Abstract
Docosahexaenoic acid (DHA) is an integral component of neural cell membranes and is critical to the development and function of the CNS. A premature delivery interrupts normal placental supply of DHA such that the infant is dependent on the nature of the nutritional support offered. The most abundant omega-3 fatty acid in pre-term formulas is α linolenic acid (ALNA), the precursor of DHA. This project studied the absorption, β-oxidation and conversion of ALNA to DHA by pre-term infants ranging from 30-37 wk of corrected gestation. [U-13C] ALNA was administered emulsified with a pre-term formula to 20 well pre-term infants on full enteral feeds. Enrichment of 13C in stool and as 13CO2 in breath was used to estimate absorption across the gut and partitioning toward β-oxidation respectively. Excretion of the administered dose of 13C in stool ranged from 2.0 to 26.2%; excretion decreased with increasing birth gestation. Appearance as 13CO2 on breath ranged from 7.6 to 19.0%. All infants synthesised eicosapentaenoic acid (EPA), docosapentaenoic acid (DPA) and DHA with the least mature having the highest cumulative plasma DHA. These results show considerable variation suggesting that the worst absorption of ALNA and the greatest production of DHA occur in infants born at the earliest gestation.
Similar content being viewed by others
Main
The long chain polyunsaturated fatty acid (LCPUFA) docosahexaenoic acid (DHA, 22:6n-3) is required for the development and function of the retina and the CNS (1). DHA is incorporated into neural cell membrane phospholipids, particularly over the last trimester of pregnancy (2). The true requirement for DHA is not known, although it has been suggested that it is about 35 mg/kg/d (3). Failure to accumulate sufficient DHA may impair neurologic development (4–6). Premature delivery interrupts normal placental supply of DHA so that the infant is dependent on the nature of the nutritional support offered. Although the need to include n-3 LCPUFA is recognised, the most abundant form in pre-term formulas is alpha linolenic acid (ALNA), the precursor of DHA. Although there is evidence that these infants can convert ALNA to DHA (7–9), the extent to which pre-term infants can meet their demands for DHA through this conversion remains uncertain.
The extent of absorption across the gastrointestinal tract, especially if immature, may also limit the availability of ALNA for DHA synthesis. Fat absorption is believed to be related to the maturity of the gastrointestinal tract in the pre-term neonate. Rings et al. demonstrated improving absorption of stearic and palmitic acid between 32 wk and 54 wk postconceptual age (10). As regards long chain polyunsaturated fatty acids, Moya and coworkers reported that the absorption of ALNA was relatively high (>90%), but the absorption of DHA was considerably less (∼62%) and more variable (11). The factors determining absorption in the pre-term infant and the clinical significance of this variation remain unclear.
The extent to which dietary LCPUFAs are partitioned toward oxidation or tissue deposition in the pre-term infant is also unclear. In the term infant Szitanyi et al. reported about 7% of 13C labelled linoleic acid was recovered on breath over 6 h (12). Tracer studies in adults have reported that up to 30% of 13C labelled ALNA was recovered on breath over 24h after feeding (13–16).
Using 13C or 2H labelled isotopes, both pre-term (7–9,17) and term (9,17) infants have been shown to convert ALNA to DHA. The extent to which this is sufficient to meet the demands of the pre-term infant for DHA and how it varies with gestational age is less clear (8). The limited numbers of observations in such studies generally precludes any direct examination of variability. However Uauy and coworkers have proposed that LCPUFA synthesis is more active at earlier gestations and diminished in growth retardation (9).
We report the metabolism of 13C labelled ALNA in 20 pre-term infants in terms of fractional recovery of label in stool and as 13CO2 on breath, and the concentrations of labelled ALNA, eicosapentaenoic acid (20:5n-3, EPA), docosapentaenoic acid (22:5n-3, DPA) and DHA in plasma and erythrocytes. Pre-term infants are a heterogeneous group. We have asked how the absorption, oxidation and conversion of ALNA to DHA varies within this group and how the partitioning of ALNA might be affected by maturity. Could some pre-term infants be more vulnerable to DHA deficit and the potential neurologic consequences as a result of this variation?
MATERIALS AND METHODS
Materials.
