Abstract
Neonatal PMN (polymorphonuclear neutrophils) exhibit altered inflammatory responsiveness and greater longevity compared with adult PMN; however, the involved mechanisms are incompletely defined. Receptors containing immunoreceptor tyrosine-based inhibitory motif (ITIM) domains promote apoptosis by activating inhibitory phosphatases, such as Src homology domain 2-containing tyrosine phosphatase-1 (SHP-1), that block survival signals. Sialic acid-binding immunoglobulin-like lectin (Siglec)-9, an immune inhibitory receptor with an ITIM domain, has been shown to induce cell death in adult PMN in association with SHP-1. To test our hypothesis that neonatal PMN inflammatory function may be modulated by unique Siglec-9 and SHP-1 interactions, we compared expression of these proteins in adult and neonatal PMN. Neonatal PMN exhibited diminished cellular expression of Siglec-9, which was phosphorylated in the basal state. Granulocyte-macrophage colony-stimulating factor (GM-CSF) treatment decreased Siglec-9 phosphorylation levels in neonatal PMN but promoted its phosphorylation in adult PMN, observations associated with altered survival signaling. Although SHP-1 expression was also diminished in neonatal PMN, GM-CSF treatment had minimal effect on phosphorylation status. Further analysis revealed that Siglec-9 and SHP-1 physically interact, as has been observed in other immune cells. Our data suggest that age-specific interactions between Siglec-9 and SHP-1 may influence the altered inflammatory responsiveness and longevity of neonatal PMN.
Similar content being viewed by others
Main
Neutrophils figure prominently at tissue sites of microbial invasion and contribute to the clearance of pathogens. During resolution of the inflammatory process, neutrophils undergo apoptosis and are removed through ingestion by resident macrophages (1,2). However, a delay in the clearance of activated neutrophils promotes their persistence in tissues, a contributing factor in the pathogenesis of a variety of chronic inflammatory conditions (3). We reported a prolonged survival of neonatal neutrophils with enhanced inflammatory and cytotoxic activity (4,5). Altered inflammatory responses and delayed apoptosis may contribute to a variety of chronic inflammatory disorders in neonates, including bronchopulmonary dysplasia (6–8). Understanding the mechanisms modulating neonatal neutrophil responses to inflammation is therefore paramount in designing targeted therapeutic approaches.
Neonatal neutrophils have an intrinsic resistance to spontaneous and Fas-mediated apoptosis associated with decreased expression of proapoptotic proteins (4,9,10); however, the underlying mechanisms remain unclear. Compromise of this neutrophil function in neonates suggests a dysregulation of mechanisms important to inflammation and its resolution. Normally, the initiation and termination of inflammatory processes are tightly regulated through a combination of activating and inhibitory signals (11). An imbalance in this regulation could result in prolongation of processes that induce tissue damage and neutrophil reactivation, setting the stage for chronic inflammation.
Inhibitory signaling can be mediated by specialized surface immune inhibitory receptors that contain immunoreceptor tyrosine-based inhibitory motifs (ITIM) in the cytoplasmic domain (11). After receptor activation, tyrosine residues of the ITIM domain can be phosphorylated by Src family kinases, resulting in the recruitment of SH2 domain-containing tyrosine phosphatases, such as SHP-1 (Src homology domain 2-containing tyrosine phosphatase-1). Their subsequent phosphorylation deactivates tyrosine kinases, leading to inhibition of survival signaling (12). Inhibitory immune receptors mediate signaling pathways and intercellular interactions associated with activation and survival (11,13). Neutrophils express a variety of ITIM-containing immune inhibitory receptors that include platelet endothelial cell adhesion molecule-1 (PECAM-1), LAIR-1 (Leukocyte-associated Ig-like receptor-1), CLECSF6 (c-type lectin superfamily 6), SIRP-α (Signal Regulatory Protein-α), and members of the Siglec (sialic-acid immunoglobulin-like lectins) family (13–15).
