Abstract
B cell dysfunction is a well-studied complication of HIV infection in adults. Data on B cell differentiation in normal and HIV-infected children are lacking. We show the distribution of B cell subsets and immunoglobulin levels in HIV-infected children compared with controls. Furthermore, we observe the long-term B cell reconstitution of vaccine-specific immunity after antiretroviral therapy (ART). Phenotype of B cells (naive, non-switched memory, switched memory) was analyzed in 48 infected children and 62 controls. In nine HIV-infected children, functional reconstitution was quantified by tetanus-specific antibodies and by performing a lymphocyte transformation test (LTT) in a longitudinal approach. Switched memory B cells are significantly reduced in HIV-infected children. Vaccine-specific antibodies and response to LTT increase after initiation of ART. Our data indicate a significant dysfunction in the B cell system, despite effective ART. Partial reconstitution of humoral immunity may have therapeutic implications in a subset of HIV-infected children.
Similar content being viewed by others
Main
HIV-1 infection leads to a profound impairment of both of the cellular and humoral arm of the immune system. Several abnormalities have been reported in the B cell compartment. Hyperactivation of B cells is thought to result in increased levels of serum immunoglobulins and spontaneous in vitro antibody secretion in unstimulated lymphocyte cultures (1,2). Both polyclonal and HIV-specific antibodies are observed (3). Increased B cell activation markers have been seen; the imbalance of B cell homeostasis is associated with an increased rate of EBV-associated B cell lymphoma (4,5). Further dysfunction results from an impaired memory B cell function. A decrease of memory B cells has been reported in adults (6,7), as well as an altered vaccine response with recall antigen and stimulation with mitogens (8,9). In children, few studies have been made in the B cell compartment. Although they are not yet fully matured in children, B cells are already subject to HIV-induced hyperactivation. Hypergammaglobulinemia is seen in children as well (10). Some groups observe a reduced total B cell count in HIV-infected children (11,12), although these studies were conducted in the pre-antiretroviral therapy (ART) era. The present study compares for the first time HIV-infected with uninfected children regarding detailed B cell differentiation. Further, we investigate the functional reconstitution of the B cell compartment after ART in HIV-infected children regarding the production of vaccine-specific tetanus toxoid antibodies.
METHODS
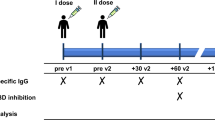
A total of 48 HIV-infected children (9.36 ± 4.15 y), who were treated at the HIV outpatient clinics of the Department of Pediatric Oncology, Hematology and Clinical Immunology, Heinrich-Heine-University Düsseldorf between 1995 and 2005, were enrolled into the patient cohort for a cross-sectional analysis of B cell differentiation. All patients were vertically infected. Children were excluded if data on complete B and T cell differentiation and viral load were not available in at least two different time points. For clinical staging we used the centers for disease control (CDC) classification (13). In a subgroup of nine infected children, vaccine responses were analyzed for functional B cell reconstitution after ART. Children were included in this cohort if vaccination with diphtheria and tetanus was done before ART and data on lymphocyte transformation test (LTT) and levels of tetanus-specific antibodies were available before and after the initiation of ART.
A total of 62 children (6.03 ± 3.95 y), who underwent elective surgery at the Department of Otolaryngology/Department of Pediatric Surgery at our university, and children in whom various immunologic and rheumatic disorders were ruled out at our department, were taken as controls. Informed consent was obtained from all parents. The Heinrich-Heine University Institutional Review Board approved the study.
Measurement of B cell subpopulations.
Within 6 h of whole blood sampling, we performed a three-color cytometry (10,000 Events; FACSCalibur, BD) applying the following Fluorescein-Isothiocyanat (FITC), phycoerythrin (PE), and peridinin chlorophyll protein (PerCP) conjugated anti-human mAbs: CD8−FITC, CD4−PE, CD3−PerCP, IgD−FITC, CD20−PerCP (Becton Dickinson, Bridgeport, NJ) and CD27−PE (Immunotech, Marseille Cedex, France). It was gated on B lymphocytes stained with anti-CD20−PerCP. CD27 and IgD expression were analyzed among the gated CD20+ population (10,000 Events). IgD+CD27− were classified as naive, IgD+CD27+ as non-switched memory, and IgD−CD27+ as switched memory B cells. A representative facial action coding system (FACS) analysis of B cell differentiation is supplemented (Fig. S1, Supplemental Digital Content 1, http://links.lww.com/PDR/A44).
