Abstract
Adenotonsillar hypertrophy is the major pathophysiological mechanism underlying obstructive sleep apnea (OSA) and recurrent tonsillitis (RI) in children. The increased expression of various mediators of the inflammatory response in tonsils of patients with OSA prompted our hypothesis that the enhanced local and systemic inflammation in children with OSA would promote tonsillar proliferation. Mixed cell cultures from tonsils recovered during adenotonsillectomy in children with OSA and RI were established, and proliferative rates were assessed. Cells were also cultured to determine the levels of proinflammatory cytokines and antioxidant protein levels and mRNA expression. Global cell proliferative rates from OSA tonsils were significantly higher than RI (p < 0.01), with CD3+, CD4+, and CD8+ cell proliferation being higher in OSA (p < 0.05). Moreover, proinflammatory cytokines, such as TNF-α, IL-6, and IL-1α, were highly expressed in OSA-derived tonsils. Furthermore, thioredoxin (TRX), an antioxidant protein, was also highly expressed in OSA tonsils at the mRNA and protein levels (p < 0.01). Thus, T cells are in a highly proliferative state in the tonsils of children with OSA and are associated with increased production of proinflammatory cytokines and TRX, when compared with children with RI.
Similar content being viewed by others
Main
Obstructive sleep apnea (OSA), a condition characterized by repetitive increases in upper airway resistance and collapse, is a common health problem in children affecting 1 to 3% of children during their first decade of life (1). In a series of previous studies from our and other laboratories, it has become apparent that children with OSA are at increased risk for a vast array of morbidities, principally affecting the CNS and cardiovascular systems (2–9). Adenotonsillar hypertrophy has been recognized as the major pathophysiological contributor of OSA in children (10), and it plays an important role as well in recurrent tonsillitis (RI) (11). Consequently, adenotonsillectomy (T&A) is currently the first line of treatment for children with these conditions (12,13). However, the exact mechanisms underlying follicular lymphoid proliferation and hyperplasia remain extremely poorly understood. In adults, there are several lines of evidence, suggesting that both local upper airway and systemic inflammation are implicated in the pathophysiology of this a priori mechanical dysfunction of the upper airway. For example, the number of immune cells is substantially increased in the upper airway mucosa and the muscle of adults with OSA (14). Similar increases in regional and systemic inflammatory markers have also been reported in children with OSA (15–17). In addition, increased expression of mediators of the inflammatory response, such as cysteinyl leukotrienes and glucocorticoid receptors, is consistently found in tonsillar tissues of children with OSA (18–20). Therefore, we hypothesized that cellular proliferation of tonsillar tissues in children with OSA would differ from that of children with RI, possibly reflecting different pathologic mechanisms and cell type involvement leading to the enlargement of upper airway lymphoid tissue in these two conditions.
METHODS
Subjects.
The study was approved by the University of Louisville Human Research Committee, and informed consent was obtained for each participant. Consecutive children with adenotonsillar hypertrophy who underwent tonsillectomy for either OSA or RI were identified. Overnight polysomnography was performed using standard methods (21–23). The diagnosis of OSA was defined as an obstructive apnea-hypopnea index (AHI) ≥5/h of total sleep time. Diagnosis of RI was based on a history of >5 tonsillar infections over a period of <6 mo, requiring administration of antibiotics, in the absence of any symptoms suggestive of OSA using a validated questionnaire (24). Overnight sleep studies were performed in the majority of children with RI (13 of 20), and showed AHI <1/h of total sleep time.
Cell culture.
Tonsils were placed in ice-cold PBS plus antibiotics, and processing began <30 min after surgical excision. Tonsils were manually dissected and gently grounded with a syringe plunger through a 70-μ mesh screen. Red blood cells were removed by lysis buffer. Cellular viability was determined by trypan blue exclusion. Specimens with a viability <70% were discarded. Cell cultures were established in standard medium RPMI 1640 supplemented with 10% heat-inactivated fetal bovine serum (FBS) plus antibiotics, which included streptomycin, fungisone, gentamicin, and penicillin. Mixed cell suspensions were transferred onto 96-round-bottom well plates at a concentration of 1 × 106 cells/well and cultured in a 5% CO2 incubator at 37°C for 48 h. Cells were also cultured using 24-well plates to determine the proinflammatory cytokine levels, to conduct flow cytometric analysis, and to extract RNA for real time quantitative PCR assays or protein for western blot analyses.
Total cell proliferation assay.
