Abstract
Perinatal hypoxia-ischemia remains a significant cause of neonatal mortality and neurodevelopmental disability. Numerous lines of evidence indicate that cerebral ischemic insults disrupt normal respiratory activity in mitochondria. Carnitine (3-hydroxy-4-N-trimethylammonium-butyrate) has an essential role in fatty acid transport in the mitochondrion and in modulating potentially toxic acyl-CoA levels in the mitochondrial matrix. There are no naturally occurring esterases available to reduce the accumulation of acyl-CoA but this process can be overcome by exogenous carnitine. We used a newborn rat model of perinatal hypoxia-ischemia to test the hypothesis that treatment with l-carnitine would reduce the neuropathologic injury resulting from hypoxia-ischemia in the developing brain. We found that treatment with l-carnitine during hypoxia-ischemia reduces neurologic injury in the immature rat after both a 7- and 28-d recovery period. We saw no neuroprotective effect when l-carnitine was administered after hypoxia-ischemia. Treatment with d-carnitine resulted in an increase in mortality during hypoxia-ischemia. Carnitine is easy to administer, has low toxicity, and is routinely used in neonates as well as children with epilepsy, cardiomyopathy, and inborn errors of metabolism. l-Carnitine merits further investigation as a treatment modality for the asphyxiated newborn or as prophylaxis for the at-risk fetus or newborn.
Similar content being viewed by others
Main
Hypoxic-ischemic injury in the developing brain is characterized by a cascade of cellular events that evolve for hours or days, a distinct clinical syndrome manifest as encephalopathy, a combination of ischemia superimposed on hypoxia, and specific regional brain vulnerability to injury (1–3). Cerebral ischemia in the adult (4) and hypoxia-ischemia in the newborn (5) disrupt mitochondrial function leading to a collapse in cell energy metabolism.
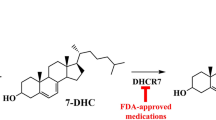
The amino acid derivative carnitine (3-hydroxy-4-N-trimethylammonium-butyrate) is required for the maintenance of normal mitochondrial function. Carnitine has three major functions: facilitating transport of acyl moieties between organs and across the mitochondrial inner membrane and the buffering of potentially toxic intracellular acyl-CoA moieties (6, 7). High levels of acyl-CoA esters impair numerous mitochondrial processes (Fig. 1) (8–10). There are no endogenous esterases available to reduce the accumulation of acyl-CoA esters. This process can be overcome by the addition of exogenous carnitine. Carnitine may function therefore in acute metabolic crises to trap toxic acyl-CoA moieties that impair fatty acid oxidation, urea cycle function metabolism, and gluconeogenesis (6, 7, 11).
Acyl-CoA moieties accumulate during ischemia or metabolic stress and inhibit multiple enzymes (shown by bars). This inhibition blocks the citrate and urea cycles, glycolysis, gluconeogenesis, and fatty acid and protein catabolism. Mitochondrial oxidative phosphorylation is reduced. These acyl-CoA effects serve important regulatory roles during normal metabolism. Exogenous carnitine reduces the toxicity resulting from excess acyl-CoA by lowering acyl-CoA levels. PEP, phosphoenolpyruvate.
Carnitine has been tested as a neuroprotective therapy in adult animal models of cerebral ischemia (12–14). However, there are no data directly addressing the effect of l-carnitine treatment on cerebral ischemic injury in the newborn. l-Carnitine is potentially an attractive therapeutic modality for perinatal asphyxia given the extensive pediatric clinical experience with the use of this drug in epilepsy, inborn errors of metabolism, cardiomyopathy, and apnea of prematurity (15–18). Accordingly, we used a rodent model of perinatal cerebral hypoxia-ischemia (19) to test the hypothesis that treatment with l-carnitine would reduce the neuropathologic injury resulting from hypoxia-ischemia in the developing brain.
METHODS
Animal protocols.
All experiments were performed in accordance with the relevant National Institutes of Health guidelines. All experimental procedures were approved by the Institutional Animal Care and Use Committee of Northwestern University, Chicago, IL, U.S.A. Pups were housed with their dam in cages in the animal facility with a 12-h light/dark cycle.
Induction of hypoxia-ischemia in the newborn rat.
We induced hypoxic-ischemic injury in P7 rats using the well-characterized method (19) of unilateral carotid ligation followed by hypoxia (20, 21) This age is approximately equivalent to the 34-wk gestation human infant (22). Male and female Wistar rats at P7 were removed from the mother and anesthetized with halothane (3.5% for induction and 1.5% for maintenance) and 50% oxygen–balance nitrogen delivered via face mask. The right common carotid artery was identified and gently separated from the vagus nerve. The vessel was ligated with double 6-0 silk sutures to ensure cessation of blood flow. The entire procedure including time for the induction of anesthesia was completed in less than 6 min. After carotid ligation, the animals were allowed to recover in a warm environment for 15 min, then returned to the dam for a further 90 min at an ambient temperature of 21°C. Induction of hypoxia was performed in custom-built Plexiglas chambers based on published methods (23, 24). The device comprises six interconnected Plexiglas chambers (440 mL) submerged in water warmed to 37.5°C. Each chamber received prewarmed, humidified hypoxia gas (8% oxygen–balance nitrogen) in a commercially calibrated preparation at a rate of 100 mL/min regulated by flowmeter. After 70 min of hypoxia, the pups were allowed to recover in room air for 15 min before being returned to the dam. Sham-operated animals underwent neck incision and vessel manipulation without ligation or hypoxia. This procedure produces selective brain injury in P7 rat pups in the hemisphere ipsilateral to the carotid occlusion. Hypoxia alone (control, contralateral hemisphere) does not result in any brain damage (19).