Primary immunization schedule.
HIV-infected children were immunized according to the German vaccination schedule (14), which includes diphtheria, tetanus, and pertussis vaccine administered at 2, 3, 4, and 11-14 mo of age, with two booster doses at 5-6 y of age and every 10 y afterward.
Lymphocyte transformation test.
In a subgroup of nine HIV-infected patients, we investigated functional reconstitution after ART. We focused on the mitogen response to phytohemagglutinin (PHA), anti-CD3 MAb (OKT3), pokeweed mitogen (PWM), Staphylococcus A Cowan I (SAC) and assessed the antigen-specific cellular response to stimulation with tetanus toxoid. LTT was performed as published (15). Cells were incubated in suspension with mitogens and tetanus toxoid for 6 d at 37°C and labeled with 3H-thymidine 18 h before the end of the culture period. The incorporation rate of thymidine was measured in counts per minute (cpm) in a Packard Tri-Carb Liquid Scintillation Counter. Proliferation was expressed as a stimulation index (SI) = mean counts of stimulated cultures/mean counts of medium control. Patients were observed at three stages—time point (tp1) children were drug naive when they obtained complete immunization against tetanus. Before initiation of ART (12.5 ± 3 mo after immunization) mitogens and tetanus toxoid-specific LTT were done and tetanus-specific antibodies were determined; (tp2) within 36 ± 20 mo after initiation of ART another series of LTT with mitogens/tetanus antibody detection was done. LTT with tetanus toxoid was available in three patients; (tp3) within 84 ± 15 mo after initiation of ART, children were boostered with tetanus vaccine and a third LTT series (tetanus toxoid and mitogens) with detection of tetanus-specific antibodies was performed.
Measurement of serum immunoglobulins, tetanus-specific antibodies and viral load.
Plasma levels of IgG, IgA, and IgM were determined by immunonephelometry and standardized according to reference data (16). Five children were excluded because of missing immunoglobulin data. Tetanus antibody levels were detected by ELISA (Progen Biotechnik, Heidelberg, Germany). Viral load was determined with quantitative PCR.
Statistical analysis.
Absolute CD4 T cell numbers were related to age and age-related percentages (ARP) were calculated as published (17,18). Percentages of B cell subpopulations refer to all CD20 gated cells (= all B cells). Data in the text are presented as median and interquartile distance, data related to LTT and tetanus-specific antibodies are presented with mean values and SD. As the age of our cohorts differ significantly (p < 0.001) two approaches to compare B cell differentiation between HIV-infected children and controls were made (1) by matching 23 individuals from each group by age or (2) by stratifying them to age-related subgroups (2-5 y; 6-10 y; 11-18 y).
There was no significant difference in viral load between the age-related subgroups (median viral load in all three groups: 102 ± 103; p1,2 p2,3 p1,3 >0.05). Age-adjusted values were calculated based on the controls. Further, we stratified patients to two subgroups regarding the viral load [<500 Eq/mL (n = 21) and >500 Eq/mL (n = 27)]. There was no significant difference in age between these two subgroups, but patient controls were significantly younger than both viral load stratified subgroups in HIV-infected children. Differences were analyzed by t test. p Values <0.05 were considered statistically significant. Correlation analysis between variables was performed by Microsoft Excel.
RESULTS
Memory B cells are decreased in HIV-infected children.
