Abstract
Previous studies to identify a genetic component to RDS have shown conflicting results. Our objectives were to evaluate and quantify the genetic contribution to RDS using data that comprehensively includes known environmental factors in a large sample of premature twins. Data from a retrospective chart review of twins born at ≤32 wk GA were obtained from two neonatal units. Mixed effects logistic regression (MELR) analysis was used to assess the influence of several independent covariates on RDS. A zygosity analysis, including the effects of additive genetic, common environmental and residual effects (ACE) factors, was performed to estimate the genetic contribution. Results reveal that the 332 twin pairs had a mean GA of 29.5 wk and birth weight (BW) of 1372 g. An MELR identified significant nongenetic covariates as male gender (p = 0.04), BW (p < 0.001), 5-min Apgar score (p < 0.001), and treating institution (p = 0.001) as significant predictors for RDS. The ACE model was used to estimate the genetic susceptibility to RDS by adjusting for the above factors. We found 49.7% (p = 0.04) of the variance in liability to RDS was the result of genetic factors alone. We conclude that there is a significant genetic susceptibility to RDS in preterm infants.
Similar content being viewed by others
Main
RDS is a disease process that results from an absent or diminished amount of surfactant in the newborn lung. Prematurity, therefore, plays a crucial role in the development of RDS. The incidence is inversely proportional to GA and birth weight (BW), with approximately 71% of neonates with BW between 501 and 750 g affected when compared with 23% of those between 1250 and 1500 g (1). In addition to prematurity, multiple additional factors have been implicated in the pathogenesis of RDS. These include maternal, intrapartum, and neonatal variables such as advanced maternal age (2), chorioamnionitis (3,4), mode of delivery (5), gender (6,7), and birth order (8–11). Despite major advances, such as increased use of prenatal steroids and postnatal surfactant in perinatal and neonatal care, RDS is a leading cause of morbidity and mortality in preterm infants and incurs an estimated annual economic burden of 2.3 billion dollars (12–14).
In preterm infants of the same GA, the clinical severity of RDS varies widely. Therefore, we hypothesized that in addition to environmental effects, unknown genetic factors play a major role in predisposing premature neonates to RDS.
Our major objective was to conduct a heritability study of a large cohort of premature twin pairs, using sophisticated statistical analyses that control for the major known independent risk factors, to identify and quantify the genetic contribution to RDS.
METHODS
Subjects.
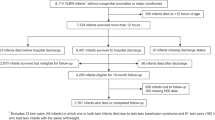
Data on premature twins born at ≤32 wk of gestation between January 1, 1994, and December 31, 2004, including zygosity information were collected from two centers (The University of Connecticut and Yale University). We included only infants who survived beyond a postmenstrual age (PMA) of 36 wk. The twin database was created to evaluate the genetic contribution to common neonatal disorders (including bronchopulmonary dysplasia). In addition, we wanted to avoid missing the diagnosis of RDS, especially if death occurred early (e.g., in the delivery room), and prevented the clinical picture and/or radiographic manifestations to be overtly manifested. Hence, for consistency, we excluded all deaths before 36 wk PMA. The institutional review boards of both centers approved this study and exempted it from obtaining informed consent, as per their guidelines.
Definitions.
Data were prospectively collected and entered into the databases by trained research personnel at both institutions, as routine practice, using similar definitions. RDS was defined as presence of respiratory distress with an oxygen requirement to maintain oxygen saturations of ≥90% in the first 6 h of life, accompanied by a characteristic chest radiograph. The time frame was selected to allow inclusion of the maximum number of cases of primary/congenital RDS and to avoid cases of acquired RDS. The chest x-ray was used for the confirmation of diagnosis by excluding other potential causes of respiratory distress, for example, transient tachypnea of the newborn. All radiographs were routinely read by trained pediatric radiologists at both institutions. Zygosity was determined by ultrasound evaluation before 20 wk GA and histopathological examination of the placenta at the Yale and the University of Connecticut with an additional confirmation of the gender. Gestational hypertension was defined as any new onset blood pressure >140/90 mm Hg or mean arterial pressure >105 mm Hg that occurred after the 20th wk of pregnancy. In vitro fertilization (IVF) was defined as any type of assisted reproductive technology that involved extracorporeal fertilization. Premature rupture of membranes (PROM) was defined as rupture that occurred at least 18 h before delivery. Histologic chorioamnionitis was defined by pathological examination of the placenta (15).
Statistical analysis.