Temperature recording.
Cerebral temperature is a critical determinant of neurologic injury after ischemic brain injury (25). We measured rectal temperatures in P7 rat pups subjected to hypoxia-ischemia and treated with l-carnitine or vehicle. A rodent rectal thermocouple probe (IT-18; Physitemp Instruments, Clifton, NJ, U.S.A.) was used to record temperatures at four times after carotid ligation: before hypoxia, at the conclusion of hypoxia, 1 h after the conclusion of hypoxia, and 2 h after the conclusion of hypoxia.
Drug administration.
l- and d-Carnitine were obtained from Sigma Chemical Co (St. Louis, MO, U.S.A.). Carnitine isomers were dissolved in saline solution and pH adjusted to 7.4. Each salt was prepared as a 1.2 M solution and administered via i.p. injection at a dose of 16 mmol/kg. This dose has been shown to double the concentration of carnitine in rat brains 1 h after administration and nearly quadruple the concentration by 24 h (26). Five experimental groups of P7 rats were prepared. In group 1, animals underwent unilateral carotid ligation followed by a 1-h recovery period. l-Carnitine or vehicle was administered as a single i.p. injection 30 min before the induction of hypoxia. The animals were killed after a 7-d recovery period. In group 2, animals were treated as in group 1 but allowed to recover for 28 d. In group 3, l-carnitine or vehicle was administered 1 h after the conclusion of hypoxia-ischemia, then followed by a 1-wk recovery. In group 4, l-carnitine or vehicle was administered 4 h after the conclusion of hypoxia-ischemia, then followed by a 1-wk recovery period. To determine the pharmacologic specificity of any neuroprotective effect observed with l-carnitine, we also investigated the effect of d-carnitine on outcome after hypoxia-ischemia. In these studies (group 5), d-carnitine (16 mmol/kg) or vehicle was administered after carotid ligation as a single i.p. injection 30 min before the induction of hypoxia.
Measurement of hemispheric weight.
The comparison of disparities in hemispheric weight as a valid outcome measure of neurologic injury in the newborn rat has been demonstrated in studies correlating changes in hemispheric weight after hypoxia-ischemia with other measures of brain injury (20, 23, 27, 28). The contralateral (nonischemic) cerebral hemisphere is used as an internal control, the size of which is comparable to that of an age-matched brain not subjected to unilateral hypoxia-ischemia (29). This method allows time for the reduction in the initial cerebral edema and the evolution of clearly detectable infarcts (30).
Animals were killed after either 7 or 28 d of recovery from hypoxia-ischemia (P14 and P35, respectively). Animals were killed by halothane overdose, and the brain was removed and placed in chilled saline. The cerebellum, olfactory lobes, and hindbrain were removed, and the hemispheres were sectioned at the midline. Left and right hemispheric weights were obtained to the nearest 0.1-mg using a high-precision balance (Mettler Instruments, Mettler-Toledo, Inc., Columbus, OH, U.S.A.). Differences in weight between the hypoxic-ischemic and control contralateral hemisphere were calculated for each animal both directly and using the following formula:

where I represents the weight of the ipsilateral hemisphere and C is the weight of the contralateral hemisphere.
Tissue processing for immunofluorescence.
Rats were deeply anesthetized, the descending aorta was clamped, and the animal was perfused through the left ventricle with PBS, pH 7.4, followed by 4% ice-cold paraformaldehyde (Electron Microscopy Sciences, Washington, PA, U.S.A.). Brains were removed and placed in paraformaldehyde containing 20% sucrose overnight at 4°C. After fixation, the tissue was dehydrated in graded alcohol solutions, cleared with xylene, and infiltrated with paraffin overnight. Sections were cut at a thickness of 10 μm on a microtome. The anterior commissure was used as a landmark to match sections across experiments. To confirm that the protection from hypoxic-ischemic injury afforded by l-carnitine treatment was associated with a reduction in neuronal injury, four serial coronal sections posterior to the anterior commissure were examined from five animals without evidence of injury (as determined by hemisphere weight) after treatment with l-carnitine. This group was compared with identical coronal sections obtained from vehicle-treated animals with evidence of brain injury shown by a reduction in ipsilateral hemisphere weight.
Immunofluorescence detection of dead neurons.
