Abstract
Background:
In neonatal jaundice, phototherapy converts bilirubin to more polar photoisomers which can be excreted without conjugation. We measured changes in the concentration of bilirubin Z,E-photoisomer during the first 4 h of intensive phototherapy using single fluorescent lights as a reference, compared to double fluorescent lights, and a single unit of photodiodes.
Methods:
Neonates (N = 42; birth weight: 1,200–4,690 g; gestational age: 28–42 wk) were studied during phototherapy. Infants were randomized to: (i) single, or (ii) double fluorescent phototherapy; or (iii) single unit photodiodes. Irradiance was measured. Serum bilirubin (by cooximetry) and Z,E bilirubin (by high-pressure liquid chromatography) were measured at 0,15, 30, 60, 120, and 240 min after the start of phototherapy. Data were analyzed with a linear mixed model.
Results:
There was a highly significant increase of Z,E-bilirubin over time (P < 0.0001), starting at 15 min. Photoisomers reached ~25% of total bilirubin concentration after 4 h. However, there were no significant differences between the three randomized groups in spite of significantly higher irradiance using double fluorescent lights vs. single fluorescent or photodiodes.
Conclusion:
Formation of bilirubin photoisomers is rapid, and occurs early during intensive phototherapy for neonatal jaundice. The rate and level of photoisomerization was not influenced by irradiance and light source.
Similar content being viewed by others
Main
Phototherapy is the standard treatment for hyperbilirubinemia in newborns, and is administered to prevent kernicterus and other sequelae of bilirubin neurotoxicity (1).
It is effective and considered safe. However, a recent report suggests that “aggressive” phototherapy in the smallest infants of birth weight 501–750 g may be associated with increased risk of death (2).
When native bilirubin IXα (Z,Z) in neonates is exposed to light, a rapid photochemical reaction produces water-soluble configurational (4Z,15E; 4E,15Z; 4E,15E) and structural (Z-lumirubin; E-lumirubin) isomers (3,4). Photooxidation may also occur (5,6). Due to increased polarity, these isomers can be excreted in bile and urine, bypassing the need for conjugation. It has recently been suggested that these isomers, because of their polarity, should be less able to cross the blood–brain barrier (1,7). If this is correct, photoisomer formation might be directly neuroprotective, irrespective of the effect on excretion. Experimental data suggest that bilirubin photoisomers are less toxic than the native IX α (Z,Z), but there are methodological weaknesses in these studies (1). Thus, experimental proof of the hypothesized direct neuroprotective effects of photoisomerization is still needed. Both different light qualities and variable light irradiance are commonly employed in practical phototherapy. Herein we have investigated whether such factors may impact on photoisomer formation.
The common light sources used in phototherapy are either fluorescent, or tungsten-halogen lamps with wide emission spectrum, or light-emitting diodes (LEDs) with narrow spectrum. Differences in peak wavelength as well as spectrum may impact on the rate and extent of bilirubin photoisomerization (8). Blue spectrum, near the bilirubin absorption maximum at 458 nm wavelength, may produce more of the Z,E isomer, and light at longer wavelengths, closer to the color turquoise, may produce more lumirubin (9). Z,E-bilirubin is more slowly cleared, thus more likely to reach significant levels in the serum and a more likely candidate for the role of “brain-sparing” bilirubin. We recently showed that a significant increase in serum Z,E-bilirubin concentration can be measured within minutes of starting phototherapy (10).
Although phototherapy has been the therapy of choice for newborns with hyperbilirubinemia for decades, there is still debate as to what is the most effective phototherapy we can provide (3). Most of the debate concerns the irradiance or the color (i.e., wavelengths and bandwidth). Blue light may be more effective, and can provide more photoisomerization than green light or daylight (11,12), but turquoise light may be more effective in preterm infants than blue light (9). Finally, photodiodes may be clinically more effective than conventional phototherapy with blue-white or green fluorescent tubes as judged by the production of lumirubin (13).