Siglecs are type I membrane proteins characterized by an amino-terminal V-set immunoglobulin domain that binds to sialic acid residues, followed by a variable number of C2-set immunoglobulin-like domains [reviewed in (13–15)]. Siglecs are variably expressed in hematopoietic cells except for Siglec-4, which is found primarily on certain nerve cells. A subgroup of Siglecs share significant homology with CD33 and contain one or more ITIM domains, including Siglecs-5 and -9 expressed on neutrophils (16–18). Ligation of Siglec-9 induced apoptosis in adult neutrophils in a caspase-dependent manner; in contrast, its activation under inflammatory conditions resulted in a caspase-independent autophagic type of cell death (18). These disparate actions implicate a unique role for Siglec-9 in modulating cell survival under inflammatory and basal conditions. A recent study showed that Siglec-9 interacted with phosphorylated SHP-1 in monocytes and natural killer cells (19), although this remains to be confirmed in neutrophils. Siglec-9 and SHP-1 interactions might also be age-dependent, as evidenced by increased SHP-1 phosphatase activity in neutrophils of elderly subjects (20). We designed studies to test our hypothesis that expression of Siglec-9 and SHP-1 is age specific, a possibility with implications for inflammatory function in neonates.
METHODS
Neutrophil isolation and culture.
Heparinized blood samples from healthy adult donors and umbilical venous cord blood from freshly delivered term placentas were processed in parallel. Neutrophils were isolated by dextran-sedimentation and density centrifugation, as described (4). For cultures, neutrophils were suspended in RPMI 1640/2% FCS and incubated at 37°C, 5% CO2, for up to 24 h, in the presence or absence of specific stimuli. Samples were collected with informed consent according to guidelines of the Institutional Review Board for Human Studies at Saint Louis University.
Reagents.
RPMI 1640 and FBS were purchased from GIBCO-BRL (Invitrogen Corporation, Carlsbad, CA) and Hyclone, Inc. (Logan, UT), respectively. Anti-Siglec-9 polyclonal Ab, anti-SHP-1 Ab, and all secondary Abs were purchased from Santa Cruz Biotechnology, Inc. (Santa Cruz, CA). Phosphotyrosine Ab (clone 4G10) was purchased from Millipore Corporation (Billerica, MA), and Ab against phosphoserine472/473 PKB/Akt, Bad, and phosphoserine136 (Bad) were purchased from Cell Signaling Technology (Beverly, MA). Antibodies for flow cytometry and anti-SHP-1 MAb were purchased from BD Biosciences (San Jose, CA). Inflammatory stimulants, rhGM-CSF (recombinant human granulocyte-macrophage colony-stimulating factor), and fMLP (formyl-methionine-leucine-phenylalanine) were purchased from R&D Systems (Minneapolis, MN) or Sigma Chemical Co.-Aldrich, Inc. (St. Louis, MO).
Flow cytometric analysis of surface Siglec-9 expression.
Neutrophils (106) were stained with saturating amounts of anti-Siglec-9 MAb (clone E10–286) conjugated with FITC or isotype control IgG, washed in PBS and erythrocytes lysed (BD FACS lysing solution) before fixation (1% paraformaldehyde). Neutrophils were identified by specific scatter characteristics, and mean fluorescence intensity (MFI) was determined in 5000–10,000 gated events using a multi-color flow cytometer (BD FACS). To determine surface Siglec-9 levels on monocytes, whole blood was incubated with anti-Siglec-9-FITC MAb and anti-CD14-PE MAb, and MFI was determined in the double-positive populations (21).
Stimulation studies.
To assess surface Siglec-9 expression as a function of inflammatory stimulation, paired samples of neonatal and adult neutrophils were incubated with fMLP (100 nM) or rhGM-CSF (100 ng/mL) for up to 120 min. Time-specific aliquots of treated neutrophils were stained with anti-Siglec-9-FITC MAb and analyzed by flow cytometry, or prepared for immunoprecipitation or Western blot studies, as described later.
Immunoprecipitation studies.
Neutrophils were lysed [lysis buffer: 50 mM Tris pH 8.0, 0.5% NP-40, 150 mM NaCl, 1 mM each of EDTA, PMSF, Na3VO4, NaF; and 1 μg/mL each of aprotinin, leupeptin, pepstatin] and centrifuged (14,000 rpm × 10 min). Cell-free supernatants incubated overnight with anti-phosphotyrosine Ab (4G10) or anti-SHP-1at 4°C were then incubated with protein G beads followed by washes in cell lysis buffer. Proteins were eluted with 2× Laemmli sample buffer, separated on a 5–12% NuPAGE Bis-Tris gradient gel (Invitrogen Corp., Carlsbad, CA), and transferred to PVDF membrane (Immobilon-P, Millipore, Bedford, MA). Blots probed overnight with primary Ab (anti-Siglec-9 or anti-SHP-1) in blocking buffer were then incubated with horseradish peroxidase (HRP)-linked secondary Ab. Protein bands were visualized by chemiluminescence (ECL, Roche, Indianapolis, IN).
