Abstract
Thyroid hormone is essential for normal brain development including structures critical for visual processing. While chick and rodent models have demonstrated abnormal visual development following prenatal thyroid hormone loss, comparable data do not exist in the human. To determine whether human infants with intrauterine and early postnatal thyroid hormone insufficiencies have compromised visual abilities, we investigated contrast sensitivity and visual acuity development in 13 infant offspring of women with hypothyroidism during pregnancy (HYPO), 16 preterm infants born between 32 and 35 weeks gestation, 12 infants with congenital hypothyroidism (CH), and 20 typically developing infants. All were assessed with the sweep visual evoked potential technique at 3, 4.5, and 6 months (corrected) age. Results showed significantly reduced contrast sensitivity but normal visual acuity in HYPO and CH groups relative to controls (p < 0.003 and p < 0.05 respectively). Stratification of the HYPO group into subgroups based on maternal TSH levels during the first half of pregnancy revealed lower contrast sensitivities for infants whose mothers' TSH values were above than below the median (p < 0.05). In the CH group, those with an absent thyroid gland and/or a newborn TSH value above 200 mIU/L had lower contrast sensitivities than did those with other etiologies or TSH levels below 100 mIU/L (p < 0.05). There were no significant effects involving the preterm group. These results indicate that thyroid hormone is important for human visual development.
Similar content being viewed by others
Main
Thyroid hormone (TH) is essential for normal brain development (1). A lack of TH during fetal or early postnatal life is associated with specific brain damage. This includes abnormal neuronal proliferation and migration (2,3), decreased dendritic densities and synaptic profiles (4), impaired synaptic transmission (5), and reduced myelination (6). TH acts by regulating specific brain genes (7) through the formation of a nuclear receptor complex (8), which serves to up- or down-regulate specific genes (9) via a variety of signaling mechanisms (10,11). Because TH-regulated gene activity varies spatially and temporally in the brain (12), different types of deficits will follow from a loss of TH at different stages of development (13,14).
In the retina, TH is needed (15–17) for the differentiation of cones versus rods (18,19), specific cone subtypes (20), and retinal oligodendrocyte precursor cells (21) and for the production of essential proteins (22,23). Animal models demonstrate that when TH is lacking at a particular time prenatally, visual development and functioning will be impaired (20). Although comparable evidence is not available on humans, visual processing deficits in children with prenatal or neonatal TH insufficiencies (24,25) suggest that the human visual system may also be vulnerable to an early lack of TH insufficiency.
Even though negative feedback regulation of the fetal thyroid by the hypothalamus and pituitary does not commence until midgestation (26), the presence of TH receptors in human fetal brain tissue in the first trimester (27) suggests that TH is probably needed well before the fetal thyroid is functional. TH of maternal origin is evident in coelomic fluid from the start of pregnancy (28), and by the end of pregnancy, maternal TH may still account for as much as 30% of the fetal TH supply (29). Maternal hypothyroidism, congenital hypothyroidism (CH), and preterm birth, which represent conditions involving an insufficient TH supply, allow one to assess the impact of insufficient TH on the developing visual system. In maternal hypothyroidism, the effects are most salient in early pregnancy, when the fetus's own TH supply is not yet available (30). Correlations between maternal TH levels in early pregnancy and the child's subsequent outcome signify that adequate levels of maternal TH are necessary for normal offspring neurodevelopment (31,32). Because children with CH do not produce enough TH on their own and the mother's thyroid cannot fulfill all of their third-trimester TH needs, they may experience TH insufficiency in the latter part of gestation (33). Also, because these children lack TH postnatally until replacement hormone takes effect (34), they may manifest further cognitive deficits (35). Children who are born preterm, who have a severed maternal thyroid supply before their own glands are fully competent (36), may exhibit low TH levels at birth, and these remain low or even decline ex utero (37,38). Low TH levels in preterm infants have also been associated with later suboptimal neurodevelopment (39,40).
In this article, we describe how a lack of TH during pregnancy or early life affects children's contrast sensitivity and visual acuity development. These core visual abilities were chosen because of their different developmental trajectories (41), and they are differentially compromised in certain pediatric conditions (42–44). We hypothesized that because maternal hypothyroidism, CH, and preterm birth each involve a different time period of TH insufficiency, they may have a different impact on contrast sensitivity and visual acuity development.