The fluorescent marker FJ-B (Histo-Chem Inc, Jefferson AR, U.S.A.) was used to identify dead and degenerating neurons (31) in paraffin-embedded tissue sections using modifications of published techniques. The dye has an emission peak at 450 nm and an excitation peak at 530 nm. FJ-B fluorescence can be visualized using an FITC filter that results in a green emission color. Paraffin-embedded sections were washed three times in xylene followed by immersion in absolute and 95% alcohol. The deparaffinized tissue was then immersed in a solution containing 1% sodium hydroxide in 80% alcohol for 5 min, followed by two 1-min washes in 70% alcohol and distilled water. The slides were then transferred to a solution of 0.06% potassium permanganate for 10 min and gently agitated at room temperature. The FJ-B dye was applied as a freshly made (from stock solution) 0.0004% solution in 0.1% acetic acid. After 20 min in the staining solution, the slides were washed three times with distilled water, dried at 50°C for 15 min, and coverslipped with DPX mounting media (Sigma Chemical Co). To visualize both viable cells and degenerating neurons on the same section, the fluorescent Nissl counterstain 4′,6-diamidino-2-phenylindole dihydrochloride (Sigma Chemical Co) was included (0.0002% concentration) in the FJ-B staining solution.
Blood gas analysis.
Mixed arterial and venous blood samples after decapitation were analyzed using a portable blood gas analyzer (I-Stat; I-Stat Corporation, Windsor, NJ, U.S.A.). Samples were obtained at two times after carotid ligation: 30 min before hypoxia; and at the conclusion of hypoxia.
Data analysis.
All data are expressed as mean ± SEM. The degree of hypoxic-ischemic brain injury after treatment with l- or d-carnitine or saline was expressed as the percentage of reduction in the tissue weight of the hemisphere ipsilateral to carotid ligation. This was calculated as a ratio of the right (ipsilateral, ischemic) to the left (contralateral, nonischemic) hemispheric weights as described previously (23). Physiologic values and the percent reduction in hemispheric weights were compared by one-way ANOVA (StatView 5.0; SAS Institute, Cary, NC, U.S.A.). The Mann-Whitney test was used to determine significance for nonparametric data. Statistical significance was assumed when p < 0.05.
RESULTS
l-Carnitine treatment reduces neurologic injury after hypoxia-ischemia.
Animals in group 1 (treatment with 16 mmol/kg l-carnitine 30 min before hypoxia) showed significantly less neurologic injury (Fig. 2A) after a 7-d recovery period. Animals treated with vehicle showed a 20.9 ± 2.6% (n = 37) reduction (data expressed as mean percent hemisphere weight loss ± SEM) in the weight of the injured hemisphere. In contrast, animals treated with l-carnitine before hypoxia showed a hemispheric weight reduction of 6.8 ± 2.4% (n = 30) which was significantly different from that measured in the vehicle-treated group (p < 0.05). The weight of the ischemic hemisphere in the vehicle-treated animals was 0.3072 ± 0.0128 g compared with 0.3637 ± 0.0097 g in the carnitine-treated animals (p < 0.05). There was no significant difference in the weight of the nonischemic (left) hemisphere between vehicle-treated (0.3857 ± 0.0057 g) and carnitine-treated (0.3919 ± 0.0064 g) animals.
Percent reduction in ipsilateral hemisphere weight after 7- (A) and 28- (B) d recovery from hypoxia-ischemia on P7. A, L-carnitine confers protection from hypoxic-ischemic brain injury in newborn rat brain after 7-d recovery. The percent reduction in ipsilateral hemisphere weight in the carnitine-treatment group was 6.8 ± 2.4% (n = 30) compared with 20.9 ± 2.6% in the vehicle-treated group (n = 37). B, treatment with L-carnitine confers sustained protection after 28-d recovery from hypoxic-ischemic brain injury. The percent reduction in ipsilateral hemisphere weight in the carnitine-treatment group was 4.9 ± 3.5% (n = 9) compared with 24.9 ± 6.5% in the vehicle-treated group (n = 15). *p < 0.05, L-carnitine vs vehicle.
l-Carnitine-mediated reduction in neurologic injury is sustained after 4 wk of recovery.
We next sought to determine whether the neuroprotection afforded by l-carnitine treatment observed after 7-d recovery was sustained (Fig. 2B) in a longer-term recovery model (group 2). We allowed these animals to recover for 28 d (to P35) and then quantified neurologic injury using hemispheric weight as the outcome measure as described above. Animals treated with vehicle showed a persistent reduction in ipsilateral hemisphere weight of 24.9 ± 6.5% (n = 15). The animals treated with l-carnitine before hypoxia showed a hemispheric weight reduction of 4.9 ± 3.5% (n = 9), which was again a significant difference from the vehicle-treated group (p < 0.05). The weight of the ischemic hemisphere in the vehicle-treated animals was 0.4171 ± 0.0385 g compared with 0.5253 ± 0.0165 g (p < 0.05) in the carnitine-treated animals. There was no significant difference in the weight of the nonischemic (left) hemisphere between vehicle-treated (0.5534 ± 0.0099 g) and carnitine-treated (0.5560 ± 0.0187 g) animals.
l-Carnitine treatment reduces neuronal death after hypoxia-ischemia.
The fluorescent dye FJ-B (31) identifies dead neurons. We did not detect FJ-B labeled cells in either the cortex (Fig. 3B) or hippocampus (Fig. 3D) of l-carnitine treated animals. In contrast, vehicle-treated animals showed FJ-B–positive neurons both in the cortex (Fig. 3A) and the hippocampal neuronal layer (Fig. 3C).