Cell proliferation was measured using a CellTiter 96 AQ nonradioactive cell proliferation assay (Promega, Madison, WI). Briefly, cells were plated in 96-well plates at a density of 1 × 106 cells/well in 200 μL of medium for 48 h; then MTS [3-(4,5-dimethylthiazol-2yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium]-phenozine methosulfate solution (30 μL/well) was added to the wells. After incubation for 4 h, the absorbance was measured at 490 nm using a plate reader (Multiscan EX, Thermo Scientific, Waltham, MA). Data representing the average of four wells were considered as one experiment.
Bromodeoxyuridine (BrdU) cell proliferation assay with flow cytometry.
To detect T-cell- and B-cell-specific proliferation, we used BrdU pulsed proliferation analysis using flow cytometry. All procedures were measured using the APC BrdU flow kit (BD Biosciences, San Diego, CA), as recommended by the manufacturer. In brief, at the end of 48 h of cell culture, cells were pulse-labeled with 1 mM BrdU for 4 h. BrdU-labeled cells were stained with a 3-color antibody combination consisting of mouse anti-human CD45/PerCP Cy7, CD3/PE, and CD19/APC-Cy7 antibodies (BD Biosciences, San Diego, CA) in 50 μL staining buffer for 15 min on ice. Cells were fixed and permeabilized with cytofix or cytoperm buffer, suspended with DNase (300 μg/mL) for 1 h at 37°C, and anti-BrdU APC antibody was added and incubated for 20 min at room temperature. Isotype controls relevant for each antibody were used to establish background fluorescence. Negative control was used as a sample, which was untreated with BrdU and was not stained with specific fluorescence antibodies. Data were acquired on a FACS Aria flow cytometer using the FACS Diva 5.5 software (BD Biosciences, San Diego, CA). After gating of lymphocytes based on CD45+ cells, T-cell and B-cell numbers were calculated as CD3+/CD19− and CD3−/CD19+ cell populations, respectively. Moreover, counting CD3+/BrdU+ and CD19+/BrdU+ cell populations identified proliferation of T cells and B cells. The results were displayed as two color dot-plots and analyzed by FlowJo software (Tree Star, San Carlos, CA). All data are expressed as the percentage of positive cell from the total cell population.
Quantitative real-time RT-PCR for cytokine expression and thioredoxin.
Total RNA was isolated with Qiagen RNAeasy mini kit (Qiagen Inc, CA). Total RNA was quantified by spectrophotometer based on the absorbance A260/A280 ratio. Quantitative real-time PCR were performed using TaqMan one-step RT-PCR reagents kits (Applied Biosystems, Foster City, CA) according to the manufacturer's instructions. The genes examined included TNF-α (NM_000594), IL-6 (NM_000600), IL-1 α (NM_000575), thioredoxin (TRX) (×77584), CD4 (NM_000616.), and CD8a (NM_171827). In brief, all reactions were carried out in a final volume of 20 μL containing 11.5 μL 2× master mix, 0.5 μL RNase inhibitor mix, 1 μL primer (20 μM), 200 ng total RNA, and the volume of RNAse free water was adjusted with template. Thermocycling was run on an ABI 7500 real-time PCR system (Applied Biosystems, Foster City, CA) as follows: 30 min at 50°C, 10 min at 95°C, 40 cycles of 15 s at 95°C, and 1 min at 60°C. Samples were normalized using the housekeeping gene, ribosomal 18S rRNA. Individual gene expression was calculated using the comparative Ct method (25). Specific mRNA expression in OSA was expressed as the relative fold increase compared with RI samples.
Detection of TNF-α, IL-6, and IL-1α in cell culture supernatants.
Proinflammatory cytokines levels, such as TNF-α, IL-6, and IL-1 α, were measured in cell-free supernatants with commercially available kits (R&D system, Minneapolis, MN) according to protocols provided by the manufacturer. Each of samples was assayed in duplicate. Interassay and intraassay coefficients of variability ranged from 3.4 to 5.3% and 3.4 to 4.5%, respectively.
Western blots.
Cells were lysed using a nuclear extract kit (Active Motiff, Carlsbad, CA). Protein concentrations were measured using the DC protein assay (BioRad, Hercules, CA). TRX expression was assessed by immunoblotting with anti-human TRX MAb (1:1000, BD Biosciences, San Diego, CA) and mouse anti-rabbit IgGs that were conjugated to horseradish peroxidase in a Tris-buffered saline supplemented with 5% nonfat dry milk. Bands corresponding to TRX were visualized with ECL and quantified in a scanner with ImageQuant software (Molecular Dynamics, GE Health Science). Normalization of integrated densities was performed by reprobing membranes with β-actin antibody.