There is no significant difference between HIV patients and controls in absolute and relative B cell numbers (HIV 369 ± 202 cells/μL, controls 400 ± 363 cells/μL, p = 0.86; HIV 13 ± 8%, controls 16 ± 9%, p = 0.37). The percentages and absolute cell count of switched memory and non-switched memory B cells are significantly decreased (switched memory B cells: HIV 20 ± 31 cells/μL, controls 40 ± 28 cells/μL, p = 0.008; HIV 5 ± 7%, controls 11 ± 10%, p < 0.001). We found an increased frequency of circulating naive B cells in percentage (HIV 85 ± 13%, controls 73 ± 17%, p = 0.003), but not in absolute number (HIV 303 ± 185 cells/μL, controls 306 ± 290 cells/μL, p = 0.397). The increased percentage mainly represents the decrease in the other two populations (Fig. 1). In addition to age-matched individuals, we compared all patients by stratifying them to age-defined groups to study the ontogenetic influence. Total B cell numbers do not show a significant difference at all, whereas percentages of all B cell subsets and absolute numbers of switched memory B cells show significant changes (decreased switched and nonswitched memory B cells, increased naive B cells; Fig. 2 and Table 1).
The memory B cell depletion is correlated with viral load, but not with clinical stage or CD4 count.
HIV-infected children with a viral load >500 Eq/mL have significantly decreased B cell counts compared with controls (controls 557 ± 468 cells/μL, HIVhigh >500 Eq/mL 308 ± 179 cells/μL, pControls/HIVhigh = 0.002). Similarly, we observe significant changes in B cell subsets. Children with a viral load >500 Eq/mL have significantly decreased switched memory B cells compared with children with a low viral load (controls 42 ± 35 cells/μL, HIV <500 Eq/mL 23 ± 40 cells/μL, HIV >500 Eq/mL: 12 ± 9 cells/μL, pControls/HIVlow = 0.011, pHIVhigh/HIVlow = 0.012, pControls/HIVhigh <0.0001, see Fig. 3). Control patients were significantly younger than both subgroups stratified by viral load, but we observe higher switched memory B cells in our control patients compared with HIV-infected children. As switched memory B cells usually increase with age, the difference in age between the groups is, therefore, an unlikely explanation for the reduction of switched memory B cells. To investigate a clinical or immunologic association with B cell differentiation we applied CDC classification for clinical staging. No significant change is noticed between any of the clinical or immunologic categories. Age-related percentages of the CD4 cell count between HIV-infected children and patient controls significantly differ as expected (controls: 101 ± 39%; HIV: 84 ± 34%; p = 0.002). We correlated the ARP CD4 cell count with the switched memory and nonswitched memory cell count), as CD4 cells are necessary for early differentiation to memory B cells. Both controls and HIV-infected children do not show a strong correlation between switched memory B cells and age-related CD4 counts (Fig. 4; Figs. S2 and S3, Supplemental Digital Content 2, http://links.lww.com/PDR/45 and Supplemental Digital Content 3, http://links.lww.com/PDR/A46). Additionally, we compared switched memory B cells between patients with an ARP of CD4 cells >60 and <60%, which did not reveal a significant difference (Table 2).
Increased IgG levels are not correlated with the number of memory B cells.
Immunoglobulin levels were compared with established reference values. Regarding IgG all age-defined groups of HIV-infected children have higher serum levels: 2-5 y 1270 ± 755 mg/dL; 6-10 y 1390 ± 405 mg/dL; 11-18 y 1310 ± 375 mg/dL [Normal range: 2-5 y 350-1300 mg/dL; 6-10 y 600-1300 mg/dL; 11-18 y 700-1600 mg/dL], whereas other immunoglobulins (IgA, IgM) are within normal levels. Immunoglobulins are produced by plasma cells, which develop from activated naive B cells or reactivated switched memory B cells. We correlated immunoglobulin levels with switched, nonswitched memory B cells, and viral load. No correlation was found.
Cellular and humoral immunity to tetanus toxoid fully reconstituted after booster.
The overall response to stimulation with mitogens increased at an average of 3 y after initiation of ART, although results varied between individuals. At an average of 7 y, response to stimulation with PWM [tp1: (29 ± 37) × 103 cpm; tp2: (49 ± 39) × 103 cpm; tp3: (27 ± 16) × 103 cpm], PHA [tp1: (82 ± 60) × 103 cpm; tp2: (108 ± 53) × 103 cpm; tp3: (59 ± 31) × 103 cpm], and SAC [tp1: (3 ± 4) × 103 cpm; tp2: (7 ± 9) × 103 cpm; tp3: (7 ± 7) × 103 cpm; SI seen in Table 3] decreased slightly, whereas response on OKT3 stimulation increased [tp1: (41 ± 26) × 103 cpm; tp2: (46 ± 32) × 103 cpm; tp3: (60 ± 24) × 103 cpm] (Fig. 5).
