Abstract
Fetuses with transposition and abnormalities of the foramen ovale and/or ductus arteriosus detected by ultrasound may develop severe hypoxemia postnatally. Higher than normal oxygen content in the pulmonary artery has been considered to be responsible. Patterns of blood flow in the normal fetus and the fetus with aortopulmonary transposition were reviewed. Well-oxygenated ductus venosus is preferentially directed through the foramen ovale into the left atrium. Normally this produces a higher oxygen content in the ascending aorta. In the fetus with transposition, pulmonary arterial oxygen content is higher. Pulmonary vascular resistance is decreased and the ductus arteriosus constricted. Increased pulmonary venous return to the left atrium tends to close the foramen ovale. Changes are more likely in the last trimester because sensitivity of the pulmonary circulation and ductus arteriosus increases. Severe ductus arteriosus constriction could result in pulmonary arterial hypertension and increased pulmonary arteriolar smooth muscle development. Variability of responses could be related to the proportion of umbilical venous blood passing through the ductus venosus. It is proposed that, in fetuses with evidence of abnormalities of the ductus arteriosus andør the foramen ovale, methods to occlude the ductus venosus be developed to avoid progressive changes.
Similar content being viewed by others
Main
In 1974, I proposed that, as a result of the patterns of blood flow in the fetus, the pulmonary circulation would be exposed to a higher oxygen saturation in the fetus with aortopulmonary transposition than in the normal fetus. This would induce pulmonary vasodilatation and increase pulmonary blood flow. As a result, the ductus arteriosus may be narrowed, because a greater proportion of the blood ejected by the right ventricle would be diverted into the pulmonary circulation away from the ductus (1). At that time it was not possible to examine the fetus in utero. However, with the advent of ultrasonography, two reports have described the presence of abnormalities of the foramen ovale and/or the ductus arteriosus in some fetuses with aortopulmonary transposition (2,3). The possible role of increased pulmonary arterial oxygen saturation in causing these changes was reiterated (2). Proposed mechanisms responsible for these changes and a possible approach to management are presented.
COURSE OF THE CIRCULATION
In the adult, blood circulates in series. It is ejected by the left ventricle and passes through the systemic circulation to the right atrium. It is then ejected by the right ventricle to the lungs where it is oxygenated and then passes into the left atrium and ventricle. Thus, oxygenated arterial and poorly oxygenated venous blood are well separated on the two sides of the heart.
Normal fetus.
The pattern of blood flow in the normal fetus is shown Figure 1 (1,4). In the fetus, blood is oxygenated in the placenta and returns to the body through the umbilical veins. Umbilical venous blood may pass through the portal venous system into the hepatic venous system and then through hepatic veins into the inferior vena cava, or it may bypass the liver and enter the inferior vena cava via the ductus venosus. Whatever the course, oxygenated blood mixes with systemic venous blood. Inferior vena cava blood may enter the right atrium or pass through the foramen ovale into the left atrium. Superior vena cava blood is channeled by the tubercle of Lower through the tricuspid valve, so that essentially none passes through the foramen ovale into the left atrium. Blood entering the right ventricle contains a major proportion of venous blood from the superior and distal inferior vena cava and a small proportion of oxygenated umbilical venous blood. In the fetal lamb, pulmonary arterial blood has an oxygen tension (Po2) of about 18 mm Hg and an oxygen saturation of about 50%. Because pulmonary vascular resistance is high in the fetus, only about 15% of right ventricular output is directed to the lungs; the remainder passes through the ductus arteriosus to the descending aorta.
Diagram of the circulation in the normal fetus, showing the patterns of blood flow and the oxygen saturations in the main vessels. Note the higher oxygen saturation in the ascending aorta compared with the descending aorta and the lower saturation in the pulmonary artery. The oxygen saturations shown are derived from fetal lambs in utero.
The left atrium and ventricle receive oxygenated blood through the foramen ovale as well as all pulmonary venous blood, which has a slightly lower oxygen saturation than pulmonary arterial blood. Because pulmonary blood flow is low, the oxygen saturation of blood entering the left atrium through the foramen ovale is not reduced greatly by the addition of pulmonary venous blood. Blood ejected by the left ventricle into the ascending aorta has an oxygen saturation of about 65% and Po2 of about 25–28 mm Hg. Descending aortic blood is derived predominantly from the ductus arteriosus, with only a small contribution from the ascending aorta across the aortic arch. The oxygen saturation of descending aortic blood is about 52–53% and Po2 is about 20 mm Hg. These differences in oxygen levels in ascending and descending aortic blood were believed to be the result of selective streaming of superior vena cava blood through the tricuspid valve into the right ventricle.