Immunohistochemistry.
Coronal sections (40 μm) of tonsils from OSA and RI were initially incubated in 1× citrate buffer (Lab Vision Corporation, Fremont, CA) at 95°C for 45 min, washed several times in PBS, and blocked with a PBS or 0.4% Triton X-100/0.5% Tyramide Signal Amplification (TSA, Perkin Elmer Life Sciences, Boston, MA) blocking reagent or 10% normal horse serum for 1 h. Sections were then serially incubated with anti-CD4 antibody (1:300, Santa Cruz Biotechnology, Santa Cruz, CA) or anti-CD8 antibody (1:1000, BD Pharmagen, San Jose, CA) at 4°C for 24 h, and then washed in PBS six times for 5 min each wash. Sections were incubated for 1 h in horse anti-mouse biotinylated antibody (1:400, Vector Labs, Burlingame, CA) in a PBS or 0.4% TSA blocking reagent or 10% horse serum solution and then with streptavidin-horseradish peroxidase diluted 1:100 in PBS/0.5% TSA blocking reagent. Subsequently, the sections were incubated with TSA fluorescein reagents diluted 1:50 in amplification diluent (Perkin Elmer Life Sciences) for 2 min. Sections were then washed and mounted onto glass slides. Negative controls were prepared by either omitting the primary or the secondary antibody. Sections were prepared from five sets of tonsils from either OSA or RI groups and were visualized using a fluorescent microscope by an investigator who was blinded to the sample source.
Statistical analysis.
All data were expressed by mean ± SD. Statistical analyses were performed using SPSS software (version 16.0; SPPS Inc., Chicago, IL). All p values reported are two-tailed with statistical significance set at <0.05.
RESULTS
Study population.
The demographic, polysomnographic, and tonsillar cell distribution characteristics of the OSA and RI cohorts are shown in Table 1. The mean age of children with OSA and RI was 6.2 ± 2.8 y and 5.8 ± 2.2 y, respectively, and genders and ethnicities were similarly represented. All OSA subjects had AHI >5/hrTST, with 12 subjects having AHI <10/hrTST, 10 subjects with AHI ≥10 but <20 /hrTST, and 3 subjects with AHI >20/hrTST. The total percentage of lymphocytes was higher in children with OSA, and the percentage of CD3+ T lymphocytes was also higher in children with OSA compared with RI (18.1 ± 4.1% versus 9.3 ± 3.9%, p < 0.05). In contrast, CD19+ B lymphocytes tended to be less abundant in OSA (42.8 ± 3.8% versus 48.1 ± 3.5%; p = 0.055).
Cell proliferation in tonsil mixed cell culture.
Cellular proliferative assays showed that the tonsils of children with OSA had significantly higher proliferative rates than those of RI (Fig. 1; OD units: 1.45 ± 0.06 versus 0.82 ± 0.02, p < 0.01).
T-cell and B-cell proliferation in tonsils.
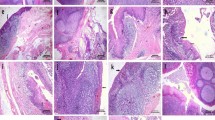
To assess T-cell and B-cell proliferation, we used the BrdU proliferation assay in combination with flow cytometry. Figure 2A illustrates the strategy for identification of and sorting of T cells and B cells. As shown in Figure 2B, the proportion of proliferating of CD3+ T cells was significantly higher in children with OSA compared with children with RI (OSA versus RI: 5.49 ± 2.10% versus 2.74 ± 0.97%, p < 0.05). However, proliferation of CD19+ B cells in children with OSA was reduced (OSA versus RI: 2.80 ± 1.04% versus 4.3 ± 1.41%, p < 0.05). In addition, mRNA expression studies in tonsil cultures from children with OSA and RI confirmed that both CD4+ and CD8+ mRNA were highly expressed in children with OSA compared with RI (Fig. 3), with CD4+ being the predominant cell type (Fig. 3). Both these T cell types were primarily located in the tonsillar extrafollicular area.
Proliferation of CD3+ and CD19+ cells in tonsils from children with OSA and RI in a mixed cell culture system. A. Illustrative example of the flow cytometry-based strategy for detection of CD3+ and CD19+ cell proliferation. B. CD3+ (▪) and CD19+ (□) cell proliferation in tonsillar cultures in a mixed cell culture system in children with OSA (n = 12) and RI (n = 11). Data are expressed as the percentage of BrdU+ cells out of total CD3+ and CD19+cell populations. *p < 0.05.