Longitudinal changes in proliferation with LTT. Stimulation with (A) SAC, (B) OKT3 and with (C) tetanus toxoid, (D) CD4 numbers, expressed in ARP. Proliferation is expressed as a stimulation index (SI = mean counts of stimulated cultures/mean counts of medium control). Patient numbers: 1 (filled squares), 2 (filled circles), 3 (filled triangles), 4 (filled diamonds), 5 (filled stars), 6 (open squares), 7 (open circles), 8 (open triangles), 9 (open diamonds), mean value (open stars).
In terms of tetanus toxoid-specific recall antigen, there was no specific response before initiation of ART, despite a history of complete vaccination (Table 3). After initiation of ART and a tetanus booster vaccination, all seven patients gained tetanus toxoid-specific proliferation (mean tp3: (14 ± 10) × 103 cpm). To exclude that this was the result of a general immune reconstitution a LTT with tetanus toxoid was performed in three patients (Patient no. 1, 4, 5 in Table 3) after initiation of ART, but before giving tetanus booster vaccination (tp2). All three patients had significantly lower response on LTT with tetanus toxoid before booster, although CD4 cells had shown a recovery. After booster vaccination, LTT with tetanus toxoid in these patients showed a much improved proliferation (tp1: 0 cpm; tp2: (3 ± 5) × 103 cpm; tp3: (18 ± 11) × 103 cpm). A correlation of OKT3 response with CD4 cell recovery was not seen (Table S1, Supplemental Digital Content 4, http://links.lww.com/PDR/A47).
Antibody response to routine tetanus toxoid immunization was measured before initiation of ART (tp1). After initiation of ART (tp2), five of nine children already had increasing titers of antibodies without booster vaccine (p = 0.07; Table 3). Application of a booster regime (tp3) provided all nine children with a protective immunity to tetanus.
DISCUSSION
B cell dysfunction in HIV-infected children has not been well characterized. In our present study, we investigated B cell numbers, B cell differentiation, the lymphocytic proliferative capacity to respond to B cell mitogens, and the ability to mount an antigen-specific antibody response. The total B cell count declines physiologically in growing children. Kam et al. (19) observed in a Chinese pediatric population the rise of total B cell numbers and percentage in the first year, before declining afterward. We did not find a significant decrease of total B cell numbers in HIV-infected children, although in children with a high viral load a decrease in B cell numbers was observed. Studies conducted on children before the availability of ART showed a reduction of B cells. Shearer et al. (11) observed a decrease of the total B cell count in HIV-infected children >4 y. Other groups described a significant decrease in absolute numbers, while finding same percentages in patient and control cohorts (12,20).
Several mechanisms of B cell depletion in HIV are being discussed. First, the number of B cells might be reduced because of hyperactivation and differentiation to antibody-secreting plasma cells (2–4). Plasma cells lose B cell antigen CD20 and were not counted in our investigation (21,22). Second, direct infection of a B cell has been reported, which may lead to destruction of some B cells (23), but probably not to a degree that might lead to a significant numerical decrease. Finally, an increased homing of B lymphocytes to lymphatic tissue is discussed due to an increased expression of homing receptors on lymphocytes (24,25).
Among B cell subsets HIV-infected children show a significant loss of relative and absolute numbers of switched memory B cells. In adults, a loss of memory B cell function has been reported (6,7,26), but data in children have not been published yet. Insufficient differentiation of naive to memory B cells, terminal differentiation of memory B cells to plasma cells, and apoptosis of memory B cells have been discussed explaining memory B cell loss. CD4 T cell depletion could lead to a decreased rate of differentiation to memory B cells. Unlike in adult studies, we did not find a strong correlation between CD4 and switched memory B cells in HIV-infected children (27). There was no significant difference between patients with an ARP of CD4 cells <60% and patients with an ARP >60%. A decrease in memory B cells could be due to an increased terminal differentiation to plasma cells. An increased CD70 expression (CD27 ligand) on CD4 T cells has been associated with increased plasma cell numbers (28). In addition, plasmocytosis in bone marrow samples was observed in infected adults (26). For further evaluation, bone marrow and peripheral blood samples would need to be examined simultaneously. Data in children are missing as bone marrow aspirates are not done routinely in HIV-infected children. Hypergammaglobulinemia for IgG, IgA, IgM in HIV-infected children has been reported (10,11,29). In contrast, we only observed an increased IgG level in HIV-infected children compared with reference values.