The [U-13C] ALNA was purchased from Martek Biosciences Corporation (Columbia, M.D. ). This preparation contained 97.1% ALNA, the remainder being medium and short chain fatty acids. All solvents were obtained from Fisher Chemicals Ltd (Loughborough, Leicestershire, UK). Internal standards were purchased from Sigma Chemical Co. (Poole, Dorset, UK). The Bond Elute solid phase extraction cartridges were purchased from Varian Limited (Walton-on-Thames, Surrey, UK).
Subject procedures.
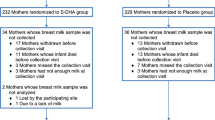
Twenty pre-term infants were studied with birth gestation ranging from 25–34 wk (median 30 wk) with a birth weight of 614–1883 g (median 1374 g). At the time of the study, these infants had a corrected gestational age of 30–37 wk (median 33 wk), postnatal age from 6–82 d (median 20 d) and weight of 1036–2080 g (median 1690 g). All babies were admitted after birth to the neonatal intensive care unit of the Royal Maternity Hospital, Belfast. The Research Ethics Committee of the Queen's University of Belfast granted ethical approval and parents gave written consent.
Babies were recruited after parents had chosen a specific low birth weight formula (SMA Low Birth Weight; SMA Nutrition, Maidenhead, Berks). SMA Low Birth Weight contains 4.4g of fat per 100 mL, 15.9% of which is linoleic acid and 0.6% is arachidonic acid whilst 1.7% is ALNA and 0.4% is DHA, (SMA Nutrition, Maidenhead, Berks). The study was carried out when each baby was clinically stable, self-ventilating in room air and established on full enteral feeds (usually 150-180 mL/kg/d). Each baby was weighed undressed immediately before the study. 20 mg/kg of [U-13C] ALNA was emulsified in 2 mL of formula feed using a system of three-way taps and syringes connected to the nasogastric tube. This was given to the baby immediately before a regular feed (and usually 2 or 3 h after the previous feed.) The 2 mL of emulsified isotope and formula milk was passed down the nasogastric tube to the baby and the remaining milk feed then used to flush the system of syringes to ensure the entire dose was administered to the baby.
Analysis of 13C excretion in stool.
Complete stool samples were collected for 5 d using nappy liners inserted in each nappy. Nursing staff placed the liner containing a stool sample in a plastic bag labelled with name, date and time before freezing them at –20°C. Stool samples were prepared for analysis as previously reported (18). Day 5 of the stool collection was used as a baseline and days 1-4 compared with this. Day 5 13C enrichment was not increased above background for any infant. Enrichment of 13C in stool was measured using Continuous Flow Isotope Ratio Mass Spectrometry (ANCA system; Europa Scientific Ltd., Crewe, United Kingdom) as described (18). Excretion of 13C in stool was calculated using the formula described by Schoeller et al. (19). The equation used is described in detail in appendix 1.
Analysis of 13CO2 excretion on breath.
Breath samples were collected using a facemask with a neoprene anaesthetic bag attached leading to a three-way tap. Once the anaesthetic bag was full of expired gas, samples were transferred into 10 mL Exetainer test tubes (Exetainer, Labco, High Wycombe, UK) using a three-way tap and syringe. Breath samples were collected before administration of the label, at hourly intervals for the first 6 h and then at 8, 10 and 24 h after administration of the [U-13C] ALNA. Indirect calorimetry (Deltatrac II; Datex Instrumentarium Corporation, Helsinki, Finland) was used to measure the whole body CO2 production before each breath sample. Enrichment of 13CO2 in breath was measured using Continuous Flow Isotope Ratio Mass Spectrometry (ANCA system; Europa Scientific Ltd., Crewe, United Kingdom) as described (18). The proportion of [U-13C] ALNA excreted as breath 13CO2 was expressed as a percentage of the absorbed dose calculated from the integrated area-under-the time × enrichment curve (AUC) over the 24 h period (13,14).
Preparation of total plasma lipids and erythrocyte phospholipids.
Blood (1.0 mL) was collected into tubes containing lithium heparin before the study and at 6, 24, 72 and 168 h. Blood samples were separated into plasma and cells by centrifugation at 2500 rpm for 15 min at 4°C. Plasma was stored at –20°C. Total plasma lipids were isolated by extraction with chloroform/methanol (2:1, v/v) (20) containing butylated hydoxytoluene (50 μg/mL) using heneicosanoic acid (100 μg/mL) (50 μg to 500 μL plasma) as an internal standard. Fatty acid methyl esters (FAME) were prepared by reaction with methanol containing 2% (v/v) H2SO4 for 18 h at 50°C (21). Erythrocytes were prepared at the time points of 24, 72 and 168 h. Cells were washed with 0.9% saline three times and total lipids were extracted. Diheptadecanoyl phosphatidyl choline was used as an internal recovery standard (25 μg to 1 mL of red cells). Phospholipids were isolated by solid phase extraction using 100 mg aminopropyl silica cartridges and FAME prepared (21).