FJ-B fluorescent labeling of dead neurons in cortex (A and B) and hippocampus (C and D) from representative coronal sections of hypoxic-ischemic P7 rats treated with L-carnitine (B and D) or vehicle (A and C). Counterstain (blue) is 4′,6-diamidino-2-phenylindole dihydrochloride. Note the FJ-B fluorescent neurons in cortex (A) and hippocampus (C) of vehicle-treated animals, which are not present in the animals treated with L-carnitine (B and D). Arrows identify dead (green) neurons. Bar, 100 μm (A, B); 25 μm (C, D).
l-Carnitine does not reduce neurologic injury when administered after hypoxia-ischemia.
The effect of potential neuroprotective therapies is critically dependent on the timing of treatment with respect to the initial insult (32). Therefore, we next examined whether l-carnitine reduced neurologic injury when administered 1 h (group 3) after the completion of hypoxia-ischemia on P7. The percent reduction in ipsilateral hemisphere weight in the l-carnitine-treated animals treated 1 h after the completion of hypoxia-ischemia (Fig. 4A) showed no significant protection (28.1 ± 3.5%; n = 13) compared with the vehicle-treated animals (32.4 ± 5.4%; n = 10). The weight of the ischemic hemisphere in the vehicle-treated animals in group 3 was 0.2986 ± 0.0187 g compared with 0.2653 ± 0.0154 g in the carnitine-treated animals. When we further delayed l-carnitine treatment (group 4) until 4 h after ligation (Fig. 4B), there was no protection. Hemispheric weight differences were 24.9 ± 9.2% (n = 5) and 32.9 ± 8.5% (n = 6) in vehicle and l-carnitine-treated pups, respectively. The weight of the ischemic hemisphere in the vehicle-treated animals in group 4 was 0.3142 ± 0.0309 g compared with 0.2431 ± 0.0304 g in the carnitine-treated animals.
Treatment with L-carnitine 1 h (A) or 4 h (B) after the conclusion of hypoxia-ischemia does not reduce neurologic injury after 7-d recovery. A, percent reduction in ipsilateral hemisphere weight in the carnitine-treatment group was 28.1 ± 3.5% (n = 13) compared with 32.4 ± 5.4% in the vehicle-treated group (n = 10). B, percent reduction in ipsilateral hemisphere weight in the carnitine-treatment group was 32.9 ± 8.5% (n = 6) compared with 24.9 ± 9.2% in the vehicle-treated group (n = 5). Brain injury in the L-carnitine-treated animals was not significantly different from that measured in the control littermates injected with vehicle.
l-Carnitine does not affect core temperature during hypoxia-ischemia.
l-Carnitine did not affect the core temperature during hypoxia-ischemia on P7 (Table 1) with an ambient room temperature of 21°C. At the start of hypoxia (30 min after drug administration), core temperature was 32.00 ± 0.19°C in the vehicle-treated animals (data expressed as mean ± SEM). This was not significantly different from the temperature measured (31.77° ± 0.16°C) in the l-carnitine-treated animals (n = 35 per group). Core temperatures in the l-carnitine-treated animals 1 h after hypoxia-ischemia were 31.20° ± 0.36°C (n = 21) and 2 h after hypoxia-ischemia were 30.45° ± 0.35°C (n = 17). These values were not significantly different from those obtained in the vehicle-treated animals at 1 h (31.29° ± 0.38°C; n = 21) and 2 h (30.81° ± 0.31°C; n = 17) of recovery.
l-Carnitine does not affect blood gas values during hypoxia-ischemia.
To determine the effect of treatment with l-carnitine on acid-base status during hypoxia-ischemia, we measured mixed venous blood gas values at different times during the procedure. We analyzed samples from animals treated with l-carnitine or vehicle after carotid ligation, 30 min before the start of hypoxia, and at the conclusion of 70 min of hypoxia (Table 2). The values in the l-carnitine-treated animals at the conclusion of hypoxia show a considerable metabolic acidosis (base deficit, 12.0 ± 1.1 mM) and hyperventilation (Pco2, 19.7 ± 1.0 mm Hg) at the end of the hypoxic exposure. There was no statistically significant difference at either point between the animals treated with l-carnitine and those treated with vehicle.
d-Carnitine increases mortality during hypoxia-ischemia.
d-Carnitine treatment after carotid ligation resulted in a profound increase in mortality (Fig. 5). Death occurred quickly. Of 21 P7 animals treated with d-carnitine 30 min before starting hypoxia, two died before the induction of hypoxia, 15 died during hypoxia, and only four survived to P14, representing a total mortality of 81%.
Treatment with d-carnitine during hypoxia-ischemia decreases survival. P7 rats underwent carotid ligation before receiving a single i.p. injection of vehicle (n = 20) or 16 mmol/kg d-carnitine (n = 21) 30 min before the induction of hypoxia. Graph shows the percentage of animals surviving at each time after injection. Note the marked increase in percent mortality of d-carnitine-treated animals at the start (10%) and conclusion of hypoxia (71%) compared with vehicle-treated animals. Arrows identify the start and conclusion of hypoxia.
DISCUSSION
The principal finding of this study is the observation that l-carnitine significantly reduces the severity of pathologic injury resulting from hypoxia-ischemia in the immature rat. Treatment with 16 mmol/kg l-carnitine reduces the neuropathologic injury associated with hypoxia-ischemia whether observed after a 7- or 28-d recovery period. The same treatment does not reduce the severity of injury when administered either 1 or 4 h after the conclusion of hypoxia-ischemia. The protective effect of l-carnitine is not associated with changes in temperature or reduction of metabolic acidosis. The administration of d-carnitine during hypoxia-ischemia is associated with a significant acute increase in mortality.