Other studies hypothesized an increased apoptosis of memory B cells by showing an increased expression of Fas, as well Fas-Ligand on B cells suggesting an autocrine apoptosis induction as a cause for memory B cell reduction (6,30–32).
In our cross-sectional analysis, children with lower viral loads had higher numbers of memory B cells. In contrast, in studies in adults, authors observed only little or no difference at all This may reflect a certain vulnerability of the B cell compartment in children and the long-term consequences of this B cell depletion are presently unknown.
Studies by Moir and coworkers (33) discern the B cell subsets by investigating CD21, CD10, and CD27 expression. Immature/transitional B cells (CD10+/CD27−) are expanded in HIV viremic patients, especially in CD4-depleted patients (34). Regarding CD21 expression, CD27+ cells are defined in mature activated (CD21low) and resting memory cells (CD21high). The latter are supposed to represent the true memory B cell compartment (35). Recently, tissue-like memory B cells (CD20++,CD27−), which have lost CD27 as the classical memory marker, are meant to be expanded in viremic patients representing hyperactivated B cells (36). Some authors do not observe a restoration of memory B cells after initiation of ART (7); however, a recent study shows an increase of resting memory B cells after 12 mo of ART (37). Memory B cells are only partly recovered compared with healthy individuals, which is consistent with our data.
In our longitudinal studies investigating six randomly selected children (data not shown), we could not find an association between change of viral load and switched memory B cells. Patients with continuously high viral loads were having low memory B cell percentages throughout the observation period. In one patient, switched memory B cell percentages increased with increasing viral load. In two patients after changing the drug regime, the viral load was suppressed going along with falling switched memory B cell percentage. For a better interpretation, longitudinal studies have to be performed prospectively in a larger patient cohort with a uniform treatment regime and clinical status.
To assess memory function in more detail, we extended our investigation on the proliferation capability of lymphocytes. All children had tetanus-specific immunity at an average of 7 y after basic vaccination. Three patients, in whom tetanus toxoid-specific proliferation was measured before booster vaccine, regained specific proliferation indicating an immune reconstitution through effective ART without any booster. Zaccarelli-Filho et al. (38) also observed low levels of vaccine specific antibodies in HIV-infected children, whereas other authors also observed good revaccination results concerning tetanus (39), measles, mumps, and rubella (40) and other live attenuated vaccines (41–44) in most children on ART.
Our present study shows that despite ART there is a decreased B cell count with decreased numbers of switched-memory B cells irrespective of the age group. This B cell defect seems to be less pronounced in effectively treated patients with low viral load. Despite lower switched memory B cell numbers complete immunity against tetanus was reached upon booster vaccination demonstrating effective memory B cell responses. The B cell defect described here may still have profound effects on the overall immunity of the child, e.g. for the immunity against HIV itself.