Western blots.
Neutrophils (5 × 106) stimulated with rhGM-CSF (25 ng/mL) were lysed in RIPA buffer containing a protease inhibitor cocktail (both, Sigma Chemical Co.-Aldrich). For phosphoprotein expression, the lysis buffer was supplemented with 2 mM each of Na orthovanadate and Na fluoride. Equivalent protein amounts of lysates in 2× Laemmli buffer were separated by SDS-PAGE and analyzed by Western blot using primary Ab and HRP-conjugated secondary Ab. Protein sample loading was normalized by reprobing blots with anti-β-actin Ab. Protein bands were visualized by chemiluminescence (ECL), and band intensities relative to β-actin expression, or the ratio of phosphorylated to total cognate protein, quantified by densitometric analysis.
Statistical analysis.
Data, expressed as mean ± SD, were analyzed by t test or by one-way ANOVA, as appropriate, using a statistical software program (SigmaStat for Windows, SPSS, Inc.). A p value <0.05 was considered significant.
RESULTS
Differential cellular Siglec-9 expression and phosphorylation status in neonatal and adult neutrophils.
Using Western blots in paired studies of neutrophil lysates, we determined that whole cell expression of Siglec-9 protein (Fig. 1A and B) was lower in neonatal neutrophils (Siglec-9/actin ratio: neonates, 0.45 ± 0.48 versus adults, 1.28 ± 0.75; p < 0.05) under basal conditions. To determine whether levels of phosphorylated Siglec-9, the active form associated with inhibitory activity, might also differ between the groups under inflammatory conditions, we assessed expression of tyrosine-phosphorylated Siglec-9 in lysates of neutrophils harvested under basal and stimulated conditions. Neutrophils at baseline (0 h) or after treatment with rhGM-CSF were lysed and then immunoprecipitated with anti-phosphotyrosine Ab. As shown (Fig. 2), the tyrosine-phosphorylated form of Siglec-9 was prevalent under basal conditions in lysates of neonatal but not adult neutrophils. In contrast, treatment with GM-CSF induced a time-dependent increase in phosphorylated Siglec-9 levels in adult neutrophils whereas phosphorylation levels temporally decreased in neonatal neutrophils. These results indicate that adult and neonatal neutrophils differ in Siglec-9 expression and basal phosphorylation state and display a reciprocal regulatory response to the inflammatory cytokine GM-CSF.
Lower whole cell expression of Siglec-9 in neonatal PMN. Siglec-9 and β-actin were detected by Western blot in lysates of adult (AD) and neonatal (CB) neutrophils. (A) The blot shown is representative of five separate paired experiments. (B) Relative densitometric units of Siglec-9 were normalized to β-actin expression, as shown in A. Solid black bar, AD PMN; hatched bar, CB PMN. *p < 0.05, AD vs CB PMN.
GM-CSF-induced phosphorylation of Siglec-9 in adult and neonatal PMN. In paired studies, adult (AD) and neonatal (CB) PMN were treated with GM-CSF (25 ng/mL) for the times shown. Lysates were immunoprecipitated with anti-phosphotyrosine Ab and then subjected to Western blotting using anti-Siglec-9 Ab. Blot shown is representative of three separate, paired experiments.
Surface expression of Siglec-9 in neonatal and adult myeloid cells.
Using flow cytometric analysis, we determined that the majority of neutrophils expressed surface Siglec-9 (neutrophils: neonates, 92 ± 3%; adults, 89 ± 2%; n = 5; p = 0.18), and surface Siglec-9 levels were greater on neonatal neutrophils (mean fluorescence intensity, MFI: neonates, 180 ± 164 versus adults, 88 ± 56; X ± SD, p < 0.01) (Fig. 3). Similar to our observations in neutrophils, most CD 14-positive monocytes expressed surface Siglec-9 (neonates, 79 ± 6% versus adults, 82 ± 6%, p = NS), and surface levels were higher on neonatal monocytes (MFI, 35 ± 12 versus adult monocytes, 18.2 ± 6.2, p < 0.05) (Fig. 3). Neutrophils had higher surface Siglec-9 levels compared with monocytes in each group (neonates, p < 0.01; adults, p < 0.05). Treatment of neutrophils with rhGM-CSF (100 ng/mL) or fMLP (100 nM) yielded no changes in surface Siglec-9 levels relative to baseline levels (data not shown), similar to observations made by von Gunten et al. (18).