METHODS
Three groups of infants with TH insufficiency and typically developing control subjects were tested at 3, 4.5, and 6 mo (corrected) age at The Hospital for Sick Children (HSC; Toronto, Ontario, Canada). Testers were masked to infant group status. Prior to testing, informal consent was obtained from all parents who received a full debriefing of procedures in accordance with the Declaration of Helsinki. The Research Ethics Board at HSC formally approved all procedures.
Participants.
From an original sample of 102 infants tested once minimally, 74 infants who participated in all three sessions were considered for this study. All of their mothers had a normal pregnancy, delivery, and, except for the preterm group, a full-term pregnancy. All children were free of neonatal or birth complications or neonatal disease (except for hypothyroidism in the CH group). From a total of 74 infants who fit these criteria, an additional 13 were eliminated because mothers reported taking medications for other illnesses during pregnancy (e.g. fluvoxamine for depression; n = 6), children took medications for illnesses in infancy (n = 4), and technical difficulties (e.g. software malfunction) or children were fussy and noncompliant (n = 3). The final sample size of 61 infants included 13 offspring of hypothyroid women (HYPO), 12 with CH, 16 who were born preterm (PREM), and 20 control subjects.
The HYPO group was recruited from data sheets for the period from April 1999 to October 2000 of the Motherisk Clinic, which provides antenatal counseling on the risks of maternal illnesses, medications, and substances of abuse to the fetus. All mothers had called this clinic to inquire about hypothyroidism predating (n = 10) or acquired during (n = 3) pregnancy. Although all were treated with l-thyroxine, their dosages were generally insufficient because all had raised TSH levels in the first and/or second trimester (45), and a few also had elevated TSH levels throughout pregnancy. The CH group consisted of infants who were identified through the Ontario newborn screening program between January 2000 and December 2001 on the basis of a TSH value >20 mIU/L (mean = 150.5 mIU/L; range = 20–400) at 2–3 d of life (46). Except for two children who were treated by a local pediatric endocrinologist, all were followed in the Endocrine Clinic at HSC and received an initial replacement therapy dose of ≈10 μg/kg l-thyroxine at a median age of 9 d (range = 6–25 d). Technetium scanning identified five with athyreosis, five with an ectopic gland, and two with dyshormonogenesis. The PREM group was born between September 2000 and May 2001 at 32–35 wk gestation in the level II nursery of Sunnybrook and Women's College Health Sciences Centre in Toronto. All were screened to be free of any gross neonatal complications (e.g. prematurity, bronchopulmonary dysplasia, intraventricular hemorrhage). Control subjects had normal TSH levels at birth and were born to women with no signs of hypothyroidism during pregnancy. For eight control infants, mothers were recruited from a local obstetrician, who measured their TSH levels at 12 wk of pregnancy (range = 1.15–2.14 mIU/L). The remaining 12 control infants were born between May and December 2000 at Sunnybrook and Women's College Health Sciences Centre and were recruited from the level I neonatal nursery monthly birth lists, which had been previously screened by a neonatologist (E.A.) to be free of neonatal or perinatal complications. Of the families listed, ≈25% who lived in the central Toronto area were invited to participate, and of these, ≈20% agreed to participate in the study.
Sweep visual evoked potentials.
Visual evoked potentials (VEPs) (47) were measured using the International 10–20 system (48). Active electrodes were placed over the infant's scalp at O1, OZ, and O2, and at CZ (reference) and Pz (ground). The analogue electroencephalograph signal was amplified using a Grass Model 12 Data Acquisition System. Analogue to digital signal conversion, data acquisition, and stimulus presentation all were controlled using the PowerDiva (49) software system. The sweep VEP technique estimated contrast sensitivity and grating acuity by tracking the amplitude of the steady-state evoked response to a black-and-white sine wave (striped) grating, which increased in contrast or spatial frequency. Thresholds were determined by performing a linear regression over a range of increasing or decreasing response values to zero amplitude.
During testing, each infant sat on his or her parent's lap 70 cm from a 17” (43 cm) monochrome video monitor. Black and white gratings changed in contrast or spatial frequency over the course of a 10-s interval. Gratings were phase-reversed 12 times per second (modulation frequency = 6 Hz) and subtended a visual angle of 21° by 21°. Mean luminance was 105 cd/m2. A small toy, which was dangled ≈2 cm from the screen, served to direct the infant's attention to the monitor.
