Abstract
Defective or immature antibody responses to pathogens in children may explain the increased susceptibility to acute otitis media (AOM) in otitis-prone children. In literature, data on immunology have been based on studies of small groups of severely otitis-prone children and have not been consistent. Humoral immune status was assessed in 365 children, 1–7 years old, with two or more documented episodes of AOM in the previous year. Children with 4 or more episodes in the preceding year were defined as otitis-prone. Serum immunoglobulin levels were determined by radial immunodiffusion. Immunoglobulin levels of otitis-prone children were compared with those of children who had experienced 2-3 AOM episodes per year. Children with recurrent episodes of AOM were found to have normal or increased serum IgA, IgM, IgG, and IgG1 levels compared with normal values for age, whereas the serum IgG2 levels were mostly in the lower normal range. Twenty-two percent of all children showed IgG2 levels lower than 2 SD below the age-specific mean. Interestingly, the otitis-prone group of children showed significantly lower median and mean levels for all immunoglobulins compared with those children with only 2-3 previous AOM episodes. Lower immunoglobulin levels in otitis-prone children suggest a generalized decreased antibody response in otitis-prone children.
Similar content being viewed by others
Main
Based on the clinical observation that some children experience recurrent episodes of acute otitis media (AOM), the term “otitis-prone” was introduced by Howie (1). In general, the otitis-prone condition is defined as three or more episodes of AOM in 6 mo or four or more episodes in 12 mo; up to 5% of all children comply with this definition (2, 3).
With respect to immunoglobulin serum levels, both normal as well as stimulated serum IgA, IgM, IgG, and IgG1 levels have been reported in otitis-prone children aged 2 mo or older (4, 5). Freijd et al. and Sørensen et al. reported lower levels of IgG2 in children with recurrent AOM compared with age-matched controls (5, 6), but others did not confirm these observations (4, 7).
With respect to antibody activity against the two main bacterial pathogens in AOM Streptococcus pneumoniae and nontypeable Haemophilus influenzae (NTHI), subnormal or absent antibody responses have been reported in otitis-prone children (8–11), as well as decreased antibody responses upon immunization with Hib conjugate and rubella vaccine (12, 13).
These findings may suggest decreased antibody responses upon both T cell-dependent as well as T cell independent antigens in otitis-prone children (14). Hitherto, immunologic evaluations have been performed only in small groups of otitis-prone children. The need to obtain more substantial data led us to analyze immunoglobulins in a large group of 365 children with varying susceptibility to acute otitis media.
METHODS
This study was conducted in a general hospital (Spaarne Hospital Haarlem) and a tertiary care hospital (University Medical Center Utrecht), the Netherlands. The Medical Ethics Committees of both participating hospitals approved the design of the study. A signed informed consent was obtained from the parents or legal guardians of all children before evaluation.
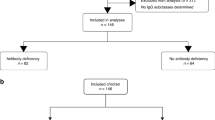
From April 1998 to February 2001, 365 children aged 1–7 y with 2 or more episodes of AOM in the previous year were included in the study. The number of previous AOM episodes was based both on parental report, with AOM defined as having one or more of the following symptoms: acute earache, new-onset otorrhea, irritability and fever, and on clinical confirmation of the diagnosis AOM by a physician. Patients with previously recognized congenital or acquired immunodeficiencies were excluded from the study.
Total serum immunoglobulin concentrations of IgA, IgM, and IgG as well as IgG1 and IgG2 subclass concentrations were determined by radial immunodiffusion (Behring Werke, Mannheim, Germany and Central Laboratory of the Red Cross Blood Transfusion Service, Amsterdam, The Netherlands). Serum immunoglobulin levels within the range of 2 SD below or above the age-specific mean were considered normal (15, 16). Total deficiency of IgA was defined as a serum level of less than ≤0.05 g/L. Total deficiency of IgG2 was defined as a serum level less than ≤0.02 g/L. To address the question whether otitis-prone children are immunologically different from children with fewer episodes of AOM, the children were divided in two groups: 231 otitis-prone children with 4 or more AOM episodes in the preceding year and 134 children with 2–3 AOM episodes in the preceding year.
Statistics.
Differences in the number of children with low serum immunoglobulin levels according to age (12–24 mo versus 25–84 mo) were analyzed using χ2 tests or Fisher exact tests when appropriate. Differences between mean immunoglobulin levels between children with 2–3 AOM and children with 4 or more episodes were analyzed with t test for independent samples or the Mann-Whitney U test when appropriate. Group differences were considered statistically significant at p < 0.05. Linear regression modeling was used to analyze the potential effect of age differences on immunoglobulin levels.