It is now recognized that streaming in the porta hepatis and proximal portion of the inferior vena cava contributes to the difference in left and right ventricular blood oxygen contents. The intra-abdominal umbilical vein enters the porta hepatis and first provides portal venous branches to the left lobe of the liver. The ductus venosus arises from the umbilical vein, which then joins the portal vein on the right side of the porta hepatis and provides the portal venous supply to the right lobe of the liver. The course of venous blood flows is shown in Figure 2. The left lobe of the liver receives venous blood exclusively from the umbilical vein; most blood in the ductus venosus is derived from the umbilical vein, with less than 10% from the portal vein. The right lobe receives almost all portal venous blood as well as a substantial portion of umbilical venous blood (5). The proportions of umbilical venous blood that are distributed to the hepatic circulation and to the ductus venosus vary greatly. Although an average of 55% of umbilical venous blood passes through the ductus venosus, the amount varies from about 20% to 80% (5–7). Ultrasound studies suggest that in human fetuses a somewhat smaller proportion of umbilical venous blood, about 25–40%, passes through the ductus venosus (8). The marked variability also has been observed in human fetuses and the proportion of umbilical venous blood distributed through the ductus venosus does not vary widely with repeated observations in the same fetus (Fig. 3) (9).
The patterns of blood flow in the umbilical, portal, and hepatic veins (LHV, RHV), and in the ductus venosus and inferior (IVC) and superior (SVC) vena cava in the fetal lamb are shown. For description see text. Reprinted from Rudolph AM Hepatology 3:254–258 ©1983 John Wiley & Sons, Inc., with permission.
The proportions of umbilical venous (UV) blood passing through the ductus venosus (DV) are shown in relation to the magnitude of umbilical blood flow in human fetuses [shown as percentage of combined ventricular output (CVO) distributed to the placenta]. Reprinted from Rudolph AM et al. Pediatr Res 5:452–465 ©1971 International Pediatric Research Foundation, with permission.
The ductus venosus and left and right hepatic veins enter the inferior vena cava just caudad to the diaphragm. Remarkable streaming can be observed in the fetal lamb; a stream of well-oxygenated blood from the ductus venosus and left hepatic vein is seen on the left posterior side of the intrathoracic inferior vena cava while poorly oxygenated blood from the distal inferior vena cava and the right hepatic vein is noted on the right anterior side. The distribution of these streams has been studied in fetal lambs using radionuclide labeled microspheres (10,11). Well-oxygenated ductus venosus blood, as well as left hepatic venous blood, streams preferentially through the foramen ovale into the left atrium and ventricle. Distal inferior vena cava and right hepatic venous blood preferentially flows through the tricuspid valve into the right ventricle. Umbilical venous blood has a Po2 of 32–35 mm Hg and an oxygen saturation of 82–88%; oxygen saturations in veins in the liver and inferior vena cava are shown in Figure 4. The preferential flow of ductus venosus blood through the foramen ovale contributes to the higher oxygen content of blood in the left ventricle and ascending aorta, as compared with the right ventricle and pulmonary artery.
Oxygen saturations in the umbilical, portal, and hepatic veins, and in the ductus venosus and inferior vena cava, are shown. These data were derived from fetal lambs in utero. DAo, descending aorta; DV, ductus venosus; IVC, inferior vena cava; LHV, RHV, left and right hepatic veins; PV, portal vein; UV, umbilical vein.
The preferential streaming of ductus venosus blood through the foramen ovale is the result of both morphologic and functional factors. In the fetal lamb, a membranous valve is attached along the inferior margin of the combined orifices of the ductus venosus and left hepatic vein at the entry into the inferior vena cava (12). This facilitates the streaming of well-oxygenated blood on the posterior left aspect of the inferior vena cava into the foramen ovale. This valve is not evident in the human fetus, but a sharp ridge at the entrance of the ductus venosus into the inferior vena cava may serve a similar purpose. Velocities of blood flow in the inferior vena cava and the ductus venosus differ markedly. In fetal lambs, mean velocity in the inferior vena cava is 16 cm/s, whereas ductus venosus mean velocity is 57 cm/s (13). This greater velocity facilitates maintaining the ductus venosus stream directed to the foramen ovale. The velocity of hepatic venous flow is similar to that in the inferior vena cava. The high velocity of ductus venosus flow has also been observed in human fetuses and mean velocity is similar to that in the lamb (14).