The aim of this randomized, controlled, nonblinded study was to compare the rate and level of 4Z,15E photoisomerization during intensive phototherapy using single vs. double fluorescent lights vs. a single unit with photodiodes.
Results
Clinical and laboratory characteristics are shown in Table 1 . Irradiance to the top surface with double fluorescent lights was significantly higher than with single fluorescent lights and photodiodes, similarly for irradiance to the flanks. There were no differences in irradiance between single fluorescent lights and single photodiodes. The irradiances at the babies, top surface (measured ~20 cm below the light source) were as follows (in W/m2, mean ± SD): single fluorescent 29.0 ± 5.7; double fluorescent 40.4 ± 5.9; photodiode device 31.6 ± 2.7.
The mean postnatal age when phototherapy was started was 65.9 h (median: 51 h).
Production of Photoisomers
The percentage of configurational 4Z,15E photoisomer increased with duration of phototherapy in all groups ( Figure 1 ). There was a significant increase of Z,E-bilirubin over time (P < 0.0001). Formation of isomers was detected as early as 15 min after onset of phototherapy, at which time the level (≈10%) was significantly higher than immediately before start-up. After about 4 h, photoisomer concentration reached 25% of total bilirubin. There were no statistically significant differences in the formation of Z,E-bilirubin photoisomers between the three groups, neither in the crude nor the adjusted model ( Table 2 ). This was true despite significantly higher irradiance in the double fluorescent group vs. single fluorescent and photodiodes.
Formation of 4Z,15 E photoisomers as a percentage of total serum bilirubin. Blue bar: Fluoroscent—single bank. Red bar: Fluoroscent double bank. Black bar: photodiodes. On each box, the central mark (in black) is the median, the edges of the box are the 25th and 75th percentiles, respectively, the whiskers extend to the most extreme data points not considered outliers. Outliers were excluded from the figure.
Total serum bilirubin (TSB) values decreased significantly more slowly (P = 0.005) in the group that received single fluorescent phototherapy vs. the two other groups. However, although statistically significant, the actual difference in 0–4 h decrease was small (7 vs. 9.5 vs. 9%, single vs. double fluorescent vs. photodiodes, respectively).
Hemoglobin (Hb) Concentration and Production of Photoisomers
The mean hemoglobin value was 10.9 g/dl (range: 11.7–22.6 g/dl). When analyzed with the linear mixed model, percent formation of photoisomers at 30 and 60 min after start of phototherapy was negatively correlated with Hb values. The percentage (mean (95% CI)) of photoisomers 30 min after the start was 12.8 (10.7, 15.0) and 17.8 (16.4, 19.3) among those with Hb ≥ 14.5 g/dl and Hb < 14.5 g/dl (P = 0.001), respectively. Corresponding numbers 60 min after the start were 16.9 (14.9, 19.0) and 21.3 (19.9, 22.8), P = 0.037. Beyond 60 min, Hb values had no impact on photoisomer formation ( Figure 2 ). Exploring further the effect of Hb by a linear regression analysis revealed that the effect of Hb was significant at 15 min (F = 7.66, P = 0.009) and 30 min (F = 4.47, P = 0.042), but not from 60 min and thereafter.
Time trend in formation of photoisomers relative to Hb ≥ 14.5 g/dl and Hb <14.5 g/dl. Hb ≥ 14.5 g/dl in black, Hb < 14.5 g/dl in gray.
Discussion
The purpose of this study was to compare the effect of phototherapy with single vs. double fluorescent vs. photodiodes on the formation of bilirubin photoisomers. The efficacy of phototherapy depends on the irradiance and wavelength of the light, and on the irradiated skin area (3,14). The efficacy of phototherapy is also influenced by bedside optimization of spectral power (e.g., using reflecting surfaces), patient characteristics, and the phototherapy device characteristics (15). The 2004 American Academy of Pediatrics guidelines on management of neonatal jaundice defined intensive phototherapy as irradiance higher than 30 μW/cm2/nm over the 430–490 nm wavelength interval (16).