For each infant, three to five thresholds were obtained per session. Sweep ranges were age appropriate (50), and order of conditions was randomized. To be scorable, all evoked responses had to meet the following criteria: 1) average amplitude of the response frequency exceeded noise by a factor of three (51); 2) phase of response was constant or synchronized with stimulus onset, or phase could lag progressively as spatial frequency increased or as contrast decreased (52); and 3) the peak amplitude of the signal was significantly above zero at the p < 0.05 level using the circular T2 statistic (52), which tests the consistency of the amplitude and phase of the averaged responses.
For deriving the dependent variables, thresholds were fitted with a negative exponential function (41) y = ce−ax, where y equals contrast sensitivity and x equals spatial frequency (Fig. 1). Four variables were obtained per session: 1) peak sensitivity (c) or the highest log contrast sensitivity; 2) the high spatial frequency roll-off (a) or rate at which contrast sensitivity is reduced as spatial frequency increases; 3) coefficient of determination (COD) or the fit of the negative exponential model; and 4) grating acuity (acuity limit of the contrast sensitivity function) obtained in the 80% spatial frequency condition. Because the COD distribution was heavily skewed, this variable was transformed (53) whereby y = 2arcsine(√p), where p was the infant's COD score.
Eye examination.
Eye examinations involved undilated retinoscopy using the Mohindra technique, an approach that shows good correlation to dilated measurement (54). Mean sphere equivalent and cylindrical error were measured at one of the infant's three visits. Fundus ophthalmoscopy showed no abnormality in any infants.
Data analyses.
VEP data were analyzed using a mixed-model repeated-measures ANOVA with groups as the between-subjects variable and age as the within-subjects variable, with repeated-measures analyses using the Greenhouse and Geisser adjustment. Significant group main effects were analyzed using pairwise F tests with controls. T tests served to compare subgroups of infants.
RESULTS
Demographic information.
Groups did not differ in sex distribution (Table 1) or maternal or socioeconomic status (data not shown). Except for CH, no differences in newborn TSH levels were seen. For the subgroup of HYPO mothers with TSH information, significantly elevated levels (p < 0.01) compared with control subjects were observed.
Between-group analyses.
Mean log peak contrast sensitivity scores ranged from 1.75 to 2.2 log units. ANOVA revealed a significant main effect of Group (F = 3.62, df = 3,57, p = 0.018), which reflected the reduced peak contrast sensitivities for HYPO and CH relative to control subjects (F = 9.36, df = 1,32, p = 0.003; and F = 4.08, df = 1,31, p = 0.04, respectively). For HYPO, the difference was ≈0.20 log units and for CH was 0.15 log units. There were no effects of age or group × age interaction. Figure 2 shows that after 3 mo of age, peak contrast sensitivity values did not change.
Table 2 presents the groups' roll-off and visual acuity parameters. For roll-off, only age was significant (F = 4.68, df = 1.9, 110, p < 0.01), which reflected a generalized increase at higher spatial frequencies. This effect was somewhat larger between 4.5 and 6 mo of age than between 3 and 4.5 mo (means across groups: 3 mo = −0.59 ± 0.03; 4.5 mo = −0.61 ± 0.04; 6 mo = −0.52 ± 0.04). An effect of age was also observed for visual acuity (F = 22.9, df = 1.9, 111.2, p < 0.001), reflecting a linear increase in acuity between 3 and 6 mo of age (F = 41.5, df = 1,57, p < 0.001). Although the group main effect and interactions were not significant for PREM, these infants showed a trend toward mildly reduced visual acuity (p = 0.065) at 6 mo of age (see Table 2).
For COD, all effects were significant. The age effect (F = 5.16, df = 1.9, 113, p < 0.007) reflected a linear increase in r2 with age (F = 6.27, df = 1,57, p < 0.015). The group effect (F = 3.29, df = 3,57, p < 0.03) and group × age interaction (F = 2.2, df = 5.9, 113.2, p < 0.048) reflected the lower COD scores by HYPO and CH (but not PREM) relative to controls (see Fig. 3). This effect was particularly evident at 3 mo of age (HYPO: F = 4.37, df = 1,32, p < 0.04; CH: F = 18.19, df = 1,31, p < 0.001). The poorer fit of the data to the curve for HYPO and CH groups reflected their reduced contrast sensitivity at the low spatial frequency end of the function (data not shown). These results therefore signify that the data of 3-mo-old children in the HYPO and CH groups did not adequately fit the exponential model of the contrast sensitivity function. A similar trend was also noted at 4.5 mo for the CH group (F = 3.11, df = 1,31, p < 0.08).