RESULTS
Table 1 provides general characteristics for all children. The median age of the total group of children was just above 2 y.
Serum concentrations of IgA, IgM, IgG, IgG1, and IgG2 according to age for the whole group of children are illustrated in Fig. 1. The IgA, IgM, IgG, and IgG1 levels were generally in the high-normal range or higher than 2 SD above the age-specific mean. In contrast, the IgG2 levels were mostly in the low-normal range and 22.5% of all children showed IgG2 levels lower than 2 SD below the age-specific mean. Table 2 shows the number of children with low immunoglobulin levels (<2 SD below the age-specific mean) according to different age groups. In children aged 12 to 24 mo significantly higher percentages of children with low serum levels of IgA (18.3%versus 7.1%, p = 0.001) and IgG2 (32.7%versus 15.1%, p = 0.001) were found compared with older children.
Total IgA deficiency was found in 3 children with 2–3 previous AOM episodes and 2 children with 4 or more AOM episodes. In contrast, the nine children with absent IgG2 serum levels all belonged to the group with 4 or more AOM episodes. These children with total IgG2 deficiency suffered from significantly more recurrent AOM episodes per year compared with the whole group of children with subnormal or normal IgG2 serum levels (8.00 and 4.97 episodes, respectively; p = 0.003).
Table 3 shows the mean total serum levels of IgA, IgM, IgG, IgG1, and IgG2 now according to number of AOM episodes in the previous year. Levels of serum immunoglobulins in otitis-prone children with 4 or more AOM episodes were significantly lower than in children with 2–3 previous AOM episodes. These differences in the serum immunoglobulin levels were not influenced by differences in age according to linear regression analyses.
DISCUSSION
In this large group of 365 children aged 1–7 y with recurrent AOM episodes, in general normal or stimulated levels of IgG, IgM, IgA, and IgG1 were found, whereas IgG2 levels proved to be in the lower normal range or depressed compared with normal control values. Markedly, 32.7% of the children aged 12–24 mo showed IgG2 levels lower than 2 SD below the age-specific mean. Most probably, due to spontaneous recovery of IgG2 levels this percentage was statistically significantly lower in older children but still impressive with 15.1%, suggesting a specific role for IgG2 in susceptibility to AOM. A higher percentage of low IgA levels was only found in the youngest group of children aged 12 to 24 mo (18.3%), at older age this percentage nearly normalized (7.1%).
IgG2 may be important in the defense against otitis pathogens like S. pneumoniae. Effective host defense against S. pneumoniae depends primarily on opsonizing antibodies against the capsular polysaccharides. In adults, pneumococcal anticapsular antibodies reside primarily in the IgG2 subclass. Our finding of low IgG2 antibody levels in children with recurrent AOM is in agreement with a previous report of otitis-prone children at 30 mo of age, who showed lower IgG2 anti-pneumococcal antibody levels compared with healthy age-matched children and adults. In contrast to IgG2, in the same report the IgG1 anti-pneumococcal antibody levels in the otitis-prone group of children were even higher than those in adults (17). Also after vaccination with pneumococcal polysaccharide vaccine low to absent IgG2 anti-pneumococcal antibody responses were observed in otitis-prone children (10). Some in vitro data showed effective phagocytosis of pneumococci to be primarily related to IgG2 anti-pneumococcal antibodies (18–20). This dependency on IgG2 antibodies may also be reflected in the low expression of FcγRIIaH131, the Fc receptor for IgG2 on effector cells, in patients with recurrent respiratory tract infections, or bacteremic pneumonia (21, 22). Our findings support the hypothesis that clinical protection against mucosal infections like AOM depends more on IgG2 levels, and not on IgG1. In addition to the relative IgG2 immunodeficiency found in our population, overall serum immunoglobulin levels were lower in children with 4 or more AOM episodes compared with children with 2–3 AOM episodes per year. It should be noted that suffering from 2–3 AOM episodes in the first years of life is not comparable to suffering from 2–3 episodes at the age of 4 to 7 y. These older children with 2–3 AOM episodes per year might also be regarded as otitis-prone. This is reflected in the fact that at the age of 2 to 4 y children with 4 or more AOM episodes show decreased IgA, IgM, and IgG2 levels compared with children with 2–3 AOM episodes. In children aged 4 to 7 y no significant differences in any of the immunoglobulin isotypes existed anymore between children with 2–3 AOM episodes per year and 4 or more (data not shown). Low serum immunoglobulin levels may indicate decreased antibody responses despite recurrent infections. Normally, recurrent infections induce high antibody levels due to repeated stimulation as for example in patients with cystic fibrosis or defective granulocyte functions. In otitis-prone children the observed humoral hyporesponsiveness may be one of the causes of the ongoing susceptibility to AOM pathogens. This hypothesis is supported by the fact that, apart from absent or low responses toward T-cell independent pneumococcal polysaccharides antigens, diminished responses toward protein (T cell dependent) antigens are also observed in otitis-prone children. Hotomi at al. demonstrated that 11 of 20 otitis-prone children older than 18 mo exhibited reduced anti-P6-IgG antibody levels to NTHI compared with healthy age matched controls despite repeated infections with NTHI (11). P6 is one of the six outer membrane proteins of NTHI. Furthermore, decreased responses to T cell independent polysaccharide Hib vaccine, as well as polysaccharide protein Hib conjugate vaccine were observed in children aged 22 to 158 mo with a history of recurrent respiratory tract infections and with normal IgG subclasses (12) Finally, 13 children with recurrent AOM showed a significantly lower antibody response to the viral rubella vaccine than did 29 children without AOM (13).