Herein we have shown that 4Z,15E bilirubin is detectable in blood within 15 min after starting efficient phototherapy. By this time, around 10% of circulating bilirubin was isomerized to 4Z,15E bilirubin ( Figure 1 ). A further increase to photoisomer levels of 23–27 % after 4 h was observed. However, our data do not show that this represents a true plateau. Notably, there was no statistically significant difference between the three groups in formation of photoisomers.
Our present observation, as well as in our previous study (10), evincing rapid formation of bilirubin photoisomers in the blood within few minutes of commencing phototherapy, is compatible with a primary site of action of phototherapy in the capillary circulation. This agrees with the findings of Donneborg et al. (17), who showed that changing the position of infants during phototherapy, as is common practice, does not increase the effect of phototherapy. They inferred that the effect of phototherapy is in the capillary circulation near the skin surface.
Because photoisomers are more polar, it can be hypothesized that they may be less able to cross the blood–brain barrier, thus possibly reducing the risk of neurotoxicity. Indeed, this was proposed by McDonagh et al. (18) more than 30 y ago. The theoretical arguments are chemically and physiologically coherent (10). Also, the reports of apparent reversibility of acute intermediate-to-advanced stage bilirubin encephalopathy with timely aggressive therapy (19,20,21), support the need to learn more about the rate of photoisomerization as a function of the emission spectrum, the irradiance of the lights, the surface area exposed, and possibly the initial serum bilirubin level (3). The percentage conversion of bilirubin to 4Z,15E bilirubin is expected to increase with time until an equilibrium between Z,Z-bilirubin and Z,E-bilirubin is obtained, that is dependent only on the emission spectrum of the light (7). Therefore, we aimed to examine the impact of the use of double compared to single unit fluorescent phototherapy, as well as that of photodiodes.
Z,E bilirubin is formed rapidly but excreted slowly. Thus, this isomer achieves a high level as a fraction of total serum bilirubin (9,22,23). It is precisely this phenomenon that allows us to speculate on a possible neuroprotective effect of phototherapy. Photoisomer formation starts long before significant changes in TSB can be detected. After 2 h of phototherapy TSB is only minimally reduced, while the 4Z,15E photoisomer alone constitutes between 20–25%, and other photoisomers, albeit present only in low concentrations, nevertheless add to that number (8). The range of photoisomer values seems wider at the earlier time points than later, and narrower as a putative equilibrium between Z, E- and Z,Z-bilirubin is approached. A wide scatter of values was also reported by Onishi et al. (24), while Myara et al. (8) found less variation. The scatter of our early values suggests the possibility that in some infants factors may be operative that allow a more rapid response as far as photoisomer formation. This is presumably explained by the very wide range of the infants’ birth weights. With low birth weight, the body surface area relative to volume is high, thus the light-exposed area in relation to weight increases. This leads to increased formation and higher serum concentration of photoisomers. When an equilibirium between Z,E- and Z, Z-bilirubin is achieved, the percentage of Z,E-bilirubin will be independent of the formation of photoisomers and thus the birth weight.
This is the first study which has compared early formation rate of photoisomers according to the type of phototherapy and the irradiance of the light source. Compared to previous studies of photoisomer formation, our sampling and sample handling have been successful as far as protection from ambient lights. Thus, in contrast to others (8,24), our results show very low isomer concentrations before phototherapy starts.
Our study supports previous studies (9,12,22,25), which showed that configurational isomers of bilirubin are formed in the plasma of infants who receive phototherapy. The early study of Costarino et al. (25) appeared to show that Z,E-bilirubin in the serum reached steady-state within 4 h after starting phototherapy. Our finding that the concentration of Z,E-bilirubin increased with the duration of phototherapy during the 4-h study period, is in part consistent with that study. Though it is possible that levels can increase even higher, as our data do not confirm that a plateau had been reached at 4 h, both the shape of the curve in Figure 1 as well as the data from Myara et al. (8), suggest that an equilibrium or “saturation” level is likely to exist.