Abbreviations
- ARP:
-
age-related percentage
- ART:
-
antiretroviral therapy
- LTT:
-
lymphocyte transformation test
- tp:
-
time point
References
Amadori A, Zamarchi R, Ciminale V, Del Mistro A, Siervo S, Alberti A, Colombatti M, Chieco-Bianchi L 1989 HIV-1-specific B cell activation. A major constituent of spontaneous B cell activation during HIV-1 infection. J Immunol 143: 2146–2152
Zamarchi R, Barelli A, Borri A, Petralia G, Ometto L, Masiero S, Chieco-Bianchi L, Amadori A 2002 B cell activation in peripheral blood and lymph nodes during HIV infection. AIDS 16: 1217–1226
Shirai A, Cosentino M, Leitman-Klinman SF, Klinman DM 1992 Human immunodeficiency virus infection induces both polyclonal and virus-specific B cell activation. J Clin Invest 89: 561–566
Martinez-Maza O, Breen EC 2002 B-cell activation and lymphoma in patients with HIV. Curr Opin Oncol 14: 528–532
Grulich AE, Wan X, Law MG, Milliken ST, Lewis CR, Garsia RJ, Gold J, Finlayson RJ, Cooper DA, Kaldor JM 2000 B-cell stimulation and prolonged immune deficiency are risk factors for non-Hodgkin's lymphoma in people with AIDS. AIDS 14: 133–140
De Milito A, Morch C, Sonnerborg A, Chiodi F 2001 Loss of memory (CD27) B lymphocytes in HIV-1 infection. AIDS 15: 957–964
Chong Y, Ikematsu H, Kikuchi K, Yamamoto M, Murata M, Nishimura M, Nabeshima S, Kashiwagi S, Hayashi J 2004 Selective CD27+ (memory) B cell reduction and characteristic B cell alteration in drug-naive and HAART-treated HIV type 1-infected patients. AIDS Res Hum Retroviruses 20: 219–226
Miedema F, Petit AJ, Terpstra FG, Schattenkerk JK, de Wolf F, Al BJ, Roos M, Lange JM, Danner SA, Goudsmit J, Schellekens PT 1988 Immunological abnormalities in human immunodeficiency virus (HIV)-infected asymptomatic homosexual men. HIV affects the immune system before CD4+ T helper cell depletion occurs. J Clin Invest 82: 1908–1914
Conge AM, Tarte K, Reynes J, Segondy M, Gerfaux J, Zembala M, Vendrell JP 1998 Impairment of B-lymphocyte differentiation induced by dual triggering of the B-cell antigen receptor and CD40 in advanced HIV-1-disease. AIDS 12: 1437–1449
IRHIC 2004 Combined antiretroviral therapy reduces hyperimmunoglobulinemia in HIV-1 infected children. AIDS 18: 1423–1428
Shearer WT, Easley KA, Goldfarb J, Rosenblatt HM, Jenson HB, Kovacs A, McIntosh K 2000 Prospective 5-year study of peripheral blood CD4, CD8, and CD19/CD20 lymphocytes and serum Igs in children born to HIV-1 women. The P(2)C(2) HIV Study Group. J Allergy Clin Immunol 106: 559–566
Ibegbu C, Spira TJ, Nesheim S, Mendez H, Lee F, Polliotti B, Caba J, Nahmias A 1994 Subpopulations of T and B cells in perinatally HIV-infected and noninfected age-matched children compared with those in adults. Clin Immunol Immunopathol 71: 27–32
CDC 1994 Revised classification system for human immunodeficiency virus infection in children less than 13 years of age. MMWR Morb Mortal Wkly Rep 43: 1–10
RKI 2008 Recommendation of the Standing Vaccination Commission at Robert Koch Institute. Epidemiol Bull 30: 235–254
Niehues T, Reichenbach J, Neubert J, Gudowius S, Puel A, Horneff G, Lainka E, Dirksen U, Schroten H, Doffinger R, Casanova JL, Wahn V 2004 Nuclear factor kappaB essential modulator-deficient child with immunodeficiency yet without anhidrotic ectodermal dysplasia. J Allergy Clin Immunol 114: 1456–1462
Johnson AM, Whicher JT 2001 Effect of certified reference material 470 (CRM 470) on national quality assurance programs for serum proteins in Europe. Clin Chem Lab Med 39: 1123–1128
Niehues T, Rocha V, Filipovich AH, Chan KW, Porcher R, Michel G, Ortega JJ, Wernet P, Gobel U, Gluckman E, Locatelli F 2001 Factors affecting lymphocyte subset reconstitution after either related or unrelated cord blood transplantation in children—a Eurocord analysis. Br J Haematol 114: 42–48
Shearer WT, Rosenblatt HM, Gelman RS, Oyomopito R, Plaeger S, Stiehm ER, Wara DW, Douglas SD, Luzuriaga K, McFarland EJ, Yogev R, Rathore MH, Levy W, Graham BL, Spector SA 2003 Lymphocyte subsets in healthy children from birth through 18 years of age: the Pediatric AIDS Clinical Trials Group P1009 study. J Allergy Clin Immunol 112: 973–980