CD4+ and CD8+ expression in intact tonsillar tissues and in a mixed cell culture system in children with OSA and RI. A. Representative immunohistochemical assessment for CD4+ and CD8+ in tonsils from children with OSA and RI. A higher abundance of CD4+ (Green) and CD8+ (Red) is apparent in the children with OSA. Scaling bars indicate 200 μm for upper panels and 50 μm for lower panels. B. CD4 (▪) and CD8 (□) mRNA expression in a mixed tonsillar cell culture system in children with OSA (n = 12) and RI (n = 11). Data are expressed as relative fold increases relative to RI. *p < 0.05.
Protein concentration and mRNA expression of TRX.
Figure 4 shows mRNA and protein expression of TRX in cells derived from tonsils in children with OSA and RI. As seen in Figure 4A, there was a 2.6-fold increase in TRX mRNA expression in children with OSA (p < 0.01). In addition, western blots confirmed these findings, such that TRX protein expression was markedly increased in tonsils from children with OSA (OSA versus RI; relative intensity: 0.86 ± 0.19 versus 0.28 ± 0.16, p < 0.01).
TRX expression at both protein and mRNA levels in children with OSA (n = 12) and RI (n = 11) in a mixed tonsillar cell culture system. A. TRX mRNA expression in children with OSA compared with children with RI, Data are expressed as fold increase relative to RI. B. Representative immunoblots are shown of TRX (detected at 12 kD) and β-actin. Data are summarized graphically in relative intensity units. **p < 0.01.
Proinflammatory cytokine expression in mixed tonsil cell culture system.
Figure 5A shows the concentrations in supernatants of proinflammatory cytokines. TNF-α and IL-6 concentrations were higher in children with OSA than in cultures from children with RI (OSA versus RI: TNF-α: 29.2 ± 6.2 pg/mL versus 10.5 ± 5.6 pg/mL, p < 0.01; IL-6: 49.6 ± 7.3 pg/mL versus 22.6 ± 9.7 pg/mL, p < 0.01). Similarly, IL-1α levels were also increased in OSA samples (OSA versus RI: 42.2 ± 9.81 pg/mL versus 25.5 ± 8.7 pg/mL, p < 0.05). As seen in Figure 5B, mRNA expression of TNF-α, IL-6, and IL-1α in tonsillar cells from children with OSA was significant higher than in children with RI (p < 0.05).
Pro-inflammatory cytokine expression at both protein and mRNA levels in children with OSA and RI in a mixed tonsillar cell culture system. A. TNF-α (▪), IL-6 (□), and IL-1α ( ) pro-inflammatory cytokine concentrations in cell-free supernatants in children with OSA (n = 23) compared with children with RI (n = 19). B. TNF-α (▪), IL-6 (□), and IL-1α (
) pro-inflammatory cytokine concentrations in cell-free supernatants in children with OSA (n = 23) compared with children with RI (n = 19). B. TNF-α (▪), IL-6 (□), and IL-1α ( ) mRNA expression in children with OSA (n = 12) compared with children with RI (n = 11). Data are expressed as fold increase. *p < 0.05, **p < 0.01.
) mRNA expression in children with OSA (n = 12) compared with children with RI (n = 11). Data are expressed as fold increase. *p < 0.05, **p < 0.01.
DISCUSSION
In this study, we show that proliferative rates are increased in tonsil mixed cell cultures harvested from children with OSA during routine T&A compared with children with RI, and this process seems to be mediated by T cells, whereas the reverse seems to occur in RI, with B cells assuming a more predominant role. Furthermore, both expression and release of proinflammatory cytokines to the supernatants, such as TNF-α, IL-6, and IL-1α, were increased in OSA, and in addition, evidence for up-regulation of the gene TRX and its transcript protein in OSA-derived cells. Taken together, the data presented herein suggest that the mechanisms underlying upper airway lymphadenoid tissue proliferation in OSA and RI are distinct and may allow for future nonsurgical disease-specific therapeutic interventions that may ultimately obviate the need for T&A, while leading to involution of the hypertrophic adenoids and tonsils.