In most clinical studies of phototherapy, the effect was measured as reduction of TSB. The presence of photoisomers has received much less attention as an effect measure, and the possible neuroprotective effect of converting one quarter of circulating bilirubin to more polar isomers has only been addressed to a very limited extent (10).
In the present study, we have documented that the proportion of the 4Z,15E isomer increases significantly over the 4-h study period, while changes in total serum bilirubin are small. However, there was no difference between the three groups in formation of photoisomers. This is in accordance with Costarino et al. (25) showing no difference in the percentage of Z,E-bilirubin in preterm infants exposed to either a low or a high light irradiance from daylight bulbs. We had expected that the serum concentration of Z,E-bilirubin would have been higher with double than single unit fluorescent phototherapy, as the in vitro production rate has been shown to increase with irradiance (3). Thus, more studies are needed to further elucidate these questions.
The efficacy of phototherapy is dependent on several factors. Hemoglobin absorbs visible light in the skin, and is the major competitor with bilirubin for light absorbtion. Therefore, it was recently suggested that a high hematocrit/hemoglobin level could reduce the therapeutic efficacy of phototherapy (26). In a post hoc analysis of hemoglobin data from our patients, we found a significant negative correlation between Hb and photoisomer formation during the early phase of phototerapy (15, 30, and 60 min), which disappeared at the later time points. This fits with the fact that a difference only exists until an equilibrium between Z,E- and Z,Z-bilirubin is achieved. The results support the suggestion by Lamola et al. (26) that the hemoglobin level will influence the efficacy of phototherapy. Possible explanations for this phenomenon are that the proportion of plasma to red cells is lower with high Hb, so it takes longer for the circulating bilirubin to be exposed to phototherapy lights. Slower capillary circulation due to the higher viscosity of high Hb blood may have the same effect, and as Hb filters the light, we speculate that with more red cells bilirubin molecules are exposed to less light.
The strength of this study is that it represents an average neonatal intensive care unit (NICU) population. The study was designed to investigate the formation of photoisomers under predefined phototherapy conditions, with clearly defined critera for, i.e., the distance of the phototherapy device from the baby. There were strict procedures for protection of blood samples from ambient light during sampling and processing. This allowed us to show low levels immediately prior to, and significant formation of photoisomers as early as 15 min after initiation of phototherapy. A possible weakness of this study is the relatively limited number of patients which may have caused us to miss a (small) difference in photoisomer formation between the groups. If, as speculated, photoisomers are less able to cross the blood–brain barrier, our findings support the hypothesis that formation of photoisomers may be a meaningful effect of phototherapy, even when there is little or no change in TSB values. Indeed, the protective effect of photoisomers may begin as soon as phototherapy is initiated.
Conclusion
Our data confirm that formation of bilirubin photoisomers occurs early in effective phototherapy, constituting ~25% of total serum bilirubin by 4 h. There was no significant difference in formation of Z,E photoisomers between the three groups despite significantly higher irradiance in double vs. single fluorescent and photodiodes. Since these photoisomers may be less able to cross the blood–brain barrier than native bilirubin IXα (Z,Z), phototherapy may protect the brain, and reduce the risk of bilirubin encephalopathy, even before changes in TSB can be detected. If this interpretation of the knowledge about bilirubin photoisomer characteristics is correct, phototherapy has two salutary effects—reduction of neurotoxicity risk through accumulation of the configurational 4Z,15E isomer, and facilitated excretion of the structural isomer lumirubin.