Demographic data were analyzed using t test, Wilcoxon rank sum test, or χ2 analysis when appropriate. For χ2 analysis of the zygosity data, the observed numbers of twin pairs with both infants affected, with only one infant affected, and with neither infant affected were found, respectively, for monozygotic (MZ) and dizygotic (DZ) groups. These observed numbers formed a 2 × 3 contingency table. Conversely, the analog expected numbers of twin pairs were calculated from the corresponding marginal totals. The observed to expected distributions of concordance were compared using χ2 analysis.
Mixed effects logistic regression (MELR) analysis was performed to identify the impact of putative factors on RDS. The covariates used in the model included maternal age, IVF, delivery type, birth order, gender, weight, 5-min Apgar score, and treating institution. The status of the outcomes from twin pairs was treated as a correlated event. An MELR model was fitted to assess the relationship between the covariates listed, the outcome of interest (RDS), and to incorporate the correlation between twin pairs.
The additive genetic, common environmental and residual effects (ACE) model (16) was then used to estimate the variance in liability for RDS. The ACE model is a mixed-effects probit model, which included covariate effects, an additive genetic effect, a common environmental effect shared by a twin pair (with no distinction between MZ and DZ twin pairs), and a residual environmental effect. The additive genetic effects, the common environmental effect, and the residual environmental effects were assumed to be independently and normally distributed. The additive genetic effects for MZ twins were assumed to be identical. For DZ twins, the covariance of the additive genetic effects was assumed to be half that of MZ twins (17). The covariates adjusted in the ACE model included all significant covariates used in the MELR analysis. The genetic heritability could then be estimated using the ratio of estimated genetic variance and the total variance of the trait.
Statistical analyses were performed using SAS 9.1 (PROC NLMIXED). A p < 0.05 was considered statistically significant.
RESULTS
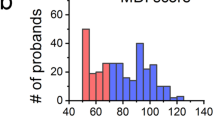
The cohort consisted of 332 twin pairs with a mean GA of 29.5 wk and BW of 1372 g. There were 70 MZ twin pairs and 262 DZ twin pairs. The RDS was diagnosed in 465 of 664 infants (70.0%). Despite a discrepancy in the overall number of twin pairs in each group, no statistically significant differences were observed between MZ and DZ twins with respect to gender, GA, weight, 5-min Apgar score, maternal race, delivery type, incidences of gestational hypertension, PROM, maternal diabetes, and chorioamnionitis, and use of antenatal steroids and antibiotics (Table 1). However, significant differences were found between MZ and DZ twins with respect to maternal age and the proportion of neonates conceived through IVF (Table 1). The distribution of patients with RDS by site and BW are shown in Table 2.
We initially performed an unadjusted concordance analysis to look for a genetic effect for RDS. The analysis revealed a significant difference of concordance distributions between MZ and DZ twin pairs (p = 0.02), suggesting a significant role for genetic factors in the pathogenesis of RDS (Table 3).
An MELR analysis was performed next using RDS as the dependent variable to identify significant nongenetic covariates that may have contributed to the outcome of interest. The analysis determined that male gender [regression coefficient = 0.401; 95% CI: (0.019-0.783); p = 0.04], BW [regression coefficient = −0.002; 95% CI: (−0.002 to −0.001); p < 0.001], 5-min Apgar score [regression coefficient = −0.552; 95% CI: (−0.782 to −0.322); p < 0.001], and institution [Yale; regression coefficient = 0.688; 95% CI: (0.284-1.091); p = 0.001] were significant covariates for the RDS (Table 4). Addition of race as a factor in the logistic regression model did not change our results in a significant manner (data not shown).
After adjusting for all significant covariates identified by the MELR, total genetic effects accounted for 49.7% (p = 0.04) of the variance in liability to RDS by ACE modeling.
DISCUSSION
In two cohort studies of women who delivered two singleton preterm infants, a comparison of the relative risk of RDS in the second infant was performed according to the RDS status of the first one (18). There was a significantly increased relative risk of RDS in the second sibling of women whose first preterm infant had RDS versus those whose first preterm infants did not have RDS. This remained significant even after controlling for confounding variables, suggesting an important genetic (or other familial) contribution to the risk of RDS (18).
Previous twin studies (10,19–21) have evaluated the genetic contribution to RDS with contradictory results. The first two studies published in 1971 (19) and 2002 (20) showed that the RDS had a significant genetic component. Myrianthopoulos et al. studied 31 twin pairs and showed a higher concordance rate between MZ compared with DZ pairs (85% concordance in MZ and 44% in DZ). In a retrospective review of all twins born during a 19-y period (1976-1995) in Amsterdam, van Sonderen et al. (20) found a RDS concordance rate of 67% when the twins were MZ when compared with only 29% when they were DZ. The Amsterdam study suggested a strong genetic influence, but only included 80 pairs with a GA of 30-34 wk (20), a population with a fairly low risk for RDS.