Carnitine treatment may address the earliest irreversible events in a hypoxic-ischemic insult. We hypothesize that high acyl-CoA levels develop within mitochondria because the downstream metabolism of acyl-CoA is inhibited during ischemic or hypoxic-ischemic insults. The accumulation of acyl-CoA results in a metabolic conundrum from which the mitochondrion cannot recover. Such high acyl-CoA levels produce a feed-forward inhibition of their own metabolism and inhibit multiple other key enzymatic processes (6–11). We hypothesize that this conundrum may be the earliest and a cardinal irreversible event in ischemia. The capacity to reduce toxic levels of acyl-CoA esters within the compromised mitochondrion is dependent on carnitine acyltransferases and endogenous carnitine (Fig. 1). This process for restoration of normal mitochondrial function appears normally limited by available carnitine. We hypothesize that the administration of exogenous carnitine during hypoxia-ischemia, as provided to our treated animals (Fig. 2), enables a reduction in the levels of excess mitochondrial acyl-CoA and thereby overcomes the acyl-CoA–mediated blockade of normal mitochondrial metabolism. The relevance of this mechanism of carnitine rescue has been demonstrated in other experiments (33) documenting the relevance of carnitine in reducing intramitochondrial acyl-CoA esters and restoring oxidative phosphorylation.
The identification of energy failure within the mitochondrion as a valid treatment target in ischemic injury has substantial precedent (34, 35). The significance of the finding that l-carnitine affords neuroprotection in the newborn rat hypoxia-ischemia model derives in part from the fact that carnitine may ameliorate pathologic events within the mitochondrion that occur early after hypoxia-ischemia. Damage during cerebral ischemia results from oxygen free radicals and nitric oxide and its metabolites (4, 5). These are critical events in the pathways leading to cell death but occur subsequent to the mitochondrial processes restored by the administration of carnitine. Treatment strategies targeted solely at these later events have had limited success in human clinical trials, emphasizing the potential importance of therapies that address the early events in the disruption of mitochondrial functioning. These latter events would not be reversed by l-carnitine, but would have their own independent effect contributing to cerebral damage. This would explain the lack of protection afforded by the delayed (1 or 4 h after hypoxia-ischemia) administration of l-carnitine (Fig. 4). Delayed treatments may need to use both l-carnitine and other neuroprotective agents.
In the asphyxiated newborn, magnetic resonance spectroscopy studies have shown impaired oxidative phosphorylation developing within 24 h after delivery and persisting for days (36), the magnitude of which is linearly related to the degree of later reduction in brain growth (37). In the newborn rat model of hypoxia-ischemia, a similar pattern of early disruption of energy metabolism (38), followed by a delayed, secondary decline (39), has also been described. Experimental and clinical evidence suggests that disruption in normal mitochondrial respiration is an early, pivotal event in cell death after cerebral ischemia.
Treatment with carnitine may be of particular significance to the term or preterm infant with brain injury. Our data show a profound acute increase in mortality associated with d-carnitine administration in newborn rats undergoing hypoxia-ischemia. This finding is in contrast to other studies in adult animals showing equal protective efficacy of l- and d-carnitine in decapitation injury (40) and ammonia-induced seizures (41). The newborn infant may be at higher risk for the development of carnitine deficiency because of the immature development of carnitine biosynthetic pathways. Thus, in preterm infants who receive total parenteral nutrition, carnitine supplementation improves carnitine concentrations and nitrogen balance (42) as well as overall growth (43).
There is precedent for the use of carnitine in the treatment of ischemic injury. In adult studies, administration of carnitine reduces myocardial injury after ischemia-reperfusion (44–46). Carnitine, or carnitine esters, has also been shown to benefit the ischemic heart in animal models (47), including the neonatal heart (48), as well as in a clinical trial of patients with ischemic cardiomyopathy (49). The protective effective of carnitine, or the short-chain ester acetyl-l-carnitine, has been demonstrated in spinal cord ischemia-reperfusion (50), transient focal (14, 51) and global cerebral ischemia (12), ammonia-induced neurotoxicity (52), and serum-deprivation–induced apoptotic neuronal death (53). However, another study of focal cerebral ischemia in the rat failed to show any reduction in infarct volume after treatment with l-carnitine (12). The use of l-carnitine for the treatment of hypoxic-ischemic insult in the newborn human or animal has not previously been directly evaluated. In the immature rat, l-carnitine treatment reduces endogenous whole-brain platelet-activating factor levels, but does not affect changes in brain platelet-activating factor during hypoxia-ischemia (54).