Immune responses to infectious agents are regulated by immune effector and cytokine producing cells. The cytokines IL-1, IL-6 and tumor necrosis factor-alpha (TNF-alpha) are glycoproteins produced by different cell types when exposed to bacteria and viruses (23). These cytokines trigger acute phase responses and induce proliferation and differentiation of T and B cells. One study showed children with recurrent AOM episodes to produce significantly lower nasopharyngeal IL-1β, IL-6 and TNF-alpha in nasopharyngeal secretions upon colonization with Haemophilus influenzae than healthy children (24). Such a local defect in cytokine production could contribute to the defective immune reactivity in otitis prone children (25).
CONCLUSION
In conclusion, a relative high percentage of low IgG2 levels is found in children with recurrent otitis media. In the youngest children, many also show low IgA levels, but this disappears at older age. Otitis prone children in general show lower total IgM, IgA, IgG, IgG1, and IgG2 levels compared with those with fewer episodes of AOM.
Abbreviations
- AOM:
-
acute otitis media
- NTHI:
-
nontypeable Haemophilus influenzae
References
Howie VM, Plouss JH, Sloyer J 1975 The “otitis-prone” condition. Am J Dis Child 129: 67–68
Dowell SF, Marcy MS, Philips WR, Gerber MA, Schwartz B 1998 Otitis media-principles of judicious use of antimicrobial agents. Pediatrics 101: 165–171
Alho OP, Koivu M, Sorri M 1991 What is an ‘otitis-prone' child?. Int J Pediatr Otorhinolaryngol 21: 201–209
Berman S, Lee B, Nuss R, Roark R, Giclas PC 1992 Immunoglobulin G, total and subclass, in children with or without recurrent otitis media. J Pediatr 121: 249–251
Sørensen CH, Nielsen LK 1988 Plasma IgG, IgG subclasses and acute-phase proteins in children with recurrent acute otitis media. APMIS 96: 676–680
Freijd A, Oxelius VA, Rynnel-Dagoo B 1985 A prospective study demonstrating an association between plasma IgG2 concentrations and susceptibility to otitis media in children. Scand J Infect Dis 17: 115–120
Jørgensen F, Andersson B, Hanson LA 1990 Gamma-globulin treatment of recurrent acute otitis media in children. Pediatr Infect Dis J 9: 389–394
Prellner K, Kalm O, Karup Pedersen F 1986 Pneumococcal antibodies and complement during and after periods of recurrent otitis. Acta Otolaryngol 101: 467–474
Gross S, Blaiss MS, Herrod HG 1992 Role of immunoglobulin subclasses and specific antibody determinations in the evaluation of recurrent infection in children. J Pediatr 121: 516–522
Sanders EAM, Rijkers GT, Tenbergen-Meekes AM, Voorhorst-Ogink MM, Zegers BJ 1995 Immunoglobulin isotype specific antibody responses to pneumococcal polysaccharide vaccine in patients with recurrent respiratory tract infections. Pediatr Res 37: 812–817
Hotomi M, Yamanaka N, Saito T, Shimada J, Suzumoto M, Suetake M, Faden H 1999 Antibody responses to the outer membrane protein P6 of nontypeable Haemophilus influenzae and pneumococcal capsular polysaccharides in otitis-prone children. Acta Otolaryngol 119: 703–707
Herrod HG, Gross S, Insel R 1989 Selective antibody deficiency to Haemophilus influenzae type B capsular polysaccharide vaccination in children with recurrent respiratory tract infection. J Clin Immunol 9: 429–434
Prellner K, Harsten G, Lofgren B, Christenson B, Heldrup J 1990 Responses to rubella, tetanus, and diphtheria vaccines in otitis-prone and non-otitis-prone children. Ann Otol Rhinol Laryngol 99: 628–632
Yamanaka N, Hotomi M, Shimada J, Togawa A 1997 Immunological deficiency in “otitis-prone” children. Ann N Y Acad Sci 830: 70–81
