variants. Epidemiology. 2017;28:30–42.
Hedberg A, Rossner S. Body weight characteristics of subjects on asthma medication. Int J Obes. 2000;24:1217–25.
Eijkemans M, Mommers M, de Vries SI, van Buuren S, Stafleu A, Bakker I, et al. Asthmatic symptoms, physical activity, and overweight in young children: a cohort study. Pediatrics. 2008;121:e666–72.
Lochte L, Nielsen KG, Petersen PE, Platts-Mills TA. Childhood asthma and physical activity: a systematic review with meta-analysis and Graphic Appraisal Tool for Epidemiology assessment. BMC Pediatr. 2016;16:50.
Egan KB, Ettinger AS, Bracken MB. Childhood body mass index and subsequent physician-diagnosed asthma: a systematic review and meta-analysis of prospective cohort studies. BMC Pediatr. 2013;13:121.
Scott HA, Gibson PG, Garg ML, Pretto JJ, Morgan PJ, Callister R, et al. Relationship between body composition, inflammation and lung function in overweight and obese asthma. Resp Res. 2012;13:10–10.
Castro-Rodriguez JA, Holberg CJ, Morgan WJ, Wright AL, Martinez FD. Increased incidence of asthmalike symptoms in girls who become overweight or obese during the school years. Am J Respir Crit Care Med. 2001;163:1344–9.
Mead J. Dysanapsis in normal lungs assessed by the relationship between maximal flow, static recoil, and vital capacity. Am Rev Respir Dis. 1980;121:339–42.
Wise RA, Enright PL, Connett JE, Anthonisen NR, Kanner RE, Lindgren P, et al. Effect of weight gain on pulmonary function after smoking cessation in the Lung Health Study. Am J Respir Crit Care Med. 1998;157:866–72.
Chen YC, Chen PC, Hsieh WS, Portnov BA, Chen YA, Lee YL. Environmental factors associated with overweight and obesity in taiwanese children. Paediatr Perinat Epidemiol. 2012;26:561–71.
Rasmussen F, Hancox RJ. Mechanisms of obesity in asthma. Curr Opin Allergy Clin Immunol. 2014;14:35–43.
Acknowledgements
The authors thank the field workers, teachers, and other school staff who supported data collection, and all parents and children who participated in this study. We also thank Ministry of Science and Technology (#101–2314-B-532–002-MY3 and #104–2314-B-532–002-MY3) and National Health Research Institutes (NHRI-EX107-10718PC) in Taiwan for grant support of this study. We thank the National Center for Genome Medicine (NCGM) for the genotyping technical support.
Author contributions
Y-CC contributed the cohort data collection, interpretation of data, and writing. H-YF and Y-TH assisted in the critical part of the statistical analysis, data interpretation, and revised it critically for important intellectual content. S-YH and T-HL contributed to analysis and interpretation of data, critically revising this manuscript for intellectual content. YL reviewed the study design, acquisition of data, interpretation of data, supervised the study, and revised the manuscript critically for important intellectual content. All authors approved the final manuscript as submitted and published, and agreed to be accountable for all aspects of the work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Chen, YC., Fan, HY., Huang, YT. et al. Causal relationships between adiposity and childhood asthma: bi-directional Mendelian Randomization analysis. Int J Obes 43, 73–81 (2019). https://doi.org/10.1038/s41366-018-0160-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0160-8
This article is cited by
-
Mechanistic Links Between Obesity and Airway Pathobiology Inform Therapies for Obesity-Related Asthma
Pediatric Drugs (2023)
-
Visceral adiposity and respiratory outcomes in children and adults: a systematic review
International Journal of Obesity (2022)
-
Obesity-related biomarkers underlie a shared genetic architecture between childhood body mass index and childhood asthma
Communications Biology (2022)