Abstract
In the perinatal period, glucocorticoids are frequently administered to enhance pulmonary maturity or prevent chronic lung disease of prematurity. Recently, it has been suggested that the perinatal exposure to glucocorticoids can be associated with unfavorable neurologic development. We studied the hypothesis that 24-h pretreatment with glucocorticoid might modify cerebrovascular responses to high and low partial arterial CO2 tension in newborn animals in vivo. A closed cranial window was implanted over the left parietal cortex of 20 anesthetized ventilated newborn (<3 d old) pigs. The actual experiments were carried out in 15 pigs: eight pretreated with a total dose of 6 mg/kg of dexamethasone and seven controls. Five pigs were used for preliminary experiments as described in the text. Pial arteriolar diameters were measured during 1) baseline conditions (normocapnia), 2) hypercapnia induced by ventilating the animals with a gas mixture containing 10% CO2, or 3) hyperventilation with resultant hypocapnia. Under these conditions, the concentrations of 6-keto-PGF1α in the CSF were measured in five experimental animals and six controls. In summary, the dexamethasone pretreatment 1) attenuated the hypercapniainduced dilator responses of pial arterioles and prevented the hypercapnia-associated fall in mean arterial blood pressure; 2) caused moderate, although not statistically significant, diminution in 6-keto-PGF1α levels in the CSF during baseline; 3) blocked hypercapnia-induced elevation of 6-keto-PGF1α; and 4) enhanced vasoconstrictive arteriolar responses to hyperventilation. We speculate that in the clinical setting, the dexamethasone effects may compromise the adjustments of global or regional cerebral blood flow to changing physiologic states in neonates.
Similar content being viewed by others
Main
Glucocorticoids, currently widely used in obstetric and neonatal intensive care to prevent neonatal respiratory distress (1), are likely to have beneficial effects on pulmonary vascular maturation (2). Glucocorticoids may also influence cerebrovascular tone and integrity via several mechanisms. Glucocorticoids influence prostaglandin biosynthesis in brain (3) and other tissues, including endothelial cells (4–6), and thus may disturb prostanoid-induced vasodilation of cerebral arteries. Steroids also regulate the expression of heme-oxygenase-2, one of the isoenzymes that produce carbon monoxide and biliverdin via the metabolism of heme (7). In this way, steroids may influence endogenous production of carbon monoxide, which has been shown to dilate pial arterioles (8).
Partial pressure of CO2 also affects cerebrovascular circulation. Key effector sites are cerebral arterioles, which are important resistance vessels in the brain circulation. Hypercapnia and acidosis lead to prostanoid-mediated vasodilation (9, 10), whereas the mechanisms of hypocapnia-induced vasoconstriction are prostanoid-independent and not yet well defined (11, 12). A report (13) suggests that dexamethasone pretreatment may attenuate hypercapnia-associated (prostanoid-mediated) dilation of cerebral arterioles. In the present study, we examined the hypothesis that 24-h dexamethasone pretreatment would modify pial arteriolar and cerebrospinal fluid prostanoid responses to both high and low partial arterial CO2 tensions in newborn pigs. We used closed cerebral window technique, which allowed us to monitor the changes in cerebral resistance vessels by measuring the diameters of pial arterioles, record the concomitant acid-base status and arterial blood pressure (aBP) levels, and draw samples of cerebrospinal fluid (CSF) for prostanoid determinations during the experiments.
METHODS
Animals.
All procedures that involved animals were reviewed and approved by the Animal Care and Use Committee of the University of Tennessee Health Science Center. Cranial window was inserted into 20 newborn (<3 d old) piglets. Before surgery, 11 piglets were given pretreatments with multiple (three or five) intramuscular dexamethasone injections during 24 or 48 h before the experiments. Two piglets with cranial window in place received one large dose of dexamethasone i.v. immediately before the experiments to assess the acute effects of dexamethasone (see below for description of dexamethasone dosing and experimental design). Seven piglets (control group) received pretreatments with vehicle only. The median (range) weight of dexamethasone-treated animals was 2.3 (1.3-2.6) kg and of controls was 2.2 (1.3-2.5) kg.
Before the experiments, the animals were anesthetized with ketamine hydrochloride (33 mg/kg intramuscularly) and acepromazine (3.3 mg/kg intramuscularly) and maintained on α-chloralose 50 mg/kg i.v., as a bolus, followed by 5 mg/kg every 3-4 h to maintain the anesthesia at the desired level. The animals were tracheostomized and ventilated with a neonatal positive pressure respirator (Bourns BP-200), using air or, if needed, air-oxygen mixture to keep partial arterial O2 tension (PaO2) above 7 kPa. Catheters were inserted into the femoral artery to draw blood samples for the determination of blood gases and pH and to record mean aBP and into the femoral vein to continue the anesthesia and provide maintenance i.v. fluids (5% dextrose, 0.9% saline). Body temperature was kept within 37-38.5°C by using rectal probe for continuous monitoring and adjusting the warmer accordingly. At the end of the experiments, the anesthetized animals were killed with i.v. injection of saturated KCl solution.