Several methodological issues deserve to be addressed. First, the remarkable similarity between the qualitative findings in the tonsillar immunohistochemistry regarding cell type distribution and the percentage of lymphocytes subtypes identified in cell culture using flow cytometry would suggest that processing of the tonsillar tissues harvested during surgery did not alter the constitutive cell populations of these tissues. Moreover, the standard procedures used herein would be expected to have a similar influence on tonsils collected from children with OSA and RI. Thus, the differences in proliferation, cytokine release, and TRX expression between the two cohorts seem to reflect the divergent intrinsic properties of these tissues, rather than reflect consequences of procedural methodologies. However, we should also remark that some differences in lymphocyte properties have been noted when different tissue processing procedures were used (26). Second, only palatine tonsils were included in this study, and therefore, differences in cytokine networks could emerge between nasopharyngeal lymphadenoid tissues and palatine tonsils, and future studies will have to examine this issue (27). Third, the two groups had similar age, gender, and ethnicity, and overnight sleep studies were conducted in the majority of children with RI, such as to more objectively confirm the two major diagnoses leading to T&A in children. Obviously, tonsil tissues from healthy children are unavailable for ethical reasons. Finally, we did not specifically assess the contributions of allergic sensitization and viral exposures on the etiology of tonsillar proliferation in either OSA or RI. Previous studies have reported a high prevalence of allergic sensitization in children with OSA (28,29), and early exposure of respiratory viruses could modify the proliferative properties of tonsils through up-regulation of nerve growth factor and neurokinin 1 receptor dependent pathways (22,30,31). Thus, further studies regarding the potential contributions of these factors are needed.
There is no doubt that adenotonsillar hypertrophy constitutes the primary contributor to OSA in children, and even if T&A does not always result in cure, significant improvements in the severity of sleep-disordered breathing are usually the rule (32–35). However, very little is known on the mechanisms that mediate proliferation of tonsils in children with either OSA or RI. We have previously shown that pathways of inflammation play a role, because both topical corticosteroids and leukotriene receptor modifiers were found to be highly effective in reversing tonsillar hypertrophy, and their receptors display increased expression patterns in the upper airways of children with OSA (16,18–21,36,37). Moreover, nerve growth factor and substance P, a major controller of sensorineural development and neuroimmuno-inflammatory responses, are also overexpressed in the tonsils tissues from children with OSA (22). Notwithstanding such encouraging results, these studies did not quantitatively assess the proliferative characteristics of tonsillar tissues in OSA or RI and did not provide information as to the major cellular populations that are regulated in this process. Therefore, we used a mixed in vitro cell culture model to more quantitatively investigate potential relationships between inflammatory responses and cell proliferation.
Considering the increased inflammatory markers in the upper airway of pediatric patients with OSA (16–19,21,22), the increased proliferative activity in tonsils from children with OSA was not unanticipated. However, and of particular interest, were the findings on the differential patterns of proliferation among T cells and B-cells in the two patient cohorts, with a T cell predominant response in OSA being associated with higher expression and release of the proinflammatory cytokines TNF-α, IL-6, and IL-1α. It is now accepted that recurrent vibration in the upper airway may promote the development of local inflammatory responses, leading to mucosal swelling (38,39), lymphadenoid tissue proliferation, and upper airway obstruction. Indeed, CD4+, CD8+, and activated CD25+ T cells were preferentially present in the mucosa and underlying muscle of the upper airway of adult patients with OSA (14). These findings have been recently confirmed (40). In children, Li et al. (17) showed marked increases in sputum neutrophil counts in OSA that correlated with the severity of the disease. The increases in serum high sensitivity C-reactive protein levels in children OSA would further attest to the presence of a systemic, inflammatory process that could also contribute to the increased proliferation of the upper airway lymphoid tissues (41–44). Based on aforementioned considerations, the favorable response of children with OSA to topical corticosteroids (37,45), and current findings, we propose that local and systemic activation of inflammatory pathways will promote preferential T-cell proliferation and upper airway lymphoid hyperplasia.
TRX has been characterized as a new oxidative stress inducible protein, and it plays an important role in intracellular signaling and resistance against oxidative stress (46). A multitude of stimuli may lead to increased TRX cellular expression, including hypoxia, lipopolysaccharide, hydrogen peroxide, and viral infections (47,48). TRX is actively secreted by a variety of normal and transformed cells, including fibroblasts, airway epithelial cells, and activated T cells (49). In a previous study, Park and Suzuki (50) proposed that TRX is mechanistically involved in intermittent hypoxia-mediated alterations in the susceptibility of the heart to oxidative stress. Recently, and in support for a potential role of TRX in OSA, adult patients with this condition had higher plasma TRX levels that were reduced after treatment with continuous positive airway pressure (51). In this study, we found that expression of TRX was markedly higher in tonsillar cells derived from children with OSA. Although we are still unclear as to the mechanisms responsible for the differential expression of TRX, we postulate that TRX may be involved in protection from oxidative stress and may also be modulating T-cell proliferative activity, and we cannot exclude a role in other inflammatory cell types, such as neutrophils. If the latter proves to be accurate, it may provide a viable target for development of interventional approaches for treatment or prevention of tonsillar hypertrophy in children with OSA.