Methods
Patient Cohort
This study was performed in the NICU at Akershus University Hospital, Norway. Infants admitted to the NICU at >276 wk gestation and >1,000 g birth weight and who were in need of phototherapy for hyperbilirubinemia according to Norwegian national guidelines (27) were invited by a staff member to participate in the study. A power analysis was performed based on a previous study (10) to detect a difference of 50% in photoisomer Z,E concentration at 15 and 60 min after initiation of treatment (judged as a “clinically significant” difference) with a power of 80% and a type I error rate of 5%, leading to 14 patients in each group, a total of 42 patients was needed.
The patients had gestational age of 37.0 + 2.9 wk (mean ± SD), range 28–42 wk. The ethnicities of the infants were 28 Caucasian, 11 Asian, 1 African, and 2 of mixed parentage. The recruitment period ran from 28 May 2009 till 18 January 2012. Clinical data and duration of phototherapy were recorded. The infants were naked except for eye pads and diapers.
Enrolled infants were randomized by drawing of sealed opaque envelopes to: (i) Single unit fluorescent phototherapy (BiliCompact Infant Phototherapy Lamp, Weyer GmbH, Kürten, Germany), or (ii) Double unit fluorescent phototherapy with BiliCompact (Weyer GmbH), or (iii) Single unit photodiodes (neoBLUE, Natus Medical Incorporated, San Carlos, CA). Of note, double unit phototherapy was not routinely used in this NICU, and there were no defined criteria for such use. Thus, no infant randomized to groups 1 or 3 was deprived of a treatment which might otherwise have been given.
Phototherapy Setup
Phototherapy was given as indicated by Norwegian National Guidelines (27). Single phototherapy was provided by either neoBLUE (Natus Medical Incorporated) or BiliCompact (Weyer GmbH) positioned at a distance of 20 cm from the infants. Spectral power was enhanced by covering the bassinet inside with white linen and by placing white linen as curtains around the unit using specially adapted racks (28). Double phototherapy was administered by two units BiliCompact (Weyer GmbH) placed above the infant, also at a distance of about 20 cm, both at an angle of ~30–40 degrees from the horizontal and facing each other.
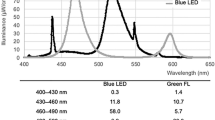
The neoBLUE (Natus Medical Incorporated) unit emits blue LED light in the 450–470 nm spectrum. This range corresponds to the bilirubin peak absorption wavelength of 458 nm. It delivers 12–30 μW/cm2/nm, depending on the distance and adjustment of irradiance by flipping a switch. BiliCompact (Weyer GmbH) contains 10 9W 12.7-cm length fluorescent bulbs (BAM/PL9/52, Ralutec 9W/71 G 23). These bulbs have broad Gaussian emission spectra roughly from 400 to 525 nm with a peak at 450 nm and intense mercury emission lines at 405, 436, and 546 nm. The radiant power over the range 400–550 nm is given as 2.3 W and their bilirubin-effective radiation intensity as 20 W/m2 at a distance of 25 cm.
Bilirubin Measurements
Capillary blood samples for TSB measurements and for high-pressure liquid chromatography (HPLC) were drawn immediately before start of phototherapy, and then 15, 30, 60, 120, or 240 min after start of phototherapy. Ethics approval allowed for five samples from each infant. Therefore, the final sample was obtained at 120 min in half of the infants in each group, and at 240 min in the other half. TSB was measured by cooximetry with an ABL 800 blood gas machine (Radiometer Medical, Brønshøj, Denmark) immediately after collection of blood samples. Supplemental clinical data and blood test results were collected from the patient records as permitted by the ethics committee.
Processing of Blood Samples for HPLC
Blood samples for HPLC were continuously protected from light by aluminum foil. Centrifugation in a HERAEUS Multifuge 1S centrifuge (Thermo scientific-Thermo Electron LED GmbH, Robert-Bosch str.1, D-63505 Langenselbold, Germany) at 2,000 rpm for 10 min in the cold (4 °C), and pipetting of blood samples were done under red light. Plasma was pipetted into polyethylene tubes and stored in these at −70 °C. All samples were transported on dry ice in one batch for analyses of bilirubin photoisomers.