Within-group analyses.
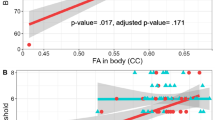
To determine whether factors within the HYPO and CH groups contributed to reduced peak contrast sensitivities, we used a median split procedure. Infants in the HYPO group were stratified into subgroups on the basis of mothers' mean TSH values (range: 3.28–7.83 mIU/L) during the first and/or second trimester of pregnancy. The more severe group had mothers with TSH values between 5.53 and 7.83 mIU/L, and the less severe subgroup had mothers with values <5.53 mIU/L. ANOVA revealed a significant group × age interaction (F = 3.94, df = 2,22, p < 0.05) but no independent effects of group or age with the interaction reflecting an increase with age in peak sensitivity in the less severe group and the opposite trend for the more severe group (see Fig. 4). A similar set of analyses on COD scores revealed no effects, suggesting that the fit of the negative exponential curve is insensitive to severity of maternal thyroid disease. Finally, an identical analysis stratifying those with available data in the HYPO group according to maternal free thyroxine levels during pregnancy yielded no significant group differences.
The CH group was stratified by the child's initial hypothyroidism severity, with the more severe subgroup consisting of six infants with either athyreosis or TSH >200 mIU/L and the less severe subgroup with a lingual gland or dyshormonogenesis and having TSH values <100 mIU/L. A one-tailed t-test revealed that these groups differed significantly in log peak sensitivity, reflecting the lower scores at 6 mo of age of the more severe CH subgroup (1.8 versus 2.08; t = 2.62, df = 11, p < 0.05) (Fig. 5). There were no differences in COD scores (Fig. 5).
Refractive Error.
To determine whether contrast sensitivity effects could be explained by optical factors, we also compared groups as to sphere equivalent and cylindrical errors. Refractive errors (Table 3) were not different among the groups. Values are comparable to those reported in another study of typically developing infants.
DISCUSSION
Present findings support our hypothesis of differences from normal in contrast sensitivity and visual acuity development in children of hypothyroid mothers, children with CH, and children who were born preterm at low risk. We found that compared with typically developing children, 3- to 6-mo-old infants whose mothers had preexisting or de novo hypothyroidism in pregnancy or who themselves had CH showed reduced contrast sensitivity at low spatial frequencies. In contrast, children who were born preterm (between 32 and 35 wk gestation) had normal contrast sensitivity but showed a trend toward weaker visual acuity. Children of hypothyroid women had large contrast sensitivity deficits when mothers had high TSH levels in the first half of pregnancy, as did children who had CH and an absent thyroid gland or very elevated TSH levels at birth. In both groups, the fit of the contrast sensitivity function was abnormal at 3 mo of age (and persisted until 4.5 mo in the CH group), suggesting an additional transient loss of sensitivity at the lowest spatial frequencies.
These findings therefore signify that adequate levels of TH are needed throughout pregnancy to ensure normal contrast sensitivity development, particularly at low spatial frequencies. Because the maternal hypothyroid group had the strongest deficit of the three clinical groups, adequate TH seems especially necessary during early pregnancy. Children with severe CH also showed reduced contrast sensitivity (but to a lesser degree than HYPO), indicating that TH is additionally needed during the third trimester for proper development. The normal maternal TH contribution in the CH group was not enough to offset their fetal thyroid hormone insufficiency because many children had elevated TSH levels at birth. Children with less severe CH had primarily postnatal hypothyroidism and attained normal contrast sensitivity functioning, suggesting that contrast sensitivity does not seem to be vulnerable to a postnatal lack of TH.