We hypothesize that l-carnitine reduces brain injury after hypoxia-ischemia by buffering toxic acyl-CoA esters and releasing critical metabolic processes from the inhibition produced by acyl-CoA (8–11, 33). Our finding that d-carnitine treatment is associated with a marked acute increase in mortality during hypoxia-ischemia provides indirect support for the importance of carnitine to cellular metabolism during ischemia and the sensitivity of the newborn to carnitine depletion. d-Carnitine reduces serum levels of l-carnitine (55) and can inhibit uptake of l-carnitine in heart (56), kidney (57), and brain (58). The increase in mortality during ischemia may, therefore, be associated with a reduction in the availability of l-carnitine. Total carnitine levels in a series of 25,644 premature and term neonates (59) were not correlated with either gestational age or birth weight, although birth weight below 2500 g and male sex were significantly associated with higher total carnitine levels. This study found an increase in the acylcarnitine-to-free carnitine ratio in the group of newborns with low total carnitine. This finding suggests that in the presence of lower total carnitine values, acyl-CoA levels are increased. Our hypothesis that low total carnitine provides less buffering for toxic acyl-CoA esters implies that that newborns with low total carnitine values may therefore be at greater risk for brain injury associated with hypoxia-ischemia.
CONCLUSIONS
Numerous studies have used the newborn rodent model to investigate the efficacy of potential neuroprotective therapeutic strategies (1). With the exception of hypothermia (60, 61) and allopurinol (62), the clinical application of these therapies in the treatment of the brain injury in the human newborn has been limited. Accordingly, there is a need for further therapeutic modalities for perinatal brain injury, which, alone or in combination with other therapies, are neuroprotective but have a low risk of adverse side effects in the asphyxiated newborn. Carnitine is easy to administer, has low toxicity, is routinely used in neonates, and may provide neuroprotection at one of the early, pivotal steps in the commitment to cell death. There is extensive pediatric clinical experience with carnitine in the management of epilepsy, inborn errors of metabolism, cardiomyopathy, and apnea of prematurity (15–18). l-Carnitine merits further investigation as a treatment modality for the asphyxiated newborn or as prophylaxis for the at-risk fetus or newborn.
Abbreviations
- FJ-B:
-
fluoro-Jade B
- P:
-
postnatal day
REFERENCES
duPlessis A, Johnston MV 1997 Hypoxic-ischemic brain injury in the newborn: cellular mechanisms and potential strategies for neuroprotection. Clin Perinatol 24: 627–654
Volpe J 1995 Hypoxic-ischemic encephalopathy. In: Volpe J (ed) Neurology of the Newborn. WB Saunders, Philadelphia, pp 211–369.
Johnston M, Trescher W, Ishida A, Nakajima W 2001 Neurobiology of hypoxic-ischemic injury in the developing brain. Pediatr Res 49: 735–741
Murphy A, Fiskum G, Beal M 1999 Mitochondria in neurodegeneration: bioenergetic function in cell life and death. J Cereb Blood Flow Metab 19: 231–245
Gilland E, Puka-Sundvall M, Hillered L, Hagberg H 1998 Mitochondrial function and energy metabolism after hypoxia-ischemia in the immature rat brain: involvement of NMDA receptors. J Cereb Blood Flow Metab 18: 297–304
Stumpf D, Parker D, Angelini C 1985 Carnitine deficiency, organic acidemias, and Reye's syndrome. Neurology 35: 1041–1045
DeVivo D, Tein I 1990 Primary and secondary disorders of carnitine metabolism. Int Pediatr 5: 134–141
Pande S, Blanchaer M 1971 Reversible inhibition of mitochondrial adenosine disphosphate phosphorylation by long chain acyl coenzyme A esters. J Biol Chem 246: 402–411
Shug A, Shrago E, Bittar N, Folts J, Koke J 1975 Acyl-CoA inhibition of adenine nucleotide translocation in ischemic myocardium. Am J Physiol 228: 689–692
Stumpf D, McAfee J, Parks J, Eguren L 1980 Propionate inhibition of succinate: CoA ligase (GDP) and the citric acid cycle in mitochondria. Pediatr Res 14: 1127–1131
Lopaschuk G 2000 Regulation of carbohydrate metabolism in ischemia and reperfusion. Am Heart J 139: S115–S119
Rosenthal R, Williams R, Bogaert Y, Getson P, Fiskum G 1992 Prevention of postischemic canine neurological injury through potentiation of brain energy metabolism by acetyl-L-carnitine. Stroke 23: 1312–1318
Slivka A, Silbersweig D, Pulsinelli W 1990 Carnitine treatment for stroke in rats. Stroke 21: 808–811
Lolic M, Fiskum G, Rosenthal R 1997 Neuroprotective effects of acetyl-L-carnitine after stroke in rats. Ann Emerg Med 29: 758–765