Higher surface expression of Siglec-9 on neonatal PMN and monocytes. In paired studies, surface expression of Siglec-9 on adult (AD) and neonatal (CB) PMN (solid black bars) and monocytes (hatched bars) was determined by flow cytometric analysis of MAb-stained cells. Results represent the mean fluorescence intensity (MFI) from experiments of duplicate samples. *p < 0.01, CB vs AD neutrophils (n = 10); **p < 0.05, CB vs AD monocytes (n = 5).
Total SHP-1 expression and phosphorylation in neonatal and adult neutrophils.
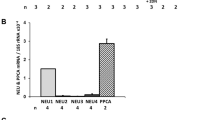
We next sought to determine whether proteins known to contribute to Siglec-9-mediated signaling might also be differentially expressed in neonatal and adult neutrophils. We focused the present studies on the expression of the inhibitory phosphatase, SHP-1, based on its greater interaction with ITIM in neutrophils (22). As shown (Fig. 4A and B), we observed lower basal expression of SHP-1 in lysates of neonatal (0.45 ± 0.08) versus adult (0.72 ± 0.16; p < 0.05) neutrophils. To compare phosphorylated SHP-1 levels, expression of the tyrosine-phosphorylated form of SHP-1 was examined in neutrophils under basal and stimulated conditions. Lysates from neutrophils at rest or after treatment with rhGM-CSF were prepared and immunoprecipitated with anti-phosphotyrosine Ab. As shown in Figure 5A, SHP-1 existed in its tyrosine-phosphorylated form in both adult and neonatal neutrophils at baseline. However, in contrast to our observations of Siglec-9 phosphorylation patterns, the phosphorylated status of SHP-1 did not change appreciably after treatment with GM-CSF.
Lower expression of SHP-1 in neonatal PMN. (A) SHP-1 protein was detected in adult (AD) and neonatal (CB) PMN lysates by Western blot, and expression was normalized to β-actin. (B) Graph represents mean densitometric SHP-1/actin ratios in three separate, paired experiments in *p < 0.05, CB vs AD PMN.
SHP-1 phosphorylation patterns and interaction with Siglec-9 in adult and neonatal PMN. (A) After stimulation with GM-CSF (25 ng/mL) for the times shown, adult (AD) and neonatal (CB) PMN lysates were immunoprecipitated with an anti-phosphotyrosine Ab and then immunoblotted with anti-SHP-1 Ab. The blot shown is representative of three separate, paired studies. (B) In immunoprecipitation studies, SHP-1 was immunoprecipitated from neutrophil lysates with an anti-SHP-1 Ab and then subjected to Western blotting using anti-Siglec-9 Ab. The blot shown is representative of three separate, paired experiments.
Siglec-9 interacts with SHP-1 in neutrophils.
We next sought to determine whether Siglec-9 physically interacts with SHP-1 in neutrophils as has been described in other immune cells, using immunoprecipitation techniques (23). Under basal conditions, neutrophil lysates were immunoprecipitated with anti-SHP-1 Ab or, conversely, with anti-Siglec-9 Ab. Immunoblots were performed on immunoprecipitated proteins using anti-Siglec-9 Ab or anti-SHP-1 Ab, respectively, as described in Methods section. As shown in Figure 5B, we observed a clear association between Siglec-9 and SHP-1 in both neonatal and adult neutrophils. These results are supportive of an interactive role between Siglec-9 and SHP-1 in neutrophils, as has been previously suggested (18).
Differential GM-CSF-induced phosphorylation of PKB/Akt and Bad in neonatal neutrophils.