Preterm infants who were born between 32 and 35 wk gestation had typical contrast sensitivity development but had mildly weaker visual acuity. Rooman et al. (37) suggested that the fetal thyroid is able to assume adequate function and has less need for maternal supplementation after 33 wk gestation. Because even the youngest preterm infants in our study (i.e. 32 wk gestation) showed no deficits, these infants likely had sufficient TH for the normal development of contrast sensitivity. Indeed, “low-risk” preterm infants have better acuity relative to age-matched term infants (55), possibly as a result of their greater visual experience. Because all groups displayed age-appropriate refractive error, observed differences in acuity cannot be attributed to optical factors.
According to Norcia et al. (41), peak contrast sensitivity is adult-like by 3 mo of age and improves little over the remainder of the first year. Our findings on typically developing infants are similar, showing no major changes in peak contrast sensitivity between 3 and 6 mo of age. However, there were contrast sensitivity changes in the HYPO and CH groups between 3 and 6 mo of age. In both groups, those with the most severe conditions showed contrast sensitivity reductions at 6 mo, with the less severe infants showing no deficit or some recovery. This finding suggests that only the severely affected infants have persisting deficits, whereas those who are less severely affected manifest only delays in development.
Animal studies have shown that TH is necessary for the development of primary visual structures—the retina, magnocellular neurons in the lateral geniculate nucleus of the thalamus, and the primary visual cortex (19)—with timing being earlier for retina than for thalamus and for thalamus than for cortex (13). Given that TH is important for neurodevelopmental processes along this pathway, a lack of TH during these periods would disrupt such development (13,14). Because the HYPO group had the most compromised contrast sensitivity, this suggests that the effects of TH loss on development was likely disrupted at retinal and/or thalamic levels. Milder deficits in the CH group suggests cortical disruption. Unfortunately, because the VEP represents a cortical response to visual stimuli (56) and reflects processing along the entire pathway, it cannot specify the neuroanatomic levels of a deficit. Further testing using electroretinograms and developmental visual marker tasks (57,58) may serve to identify affected neuroanatomic sites.
Although this is the first study of its kind to compare models of human TH insufficiency at a basic functional level, it is limited for several reasons. Our small sample sizes may have reduced the ability to detect differences on variables other than peak contrast sensitivity and so not allow for in-depth analysis of within-group differences. A median split procedure that was used to stratify infants into more versus less severely affected subgroups did not permit determination of the TSH levels that define impairment or the critical period for deficits to occur. Because most mothers were under the care of family doctors and clinical community endocrinologists, who measured TSH mainly and at varying intervals and frequencies, we were not able to control when exactly thyroid hormones were measured. Subanalyses that are based on TSH values may not be ideal because TSH does not predict later infant outcome as well as does free thyroxine (48). Finally, because the sweep VEP is not ideal for estimating results of individual subjects, conclusions about timing effects for specific cases were limited.
Nevertheless, our results do demonstrate that adequate levels of TH are necessary throughout pregnancy for normal human contrast sensitivity development. Although the critical period extends throughout gestation, insufficient TH during early pregnancy produces a strong and persisting contrast sensitivity deficit. The clinical relevance of present findings awaits further testing (currently ongoing) that will determine specific cognitive dysfunctions. Given previous findings that showed suboptimal visuospatial and visuomotor abilities in thyroid-insufficient infants, these particular abilities may be dependent on normal contrast sensitivity functioning.
CONCLUSION
In conclusion, present findings suggest that TH is definitely necessary for human visual development, and some effects of TH loss during pregnancy may manifest in structures that are critical for visual processing.