Fetus with aortopulmonary yransposition.
The morphology of the umbilical, portal, and hepatic venous circulations is not altered in the fetus with transposition. The patterns of umbilical and portal venous and ductus venosus blood flows can be assumed to be similar to those in the normal fetal circulation. Also, the preferential streaming of ductus venosus blood through the foramen ovale is probably maintained, so that left ventricular blood oxygen saturation will, as in the normal fetus, be higher than right ventricular saturation. However, because the aorta arises from the right ventricle, oxygen saturation of ascending aortic blood is considerably lower than normal. Conversely, oxygen saturation in the pulmonary artery is probably considerably higher than normal; in addition to the fact that well-oxygenated blood from the foramen ovale enters the left ventricle and pulmonary artery, pulmonary venous blood will have a high oxygen saturation because oxygen extraction by the lung is small. An estimate of blood oxygen saturations in different sites of the circulation in the fetus with transposition is presented in Figure 5. In making these estimates, I have assumed that the volumes of blood flow in the inferior and superior vena cava and the ductus venosus as well as that through the foramen ovale, are similar to those in the normal fetus.
Diagram showing patterns of blood flow and oxygen saturations in major vessels in the fetus with aortopulmonary transposition. The pulmonary artery arises from the left ventricle and the aorta from the right ventricle. Oxygen saturation in the pulmonary artery is considerably greater than normal and in the ascending aorta less than normal. Descending aortic blood oxygen saturation is similar to that in the normal fetus. Assumptions of volumes of blood flow were used in calculating oxygen saturations in the main vessels.
Ascending aortic blood oxygen saturation would be about 20% lower than normal in the fetus with transposition. Thus, oxygen content of blood delivered to both the heart and the brain would be greatly reduced. However, as shown in fetal lambs, this degree of hypoxemia does not reduce oxygen delivery to the brain or heart, because blood flow to these organs increases (15). Furthermore, oxygen consumption in the heart (16) and brain (17) are maintained at normal levels during hypoxemia. However, reserve of oxygen supply is limited, so that interference with oxygen supply resulting from fetal hypoxic stress or reduced blood flow could drastically affect oxygen supply. Also the possible effects of persistent high blood flows in the brain and myocardium on development should be considered.
As shown in Figure 5, only minor changes in oxygen levels in descending aortic blood are likely to occur, so that oxygen delivery to lower body organs is probably not altered.
ROLE OF THE PULMONARY CIRCULATION AND FORAMEN OVALE
Pulmonary vascular resistance in the fetus is very high, so that pulmonary blood flow is relatively small. In late gestation fetal lambs, only about 8% of combined ventricular output is distributed to the lungs (1,4). There are few studies in the human fetus, but pulmonary blood flow appears to be greater, representing about 15–20% of combined ventricular output (18). The fetal pulmonary vascular resistance is very sensitive to changes in Po2. A decrease in pulmonary arterial Po2 resulting from fetal hypoxemia induces marked pulmonary vasoconstriction (15,19). Increasing the Po2 by ventilation with air or oxygen results in a marked decrease in pulmonary vascular resistance and increase in pulmonary blood flow (20,21). Expansion of the lungs without changing fetal blood gases dramatically reduces pulmonary vascular resistance. In the fetus with transposition, pulmonary arterial blood oxygen saturation increases in the absence of ventilation; in fetal lambs in utero (22,23), as well as in the human fetus (18), increased oxygen levels induce pulmonary vasodilatation and increase pulmonary blood flow. In the study by Konduri et al. (23), an increase in fetal arterial Po2 of 7 mm Hg was associated with a 3-fold increase of pulmonary blood flow.
I have postulated that pulmonary arterial oxygen saturation could be increased to more than 70% in the fetus with transposition. This would be equivalent to an increase of Po2 of about 10 mm Hg and result in a marked increase in pulmonary blood flow. The increase in pulmonary blood flow would have two effects. Firstly, it would cause a marked increase in pulmonary venous return to the left atrium and result in an elevation of left atrial pressure, thus tending to close the foramen ovale. This could account for the abnormal and small foramen ovale observed in some fetuses with transposition. Secondly, because a large proportion of blood ejected into the main pulmonary artery would be directed to the relatively low resistance pulmonary circulation, a much smaller amount than normal would pass through the ductus arteriosus and this could account at least in part, for the smaller diameter of the ductus arteriosus in some fetuses with transposition.