We next sought to determine whether differences in the expression of Siglec-9 and SHP-1 under inflammatory conditions might be linked to survival pathways in neutrophils. The serine/threonine kinase Akt is at the hub of survival signaling, and because SHP-1 has been shown to modulate PKB/Akt activity, we compared the activation status of PKB/Akt in neonatal and adult neutrophils (23,24). We observed that although basal phosphorylation levels of PKB/Akt at serine 473 (AktS473) were similar between the groups, GM-CSF treatment induced a more robust phosphorylation response in neonatal neutrophils (Fig. 6B). Because PKB/Akt promotes survival signaling by phosphorylating the proapoptotic protein, Bad, we examined the phosphorylation status of Bad on serine 136 on the same blots (25). GM-CSF treatment induced a latent phosphorylation of Bad between 30 and 60 min in neonatal neutrophils (Fig. 6A). In contrast, adult neutrophils exhibited phosphorylation of Bad that peaked at 15 min followed by its decline. Expression of the unphosphorylated, proapoptotic form of Bad temporally decreased in neonatal neutrophils while Bad expression continued to increase in adult neutrophils, a profile consistent with progressive apoptosis. The ratio of phosphorylated Bad/total Bad levels progressively increased in neonatal neutrophils during GM-CSF treatment, whereas adult neutrophils exhibited a temporal decrease (Fig. 6C). Collectively, these data suggest a greater activation of survival mechanisms in neonatal neutrophils in response to GM-CSF.
Differential phosphorylation of PKB/Akt and Bad in neonatal and adult PMN. In the same blots of GM-CSF-treated PMN (Fig. 5), Akt and Bad expression was analyzed by Western blot using Ab against Akt or phospho-AktSer473, or anti-Bad and anti-phospho-BadSer136 Ab. (A) Blot shown is representative of 2–4 separate, paired experiments. (B) Levels of phosphorylated protein were normalized to total cognate protein, and the mean densitometric ratios of phospho-Akt/total Akt are shown on the graph; AD PMN (solid black bars) vs CB PMN (hatched bars). *p < 0.05; CB PMN vs time zero (n = 4 paired studies). (C) Graph showing mean densitometric ratios of phospho-Bad/total Bad in blots of AD PMN (solid line) vs CB PMN (broken line); (n = 2).
DISCUSSION
We and others previously reported a prolonged survival in neonatal neutrophils both constitutively and under inflammatory conditions, although the mechanisms have been incompletely defined (4,10). The present studies were designed to test our hypothesis that age-specific differences exist in the neutrophil expression of the proapoptotic proteins, Siglec-9 and SHP-1, and their activation in response to inflammatory stimuli. We present data showing that the ITIM-containing death receptor protein, Siglec-9, was less abundant in neonatal neutrophils relative to adult neutrophils, as was a down-stream signaling protein, SHP-1, an inhibitory tyrosine phosphatase with proapoptotic function. Neonatal neutrophils exhibited basal expression of the active (tyrosine-phosphorylated) form of Siglec-9, and phosphorylation levels temporally decreased during stimulation with GM-CSF. In contrast, adult neutrophils exhibited minimal basal Siglec-9 phosphorylation, which dramatically increased with GM-CSF treatment, an observation consistent with the Siglec-mediated cell death in neutrophils reported by von Gunten et al. (18).
In this study, we also confirmed a physical relationship between Siglec-9 and SHP-1 as was previously suggested in neutrophils and reported in other types of immune cells (18,19). Phosphorylation of the ITIM domain of Siglec-9 can recruit and activate SHP-1 (19). Thus, the progressive phosphorylation of Siglec-9 in GM-CSF-treated adult neutrophils first observed by von Gunten et al. (18) and confirmed in our present studies could be consistent with increasing recruitment of SHP-1. Previous data suggest that Siglec-9/SHP-1 interactions are an operative mechanism in neutrophil cell death (18). In contrast, we observed alterations of Siglec-9 and SHP-1 expression levels in neonatal neutrophils. These observations suggest a possible difference in the contributions of these proteins to postinflammatory neutrophil clearance mechanisms in neonates.
A potential limitation of proapoptotic Siglec-9/SHP-1 interactions could contribute to the greater survival of neonatal neutrophils. In support of this premise, we observed a prominent basal phosphorylation of Siglec-9 in neonatal neutrophils not seen in adult neutrophils (Fig. 2). This finding was unexpected, because the phosphorylated (active) form of Siglec-9 has been linked with cell death, and neonatal neutrophils exhibit a prolonged survival (4,10,18). The striking inverse pattern of Siglec-9 phosphorylation that we observed under inflammatory conditions (Fig. 2), associated with progressive dephophorylation of this ITIM-containing protein in neonatal neutrophils, provides a compelling mechanistic link to enhanced neonatal neutrophil survival.