HPLC
Bilirubin isomers were analyzed on a Dionex Ultimate 3000 system, including a multiple Wavelength detector (Dionex, Sunnyvale, CA). The column used for HPLC was a Kinetex core-shell 2.6 µm C-18 (15 × 0.46 cm) (Phenomenex, Torrance, CA). HPLC was performed according to Itoh et al. (29) using a gradient with primary eluent:
Acetonitrile—0.01 M sodium phosphate (pH 5.5)—dimethyl formamide (50:300:650), and secondary eluent: acetonitrile—0.01 M sodium phosphate—dimethyl formamide (200:150:650).
The flow rate was 0.25 ml/min and eluates were detected as absorbance at 455 nm. Areas under the peaks of the chromatograms were used in calculation of the relative concentration of the bilirubin isomers. The relative molar absorptivity values at 455 nm used were: (Z,Z)-bilirubin: (Z,E)-bilirubin: (E,Z)-bilirubin: (E,Z)-lumirubin (E,E) lumirubin = 1.00: 0.81: 0.54: 0.46: 0.39 (29). Fifty microliters of serum were mixed with 50 µl acetonitrile and dimethylsulfoxid, vortexed for 10 s and centrifuged at 22,000 g for 20 s. Twenty-five microliters were injected onto the column. All preparations and procedures were done under red light conditions.
Irradiance Measurements
Irradiance was measured at the babies’ top surface ~20 cm below the light source and in the flanks with an LMT-Pocket Ebi photometer, which has a sensitivity spectrum of 388–555 nm and a peak at 475 nm. (LMT Lichtmesstechnik; GmbH, Berlin, Germany)
Data Handling
Clinical and laboratory characteristics were described by means (SD) and medians with intervals specifying minimum and maximum values. Box plots were used to present data graphically. Median test was applied to assess the differences in characteristics across all three light sources as well as pairwise differences. A linear mixed model with first-, second- and third-order time components as fixed effects and random intercepts was fitted to assess trends in Z,E-bilirubin concentrations (SAS MIXED procedure). Such a model takes correlations due to repeated measurements into account, and may prevent false significant findings. The light source variable was used as predictor with the single unit fluorescent light (BiliCompact) group as reference. The model was further adjusted for potential confounders; irradiance values on the babies’ top surface, hemoglobin concentrations, and birth weight. Data were presented as regression coefficients with 95% confidence intervals (CI) and P values. All statistical analyses were performed with SPSS v20 (IBM, Released 2011. IBM SPSS Statistics for Windows, Version 20.0, IBM, Armnok, NY) and SAS v 9.3 (SAS software Copyright, SAS Institute, NC).
The inclusion of patients was completed before the publication by Lamola et al. (26), proposing that the level of hemoglobin at the time of phototherapy may impact on the formation of photoisomers. Therefore, we retrospectively abstracted from the charts the hemoglobin values of our patients at the time of phototherapy. Such values were available for 36 of the 42 patients. Because we had not found any significant differences between the study groups as far as formation of photoisomers, data from all three groups were pooled. The data were then organized in three groups each of size 12 according to the levels of Hb (<14.5 g/dl; 14.5–17.5 g/dl; >17.5 g/dl). As there was no statistically significant difference between the two groups at cut-off >14.5 g/dl, the two last groups were also pooled for the final analysis, when estimating a linear mixed model. The results were presented graphically as means estimated by the model at each time point with corresponding 95% CI in two groups of Hb.
However, because the model of Hb influence predicts that these effects will only be apparent during the early phase of phototherapy, before equilibrium between the 4Z,15Z and the 4Z,15E has been achieved, the data was further explored by a linear regression model at each individual time point.