Abbreviations
- CH:
-
congenital hypothyroidism
- COD:
-
coefficient of determination
- HSC:
-
The Hospital for Sick Children
- HYPO:
-
maternal hypothyroidism
- PREM:
-
preterm birth
- TH:
-
thyroid hormone
- VEP:
-
visual evoked potential
References
Bernal J, Nunez J 1995 Thyroid hormones and brain development. Eur J Endocrinol 133: 390–398
Potter BJ, Mano MT, Belling GB, McIntosh GH, Hua C, Cragg BG, Marshall J, Wellby ML, Hetzel BS 1982 Retarded fetal brain development resulting from severe dietary iodine deficiency in sheep. Neuropathol Appl Neurobiol 8: 303–313
Shapiro S 1966 Metabolic and maturational effects of thyroxine in the infant rat. Endocrinology 78: 527–532
Legrand J 1984 Effects of thyroid hormone on central nervous system development. Ophthalmic Physiol Opt 13: 9–16
Gilbert ME, Paczkowski C 2003 Propylthiouracil (PTU)-induced hypothyroidism in the developing rat impairs synaptic transmission and plasticity in the dentate gyrus of the adult hippocampus. Brain Res Dev Brain Res 145: 19–29
Rosman NP, Malone MJ, Helfenstein M, Kraft E 1972 The effect of thyroid deficiency on myelination of brain. A morphological and biochemical study. Neurology 22: 99–106
Koibuchi N, Chin WW 2000 Thyroid hormone action and brain development. Trends Endocrinol Metab 11: 123–128
Brent GA 2000 Tissue-specific actions of thyroid hormone: insights from animal models. Rev Endocr Metab Disord 1: 27–33
Forrest D, Reh TA, Rusch A 2002 Neurodevelopmental control by thyroid hormone receptors. Curr Opin Neurobiol 12: 49–56
Anderson GW 2001 Thyroid hormones and the brain. Front Neuroendocrinol 22: 1–17
Thompson CC, Potter GB 2000 Thyroid hormone action in neural development. Cereb Cortex 10: 939–945
Bradley DJ, Towle HC, Young WS 3rd 1992 Spatial and temporal expression of alpha- and beta-thyroid hormone receptor mRNAs, including the beta 2-subtype, in the developing mammalian nervous system. J Neurosci 12: 2288–2302
Morreale de Escobar G, Obregon MJ, Escobar del Rey F 2000 Is neuropsychological development related to maternal hypothyroidism or to maternal hypothyroxinemia?. J Clin Endocrinol Metab 85: 3975–3987
Howedeshell K 2002 A model of the development of the brain as a construct of the thyroid system. Environ Health Perspect 110: 337–348
Gamborino MJ, Sevilla-Romero E, Munoz A, Hernandez-Yago J, Renau-Piqueras J, Pinazo-Duran MD 2001 Role of thyroid hormone in craniofacial and eye development using a rat model. Ophthalmic Res 33: 283–291
Kelley MW, Turner JK, Reh TA 1995 Ligands of steroid/thyroid receptors induce cone photoreceptors in vertebrate retina. Development 121: 3777–3785
Knipper M, Zinn C, Maier H, Praetorius M, Rohbock K, Kopschall I, Zimmermann U 2000 Thyroid hormone deficiency before the onset of hearing causes irreversible damage to peripheral and central auditory systems. J Neurophysiol 83: 3101–3112
Sevilla-Romero E, Munoz A, Pinazo-Duran MD 2002 Low thyroid hormone levels impair the perinatal development of the rat retina. Ophthalmic Res 34: 181–191
Sjoberg M, Vennstrom B, Forrest D 1992 Thyroid hormone receptors in chick retinal development: differential expression of mRNAs for alpha and N-terminal variant beta receptors. Development 114: 39–47
Ng L, Hurley JB, Dierks B, Srinivas M, Salto C, Vennstrom B, Reh TA, Forrest D 2001 A thyroid hormone receptor that is required for the development of green cone photoreceptors. Nat Genet 27: 94–98
Baas D, Legrand C, Samarut J, Flamant F 2002 Persistence of oligodendrocyte precursor cells and altered myelination in optic nerve associated to retina degeneration in mice devoid of all thyroid hormone receptors. Proc Natl Acad Sci USA 99: 2907–2911
Ikeda A, Nishina PM, Naggert JK 2002 The tubby-like proteins, a family with roles in neuronal development and function. J Cell Sci 115: 9–14
Nguyen-Legros J, Versaux-Botteri C, Vigny A 1986 Early development of tyrosine hydroxylase-like and substance P-like immunoreactivity in the human fetal retina. Hum Neurobiol 5: 115–120
Rovet JF 1999 Congenital hypothyroidism: long-term outcome. Thyroid 9: 741–748