Neutrophil survival is regulated by finely balanced interactions between proapoptotic and survival signals, and phosphatases play a critical role in these processes (22,26,27). Alteration of SHP-1-mediated signal deregulation is an attractive explanation for the greater survival of neonatal neutrophils, because SHP-1 inhibits kinases involved in cell survival processes, including Lyn and PKB/Akt (12,22,27–29). Several lines of evidence are consistent with altered SHP-1 function in neonatal neutrophils. SHP-1 de-phosphorylates Lyn, and neonatal neutrophils were shown to have constitutively phosphorylated levels of Lyn, which infers diminished SHP-1 functionality (22,29). In addition, low neutrophil SHP-1 activity in the presence of increased Lyn expression during sepsis inhibited the proapoptotic activity of caspase-8 (30). The diminished caspase-8 activity that we previously reported in neonatal neutrophils is therefore also consistent with decreased SHP-1 activity in these cells (9). Thus, diminished SHP-1 activity in neonatal neutrophils could be insufficient to block survival signaling, a possibility consistent with the protracted survival pattern of Akt and Bad phosphorylation that we observed in neonatal neutrophils, in contrast to the transient survival response in adult neutrophils. In addition to its effect on survival, the enhanced neutrophil infiltration of tissues in SHP-1 −/− mice also suggests a link between diminished SHP-1 function in neonatal neutrophils and a potential contribution to chronic inflammation (8,12).
Alternatively, the progressive dephosphorylation of Siglec-9 in inflammatory neonatal neutrophils might be related to altered functional interactions among Siglec-9, SHP-1 and Src kinases. This possibility is not without precedence, because regulation of signaling through the lipid kinase, phosphatidylinositol 3-kinase, was shown to be mediated through its engagement of SHP-1 and a constitutively activated form of the Src kinase, Lck, in T lymphocytes (23). Bortolussi and coworkers (29) observed constitutive phosphorylation of another Src kinase, Lyn, which was trapped in the membrane fraction in neonatal neutrophils. Neutrophils of elderly subjects also exhibited baseline phosphorylation of Lyn, and altered recruitment of Lyn to lipid rafts during GM-CSF stimulation was associated with impaired SHP-1 function (20). Furthermore, regulation of the proapoptotic activity of caspase-8 was shown to be dependent on SHP-1 and phosphorylated Lyn levels (30). On the basis of the unique pattern of Siglec-9 phosphorylation that we observed in neonatal neutrophils (Fig. 2), we postulate that membrane recruitment of SHP-1 could lead to latent complex formation with Siglec-9 (perhaps through constitutively phosphorylated Lyn) in neonatal neutrophils at rest, perhaps entrapped in the membrane fraction or lipid rafts. Conversely, under inflammatory conditions, SHP-1-mediated phosphatase activity could lead to the dephosphorylation (and deactivation) of Siglec-9 and the promotion of survival mechanisms. This scenario is supported by the sustained signaling profile of Akt and Bad that we also observed in neonatal neutrophils under similar inflammatory conditions (Fig. 6). In contrast, adult neutrophils seem to be primed to engage in proapoptotic cascades during inflammation, as evidenced by the rapid phosphorylation of Siglec-9 previously reported by von Gunten et al. (18) and which we also observed in association with transient Akt and Bad survival phosphorylation patterns (Fig. 6). However, further studies will be needed to more closely examine and establish these possible mechanisms.
The comparatively lower surface levels of Siglec-9 on adult myeloid cells could be related to the formation of inactive cis complexes between Siglecs and adjacent surface sialic acids, effectively “masking” binding sites (13,31). However, this possibility is unlikely based on the reported lack of an effect of sialidase treatment on surface Siglec-9 levels (18). Alternatively, the incongruity between surface and cellular levels might reflect an age-related differential subcellular localization and membrane trapping of Siglec-9, as was reported for Lyn (20,29). These potential explanations merit further investigation.
In summary, our observations provide evidence of disparate roles for Siglec-9 and SHP-1 in the inflammatory function of neonatal and adult neutrophils and offer new potential explanations for the preferential survival of neonatal neutrophils. Although adult neutrophils are programmed toward a more rapid cell death, they are generally more functionally effective than neonatal neutrophils (32). Prolonged functional survival of neutrophils in the presence of restricted reserves may reflect a teleological mechanism to protect the developing human against infection. However, this potential benefit is a two-edged sword, because promotion of survival pathways is also linked to cellular activation and chronic inflammation. Continued delineation of the complex processes contributing to altered neutrophil survival will be critical to the development of novel, targeted approaches to inflammatory disorders in neonates.