In summary, we have established that T cells are in a highly proliferative state in the tonsils of children with OSA and are associated with increased production of proinflammatory cytokines and TRX, when compared with children with RI. These findings not only shed additional light on the differential regulatory mechanisms underlying tonsillar hypertrophy in two common pediatric conditions, namely RI and OSA, but also provide an in vitro model that should permit objective characterization and development of specific treatments for these disease processes.
Abbreviations
- AHI:
-
Obstructive Apnea Hypopnea Index
- BrdU:
-
bromodeoxyuridine
- OSA:
-
obstructive sleep apnea
- RI:
-
recurrent infection
- TRX:
-
thioredoxin
References
Lumeng JC, Chervin RD 2008 Epidemiology of pediatric obstructive sleep apnea. Proc Am Thorac Soc 5: 242–252
Gozal D 1998 Sleep-disordered breathing and school performance in children. Pediatrics 102: 616–620
Chervin RD, Archbold KH 2001 Hyperactivity and polysomnographic findings in children evaluated for sleep-disordered breathing. Sleep 24: 313–320
Amin RS, Kimball TR, Kalra M, Jeffries JL, Carroll JL, Bean JA, Witt SA, Glascock BJ, Daniels SR 2005 Left ventricular function in children with sleep-disordered breathing. Am J Cardiol 95: 801–804
Gozal D, Kheirandish-Gozal L 2007 Neurocognitive and behavioral morbidity in children with sleep disorders. Curr Opin Pulm Med 13: 505–509
Kheirandish L, Gozal D 2006 Neurocognitive dysfunction in children with sleep disorders. Dev Sci 9: 388–399
O'Brien LM, Mervis CB, Holbrook CR, Bruner JL, Smith NH, McNally N, McClimment MC, Gozal D 2004 Neurobehavioral correlates of sleep-disordered breathing in children. J Sleep Res 13: 165–172
Capdevila OS, Kheirandish-Gozal L, Dayyat E, Gozal D 2008 Pediatric obstructive sleep apnea: complications, management, and long-term outcomes. Proc Am Thorac Soc 5: 274–282
Gozal D, Kheirandish-Gozal L, Serpero LD, Sans Capdevila O, Dayyat E 2007 Obstructive sleep apnea and endothelial function in school-aged nonobese children: effect of adenotonsillectomy. Circulation 116: 2307–2314
Katz ES, D'Ambrosio CM 2008 Pathophysiology of pediatric obstructive sleep apnea. Proc Am Thorac Soc 5: 253–262
Webb CJ, Osman E, Ghosh SK, Hone S 2004 Tonsillar size is an important indicator of recurrent acute tonsillitis. Clin Otolaryngol Allied Sci 29: 369–371
Schechter MS, Section on Pediatric Pulmonology Subcommittee on Obstructive Sleep Apnea Syndrome 2002 Technical report: diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics 109: e69
Darrow DH, Siemens C 2002 Indications for tonsillectomy and adenoidectomy. Laryngoscope 112: 6–10
Boyd JH, Petrof BJ, Hamid Q, Fraser R, Kimoff RJ 2004 Upper airway muscle inflammation and denervation changes in obstructive sleep apnea. Am J Respir Crit Care Med 170: 541–546
Gozal D, Crabtree VM, Sans Capdevila O, Witcher LA, Kheirandish-Gozal L 2007 C-reactive protein, obstructive sleep apnea, and cognitive dysfunction in school-aged children. Am J Respir Crit Care Med 176: 188–193
Goldbart AD, Krishna J, Li RC, Serpero LD, Gozal D 2006 Inflammatory mediators in exhaled breath condensate of children with obstructive sleep apnea syndrome. Chest 130: 143–148
Li AM, Hung E, Tsang T, Yin J, So HK, Wong E, Fok TF, Ng PC 2007 Induced sputum inflammatory measures correlate with disease severity in children with obstructive sleep apnoea. Thorax 62: 75–79
Goldbart AD, Veling MC, Goldman JL, Li RC, Brittian KR, Gozal D 2005 Glucocorticoid receptor subunit expression in adenotonsillar tissue of children with obstructive sleep apnea. Pediatr Res 57: 232–236
Goldbart AD, Goldman JL, Li RC, Brittian KR, Tauman R, Gozal D 2004 Differential expression of cysteinyl leukotriene receptors 1 and 2 in tonsils of children with obstructive sleep apnea syndrome or recurrent infection. Chest 126: 13–18