Man EB, Brown JF, Serunian SA 1991 Maternal hypothyroxinemia: psychoneurological deficits of progeny. Ann Clin Lab Sci 21: 227–239
Fisher DA, Klein AH 1981 Thyroid development and disorders of thyroid function in the newborn. N Engl J Med 304: 702–712
Chan S, Kachilele S, McCabe CJ, Tannahill LA, Boelaert K, Gittoes NJ, Visser TJ, Franklyn JA, Kilby MD 2002 Early expression of thyroid hormone deiodinases and receptors in human fetal cerebral cortex. Brain Res Dev Brain Res 138: 109–116
Calvo RM, Jauniaux E, Gulbis B, Asuncion M, Gervy C, Contempre B, Morreale de Escobar G 2002 Fetal tissues are exposed to biologically relevant free thyroxine concentrations during early phases of development. J Clin Endocrinol Metab 87: 1768–1777
Vulsma T, Gons MH, de Vijlder JJ 1989 Maternal-fetal transfer of thyroxine in congenital hypothyroidism due to a total organification defect or thyroid agenesis. N Engl J Med 321: 13–16
Burrow GN, Fisher DA, Larsen PR 1994 Maternal and fetal thyroid function. N Engl J Med 331: 1072–1078
Pop VJ, Kuijpens JL, van Baar AL, Verkerk G, van Son MM, de Vijlder JJ, Vulsma T, Wiersinga WM, Drexhage HA, Vader HL 1999 Low maternal free thyroxine concentrations during early pregnancy are associated with impaired psychomotor development in infancy. Clin Endocrinol (Oxf) 50: 149–155
Haddow JE, Palomaki GE, Allan WC, Williams JR, Knight GJ, Gagnon J, O'Heir CE, Mitchell ML, Hermos RJ, Waisbren SE, Faix JD, Klein RZ 1999 Maternal thyroid deficiency during pregnancy and subsequent neuropsychological development of the child. N Engl J Med 341: 549–555
Rovet J, Ehrlich R, Sorbara D 1987 Intellectual outcome in children with fetal hypothyroidism. J Pediatr 110: 700–704
Hanukoglu A, Perlman K, Shamis I, Brnjac L, Rovet J, Daneman D 2001 Relationship of etiology to treatment in congenital hypothyroidism. J Clin Endocrinol Metab 86: 186–191
Song SI, Daneman D, Rovet J 2001 The influence of etiology and treatment factors on intellectual outcome in congenital hypothyroidism. J Dev Behav Pediatr 22: 376–384
LaFranchi S 1999 Thyroid function in the preterm infant. Thyroid 9: 71–78
Rooman RP, Du Caju MV, De Beeck LO, Docx M, Van Reempts P, Van Acker KJ 1996 Low thyroxinaemia occurs in the majority of very preterm newborns. Eur J Pediatr 155: 211–215
Ares S, Escobar-Morreale HF, Quero J, Duran S, Presas MJ, Herruzo R, Morreale de Escobar G 1997 Neonatal hypothyroxinemia: effects of iodine intake and premature birth. J Clin Endocrinol Metab 82: 1704–1712
Reuss ML, Paneth N, Pinto-Martin JA, Lorenz JM, Susser M 1996 The relation of transient hypothyroxinemia in preterm infants to neurologic development at two years of age. N Engl J Med 334: 821–827
Lucas A, Morley R, Fewtrell MS 1996 Low triiodothyronine concentration in preterm infants and subsequent intelligence quotient (IQ) at 8 year follow up. BMJ 312: 1132–1133; discussion
Norcia AM, Tyler CW, Hamer RD 1990 Development of contrast sensitivity in the human infant. Vision Res 30: 1475–1486
Adams RJ, Courage ML 1990 Assessment of visual acuity in children with severe neurological impairments. J Pediatr Ophthalmol Strabismus 27: 185–189
Diamond A, Herzberg C 1996 Impaired sensitivity to visual contrast in children treated early and continuously for phenylketonuria. Brain 119: 523–538
Perron A, Westall CA, Mirabella G, Buncic JR, Logan WJ, Snead OC 2001 Contrast sensitivity changes in children prescribed the antiepileptic drug vigabatrin. Invest Ophthalmol Vis Sci 42: S388
Berghout A, Endert E, Ross A, Hogerzeil HV, Smits NJ, Wiersinga WM 1994 Thyroid function and thyroid size in normal pregnant women living in an iodine replete area. Clin Endocrinol (Oxf) 41: 375–379
Rovet J, Daneman D 2003 Congenital hypothyroidism: a review of current diagnostic and treatment practices in relation to neuropsychologic outcome. Paediatr Drugs 5: 141–149
Norcia AM, Tyler CW, Allen D 1986 Electrophysiological assessment of contrast sensitivity in human infants. Am J Optom Physiol Opt 63: 12–15