Analysis of 13C labeled fatty acids in plasma and erythrocytes.
13C enrichment of n-3 fatty acids was measured by Gas Chromatography Combustion Isotope Ratio Mass Spectrometry (GC-C-IRMS) as described (13,14). FAME were resolved on a 50 m × 0.25 μm × 0.32 mm BPX-70 fused silica capillary column (SGE Europe Ltd., Milton Keynes, UK) using an HP6890 GC (Hewlett Packard, Wokingham, Berkshire, UK) with an Orchid interface (PDZ-Europa), combusted to CO2 by heating to 860°C in the presence of PtCuO and the 13CO2: 12CO2 ratio was determined by a 20/20 Stable Isotope Analyser (PDZ Europa). Tricosanoic acid methyl ester was used as the isotopic reference standard. ALNA, eicosapentaenoic acid (EPA), docosapentaenoic acid (DPA) and DHA were all resolved to baseline including complete separation of DPA from 24:0 and 24:1. FAME were identified by their retention times relative to standards. Concentrations of total fatty acids were calculated as described (13,14).
The relative area under the concentration time × enrichment curve for each labelled fatty acid has been previously used to estimate fractional conversion of ALNA to EPA, DPA and DHA (13,14,22). However, due to the restricted number of time points at which blood was collected, and therefore the limited value of the area under the curve, we have used the cumulative concentration of each labelled fatty acid to estimate the proportion of ALNA converted to longer chain, more unsaturated fatty acids. This method has been used before to estimate the conversion of ALNA to longer chain metabolites (23).
Statistical analysis.
The data describing the infants and the breath, stool and fatty acid data are presented as range and median. Where correlations are quoted Spearman's coefficient was used. The Mann Whitney U-test was used to compare the differences between groups of different maturity.
RESULTS
The fractional absorption of [U-13C] ALNA was estimated from its appearance in stool samples collected for four days after administration of the labelled fatty acid. Excretion of 13C in stool (n = 20) ranged from 2.0–26.0% of administered dose with a median of 7.0%. Stool 13C excretion decreased with increasing birth gestation (Spearman's r = −0.57, p = 0.008) (Fig. 1A) and birth weight (r = −0.60, p = 0.005) (Fig. 1B). Infants born at less than 30 wk gestation had nearly twice as much 13C in stool than those born at 30 wk and above (median 10.6 v 5.7; p = 0.03). There was no statistically significant relationship between stool excretion and corrected gestation (i.e., at the time of study), postnatal age, rate of growth or excretion of 13CO2 on breath.
Figure 2 illustrates the pattern of recovery of [U-13C] ALNA as 13CO2 on breath excretion over the first 24 h for 17 infants (two babies did not tolerate breath sampling and samples of one infant were lost). Excretion of 13CO2 above baseline was detected from the first hour after administration of the label, reaching a maximum at 4 h. At 24 h excretion had almost returned to baseline. Excretion of [U-13C] ALNA on breath as 13CO2 (n = 17) ranged from 7.6-19.0% (median 12.8%) of the absorbed dose over 24 h (it ranged from 6.9–17.7% (median 11.5%) of administered dose). Excretion on breath as a percentage of absorbed dose was greater with increasing weight gain (g/kg birth weight/d) (r = 0.53, p = 0.03) and postnatal age (r = 0.5, p = 0.04) but was not related to gestation, corrected gestation, birth weight or weight at the time of study. There was no statistical difference in breath excretion before and after 30 wk gestation (for either breath excretion calculated as a percentage of administered or absorbed dose). Excretion on breath as a percentage of administered dose increased with study gestation (r = 0.65, p = 0.005), but was not related to weight gain, birth weight, weight at the time of study, postnatal age or birth gestation.