In contrast, Marttila et al. (21) evaluated 100 same-gender twin pairs with RDS and found a concordance difference of only 10% (95% CI: −0.1 to + 0.3, p = 0.32), suggesting an insignificant genetic contribution. The authors' concluded that the small concordance difference did not rule out the possibility of a genetic component of RDS (21). The same group of investigators then conducted a registry-based study that assessed the intrapair differences in susceptibility to RDS in a homogenous population of European ancestry (10). They concluded that environmental factors predominate over genetic factors based on a lack of concordance difference between same-gender twins compared with opposite-gender twins. Although this study included a large number of twin pairs, the zygosity was inferred by considering all the gender discordant pairs as DZ and then estimating the number of MZ twin pairs from the gender concordant cohort (10).
A summary of the previous twin studies on the heritability of RDS and a comparison to the present one has been shown in Table 5. Interpretation of the results of previous studies were limited by sample size, variability in the methods for confirmation of zygosity, and the exclusion of confounding variables known to contribute to the risk of RDS. Using a large sample size, a standard method for ascertaining zygosity, and including and controlling for virtually all major known nongenetic (i.e., environmental) risk factors for RDS, we were able to establish that a significant genetic contribution to RDS exists. Furthermore, we were able to quantify this contribution.
Despite lacking evidence for a definitive genetic contribution to RDS, investigators have attempted to identify specific genes that may contribute to its risk. The studies of SP-A and SP-B genes associated with RDS have been summarized in Table 6. Logistic regression analysis was used to test whether SP-C alleles coding for 138 Asn or 186 Asn explained the risk of RDS when gender was included in the analysis as a confounding factor. It was found that both alleles were independent risk factors for RDS (22). Recently, a variant of the SP-D gene (rs1923537) was associated with a lower prevalence of RDS (23). Another case-control study has suggested an association of G protein-coupled receptor for asthma susceptibility (GPR154 or GPRA) and neonatal RDS (24).
To the extent that some of these candidate gene studies show a significance for various alleles, polymorphisms, and haplotypes does not address the central question: to what extent is RDS a genetic disease? Knowing this will determine whether further studies are justified to identify the genes that comprise the additive genetic effect in the ACE modeling, to identify genetic modifiers encoded in chromosomes, or to identify epigenetic modifiers, with the ultimate goal of informing rationale drug design. Although surfactant-B deficiency is a validated autosomal dominant lethal form of lung disease (25), it is rare and does not significantly contribute to the common forms of RDS encountered by neonatologists daily; nor does it necessarily follow that because surfactant proteins are encoded in the chromosomal DNA, therefore RDS is genetic.
The data reported in this study are the first to quantify the genetic component to RDS. The strengths of our study include a large number of twins from a very heterogeneous population, and data on a large number of known confounding variables, including fertility treatment, prenatal steroids, and maternal information related to pregnancy-specific conditions.
There are some limitations to our study. The zygosity was determined using ultrasound, placental histopathology, and gender, instead of DNA confirmation. A monochorionic placenta was regarded as representing MZ twins. Approximately 9% of similar gender dichorionic placentas are MZ (26). The results were not affected when adjustments were made for these worst-case scenarios. We included most of the known potential contributing factors, but there may be other factors that could affect the outcome of RDS. We did attempt to control for these unknown variables in our statistical model.
Twin studies are a powerful non-DNA-based approach to determine the amount of the variance contributed by total genetic effects. These analyses are conditioned by the assumption that MZ twins share 100% of their chromosomal DNA and that DZ twins share, on average, 50%. The heritability of ∼50% for RDS is significant and comparable with that of other medical conditions, such as bronchopulmonary dysplasia (27,28) and retinopathy of prematurity (29). Although epigenetics and other modifications to chromosomal DNA may suggest that these assumptions should slightly be adjusted, non-DNA-based twin heritability studies remain robust.
We conclude that there is a strong genetic susceptibility to the development of RDS in preterm infants. This should act as a further impetus to spur the identification of the genetic elements of this condition, which, in turn, has the potential to make a significant impact on neonatal outcomes.