Kaditis AG, Ioannou MG, Chaidas K, Alexopoulos EI, Apostolidou M, Apostolidis T, Koukoulis G, Gourgoulianis K 2008 Cysteinyl leukotriene receptors are expressed by tonsillar T cells of children with obstructive sleep apnea. Chest 134: 324–331
Goldbart AD, Goldman JL, Veling MC, Gozal D 2005 Leukotriene modifier therapy for mild sleep-disordered breathing in children. Am J Respir Crit Care Med 172: 364–370
Goldbart AD, Mager E, Veling MC, Goldman JL, Kheirandish-Gozal L, Serpero LD, Piedimonte G, Gozal D 2007 Neurotrophins and tonsillar hypertrophy in children with obstructive sleep apnea. Pediatr Res 62: 489–494
Montgomery-Downs HE, O'Brien LM, Gulliver TE, Gozal D 2006 Polysomnographic characteristics in normal preschool and early school-aged children. Pediatrics 117: 741–753
Montgomery-Downs HE, O'Brien LM, Holbrook CR, Gozal D 2004 Snoring and sleep-disordered breathing in young children: subjective and objective correlates. Sleep 27: 87–94
Livak KJ, Schmittgen TD 2001 Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods 25: 402–408
Giger B, Bonanomi A, Odermatt B, Ladell K, Speck RF, Kojic D, Berger C, Niggli FK, Nadal D 2004 Human tonsillar tissue block cultures differ from autologous tonsillar cell suspension cultures in lymphocyte subset activation and cytokine gene expression. J Immunol Methods 289: 179–190
Komorowska A, Komorowski J, Banasik M, Lewkowicz P, Tchorzewski H 2005 Cytokines locally produced by lymphocytes removed from the hypertrophic nasopharyngeal and palatine tonsils. Int J Pediatr Otorhinolaryngol 69: 937–941
McColley SA, Carroll JL, Curtis S, Loughlin GM, Sampson HA 1997 High prevalence of allergic sensitization in children with habitual snoring and obstructive sleep apnea. Chest 111: 170–173
Duchna HW, Rasche K, Lambers N, Orth M, Merget R, Schultze-Werninghaus G 1997 [Incidence of cutaneous sensitization to environmental allergens in obstructive sleep apnea syndrome]. Pneumologie 51: 763–766
Piedimonte G, Hegele RG, Auais A 2004 Persistent airway inflammation after resolution of respiratory syncytial virus infection in rats. Pediatr Res 55: 657–665
Piedimonte G, Rodriguez MM, King KA, McLean S, Jiang X 1999 Respiratory syncytial virus upregulates expression of the substance P receptor in rat lungs. Am J Physiol 277: L831–L840
Lipton AJ, Gozal D 2003 Treatment of obstructive sleep apnea in children: do we really know how?. Sleep Med Rev 7: 61–80
Tauman R, Gulliver TE, Krishna J, Montgomery-Downs HE, O'Brien LM, Ivanenko A, Gozal D 2006 Persistence of obstructive sleep apnea syndrome in children after adenotonsillectomy. J Pediatr 149: 803–808
Guilleminault C, Huang YS, Glamann C, Li K, Chan A 2007 Adenotonsillectomy and obstructive sleep apnea in children: a prospective survey. Otolaryngol Head Neck Surg 136: 169–175
Mitchell RB, Kelly J 2007 Outcome of adenotonsillectomy for obstructive sleep apnea in obese and normal-weight children. Otolaryngol Head Neck Surg 137: 43–48
Kaditis AG, Alexopoulos E, Chaidas K, Ntamagka G, Karathanasi A, Tsilioni I, Kiropoulos TS, Zintzaras E, Gourgoulianis K 2009 Urine concentrations of cysteinyl leukotrienes in children with obstructive sleep-disordered breathing. Chest 135: 1496–501
Kheirandish-Gozal L, Gozal D 2008 Intranasal budesonide treatment for children with mild obstructive sleep apnea syndrome. Pediatrics 122: e149–e155
Puig F, Rico F, Almendros I, Montserrat JM, Navajas D, Farre R 2005 Vibration enhances interleukin-8 release in a cell model of snoring-induced airway inflammation. Sleep 28: 1312–1316
Almendros I, Carreras A, Ramírez J, Montserrat JM, Navajas D, Farré R 2008 Upper airway collapse and reopening induce inflammation in a sleep apnoea model. Eur Respir J 32: 399–404