Figure 3 summarises the cumulative labelled plasma fatty acid concentrations over the study period. The range of cumulative ALNA was 1.97–14.5 μM (median 8.54 μM), cumulative EPA was 0.27–2.65 μM (median 0.96 μM), cumulative DPA was 0.05–0.99 μM (median 0.24 μM) and cumulative DHA was 0.03–0.73 μM (median 0.35 μM). The fractional cumulative concentration was 84.6% for ALNA, 9.5% for EPA, 2.4% for DPA and 3.5% for DHA. The most immature infants (i.e., those with the earliest corrected gestational age) tended to have the highest cumulative plasma [13C] DHA (r = −0.52, p = 0.04). Infants of less than 30 wk gestation at birth had two to three times greater cumulative DHA than those born from 30 wk onwards (median 0.46 μM v 0.18 μM; p = 0.03). There was no significant relationship between cumulative plasma [13C] DHA and excretion of 13CO2 on breath (either as a percentage of administered or absorbed dose), weight (at birth or study time), weight gain or postnatal age.
Cumulative concentrations (t = 6, 24, 72 and 168 h) of the 13C labelled n-3 fatty acids α-linolenic acid (α-LNA), eicosapentaenoic acid (EPA), docosapentaenoic acid (DPA) and docosahexaenoic acid (DHA) in total plasma lipids following oral administration of 20 mg/kg of [U-13C] α-linolenic acid at t = 0. Horizontal bars represent medians. (n = 20).
Incorporation of labelled fatty acids into erythrocyte phospholipids was used as a marker of cellular uptake of n-3 fatty acids into cell membrane phospholipids. Figure 4 illustrates the cumulative labelled fatty acid concentrations in erythrocyte phospholipids. [U-13C] ALNA was not detected in erythrocyte phospholipids at any time. The range of cumulative erythrocyte EPA concentration was 0.02–0.20 μM (median 0.06 μM), cumulative DPA was 0.01–0.07 μM (median 0.03 μM) and cumulative DHA was 0.00–0.09 μM (median 0.04 μM). There was no significant relationship between any measured LCPUFA in erythrocyte phospholipids and corrected gestation, weight (at birth or study time), weight gain or postnatal age.
Cumulative concentrations (t = 24, 72 and 168 h) of the 13C labelled n-3 fatty acids eicosapentaenoic acid (EPA), docosapentaenoic acid (DPA) and docosahexaenoic acid (DHA) in erythrocyte membrane phospholipids, following administration of 20 mg/kg of oral [U-13C] α-linolenic acid at t = 0. Horizontal bars represent medians. (n = 16)
DISCUSSION
This paper describes for the first time the absorption, extent of partitioning toward β-oxidation and apparent conversion of ALNA to longer chain fatty acids by pre-term infants of differing gestational ages fed a DHA enriched formula. It appears that infants at less than 30 wk gestation have higher 13C losses in stool and similar β-oxidation, but higher plasma 13C DHA concentrations than those born after 30 wk gestation.
The median stool excretion of labelled ALNA (7%) is comparable to that of previous studies in term and pre-term infants using different methods (10,11). Although as a group, these infants appear to absorb ALNA well, availability varied widely with the poorest absorption in the most premature. Absorption was related to gestational age at birth rather than gestational age at the time of the study or postnatal age. We speculate that a premature birth is associated with an impairment of gut function that persists for weeks after delivery. The extent to which the ability to absorb fat improves in early life has not otherwise been studied in detail. The differences in losses of label in stool probably reflect impaired absorption rather than maldigestion as ALNA was administered as a FFA. Previous work has demonstrated impaired absorption of other fatty acids (10), which is generally attributed to low bile salt production impairing solubilization and fatty acid absorption (24). Thus infants who were likely to have the lowest accumulation of DHA into neurologic tissues were the least able to assimilate ALNA from the diet.
Weight gain is used as a guide to nutritional management but the infant with the worst absorption of ALNA (26.2% of administered dose) had a weight gain (18.5 g/kg/d) that was within the clinically acceptable range. Thus weight gain does not provide a reliable index of assimilation of nutrients such as ALNA.