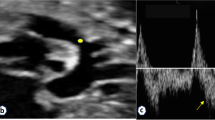
ROLE OF THE DUCTUS ARTERIOSUS
The diameter of the ductus arteriosus may be reduced, not only by the reduction in blood flow but also as a result of the increase in pulmonary arterial oxygen saturation. The ductus arteriosus is constricted by an increase in Po2 (24). In the normal fetus, the ductus arteriosus is exposed to the pulmonary arterial blood oxygen saturation of about 50%, because flow is exclusively from the pulmonary artery to the descending aorta. In transposition, the high oxygen saturation of pulmonary arterial blood could induce constriction of the ductus. The bidirectional flow of blood observed in some fetuses with transposition (2,3) could be related to the decreased pulmonary vascular resistance. During systole the high velocity of blood associated with ejection results in flow from the pulmonary artery to the descending aorta, but during diastole, blood flows from the aorta to the pulmonary circulation.
INCREASED PULMONARY VASCULAR RESISTANCE
The occurrence of persistent pulmonary hypertension of the newborn in some infants with aortopulmonary transposition (2) could also be the result of ductus arteriosus constriction. Experimental studies in fetal lambs have shown that partial compression of the ductus arteriosus results in pulmonary arterial hypertension and an increase in the thickness of smooth muscle in fifth generation pulmonary arteries (25,26). Newborn lambs that had constriction of the ductus arteriosus in utero had pulmonary hypertension and pulmonary vascular resistance did not respond normally to ventilation (26).
The factors determining the response of the pulmonary circulation in the fetus with transposition are of considerable interest. Whereas the increase in pulmonary arterial oxygen saturation decreases pulmonary vascular resistance, pulmonary arterial hypertension resulting from ductus arteriosus constriction increases the smooth muscle thickness of the arteriolar wall and eventually increases resistance, apparently independent of the level of oxygen saturation. The increase in resistance would be related to the severity and duration of constriction of the ductus. An elevated resistance would raise the afterload on the left ventricle and reduce ejection and pulmonary blood flow. Also, flow through the constricted ductus arteriosus would occur only from the pulmonary artery to the aorta. Thus, in the presence of a constricted ductus arteriosus, conversion of bidirectional flow to flow from the pulmonary artery to descending aorta alone would predict the likelihood of postnatal pulmonary arterial hypertension. The degree of constriction of the ductus arteriosus could be related to factors other than the level of oxygen in pulmonary arterial blood. Prostaglandin, particularly PGE2 relaxes the ductus arteriosus, even in the presence of elevated oxygen levels (27), and thus the concentration of circulating prostaglandin could modify the response of the ductus to oxygen.
Although the increased pulmonary vascular resistance would reduce flow through the foramen ovale and pulmonary blood flow, the elevated pulmonary arterial pressure will be maintained by the narrowed ductus arteriosus.
TIMING OF CHANGES IN FORAMEN OVALE AND DUCTUS ARTERIOSUS
Most ultrasound studies reported in fetuses with aortopulmonary transposition are beyond 30 wk gestation. In the report of Maeno et al. (2) one fetus at 23 wk gestation had no abnormalities of the foramen ovale or ductus arteriosus and four fetuses at 27–28 wk gestation showed either mild ductus narrowing or intermittent bidirectional shunting. Based on studies of the responses of the pulmonary circulation to changes in the Po2, it is unlikely that pulmonary vascular resistance would be decreased significantly in fetuses with transposition until the last trimester of gestation. In fetal lambs studied in utero (19), only minor responses to changes in pulmonary arterial Po2 were noted at gestational age below100 d (term is 150 d). Response increased progressively with gestational age during the third trimester (Fig. 6). In a study of human fetuses, inhalation of oxygen by the mother was associated with no change of pulmonary blood flow at about 25–26 wk gestation, but with a significant increase in flow beyond 30 wk (18).