Abbreviations
- ACE:
-
additive genetic, common environmental and residual effects
- BW:
-
birth weight
- DZ:
-
dizygotic
- IVF:
-
in vitro fertilization
- MELR:
-
mixed effects logistic regression
- MZ:
-
monozygotic
- SP:
-
surfactant proteins
References
Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR, Bauer CR, Donovan EF, Korones SB, Laptook AR, Lemons JA, Oh W, Papile LA, Shankaran S, Stevenson DK, Tyson JE, Poole WK 2007 Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol 196: 147.e141–e148
Dani C, Reali MF, Bertini G, Wiechmann L, Spagnolo A, Tangucci M, Rubaltelli FF 1999 Risk factors for the development of respiratory distress syndrome and transient tachypnoea in newborn infants. Italian Group of Neonatal Pneumology. Eur Respir J 14: 155–159
Dempsey E, Chen MF, Kokottis T, Vallerand D, Usher R 2005 Outcome of neonates less than 30 weeks gestation with histologic chorioamnionitis. Am J Perinatol 22: 155–159
Namavar Jahromi B, Ardekany MS, Poorarian S 2000 Relationship between duration of preterm premature rupture of membranes and pulmonary maturation. Int J Gynaecol Obstet 68: 119–122
Ziadeh SM, Sunna E, Badria LF 2000 The effect of mode of delivery on neonatal outcome of twins with birthweight under 1500 grams. J Obstet Gynaecol 20: 389–391
Klein JM, Nielsen HC 1993 Androgen regulation of epidermal growth factor receptor binding activity during fetal rabbit lung development. J Clin Invest 91: 425–431
Luerti M, Parazzini F, Agarossi A, Bianchi C, Rocchetti M, Bevilacqua G 1993 Risk factors for respiratory distress syndrome in the newborn. A multicenter Italian survey. Study Group for Lung Maturity of the Italian Society of Perinatal Medicine. Acta Obstet Gynecol Scand 72: 359–364
Hacking D, Watkins A, Fraser S, Wolfe R, Nolan T 2001 Respiratory distress syndrome and birth order in premature twins. Arch Dis Child Fetal Neonatal Ed 84: F117–F121
Balchin I, Whittaker JC, Lamont RF, Steer PJ 2008 Timing of planned cesarean delivery by racial group. Obstet Gynecol 111: 659–666
Marttila R, Kaprio J, Hallman M 2004 Respiratory distress syndrome in twin infants compared with singletons. Am J Obstet Gynecol 191: 271–276
Shinwell ES, Blickstein I, Lusky A, Reichman B 2004 Effect of birth order on neonatal morbidity and mortality among very low birthweight twins: a population based study. Arch Dis Child Fetal Neonatal Ed 89: F145–F148
Mathews TJ, MacDorman MF 2007 Infant mortality statistics from the 2004 period linked birth/infant death data set. Natl Vital Stat Rep 57: 1–32
Sinha SK, Gupta S, Donn SM 2008 Immediate respiratory management of the preterm infant. Semin Fetal Neonatal Med 13: 24–29
American Lung Association 2008 Respiratory distress syndrome and bronchopulmonary dysplasia. Available at: http://www.lungusa.org/site/c.dvLUK9O0E/b.4023541. Accessed July 23, 2009.
Holzman C, Lin X, Senagore P, Chung H 2007 Histologic chorioamnionitis and preterm delivery. Am J Epidemiol 166: 786–794
Feng R, Zhou G, Zhang M, Zhang H 2008 Analysis of twin data using SAS. Biometrics 65: 584–589
Falconer DS, Mackay TF 1996 Introduction to Quantitative Genetics. Prentice Hall, Harlow, UK
Nagourney BA, Kramer MS, Klebanoff MA, Usher RH 1996 Recurrent respiratory distress syndrome in successive preterm pregnancies. J Pediatr 129: 591–596
Myrianthopoulos NC, Churchill JA, Baszynski AJ 1971 Respiratory distress syndrome in twins. Acta Genet Med Gemellol (Roma) 20: 199–204
van Sonderen L, Halsema EF, Spiering EJ, Koppe JG 2002 Genetic influences in respiratory distress syndrome: a twin study. Semin Perinatol 26: 447–449
Marttila R, Haataja R, Ramet M, Lofgren J, Hallman M 2003 Surfactant protein B polymorphism and respiratory distress syndrome in premature twins. Hum Genet 112: 18–23
Lahti M, Marttila R, Hallman M 2004 Surfactant protein C gene variation in the Finnish population— association with perinatal respiratory disease. Eur J Hum Genet 12: 312–320