About 13% of the administered label was recovered on breath as 13CO2. This may be an underestimate because of trapping of 13CO2 in the bicarbonate pool (25) although it should be noted that enrichment within breath returned to baseline by 24 h. Comparison to breath excretion of other labelled fats in pre-term infants (26) suggests that ALNA is neither spared nor used preferentially as an energy source relative to palmitic acid. Label excretion on breath in pre-term infants is half that seen in adults using comparable techniques (13–16). The smaller proportion of the label recovered on the breath may reflect lower β-oxidation activity due to immaturity of muscle and liver or selective partitioning of ALNA away from oxidation toward storage or synthesis (although there was no significant inverse relationship between measures of synthesis and oxidation). This in turn may increase the availability of ALNA for conversion to longer chain fatty acids. This is supported by the observation that women have both lower partitioning of ALNA toward β-oxidation and exhibit greater DHA synthesis compared with men (13,14).
Infants with the greatest weight gain had the greatest partitioning toward β-oxidation. This may be explained by the development of tissues with high β-oxidation activity such as muscle, liver and kidney. This group will also have the highest demand for DHA to support the growing CNS. Thus although these infants were gaining weight, the increase in capacity for β-oxidation may also limit the availability of ALNA for DHA synthesis.
All of the pre-term infants in this study converted [U-13C] ALNA to EPA, DPA and DHA, which is in agreement with previous reports (7–9,17). Labelled EPA, DPA and DHA were incorporated into erythrocyte membrane phospholipids. Postmortems carried out on infants who have died of sudden infant death suggest that red cell DHA may be a valid marker for brain DHA and that both are elevated in breast fed infants compared with unsupplemented formula fed infants (27).
Our data suggest that ALNA conversion is greatest in the most immature infant. Uauy et al. have previously suggested that this is the case (9). This implies that the capacity to synthesise DHA is greatest in those with the greatest demands. This could reflect an adaptation to premature delivery or the normal pattern of change taking place in fetal development.
We did not set out to study the overall retention or status of DHA or to determine the true dietary requirement for ALNA or DHA, instead we have studied ALNA metabolism. Our observations afforded the opportunity to estimate the DHA available to the infant allowing for absorption, oxidation and conversion together with preformed DHA from the feed. We reflected on the implications of our findings in relation to current guidelines and practice. To do this, it was necessary to make a series of assumptions. First, taking into account the loss in stool and breath and using the ratio of cumulative ALNA concentration to cumulative DHA concentration, the potential DHA yield from dietary ALNA would be about 4 mg/d (median and ranging from 0 to 18 mg/d). Second, assuming that preformed DHA in the formula feed would be absorbed and oxidised to the same extent as ALNA, then an additional median of 45 mg DHA/d would be provided by the formula feed (27 to 51 mg/d). Thus the average net DHA yield from formula as DHA from ALNA conversion and preformed DHA would be of the order of 53 mg/d (ranging from 33 to 69 mg/d). Finally, the likely DHA requirements were assumed to be at least 35 mg/kg/d (3). Taking this approach, the median estimated DHA deficit would be of the order of 18% ranging from a deficit of 30% to an excess of 3%. This potential shortfall in DHA could be an underestimate, as the demands of tissues other than the brain have not been taken into account. We recognize that there are substantial limitations in these calculations. It is assumed that fatty acid plasma concentration is a measure of total body DHA production and that concentrations can be compared with provide a measure of synthesis. We also have not taken into account the uptake of labeled DHA within cell membranes or retained within the liver and so not available in the plasma pool. Despite these limitations our data are consistent with the conclusions of Salem et al. (8) that in all infants, DHA synthesis from ALNA is unlikely to be sufficient to meet the demands for DHA.
This is the first study of its kind to be carried out on infants fed on a DHA enriched formula. Other isotope studies have used breast milk in some of their subjects (8,9) and therefore did supply preformed DHA. It is difficult to be sure of the extent to which a DHA enriched formula could have suppressed ALNA conversion, but Uauy et al. (9) in a post hoc analysis compared enterally fed to non- enterally fed babies after deuterium labeled ALNA administration showing that DHA synthesis is reduced albeit not statistically significantly. Further work is required to decide the extent to which ALNA metabolism can contribute to DHA requirements when a DHA enriched formula is used.
This study highlights the marked variability in the absorption, oxidation and conversion of ALNA to DHA in pre-term infants of differing gestational age. ALNA absorption was worst in those born most pre-term whilst the ability to convert to DHA may be greatest at this stage. The current approach to nutritional care does not take this variation into account. Our observations taken together with that reported previously, lead us to speculate that an approach that fails to accommodate this inherent variability may expose some infants, particularly the least mature, to an increased risk of DHA deficit.