Abbreviations
- fMLP:
-
formyl-methionine-leucine-phenylalanine
- ITIM:
-
immunoreceptor tyrosine-based inhibitory motif
- MFI:
-
mean fluorescence intensity
- rhGM-CSF:
-
recombinant human granulocyte-macrophage colony-stimulating factor
- SHP-1:
-
Src homology domain 2-containing tyrosine phosphatase-1
- Siglec:
-
Sialic acid-binding immunoglobulin-like lectin
References
Dransfield I, Rossi AG, Brown SB, Hart SP 2005 Neutrophils: dead or effete? Cell surface phenotype and implications for phagocytic clearance. Cell Death Differ 12: 1363–1367
Luo HR, Loison F 2008 Constitutive neutrophil apoptosis: mechanisms and regulation. Am J Hematol 83: 288–295
Haslett C 1997 Granulocyte apoptosis and inflammatory disease. Br Med Bull 53: 669–683
Allgaier B, Shi M, Luo D, Koenig JM 1998 Spontaneous and Fas-mediated apoptosis are diminished in umbilical cord blood neutrophils compared with adult neutrophils. J Leukoc Biol 64: 331–336
Koenig JM, Stegner JJ, Schmeck AC, Saxonhouse MA, Kenigsberg LE 2005 Neonatal neutrophils with prolonged survival exhibit enhanced inflammatory and cytotoxic responsiveness. Pediatr Res 57: 424–429
Kotecha S, Mildner RJ, Prince LR, Vyas JR, Currie AE, Lawson RA, Whyte MK 2003 The role of neutrophil apoptosis in the resolution of acute lung injury in newborn infants. Thorax 58: 961–967
Oei J, Lui K, Wang H, Henry R 2003 Decreased neutrophil apoptosis in tracheal fluids of preterm infants at risk of chronic lung disease. Arch Dis Child Fetal Neonatal Ed 88: F245–F249
Speer CP 2006 Inflammation and bronchopulmonary dysplasia: a continuing story. Semin Fetal Neonatal Med 11: 354–362
Luo D, Schowengerdt KO Jr, Stegner JJ, May WS Jr, Koenig JM 2003 Decreased functional caspase-3 expression in umbilical cord blood neutrophils is linked to delayed apoptosis. Pediatr Res 53: 859–864
Hanna N, Vasquez P, Pham P, Heck DE, Laskin JD, Laskin DL, Weinberger B 2005 Mechanisms underlying reduced apoptosis in neonatal neutrophils. Pediatr Res 57: 56–62
Ravetch JV, Lanier LL 2000 Immune inhibitory receptors. Science 290: 84–89
Yousefi S, Simon HU 2003 SHP-1: a regulator of neutrophil apoptosis. Semin Immunol 15: 195–199
Crocker PR, Paulson JC, Varki A 2007 Siglecs and their roles in the immune system. Nat Rev Immunol 7: 255–266
Crocker PR, Varki A 2001 Siglecs, sialic acids, and innate immunity. Trends Immunol 22: 337–342
Varki A, Angata T 2006 Siglecs—the major subfamily of I-type lectins. Glycobiology 16: 1R–27R
Zhang JQ, Nicoll G, Jones C, Crocker PR 2000 Siglec-9, a novel sialic acid binding member of the immunoglobulin superfamily expressed broadly on human blood leukocytes. J Biol Chem 275: 22121–22126
Erickson-Miller CL, Freeman SD, Hopson CB, D'Alessio KJ, Fischer EI, Kikly KK, Abrahamson JA, Holmes SD, King AG 2003 Characterization of Siglec-5 (CD170) expression and functional activity of anti-Siglec-5 antibodies on human phagocytes. Exp Hematol 31: 382–388
von Gunten S, Yousefi S, Seitz M, Jakob SM, Schaffner T, Seger R, Takala J, Villiger PM, Simon HU 2005 Siglec-9 transduces apoptotic and nonapoptotic death signals into neutrophils depending on the proinflammatory cytokine environment. Blood 106: 1423–1431
Avril T, Floyd H, Lopez F, Vivier E, Crocker PR 2004 The membrane-proximal immunoreceptor tyrosine-based inhibitory motif is critical for the inhibitory signaling mediated by Siglecs-7 and -9, CD33-related Siglecs expressed on human monocytes and NK cells. J Immunol 173: 6841–6849