Ethical Considerations
The study protocol was approved by the Health South-East regional committee for medical and health research ethics and by the Norwegian Data Directorate. Infants were enrolled in the study after spoken and written informed consent by the parents. The ethics committee stipulated that the number of blood draws per baby should be limited to five. This trial was registered with number ACTRN12614000716662 in the Australian New Zealand Clinical Trials Registry (ANZCTR), under the title: “Early isomerization of bilirubin in optimized phototherapy of neonatal jaundice”.
Statement of Financial Support
This study was supported by the Faculty of Medicine, University of Oslo through annual operating funds for Drs. Nakstad and Hansen, by the Department of Pediatric and Adolescent Medicine, Akershus University Hospital through salary support for Dr. Mreihil, and by the Women and Infants’ Division, Oslo University Hospital.
Disclosure
The authors declare that they have no financial relationships with any organizations that may have an interest in the submitted work and no other relationships or activities that could appear to have influenced the submitted work.
References
Hansen TW. Phototherapy for neonatal jaundice--therapeutic effects on more than one level? Semin Perinatol 2010;34:231–4.
Tyson JE, Pedroza C, Langer J, et al.; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Does aggressive phototherapy increase mortality while decreasing profound impairment among the smallest and sickest newborns? J Perinatol 2012;32:677–84.
Maisels MJ, McDonagh AF. Phototherapy for neonatal jaundice. N Engl J Med 2008;358:920–8.
McDonagh AF, Lightner DA. Phototherapy and the photobiology of bilirubin. Semin Liver Dis 1988;8:272–83.
McDonagh AF, Palma LA, Trull FR and Lightner DA. Phototherapy for neonatal jaundice. Configurational isomers of bilirubin. J Am Chem Soc 1982;104:6865–7.
McDonagh AF, Palma LA and Lightner DA. Phototherapy for neonatal jaundice. Stereospecific and regioselective photoisomerization of bilirubin bound to human serum albumin and NMR characterization of intramolecularly cyclized photoproducts. J Am Chem Soc 1982;104:6867–8.
McDonagh AF. Controversies in bilirubin biochemistry and their clinical relevance. Semin Fetal Neonatal Med 2010;15:141–7.
Myara A, Sender A, Valette V, et al. Early changes in cutaneous bilirubin and serum bilirubin isomers during intensive phototherapy of jaundiced neonates with blue and green light. Biol Neonate 1997;71:75–82.
Ebbesen F, Madsen P, Støvring S, Hundborg H, Agati G. Therapeutic effect of turquoise versus blue light with equal irradiance in preterm infants with jaundice. Acta Paediatr 2007;96:837–41.
Mreihil K, McDonagh AF, Nakstad B, Hansen TW. Early isomerization of bilirubin in phototherapy of neonatal jaundice. Pediatr Res 2010;67:656–9.
Ennever JF, Sobel M, McDonagh AF, Speck WT. Phototherapy for neonatal jaundice: in vitro comparison of light sources. Pediatr Res 1984;18:667–70.
Costarino AT Jr, Ennever JF, Baumgart S, Speck WT, Polin RA. Effect of spectral distribution on isomerization of bilirubin in vivo. J Pediatr 1985;107:125–8.
Okada H, Abe T, Etoh Y, et al. In vitro production of bilirubin photoisomers by light irradiation using neoBLUE. Pediatr Int 2007;49:318–21.
Maisels MJ. Phototherapy--traditional and nontraditional. J Perinatol 2001;21:Suppl 1:S93–97; discussion S104–107.
Vreman HJ, Wong RJ, Murdock JR, Stevenson DK. Standardized bench method for evaluating the efficacy of phototherapy devices. Acta Paediatr 2008;97:308–16.
American Academy of Pediatrics Subcomittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 2004;114:297–316.
Donneborg ML, Knudsen KB, Ebbesen F. Effect of infants’ position on serum bilirubin level during conventional phototherapy. Acta Paediatr 2010;99:1131–4.