DeVivo D, Bohan T, Coulter D, Dreifuss F, Greenwood R Jr, Shields W, Stafstrom C, Tein I 1998 L-carnitine supplementation in childhood epilepsy: current perspectives. Epilepsia 39: 1216–1225
Pons R, DeVivo D 1995 Primary and secondary carnitine deficiency syndromes. J Child Neurol 10: S8–S24
Winter S, Jue K, Prochazka J, Francis P, Hamilton W, Linn L, Helton E 1995 The role ofL-carnitine in pediatric cardiomyopathy. J Child Neurol 10: S45–S51
O'Donnell J, Finer N, Rich W, Barshop B, Barrington K 2002 Role ofL-carnitine in apnea of prematurity: a randomized controlled trial. Pediatrics 109: 622–626
Rice J III, Vannucci R, Brierley J 1981 The influence of immaturity on hypoxic-ischemic brain damage in the rat. Ann Neurol 9: 131–141
Gidday J, Shah A, Maceren R, Wang Q, Pellegrino D, Holtzman D, Park T 1999 Nitric oxide mediates cerebral ischemic tolerance in a neonatal rat model of hypoxic preconditioning. J Cereb Blood Flow Metab 19: 331–340
Vannucci R, Towfighi J, Vannucci S 1998 Hypoxic preconditioning and hypoxic-ischemic brain damage in the immature rat: pathologic and metabolic correlates. J Neurochem 71: 1215–1220
Romijn H, Hofman M, Gramsbergen A 1991 At what age is the developing cerebral cortex of the rat comparable to that of the full-term human baby?. Early Hum Dev 26: 61–67
Gidday J, Fitzgibbons J, Shah A, Park T 1994 Neuroprotection from ischemic brain injury by hypoxic preconditioning in the neonatal rat. Neurosci Lett 168: 221–224
Gidday J, Fitzgibbons J, Shah A, Kraujalis M, Park T 1995 Reduction in cerebral ischemic injury in the newborn rat by potentiation of endogenous adenosine. Pediatr Res 38: 306–311
Busto R, Dietrich W, Globus M-T, Vakdes I, Schenberg P, Ginsberg M 1987 Small differences in intraischemic brain temperature critically determine the extent of ischemic neuronal injury. J Cereb Blood Flow Metab 7: 729–738
Hearn T, Coleman A, Lai J, Griffith O, Cooper A 1980 l -Carnitine: a possible therapeutic agent in liver disease. In: Borum P (ed) Clinical Aspects of Human Carnitine Deficiency. Pergamon Press, New York, pp 238–239.
Bona E, Aden U, Fredholm B, Hagberg H 1995 The effect of long-term caffeine treatment on hypoxic-ischemic brain damage in the neonate. Pediatr Res 38: 312–331
McDonald J, Roeser N, Silverstein F, Johnston M 1989 Quantitative assessment of neuroprotection against NMDA-induced brain injury. Exp Neurol 106: 289–296
Towfighi J, Housman C, Vannucci R, Heitjan D 1994 Effect of unilateral perinatal hypoxic-ischemic brain damage on the gross development of the opposite cerebral hemisphere. Biol Neonate 65: 108–118
Halle J, Kasper C, Gidday J, Koos B 1997 Enhancing adenosine A1 receptor binding reduces hypoxic-ischemic brain injury in newborn rats. Brain Res 759: 309–312
Schmued L, Hopkins K 2000 Fluoro-Jade B: a high affinity fluorescent marker for the localization of neuronal degeneration. Brain Res 874: 123–130
[No authors listed] 1999 Recommendations for standards regarding preclinical neuroprotective and restorative drug development. Stroke 30: 2752–2758
Matsuishi T, Stumpf D, Seliem M, Eguren L, Chrislip K 1991 Propionate mitochondrial toxicity in liver and skeletal muscle: acyl CoA levels. Biochem Med Metabol Biol 45: 244–253
Abe K, Aoki M, Kawagoe J, Yosida T, Hattori A, Kogure K, Itoyan Y 1995 Ischemic delayed neuronal death, a mitochondrial hypothesis. Stroke 26: 1478–1489
Green D, Reed J 1998 Mitochondria and apoptosis. Science 281: 1309–1312
Hope P, Costello A, Cady E, Delpy D, Tofts P, Chu A, Hamilton P, Reynolds E, Wilkie D 1984 Cerebral energy metabolism studied with phosphorus NMR spectroscopy in normal and birth-asphyxiated infants. Lancet 2: 366–370
Roth S, Baudin J, Cady E, Johal K, Townsend J, Wyatt J, Reynolds E, Stewart A 1997 Relation of deranged neonatal cerebral metabolism with neurodevelopmental outcome and head circumference at 4 years. Dev Med Child Neurol 39: 718–725
Puka-Sundvall M, Wallin C, Gilland E, Hallin U, Sandberg M, Carlson J-O, Blomgren K, Hagberg H 2000 Impairment of mitochondrial respiration after cerebral hypoxia-ischemia in immature rats: relationship to activation of caspase-3 and neuronal injury. Brain Res Dev Brain Res 125: 43–50
Blumberg RM, Cady EB, Wigglesworth JS, McKenzie JE, Edwards AD 1997 Relation between delayed impairment of cerebral energy metabolism and infarction following transient focal hypoxia-ischaemia in the developing brain. Exp Brain Res 113: 130–137
Matsuoka M, Igisu H, Iryo Y 1992 Preservation of energy metabolites by carnitine in the mouse brain under ischemia. Brain Res 590: 334–336
Igisu H, Matsuoka M, Iryo Y 1995 Protection of the brain by carnitine. J Occup Health 37: 75–82