Hilgendorff A, Heidinger K, Bohnert A, Kleinsteiber A, Konig IR, Ziegler A, Lindner U, Frey G, Merz C, Lettgen B, Chakraborty T, Gortner L, Bein G 2009 Association of polymorphisms in the human surfactant protein-D (SFTPD) gene and postnatal pulmonary adaptation in the preterm infant. Acta Paediatr 98: 112–117
Pulkkinen V, Haataja R, Hannelius U, Helve O, Pitkanen OM, Karikoski R, Rehn M, Marttila R, Lindgren CM, Hastbacka J, Andersson S, Kere J, Hallman M, Laitinen T 2006 G protein-coupled receptor for asthma susceptibility associates with respiratory distress syndrome. Ann Med 38: 357–366
Nogee LM, Garnier G, Dietz HC, Singer L, Murphy AM, deMello DE, Colten HR 1994 A mutation in the surfactant protein B gene responsible for fatal neonatal respiratory disease in multiple kindreds. J Clin Invest 93: 1860–1863
Bhandari V, Zhou G, Bizzarro MJ, Buhimschi C, Hussain N, Gruen JR, Zhang H 2009 Genetic contribution to patent ductus arteriosus in the premature newborn. Pediatrics 123: 669–673
Bhandari V, Bizzarro MJ, Shetty A, Zhong X, Page GP, Zhang H, Ment LR, Gruen JR 2006 Familial and genetic susceptibility to major neonatal morbidities in preterm twins. Pediatrics 117: 1901–1906
Lavoie PM, Pham C, Jang KL 2008 Heritability of bronchopulmonary dysplasia, defined according to the consensus statement of the national institutes of health. Pediatrics 122: 479–485
Bizzarro MJ, Hussain N, Jonsson B, Feng R, Ment LR, Gruen JR, Zhang H, Bhandari V 2006 Genetic susceptibility to retinopathy of prematurity. Pediatrics 118: 1858–1863
Kala P, Ten Have T, Nielsen H, Dunn M, Floros J 1998 Association of pulmonary surfactant protein A (SP-A) gene and respiratory distress syndrome: interaction with SP-B. Pediatr Res 43: 169–177
Ramet M, Haataja R, Marttila R, Floros J, Hallman M 2000 Association between the surfactant protein A (SP-A) gene locus and respiratory-distress syndrome in the Finnish population. Am J Hum Genet 66: 1569–1579
Haataja R, Ramet M, Marttila R, Hallman M 2000 Surfactant proteins A and B as interactive genetic determinants of neonatal respiratory distress syndrome. Hum Mol Genet 9: 2751–2760
Floros J, Fan R, Diangelo S, Guo X, Wert J, Luo J 2001 Surfactant protein (SP) B associations and interactions with SP-A in white and black subjects with respiratory distress syndrome. Pediatr Int 43: 567–576
Haataja R, Marttila R, Uimari P, Lofgren J, Ramet M, Hallman M 2001 Respiratory distress syndrome: evaluation of genetic susceptibility and protection by transmission disequilibrium test. Hum Genet 109: 351–355
Makri V, Hospes B, Stoll-Becker S, Borkhardt A, Gortner L 2002 Polymorphisms of surfactant protein B encoding gene: modifiers of the course of neonatal respiratory distress syndrome?. Eur J Pediatr 161: 604–608
Marttila R, Haataja R, Guttentag S, Hallman M 2003 Surfactant protein A and B genetic variants in respiratory distress syndrome in singletons and twins. Am J Respir Crit Care Med 168: 1216–1222
Thomas NJ, Fan R, Diangelo S, Hess JC, Floros J 2007 Haplotypes of the surfactant protein genes A and D as susceptibility factors for the development of respiratory distress syndrome. Acta Paediatr 96: 985–989
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported, in part, by Grant T32 HD 07094 from the National Institute of Child Health and Human Development Training (O.L.) and Grants K02DA017713 and R01DA016750 from the National Institute on Drug Abuse (H.Z. and Y.J.). Supported by Grant R01 NS43530 from the National Institute of Neurological Disorders and Stroke (J.R.G.) and Grant K08 HL 074195 from the National Heart, Lung, and Blood Institute (V.B.).
Presented as a poster at the Pediatric Academic Societies Meeting at Baltimore, MD, May 2-5, 2009.
Rights and permissions
About this article
Cite this article
Levit, O., Jiang, Y., Bizzarro, M. et al. The Genetic Susceptibility to Respiratory Distress Syndrome. Pediatr Res 66, 693–697 (2009). https://doi.org/10.1203/PDR.0b013e3181bbce86
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3181bbce86