Diagram showing the increasing sensitivity of pulmonary vascular resistance (PVR) response to changes in pulmonary arterial Po2 with advancing gestational age in fetal lambs in utero. Gestational age shown in days (d). Reprinted from Lewis AB et al. Circ Res 39:536–541 ©1976 Lippincott, Williams and Wilkins, with permission.
A gestational-dependent response of the ductus arteriosus has been demonstrated in fetal lambs. Perfusion of isolated ductus arteriosus showed little change in ductus resistance with increasing Po2 at less than 100 d gestation, but there was a progressive increase in the constrictor response to Po2 with advancing gestation (28) (Fig. 7). These findings would all suggest that it is unlikely that the elevated Po2 in pulmonary arterial blood in fetuses with transposition would have a significant effect until the latter part of the second, or early part of the third, trimester.
Diagrammatic representation of increasing responsiveness of the ductus arteriosus to change in Po2. Ductuses of fetal lambs at different gestational age were perfused with solutions with different Po2 levels and changes in resistance (RDA) calculated. Gestational age shown in days (d). Reprinted from McMurphy DM et al. Pediatr Res 6:231–238 ©1972 International Pediatric Research Foundation, with permission.
WHY ARE ONLY SOME FETUSES WITH TRANSPOSITION AFFECTED?
In the study of Jouannic et al. (3) of 119 fetuses with transposition in the last trimester, 24 had abnormalities of the foramen ovale or ductus arteriosus or both. That only some fetuses are affected could be related to differences in the responsiveness of the pulmonary circulation and/or ductus arteriosus to increases of Po2. A more plausible explanation is that it is related to the proportion of umbilical venous return that is directed through the ductus venosus. In fetal lambs, although an average of 55% of umbilical venous blood flows through the ductus venosus, the proportion varies from about 20% to 80% in different animals (5–7). In a study of human fetuses (9), the proportion also varied from about 20% to 80% and was not significantly different in the same fetus in relation to the magnitude of umbilical blood flow (Fig. 3). The mechanisms responsible for these wide variations in ductus venosus flows have not been resolved. However, a high flow through the ductus venosus, with high velocity and preferential streaming through the foramen ovale, would tend to result in a higher oxygen saturation in the left ventricle and pulmonary artery in the fetus with transposition, than if the ductus venosus flow was low.
PROPOSAL FOR FETAL THERAPY
A study of infants with aortopulmonary transposition showed that, of 295 candidates for an aortopulmonary switch procedure, 4.1% died before surgery (29). A common feature in these infants was the presence of a small foramen ovale. The status of the ductus arteriosus was not reported, but it is likely it was abnormal in some infants because they did not respond to prostaglandin infusion. In addition, a number of infants with transposition who have had surgery are noted to have high pulmonary vascular resistance that responds poorly to vasodilator therapy.
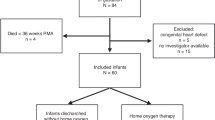
In this era of attempts to alter the course of some congenital cardiac lesions in the fetus by prenatal intervention, I propose that this be considered in the fetus with aortopulmonary transposition with abnormalities of the foramen ovale or ductus arteriosus. As postulated above, the changes are the result of the increased oxygenation of pulmonary arterial blood. If flow of ductus venosus blood across the foramen ovale could be prevented, the oxygen level of pulmonary arterial blood would be reduced. Figure 8 shows a diagram of the circulation in the fetus with aortopulmonary transposition, in which the ductus venosus has been eliminated and all umbilical venous blood flows through the liver. This results in mixing in the inferior vena cave below the diaphragm and the mixed blood is distributed to both the right and left sides of the heart. Based on assumptions of magnitude of blood flows, the effects of closure of the ductus venosus on oxygen levels in the major arteries in the fetus with aortopulmonary transposition are shown in Table 1.
Diagram showing patterns of blood flow and oxygen saturations in major vessels in the fetus with aortopulmonary transposition after closure of the ductus venosus. Oxygen saturation in the pulmonary artery is higher and in the ascending aorta is lower than in Figure 5, in which the ductus venosus is open. Descending aortic blood oxygen saturation is similar to that in the normal fetus. Assumptions of volumes of blood flow were used in calculating oxygen saturations in the main vessels.