Abbreviations
- ALNA:
-
alpha linolenic acid (18:3n-3)
- DHA:
-
docosahexaenoic acid (22:6n-3)
- DPA:
-
docosapentaenoic acid (22:5n-3)
- EPA:
-
eicosapentaenoic acid (20:5n-3)
- FAME:
-
fatty acid methyl ester
- LCPUFA:
-
long chain polyunsaturated fatty acid
References
Uauy R, Mena P, Rojas C 2000 Essential fatty acid metabolism in the micropremie. Clin Perinatol 27: 71–93
Martinez M 1992 Tissue levels of polyunsaturated fatty acids during early human development. J Pediatr 120: S129–S138
Clandinin MT, Chappell JE, Heim T, Swyer PR, Chance GW 1981 Fatty acid utilization in perinatal de novo synthesis of tissues. Early Hum Dev 5: 355–366
Simmer K, Patole S 2004 Longchain polyunsaturated fatty acid supplementation in pre-term infants. The Cochrane Database Syst Rev [on CD-ROM] (1) CD 000375
SanGiovanni JP, Parra-Cabrera S, Colditz GA, Berkey CS, Dwyer JT 2000 Meta-analysis of dietary essential fatty acids and long-chain polyunsaturated fatty acids as they relate to visual resolution acuity in healthy pre-term infants. Pediatrics 105: 1292–1298
Gibson RA, Makrides M 1999 Polyunsaturated fatty acids and infant visual development: a critical appraisal of randomized clinical trials. Lipids 34: 179–184
Carnielli VP, Wattimena DJ, Luijendijk IH, Boerlage A, Degenhart HJ, Sauer PJ 1996 The very low birth weight premature infant is capable of synthesizing arachidonic and docosahexaenoic acids from linoleic and linolenic acids. Pediatr Res 40: 169–174
Salem N Jr, Wegher B, Mena P, Uauy R 1996 Arachidonic and docosahexaenoic acids are biosynthesized from their 18-carbon precursors in human infants. Proc Natl Acad Sci USA 93: 49–54
Uauy R, Mena P, Wegher B, Nieto S, Salem N Jr 2000 Long chain polyunsaturated fatty acid formation in neonates: effect of gestational age and intrauterine growth. Pediatr Res 47: 127–35
Rings EH, Minich DM, Vonk RJ, Stellaard F, Fetter WP, Verkade HJ 2002 Functional development of fat absorption in term and pre-term neonates strongly correlates with ability to absorb long-chain fatty acids from intestinal lumen. Pediatr Res 51: 57–63
Moya M, Cortes E, Juste M, De Dios JG, Vera A 2001 Fatty acid absorption in pre-terms on formulas with and without long- chain polyunsaturated fatty acids and in terms on formulas without these added. Eur J Clin Nutr 55: 755–762
Szitanyi P, Koletzko B, Mydlilova A, Demmelmair H 1999 Metabolism of 13C- labeled linoleic acid in newborn infants during the first week of life. Pediatr Res 45: 669–673
Burdge GC, Jones AE, Wootton SA 2002 Eicosapentaenoic and docosapentaenoic acids are the principal products of alpha-linolenic acid metabolism in young men. Br J Nutr 88: 355–363
Burdge GC, Wootton SA 2002 Conversion of alpha-linolenic acid to eicosapentaenoic, docosapentaenoic and docosahexaenoic acids in young women. Br J Nutr 88: 411–420
Demmelmair H, Baumheuer M, Koletzko B, Dokoupil K, Kratl G 2001 Investigation of long-chain polyunsaturated fatty acid metabolism in lactating women by means of stable isotope techniques. Adv Exp Med Biol 501: 169–177
Vermunt SH, Mensink RP, Simonis MM, Hornstra G 2000 Effects of dietary alpha-linolenic acid on the conversion and oxidation of 13C-alpha-linolenic acid. Lipids 35: 137–142
Sauerwald TU, Hachey DL, Jensen CL, Chen H, Anderson RE, Heird WC 1997 Intermediates in endogenous synthesis of C22: 6n3 and C20: 4n6 by term and pre-term infants. Pediatr Res 41: 183–187
Murphy JL, Jones A, Brookes S, Wootton SA 1995 The gastrointestinal handling and metabolism of [1-13C] palmitic acid in healthy women. Lipids 30: 291–298
Schoeller DA, Klein PD, MacLean WC Jr, Watkins JB, van Santen E 1981 Fecal 13C analysis for the detection and quantitation of intestinal malabsorption. Limits of detection and application to disorders of intestinal cholylglycine metabolism. J Lab Clin Med 97: 440–448