Kam KM, Leung WL, Wong KH, Lee SS, Hung MY, Kwok MY 2001 Maturational changes in peripheral lymphocyte subsets pertinent to monitoring human immunodeficiency virus-infected Chinese pediatric patients. Clin Diagn Lab Immunol 8: 926–931
Rodriguez C, Thomas JK, O'Rourke S, Stiehm ER, Plaeger S 1996 HIV disease in children is associated with a selective decrease in CD23+ and CD62L+ B cells. Clin Immunol Immunopathol 81: 191–199
Kansas GS, Dailey MO 1989 Expression of adhesion structures during B cell development in man. J Immunol 142: 3058–3062
LeBien TW 2000 Fates of human B-cell precursors. Blood 96: 9–23
Malaspina A, Moir S, Nickle DC, Donoghue ET, Ogwaro KM, Ehler LA, Liu S, Mican JA, Dybul M, Chun TW, Mullins JI, Fauci AS 2002 Human immunodeficiency virus type 1 bound to B cells: relationship to virus replicating in CD4+ T cells and circulating in plasma. J Virol 76: 8855–8863
Forster R, Schweigard G, Johann S, Emrich T, Kremmer E, Nerl C, Lipp M 1997 Abnormal expression of the B-cell homing chemokine receptor BLR1 during the progression of acquired immunodeficiency syndrome. Blood 90: 520–525
Jinquan T, Moller B, Storgaard M, Mukaida N, Bonde J, Grunnet N, Black FT, Larsen CG, Matsushima K, Thestrup-Pedersen K 1997 Chemotaxis and IL-8 receptor expression in B cells from normal and HIV-infected subjects. J Immunol 158: 475–484
Nagase H, Agematsu K, Kitano K, Takamoto M, Okubo Y, Komiyama A, Sugane K 2001 Mechanism of hypergammaglobulinemia by HIV infection: circulating memory B-cell reduction with plasmacytosis. Clin Immunol 100: 250–259
D'Orsogna LJ, Krueger RG, McKinnon EJ, French MA 2007 Circulating memory B-cell subpopulations are affected differently by HIV infection and antiretroviral therapy. AIDS 21: 1747–1752
Nagumo H, Agematsu K, Shinozaki K, Hokibara S, Ito S, Takamoto M, Nikaido T, Yasui K, Uehara Y, Yachie A, Komiyama A 1998 CD27/CD70 interaction augments IgE secretion by promoting the differentiation of memory B cells into plasma cells. J Immunol 161: 6496–6502
de Martino M, Tovo PA, Galli L, Gabiano C, Cozzani S, Gotta C, Scarlatti G, Fiocchi A, Cocchi P, Marchisio P, Canino R, Mautone A, Chiappe F, Campelli A, Consolini R, Izzi G, Laverda A, Alberti S, Tozzi AE, Duse M 1991 Prognostic significance of immunologic changes in 675 infants perinatally exposed to human immunodeficiency virus. The Italian Register for Human Immunodeficiency Virus Infection in Children. J Pediatr 119: 702–709
Moir S, Malaspina A, Pickeral OK, Donoghue ET, Vasquez J, Miller NJ, Krishnan SR, Planta MA, Turney JF, Justement JS, Kottilil S, Dybul M, Mican JM, Kovacs C, Chun TW, Birse CE, Fauci AS 2004 Decreased survival of B cells of HIV-viremic patients mediated by altered expression of receptors of the TNF superfamily. J Exp Med 200: 587–599
Samuelsson A, Sonnerborg A, Heuts N, Coster J, Chiodi F 1997 Progressive B cell apoptosis and expression of Fas ligand during human immunodeficiency virus type 1 infection. AIDS Res Hum Retroviruses 13: 1031–1038
Titanji K, Chiodi F, Bellocco R, Schepis D, Osorio L, Tassandin C, Tambussi G, Grutzmeier S, Lopalco L, De Milito A 2005 Primary HIV-1 infection sets the stage for important B lymphocyte dysfunctions. AIDS 19: 1947–1955
Malaspina A, Moir S, Ho J, Wang W, Howell ML, O'Shea MA, Roby GA, Rehm CA, Mican JM, Chun TW, Fauci AS 2006 Appearance of immature/transitional B cells in HIV-infected individuals with advanced disease: correlation with increased IL-7. Proc Natl Acad Sci USA 103: 2262–2267
Malaspina A, Moir S, Chaitt DG, Rehm CA, Kottilil S, Falloon J, Fauci AS 2007 Idiopathic CD4+ T lymphocytopenia is associated with increases in immature/transitional B cells and serum levels of IL-7. Blood 109: 2086–2088
Moir S, Fauci AS 2008 Pathogenic mechanisms of B-lymphocyte dysfunction in HIV disease. J Allergy Clin Immunol 122: 12–19; quiz 20–21.