Van der Giessen M, Rossouw E, van Veen TA, van Loghum E, Zegers BJ, Sander PC 1975 Quantification of IgG subclasses in sera of normal adults and healthy children between 4 and 12 years of age. Clin Exp Immunol 21: 501–509
Vlug A, Nieuwenhuys EJ, van Eijk RV, Geertzen HG, van Houte AJ 1994 Nephelometric measurements of human IgG subclasses and their reference ranges. Ann Biol Clin (Paris) 52: 561–567
Freijd A, Hämmarström L, Persson MAA, Smith CI 1984 Plasma anti-pneumococcal antibody activity of the IgG class and subclasses in otitis prone children. Clin Exp Immunol 56: 233–238
Lortan JE, Kaniuk AS, Monteil MA 1993 Relationship of in vitro phagocytosis of serotype 14 Streptococcus pneumoniae to specific class and IgG subclass antibody levels in healthy adults. Clin Exp Immunol 91: 54–57
Rodriguez ME, Pol van de WL, Sanders EAM, Winkel van de JGJ 1999 Crucial role of FcγRIIa (CD32) in assessment of functional anti-S pneumoniae antibody activity in human sera. J Infect Dis 179: 423–433
Jansen WT, Breukels MA, Snippe H, Sanders EAM, Verheul AF, Rijkers GT 1999 Fcγreceptor polymorphisms determine the magnitude of vitro phagocytosis of Streptococcus pneumoniae mediated by pneumococcal conjugate sera. J Infect Dis 180: 888–891
Sanders EAM, Van de Winkel JG, Rijkers GT, Voorhorst-Ogink MM, de Haas M, Capel PJ, Zegers BJ 1994 Fcγreceptor IIa (CD32) heterogeneity in patients with recurrent bacterial respiratory tract infections. J Infect Dis 170: 854–861
Yee AM, Phan HM, Zuniga R, Salmon JE, Musher DM 2000 Association between FcγRIIa-R131 allotype and bacteremic pneumococcal pneumonia. Clin Infect Dis 30: 25–28
Waage A, Halstensen A, Shalaby R, Brandtzaeg P, Kierulf P, Espevik T 1989 Local production of tumor necrosis factor alfa, interleukin 1, and interleukin 6 in meningococcal meningitis. Relation to the inflammatory response. J Exp Med 170: 1859–1867
Lindberg K, Rynnel-Dagöö B, Sundqvist KG 1994 Cytokines in nasopharyngeal secretions; evidence for defective IL-1beta production in children with recurrent episodes of acute otitis media. Clin Exp Immunol 97: 396–402
Rynnel-Dagöö B, Ågren 2001 The nasopharynx and the middle ear. Inflammatory reactions in middle ear disease. Vaccine 19: S26–31
Author information
Authors and Affiliations
Corresponding author
Additional information
This study is supported by grants from Zon Mw, the Netherlands Organization for Health, Research and Development, and the Health Insurance Company Zilveren Kruis–Achmea.
Rights and permissions
About this article
Cite this article
Veenhoven, R., Rijkers, G., Schilder, A. et al. Immunoglobulins in Otitis-Prone Children. Pediatr Res 55, 159–162 (2004). https://doi.org/10.1203/01.PDR.0000099776.66136.39
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000099776.66136.39
This article is cited by
-
Otitis Media in Children with Congenital Immunodeficiencies
Current Allergy and Asthma Reports (2010)
-
Otitis media as a presenting complaint in childhood immunodeficiency diseases
Current Allergy and Asthma Reports (2008)
-
Study of nasopharyngeal bacterial flora. Variations in nasopharyngeal bacterial flora in schoolchildren and adults when administered antimicrobial agents
Journal of Infection and Chemotherapy (2007)
-
Immunological Status in the Aetiology of Recurrent Otitis Media with Effusion: Serum Immunoglobulin Levels, Functional Mannose-Binding Lectin and Fc Receptor Polymorphisms for IgG
Journal of Clinical Immunology (2005)
-
Immunologic screening of children with recurrent otitis media
Current Allergy and Asthma Reports (2005)