Harding GFA, Odom JV, Spileers W, Spekreijse H 1996 Standard for the visual evoked potential. Vision Res 36: 3567–3572
Norcia AM 2001 PowerDiva Manual (Version 1.5). Smith-Kettlewell Eye Research Institute, San Francisco, pp 2–31I
Norcia AM, Tyler CW, Hamer RD, Wesemann W 1989 Measurement of spatial contrast sensitivity with the swept contrast VEP. Vision Res 29: 627–637
Norcia AM, Tyler CW 1985 Spatial frequency sweep VEP: visual acuity during the first year of life. Vision Res 25: 1399–1408
Norcia AM, Tyler CW, Hamer RD 1988 High visual contrast sensitivity in the young human infant. Invest Ophthalmol Vis Sci 29: 44–49
Howell DC 1997 Simple analysis of variance. In: Statistical Methods for Psychology. Wadsworth Publishing Co, Scarborough, Canada, pp 275–323
Saunders KJ, Westall CA 1992 Comparison between near retinoscopy and cycloplegic retinoscopy in the refraction of infants and children. Optom Vis Sci 69: 615–622
Norcia AM, Tyler CW, Piecuch R, Clyman R, Grobstein J 1987 Visual acuity development in normal and abnormal preterm human infants. J Pediatr Ophthalmol Strabismus 24: 70–74
Regan D 1989 Basic research. In: Human Brain Electrophysiology: Evoked Potentials and Evoked Magnetic Fields in Science and Medicine. Elsevier Science Publishing Co, New York, pp 167–482
Johnson MH 2000 Functional brain development in infants: elements of an interactive specialization framework. Child Dev 71: 75–81
Braddick OJ, O'Brien JM, Wattam-Bell J, Atkinson J, Turner R 2000 Form and motion coherence activate independent, but not dorsal/ventral segregated, networks in the human brain. Curr Biol 10: 731–734
Acknowledgements
The work was obtained in partial fulfillment of G.M. doctoral thesis.
Portions of this paper were presented at conferences of the American Thyroid Association, September 2002, Los Angeles, CA; Association of Research in Vision and Ophthalmology, May 2002, Fort Lauderdale, FL; the International Society of Infant Studies, April 2004, Chicago, IL; the International Neuropsychology Society, February 2003, Honolulu, HI; Neurotoxicology, February 2004, Honolulu, HI.
We are indebted to Julie Cunningham for recruiting and scheduling the children and to Adena Perron, who assisted in testing. We also thank Dr. Wendy Wolfman, who allowed us to recruit control mothers through her obstetrics practice; Lori Brnjac, who recruited many of the children with CH; Dr. Michael Simone, from whom we obtained two of the CH cases; and the Motherisk Program at HSC, from which we recruited the hypothyroid women. We are also extremely grateful to Dr. Anthony Norcia and members of his laboratory, who provided the software as well as the direction and guidance in using the Power Diva System. Finally, we thank all of the mothers and their infants who so willingly participated in this research.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by a RESTRACOMP scholarship through the Research Institute of The Hospital for Sick Children (G.M.), an operating grant from the Canadian Institutes of Health Research (J.R.), and a National Science and Engineering Research Council postdoctoral fellowship (G.M.).
Rights and permissions
About this article
Cite this article
Mirabella, G., Westall, C., Asztalos, E. et al. Development of Contrast Sensitivity in Infants with Prenatal and Neonatal Thyroid Hormone Insufficiencies. Pediatr Res 57, 902–907 (2005). https://doi.org/10.1203/01.PDR.0000157681.38042.B4
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000157681.38042.B4
This article is cited by
-
Ocular morphology development and function in children with congenital hypothyroidism diagnosed by neonatal screening
Endocrine (2021)
-
Neurophysiologic evaluation of infants with congenital hypothyroidism before and after treatment
Acta Neurologica Belgica (2015)
-
Making sense with thyroid hormone—the role of T3 in auditory development
Nature Reviews Endocrinology (2013)
-
Paradoxical robust visual evoked potentials in young patients with cortical blindness
Documenta Ophthalmologica (2009)