Folch J, Lees M, Sloane Stanley GH 1957 A simple method for the isolation and purification of total lipids from animal tissues. J Biol Chem 226: 497–509
Burdge GC, Wright P, Jones AE, Wootton SA 2000 A method for separation of phosphatidylcholine, triacylglycerol, non- esterified fatty acids and cholesterol esters from plasma by solid- phase extraction. Br J Nutr 84: 781–787
Emken EA, Adlof RO, Gulley RM 1994 Dietary linolenic acid influences desaturation and acylation of deuterium-labeled linoleic and linolenic acids in young adult males. Biochim Biophys Acta 1213: 277–288
Burdge GC, Finnegan YE, Minihane AM, Williams CM, Wootton SA 2003 Effect of altered dietary n-3 fatty acid intake upon plasma lipid fatty acid composition, conversion of [13C] alpha-linolenic acid to longer-chain fatty acids and partitioning towards beta-oxidation in older men. Br J Nutr 90: 311–321
Watkins JB, Szczepanik P, Gould JB, Klein P, Lester R 1975 Bile salt metabolism in the human premature infant. Preliminary observations of pool size and synthesis rate following prenatal administration of dexamethasone and phenobarbital. Gastroenterology 69: 706–713
Irving CS, Wong WW, Shulman RJ, Smith EO, Klein PD 1983 [13C] bicarbonate kinetics in humans: intra- vs. interindividual variations. Am J Physiol 245: R190–R202
Craig JS, Mitchell DJ, Tubman TRJ, O'Hare MMT, McClure BG, Williams PD, McCallum A, Cawood A, Murphy JL, Wootton SA 2000 The gastrointestinal handling and metabolic disposal of 13C-labelled tripalmitin by pre-term infants. Proc Nutr Soc 59: 41A
Makrides M, Neumann MA, Byard RW, Simmer K, Gibson RA 1994 Fatty acid composition of brain, retina, and erythrocytes in breast- and formula-fed infants. Am J Clin Nutr 60: 189–194
Acknowledgements
The authors thank Mrs. Angela Hounslow for excellent technical assistance in conducting the analysis of stool and breath enrichment, as well as the nursing staff of the Neonatal Intensive Care Unit of the Royal Jubilee Maternity Service for their assistance with stool collection.
Author information
Authors and Affiliations
Corresponding author
Additional information
We wish to acknowledge financial support towards this study from the Northern Ireland Mother and Baby Action, the Medical staff committee of the Royal Maternity Hospital, Belfast, the Royal Maternity Fellowship Award, the Belfast Perinatal Trust, Wyeth Pharmaceuticals and Milupa.
APPENDIX
APPENDIX
Worked example for percentage of 13C label excreted in stool.
13C isotopic enrichment of label = 99 atom %
Moles of 13C/mol of ALNA = 18
Molecular weight of [U-13C] ALNA = MW
Weight of ALNA administered = W
Atom % of baseline stool sample = atom % b
Atom % of stool sample collected = atom % s
Mmol of Carbon in dry stool sample = C
1) Calculate the amount of 13C administered as [U-13C] ALNA (W/MW) × 18 × (99/100)
2) Calculate amount of 13C in stool sample above baseline (atom % s – atom % b)/100 = stool 13C
3) Calculate the percentage of 13C label in stool sample collected (stool 13C/amount of 13C administered) × C × 100
Rights and permissions
About this article
Cite this article
Mayes, C., Burdge, G., Bingham, A. et al. Variation in [U-13C] α Linolenic Acid Absorption, β-oxidation and Conversion to Docosahexaenoic Acid in the Pre-Term Infant Fed a DHA-Enriched Formula. Pediatr Res 59, 271–275 (2006). https://doi.org/10.1203/01.pdr.0000196372.29648.7a
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.pdr.0000196372.29648.7a
This article is cited by
-
Sicherheit und Risiken vegetarischer und veganer Ernährung in Schwangerschaft, Stillzeit und den ersten Lebensjahren
Monatsschrift Kinderheilkunde (2019)
-
Natural lecithin promotes neural network complexity and activity
Scientific Reports (2016)