Series F, Chakir J, Boivin D 2004 Influence of weight and sleep apnea status on immunologic and structural features of the uvula. Am J Respir Crit Care Med 170: 1114–1119
Gozal D, Kheirandish L 2006 Oxidant stress and inflammation in the snoring child: confluent pathways to upper airway pathogenesis and end-organ morbidity. Sleep Med Rev 10: 83–96
Tauman R, Ivanenko A, O'Brien LM, Gozal D 2004 Plasma C-reactive protein levels among children with sleep-disordered breathing. Pediatrics 113: e564–e569
Khalyfa A, Capdevila OS, Buazza MO, Serpero LD, Kheirandish-Gozal L, Gozal D 2009 Genome-wide gene expression profiling in children with non-obese obstructive sleep apnea. Sleep Med 10: 75–86
Gozal D, Capdevila OS, Kheirandish-Gozal L 2008 Metabolic alterations and systemic inflammation in obstructive sleep apnea among nonobese and obese prepubertal children. Am J Respir Crit Care Med 177: 1142–1149
Alexopoulos EI, Kaditis AG, Kalampouka E, Kostadima E, Angelopoulos NV, Mikraki V, Skenteris N, Gourgoulianis K 2004 Nasal corticosteroids for children with snoring. Pediatr Pulmonol 38: 161–167
Hirota K, Nakamura H, Masutani H, Yodoi J 2002 Thioredoxin superfamily and thioredoxin-inducing agents. Ann N Y Acad Sci 957: 189–199
Kondo N, Nakamura H, Masutani H, Yodoi J 2006 Redox regulation of human thioredoxin network. Antioxid Redox Signal 8: 1881–1890
Yoshioka J, Schreiter ER, Lee RT 2006 Role of thioredoxin in cell growth through interactions with signaling molecules. Antioxid Redox Signal 8: 2143–2151
Perl A, Gergely P Jr Puskas F, Banki K 2002 Metabolic switches of T-cell activation and apoptosis. Antioxid Redox Signal 4: 427–443
Park AM, Suzuki YJ 2007 Effects of intermittent hypoxia on oxidative stress-induced myocardial damage in mice. J Appl Physiol 102: 1806–1814
Takahashi K, Chin K, Nakamura H, Morita S, Sumi K, Oga T, Matsumoto H, Niimi A, Fukuhara S, Yodoi J, Mishima M 2008 Plasma thioredoxin, a novel oxidative stress marker, in patients with obstructive sleep apnea before and after nasal continuous positive airway pressure. Antioxid Redox Signal 10: 715–726
Acknowledgements
We thank Kenneth R. Brittian for technical assistance with immunohistochemical procedures.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by National Institutes of Health grants HL-065270, HL-086662, and HL-083075 (D.G.), the Commonwealth of Kentucky Research Challenge for Excellence Trust Fund (D.G.), the Children's Foundation Endowment for Sleep Research (D.G.), and an investigator initiated grant from Merck Company (L.K.G.).
Rights and permissions
About this article
Cite this article
Kim, J., Bhattacharjee, R., Dayyat, E. et al. Increased Cellular Proliferation and Inflammatory Cytokines in Tonsils Derived From Children With Obstructive Sleep Apnea. Pediatr Res 66, 423–428 (2009). https://doi.org/10.1203/PDR.0b013e3181b453e3
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3181b453e3
This article is cited by
-
Association of preoperative neutrophil–lymphocyte ratios with the emergence delirium in pediatric patients after tonsillectomy and adenoidectomy: an observational prospective study
Journal of Anesthesia (2024)
-
Possible mechanism of CHI3L1 promoting tonsil lymphocytes proliferation in children with obstructive sleep apnea syndrome
Pediatric Research (2022)
-
Systemic corticosteroids could be used as bridge treatment in children with obstructive sleep apnea syndrome waiting for surgery
Sleep and Breathing (2022)
-
Haematologic Markers and Tonsil-to-Body Weight Ratio to Assist Adenotonsillar Hypertrophy Diagnosis
Indian Journal of Otolaryngology and Head & Neck Surgery (2022)
-
Association of chronic and acute inflammation of the mucosa-associated lymphoid tissue with psychiatric disorders and suicidal behavior
Translational Psychiatry (2019)