Moir S, Ho J, Malaspina A, Wang W, DiPoto AC, O'Shea MA, Roby G, Kottilil S, Arthos J, Proschan MA, Chun TW, Fauci AS 2008 Evidence for HIV-associated B cell exhaustion in a dysfunctional memory B cell compartment in HIV-infected viremic individuals. J Exp Med 205: 1797–1805
Moir S, Malaspina A, Ho J, Wang W, Dipoto AC, O'Shea MA, Roby G, Mican JM, Kottilil S, Chun TW, Proschan MA, Fauci AS 2008 Normalization of B cell counts and subpopulations after antiretroviral therapy in chronic HIV disease. J Infect Dis 197: 572–579
Zaccarelli-Filho CA, Ono E, Machado DM, Brunialti M, Succi RC, Salomao R, Kallas EG, de Moraes-Pinto MI 2007 HIV-1-infected children on HAART: immunologic features of three different levels of viral suppression. Cytometry B Clin Cytom 72: 14–21
Rosenblatt HM, Song LY, Nachman SA, Stanley KE, Krogstad PA, Johnson GM, Wiznia AA 2005 Tetanus immunity after diphtheria, tetanus toxoids, and acellular pertussis vaccination in children with clinically stable HIV infection. J Allergy Clin Immunol 116: 698–703
Arpadi SM, Markowitz LE, Baughman AL, Shah K, Adam H, Wiznia A, Lambert G, Dobroszycki J, Heath JL, Bellini WJ 1996 Measles antibody in vaccinated human immunodeficiency virus type 1-infected children. Pediatrics 97: 653–657
Berkelhamer S, Borock E, Elsen C, Englund J, Johnson D 2001 Effect of highly active antiretroviral therapy on the serological response to additional measles vaccinations in human immunodeficiency virus-infected children. Clin Infect Dis 32: 1090–1094
Levin MJ, Gershon AA, Weinberg A, Blanchard S, Nowak B, Palumbo P, Chan CY 2001 Immunization of HIV-infected children with varicella vaccine. J Pediatr 139: 305–310
Lima M, De Menezes Succi RC, Nunes Dos Santos AM, Weckx LY, De Moraes-Pinto MI 2004 Rubella immunization in human immunodeficiency virus type 1-infected children: cause for concern in vaccination strategies. Pediatr Infect Dis J 23: 604–607
Melvin AJ, Mohan KM 2003 Response to immunization with measles, tetanus, and Haemophilus influenzae type b vaccines in children who have human immunodeficiency virus type 1 infection and are treated with highly active antiretroviral therapy. Pediatrics 111: e641–e644
Acknowledgements
We thank Sven Bellert and the members of the Laboratory of Pediatric Immunology at the University Hospital of Düsseldorf for their excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.pedresearch.org).
Rights and permissions
About this article
Cite this article
Ghosh, S., Feyen, O., Jebran, A. et al. Memory B Cell Function in HIV-Infected Children—Decreased Memory B Cells Despite ART. Pediatr Res 66, 185–190 (2009). https://doi.org/10.1203/PDR.0b013e3181aa057d
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3181aa057d
This article is cited by
-
Impfen bei Immundefizienz
Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz (2018)