Helms R, Mauer E, Hay W, Christensen M, Storm M 1990 Effect of intravenousL-carnitine on growth parameters and fat metabolism during parenteral nutrition in neonates. J Parenter Enteral Nutr 14: 448–453
Helms R, Whitington P, Mauer E, Catarau E, Christensen M, Borum P 1986 Enhanced lipid utilization in infants receiving oralL-carnitine during long-term parenteral nutrition. J Pediatr 109: 984–988
Arsenian M 1997 Carnitine and its derivatives in cardiovascular disease. Prog Cardiovasc Dis 40: 265–286
Folts J, Shug A, Koke J, Bittar N 1978 Protection of the ischemic heart myocardium with carnitine. Am J Cardiol 41: 1209–1214
Thomsen J, Shug A, Yap V, Patel A, Karras T, DeFelice S 1979 Improved pacing tolerance of the ischemic human myocardium after administration of carnitine. Am J Cardiol 43: 300–306
Schonekess B, Allard M, Lopaschuk G 1995 PropionylL-carnitine improvement of hypertrophied heart function is accompanied by an increase in carbohydrate oxidation. Circ Res 77: 726–734
Nemoto S, Aoki M, Dehua C, Imai Y 2001 Effects of carnitine on cardiac function after cardioplegic ischemia in neonatal rabbit hearts. Ann Thoracic Surg 71: 254–259
Gurlek A, Tutar E, Akcil E, Dincer I, Erol C, Kocaturk P, Oral D 2000 The effects ofL-carnitine treatment on left ventricular function and erythrocyte superoxide dismutase activity in patients with ischemic cardiomyopathy. Eur J Heart Failure 2: 189–193
Rahman A, Ustundag B, Burma O, Ozercan I, Erol F 2001 Neuroprotective effect of regional carnitine on spinal cord ischemia-reperfusion injury. Eur J Cardiothoracic Surg 20: 65–70
Shuaib A, Waqaar T, Wishart T, Kanthan R, Howlett W 1995 Acetyl-L-carnitine attenuates neuronal damage in gerbils with transient forebrain ischemia only when given before the insult. Neurochem Res 9: 1021–1025
Matsuoka M, Igisu H 1993 Comparison of the effects ofL-carnitine andd-carnitine and acetyl-L-carnitine on the neurotoxicity of ammonia. Biochem Pharmacol 46: 159–164
Ishii T, Shimpo Y, Matsuoka Y, Kinoshita K 2000 Anti-apoptotic effect of acetyl-L-carnitine andL-carnitine in primary cultured neurons. Jpn J Pharmacol 83: 119–124
Akisu M, Kultursay N, Coker I, Huseyinov A 1998 The effect ofL-carnitine on platelet activating factor concentration in the immature rat model of hypoxic-ischemic brain injury. Acta Med Okayama 52: 183–187
Rebouche C 1983 Effect of dietary carnitine isomers and gammabutyrobetaine onL-carnitine biosynthesis and metabolism in the rat. J Nutr 113: 1906–1913
Vary T, Neely J 1982 Characterization of carnitine transport in isolated perfused adult rat hearts. Am J Physiol 242: H585–H592
Huth P, Shug A 1980 Characterization of carnitine transport in rat kidney cortex brain slices. Biochim Biophys Acta 602: 621–634
Huth P, Schmidt M, Hall P, Rg F, Shug A 1981 The uptake of carnitine by slices of rat cerebral cortex. J Neurochem 36: 715–723
Chace DH, Pons R, Chiriboga CA, McMahon D, Tein I, Naylor EW, De Vivo DC 2003 Neonatal blood carnitine concentrations: normative data by electrospray tandem mass spectrometry. Pediatr Res 53: 1–7
Gunn A, Gluckman P, Gunn T 1998 Selective head cooling in newborn infants after perinatal asphyxia: a safety study. Pediatrics 102: 885–892
Wagner C, Eicher D, Katikaneni L, Barbosa E, Holden K 1999 The use of hypothermia: a role in the treatment of neonatal asphyxia?. Pediatr Neurol 21: 429–443
Clancy R, McGaurn S, Goin J, Hirtz D, Norwood W, Gaynor W, Jacobs M, Wernovsky G, Mahle WT, Murphy J, Nicolson S, Steven J, Spray T 2001 Allopurinol neurocardiac protection trial in infants undergoing heart surgery using deep hypothermic circulatory arrest. Pediatrics 108: 61–70
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by The Women's Board, Children's Memorial Hospital.
Rights and permissions
About this article
Cite this article
Wainwright, M., Mannix, M., Brown, J. et al. L-Carnitine Reduces Brain Injury after Hypoxia-Ischemia in Newborn Rats. Pediatr Res 54, 688–695 (2003). https://doi.org/10.1203/01.PDR.0000085036.07561.9C
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000085036.07561.9C
This article is cited by
-
l-Carnitine and Acetyl-l-carnitine Roles and Neuroprotection in Developing Brain
Neurochemical Research (2017)
-
Therapeutic Hypothermia Achieves Neuroprotection via a Decrease in Acetylcholine with a Concurrent Increase in Carnitine in the Neonatal Hypoxia-Ischemia
Journal of Cerebral Blood Flow & Metabolism (2015)
-
Brain Barrier Properties and Cerebral Blood Flow in Neonatal Mice Exposed to Cerebral Hypoxia-Ischemia
Journal of Cerebral Blood Flow & Metabolism (2015)
-
Metabolic Alterations in Developing Brain After Injury: Knowns and Unknowns
Neurochemical Research (2015)
-
L-Carnitine preserves endothelial function in a lamb model of increased pulmonary blood flow
Pediatric Research (2013)