The ductus venosus is not essential for mammalian fetal survival; it is absent in the horse fetus, except possibly in very early gestation, and also in late gestation in the fetal pig (30). It is unlikely that closure of the ductus venosus would significantly affect flow across the foramen ovale, because a larger amount of inferior vena caval blood would enter the foramen. This would decrease pulmonary arterial oxygen saturation. The use of pharmacologic agents to constrict the ductus venosus should be considered. The prostaglandin synthesis inhibitor, indomethacin, has been shown to increase resistance across the ductus venosus (31). However, it has the disadvantage that it also constricts the ductus arteriosus. Currently, the use of a mechanical device to occlude the ductus venosus seems more feasible. Although the ductus venosus has been traversed by catheters passed through the umbilical vein in the lamb fetus, I suggest that an approach be made from the maternal abdominal surface, as has been done to create an atrial septal opening in the human fetus with hypoplastic left heart (32). An occluder device could be manipulated into the ductus venosus to achieve closure.
Abbreviations
- PGE2:
-
prostaglandin E2
References
Rudolph AM 1974 Congenital Diseases of the Heart. Year Book, Chicago IL, pp 466–468
Maeno YV, Kamenir SA, Sinclair B, van der Velde ME, Smallhorn JF, Hornberger LK 1999 Prenatal features of ductus arteriosus constriction and restrictive foramen ovale in d-transposition of the great arteries. Circulation 99: 1209–1214
Jouannic JM, Gavard L, Fermont L, Le Bidois J, Parat S, Vouhe PR, Dumez Y, Sidi D, Bonnet D 2004 Sensitivity and specificity of prenatal features of physiological shunts to predict neonatal clinical status in transposition of the great arteries. Circulation 110: 1743–1746
Rudolph AM 1985 Distribution and regulation of blood flow in the fetal and neonatal lamb. Circ Res 57: 811–821
Edelstone DI, Rudolph AM, Heymann MA 1978 Liver and ductus venosus blood flows in fetal lambs in utero. Circ Res 42: 426–433
Rudolph CD, Meyers RL, Paulick RP, Rudolph AM 1991 Effects of ductus venosus obstruction on liver and regional blood flows in the fetal lamb. Pediatr Res 29: 347–352
Edelstone DL, Rudolph AM, Heymann MA 1980 Effects of hypoxia and decreasing umbilical blood flow on liver and ductus venosus blood flows in fetal lambs. Am J Physiol 238: H656–H663
Kiserud T 1999 Hemodynamics of the ductus venosus. Eur J Obstet Gynecol Reprod Biol 84: 139–147
Rudolph AM, Heymann MA, Teramo KA, Barrett CT, Raiha NC 1971 Studies on the circulation of the previable human fetus. Pediatr Res 5: 452–465
Edelstone DI, Rudolph AM 1979 Preferential streaming of ductus venosus blood to the brain and heart in fetal lambs. Am J Physiol 237: H724–H729
Reuss ML, Rudolph AM 1980 Distribution and recirculation of umbilical and systemic venous blood flow in fetal lambs during hypoxia. J Dev Physiol 2: 71–84
Bristow J, Rudolph AM, Itskovitz J 1981 A preparation for studying liver blood flow, oxygen consumption, and metabolism in the fetal lamb in utero. J Dev Physiol 3: 255–266
Schmidt KG, Silverman NH, Rudolph AM 1996 Assessment of flow events at the ductus venosus–inferior vena cava junction and at the foramen ovale in fetal sheep by use of multimodal ultrasound. Circulation 93: 826–833
Kiserud T 1999 Hemodynamics of the ductus venosus. Eur J Obstet Gynecol Reprod Biol 84: 139–147
Cohn HE, Sacks EJ, Heymann MA, Rudolph AM 1974 Cardiovascular responses to hypoxemia and acidemia in fetal lambs. Am J Obstet Gynecol 120: 817–824
Fisher DJ, Heymann MA, Rudolph AM 1982 Fetal myocardial oxygen and carbohydrate consumption during acutely induced hypoxemia. Am J Physiol 242: H647–H663
van Bel F, Sola A, Roman C, Rudolph AM 1995 Role of nitric oxide in the regulation of the cerebral circulation in the lamb fetus during normoxemia and hypoxemia. Biol Neonate 68: 200–210
Rasanen J, Wood DC, Debbs RH, Cohen J, Weiner S, Huhta JC 1998 Reactivity of the human fetal pulmonary circulation to maternal hyperoxygenation increases during the second half of pregnancy; a randomized study. Circulation 97: 257–262