McDonagh AF, Lightner DA. ‘Like a shrivelled blood orange’–bilirubin, jaundice, and phototherapy. Pediatrics 1985;75:443–55.
Johnson L, Bhutani VK, Karp K, Sivieri EM, Shapiro SM. Clinical report from the pilot USA Kernicterus Registry (1992 to 2004). J Perinatol 2009:29:Suppl 1:S25–45.
Harris MC, Bernbaum JC, Polin JR, Zimmerman R, Polin RA. Developmental follow-up of breastfed term and near-term infants with marked hyperbilirubinemia. Pediatrics 2001;107:1075–80.
Hansen TW, Nietsch L, Norman E, et al. Reversibility of acute intermediate phase bilirubin encephalopathy. Acta Paediatr 2009;98:1689–94.
Lamola AA, Blumberg WE, McClead R, Fanaroff A. Photoisomerized bilirubin in blood from infants receiving phototherapy. Proc Natl Acad Sci USA 1981;78:1882–6.
Onishi S, Isobe K, Itoh S, Kawade N, Sugiyama S. Demonstration of a geometric isomer of bilirubin-IX alpha in the serum of a hyperbilirubinaemic newborn infant and the mechanism of jaundice phototherapy. Biochem J 1980;190:533–6.
Onishi S, Isobe K, Itoh S, et al. Metabolism of bilirubin and its photoisomers in newborn infants during phototherapy. J Biochem 1986;100:789–95.
Costarino AT, Ennever JF, Baumgart S, Speck WT, Paul M, Polin RA. Bilirubin photoisomerization in premature neonates under low- and high-dose phototherapy. Pediatrics 1985;75:519–22.
Lamola AA, Bhutani VK, Wong RJ, Stevenson DK, McDonagh AF. The effect of hematocrit on the efficacy of phototherapy for neonatal jaundice. Pediatr Res 2013;74:54–60.
Bratlid D, Nakstad B, Hansen TW. National guidelines for treatment of jaundice in the newborn. Acta Paediatr 2011;100:499–505.
Djokomuljanto S, Quah BS, Surini Y, et al. Efficacy of phototherapy for neonatal jaundice is increased by the use of low-cost white reflecting curtains. Arch Dis Child Fetal Neonatal Ed 2006;91:F439–42.
Itoh S, Isobe K, Onishi S. Accurate and sensitive high-performance liquid chromatographic method for geometrical and structural photoisomers of bilirubin IX alpha using the relative molar absorptivity values. J Chromatogr A 1999;848:169–77.
Acknowledgements
We thank Angelo Lamola, PhD, for helpful discussions on the analysis of the Hb data. We thank nurses at the NICU at Akershus University Hospital for good collaboration
Author information
Authors and Affiliations
Corresponding author
PowerPoint slides
Rights and permissions
About this article
Cite this article
Mreihil, K., Madsen, P., Nakstad, B. et al. Early formation of bilirubin isomers during phototherapy for neonatal jaundice: effects of single vs. double fluorescent lamps vs. photodiodes. Pediatr Res 78, 56–62 (2015). https://doi.org/10.1038/pr.2015.61
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2015.61
This article is cited by
-
Sixty years of phototherapy for neonatal jaundice – from serendipitous observation to standardized treatment and rescue for millions
Journal of Perinatology (2020)
-
Double versus single intensive phototherapy with LEDs in treatment of neonatal hyperbilirubinemia
Journal of Perinatology (2018)
-
The impact of hemoglobin on the efficacy of phototherapy in hyperbilirubinemic infants
Pediatric Research (2017)
-
Spectral Range Optimization to Enhance the Effectiveness of Phototherapy for Neonatal Hyperbilirubinemia
Journal of Applied Spectroscopy (2017)
-
Bilirubin isomer distribution in jaundiced neonates during phototherapy with LED light centered at 497 nm (turquoise) vs. 459 nm (blue)
Pediatric Research (2016)