Fortin CF, Larbi A, Lesur O, Douziech N, Fulop T Jr 2006 Impairment of SHP-1 down-regulation in the lipid rafts of human neutrophils under GM-CSF stimulation contributes to their age-related, altered functions. J Leukoc Biol 79: 1061–1072
Kirchhofer D, Riederer MA, Baumgartner HR 1997 Specific accumulation of circulating monocytes and polymorphonuclear leukocytes on platelet thrombi in a vascular injury model. Blood 89: 1270–1278
Daigle I, Yousefi S, Colonna M, Green DR, Simon HU 2002 Death receptors bind SHP-1 and block cytokine-induced anti-apoptotic signaling in neutrophils. Nat Med 8: 61–67
Cuevas B, Lu Y, Watt S, Kumar R, Zhang J, Siminovitch KA, Mills GB 1999 SHP-1 regulates Lck-induced phosphatidylinositol 3-kinase phosphorylation and activity. J Biol Chem 274: 27583–27589
Zhu D, Hattori H, Jo H, Jia Y, Subramanian KK, Loison F, You J, Le Y, Honczarenko M, Silberstein L, Luo HR 2006 Deactivation of phosphatidylinositol 3,4,5-trisphosphate/Akt signaling mediates neutrophil spontaneous death. Proc Natl Acad Sci USA 103: 14836–14841
Datta SR, Dudek H, Tao X, Masters S, Fu H, Gotoh Y, Greenberg ME 1997 Akt phosphorylation of BAD couples survival signals to the cell-intrinsic death machinery. Cell 91: 231–241
Brumell JH, Chan CK, Butler J, Borregaard N, Siminovitch KA, Grinstein S, Downey GP 1997 Regulation of Src homology 2-containing tyrosine phosphatase 1 during activation of human neutrophils. Role of protein kinase C. J Biol Chem 272: 875–882
Klein JB, Rane MJ, Scherzer JA, Coxon PY, Kettritz R, Mathiesen JM, Buridi A, McLeish KR 2000 Granulocyte-macrophage colony-stimulating factor delays neutrophil constitutive apoptosis through phosphoinositide 3-kinase and extracellular signal-regulated kinase pathways. J Immunol 164: 4286–4291
Nishizumi H, Horikawa K, Mlinaric-Rascan I, Yamamoto T 1998 A double-edged kinase Lyn: a positive and negative regulator for antigen receptor-mediated signals. J Exp Med 187: 1343–1348
Yan SR, Byers DM, Bortolussi R 2004 Role of protein tyrosine kinase p53/56lyn in diminished lipopolysaccharide priming of formylmethionylleucyl- phenylalanine-induced superoxide production in human newborn neutrophils. Infect Immun 72: 6455–6462
Jia SH, Parodo J, Kapus A, Rotstein OD, Marshall JC 2008 Dynamic regulation of neutrophil survival through tyrosine phosphorylation or dephosphorylation of caspase-8. J Biol Chem 283: 5402–5413
Freeman SD, Kelm S, Barber EK, Crocker PR 1995 Characterization of CD33 as a new member of the sialoadhesin family of cellular interaction molecules. Blood 85: 2005–2012
Koenig JM, Yoder MC 2004 Neonatal neutrophils: the good, the bad, and the ugly. Clin Perinatol 31: 39–51
Acknowledgements
We thank the obstetricians and the Labor & Delivery staff at SSM St. Mary's Health Center and particularly the adult blood donors for helping us obtain samples critical for our studies.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by Grant HD47401 from NIH/NICHD (to J.M.K), the Fleur-de-Lis Foundation (to R.R.), and the Pediatric Research Institute, Department of Pediatrics, Saint Louis University (to J.M.K.).
Rights and permissions
About this article
Cite this article
Rashmi, R., Bode, B., Panesar, N. et al. Siglec-9 and SHP-1 Are Differentially Expressed in Neonatal and Adult Neutrophils. Pediatr Res 66, 266–271 (2009). https://doi.org/10.1203/PDR.0b013e3181b1bc19
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3181b1bc19
This article is cited by
-
Neonatal neutrophils stimulated by group B Streptococcus induce a proinflammatory T-helper cell bias
Pediatric Research (2018)
-
Cell Death Modulation by Intravenous Immunoglobulin
Journal of Clinical Immunology (2010)