Lewis AB, Heymann MA, Rudolph AM 1976 Gestational changes in pulmonary vascular responses in fetal lambs in utero. Circ Res 39: 536–541
Cassin S, Dawes GS, Mott JC, Ross BB, Strang LB 1964 The vascular resistance of the foetal and newly ventilated lung of the lamb. J Physiol 171: 61–79
Teitel DF, Iwamoto HS, Rudolph AM 1990 Changes in the pulmonary circulation during birth-related events. Pediatr Res 27: 372–378
Heymann MA, Rudolph AM, Nies AS, Melmon KL 1969 Bradykinin production association with oxygenation of the fetal lamb. Circ Res 25: 521–534
Konduri GG, Gervasio CT, Theodorou AA 1993 Role of adenosine triphosphate and adenosine in oxygen-induced pulmonary vasodilation in fetal lambs. Pediatr Res 33: 533–539
Oberhansli-Weiss I, Heymann MA, Rudolph AM, Melmon KL 1972 The pattern and mechanism of response of the ductus arteriosus and umbilical artery to oxygen. Pediatr Res 6: 693–700
Levin DL, Hyman AI, Heymann MA, Rudolph AM 1978 Fetal hypertension and the development of increased pulmonary vascular smooth muscle: a possible mechanism for persistent pulmonary hypertension of the newborn infant. J Pediatr 92: 265–269
Abman SH, Shanley PF, Accurso FJ 1989 Failure of postnatal adaptation of the pulmonary circulation after intrauterine pulmonary hypertension in fetal lambs. J Clin Invest 83: 1849–1858
Clyman RI, Heymann MA, Rudolph AM 1977 Ductus arteriosus responses to prostaglandin E1 at high and low oxygen concentrations. Prostaglandins 13: 219–223
McMurphy DM, Heymann MA, Rudolph AM, Melmon KL 1972 Developmental changes in constriction of the ductus arteriosus: responses to oxygen and vasoactive substances in the isolated ductus arteriosus of the fetal lamb. Pediatr Res 6: 231–238
Soongswang J, Adatia I, Newman C, Smallhorn JF, Williams WG, Freedom RM 1998 Mortality in potential arterial switch candidates with transposition of the great arteries. J Am Coll Cardiol 32: 753–757
Barclay AE, Franklin KJ, Pritchard MM 1945 The Foetal Circulation. Charles C. Thomas, Springfield, pp 169–172
Paulick RP, Meyers RL, Rudolph CD, Rudolph AM 1990 Venous and hepatic vascular responses to indomethacin and prostaglandin E1 in the fetal lamb. Am J Obstet Gynecol 163: 1357–1363
Marshall AC, van der Velde ME, Tworetzky W, Gomez CA, Wilkins-Haug L, Benson CB, Jennings RW, Lock JE 2004 Creation of An atrial septal defect in utero for fetuses with hypoplastic left heart syndrome and intact or highly restrictive atrial septum. Circulation 110: 253–258
Acknowledgements
On occasion, Dr. Norman Silverman and I discuss abnormal circulatory dynamics of fetuses with congenital cardiac lesions. This presentation was stimulated by his observations of ductus arteriosus narrowing and bidirectional ductus arteriosus in fetuses with aortopulmonary transposition.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rudolph, A. Aortopulmonary Transposition in the Fetus: Speculation on Pathophysiology and Therapy. Pediatr Res 61, 375–380 (2007). https://doi.org/10.1203/pdr.0b013e318030d5b9
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/pdr.0b013e318030d5b9
This article is cited by
-
Speckle Tracking Analysis in Fetuses with D-Transposition: Predicting the Need for Urgent Neonatal Balloon Atrial Septostomy
Pediatric Cardiology (2023)
-
D-Transposition of the great arteries with restrictive foramen ovale in the fetus: the dilemma of predicting the need for postnatal urgent balloon atrial septostomy
Archives of Gynecology and Obstetrics (2023)
-
Evaluation of fetal foramen ovale blood flow by pulsed Doppler ultrasonography combined with spatiotemporal image correlation
Cardiovascular Ultrasound (2021)
-
Reliability of Fetal Echocardiography in Predicting Postnatal Critical Hypoxia in Patients with Transposition of Great Arteries and Intact Ventricular Septum
Pediatric Cardiology (2021)
-
Impaired cerebral development in fetuses with congenital cardiovascular malformations: Is it the result of inadequate glucose supply?
Pediatric Research (2016)