Cranial window placement.
A closed cranial window was implanted over the left parietal cortex for measurement of pial arteriole diameters and collection of CSF as described previously (14, 15). For implantation, the scalp was retracted and a 2-cm-diameter hole was made in the skull over the parietal cortex. The dura was cut without touching the brain, and all cut edges were retracted over the bone. A stainless steel and glass cranial window was placed in the hole and cemented into place with dental acrylic. The space under the window was filled with artificial CSF that was equilibrated with 6% CO2 and 6% O2, which produced gases and pH within the normal range for CSF [pH 7.33-7.40, partial arterial CO2 tension (PaCO2) 42-46 mm Hg (corresponding 5.6-6.1 kPa)], PaO2 43-50 mm Hg (corresponding 5.7-6.6 kPa)]. Artificial CSF could be injected and samples collected from the needle ports on the sides of the window. The volume of the fluid directly under the window was 500 μL and was contiguous with the periarachnoid space. Pial vessels were observed with dissecting microscope. Diameters were measured using a video micrometer, coupled to microscope, television camera, and video monitor. When feasible, one small (60-70 μm diameter) and one large (˜100 μm diameter) arteriole per animal were measured and analyzed at different times, according to the experimental design described below. We were able to identify eight small and seven large pial arterioles in eight animals belonging to the dexamethasone pretreated (DEXA) experimental group (see below) and, correspondingly, six small and seven large pial arterioles in seven control animals.
Determination of dosing for dexamethasone pretreatment.
The dexamethasone solution used in all of the experiments was made by dissolving dexamethasone sodium phosphate (purchased from Sigma Chemical Co., St. Louis, MO, U.S.A.) in sterile physiologic saline to produce concentration of 10 mg/mL. Before choosing the dose and duration of pretreatment, we first evaluated the acute effects of a single large parenteral dose of dexamethasone. In two piglets with cranial window in place, six pial arterioles with 70-100 μm diameter (three arterioles per animal) were located and measured. Then, 18 mg/kg dexamethasone was given as a rapid i.v. bolus injection. The diameters of the selected arterioles were measured at 5, 15, 30, 45, 60, 90, and 120 min after the injection. No changes were observed in the resting diameters. We then performed the hypercapnia and hyperventilation experiments according to the experimental design (see below) and found no differences in hypercapnia- or hyperventilation-induced responses when compared with controls (data not shown).
Before the actual experiments, we performed a small pilot study to compare the effects of two dexamethasone pretreatment regimens. According to the first regimen, each animal (n = 3) received a 3-mg dose of dexamethasone intramuscularly three times, starting 24 h before the cranial window placement. According to the second regimen, each animal (n = 3) received a 3-mg dose of dexamethasone intramuscularly five times, starting 48 h before the cranial window placement. We found no differences in pial arteriolar reactivity between these two groups, measured by using the experimental design described below (data not shown), and therefore decided to use the 24-h pretreatment regimen throughout the series of the experiments. The three animals in the pilot group pretreated according to the first regimen were included to the experimental group (total n = 8). The mean dose of dexamethasone was 6 mg/kg. Control animals (n = 7) were pretreated with corresponding volumes (0.3 mL) of sterile physiologic saline.
Producing hypercapnia and hypocapnia.
Hypercapnia was produced by ventilating the animal with a gas mixture containing 10% CO2 as described previously (15). Hypocapnia was produced by hyperventilating the animals by increasing the proximal inspiratory pressure from baseline levels (10-12 cm H2O) to 20 cm H2O and increasing ventilation frequency from 10-15 breaths/min to 18-20 breaths/min. Before deciding the optimal duration of hyperventilation, we measured blood gases and pH during baseline conditions (16 observations) and consecutively after 1-2 min (6 observations), 5 min (15 observations), and 10 min (9 observations) of hyperventilation. Already after 2 min of hyperventilation, all PaCO2 values had declined to hypocapnic range (below 3.9 kPa) and were maintained within this level, with resultant increase in all pH values to alkalotic range (7.48-7.54) after 5 min of hyperventilation.
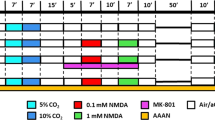
Experimental design.
The time and event line (Fig. 1) gives the detailed timing of dexamethasone versus saline pretreatment, surgery, blood and CSF samples, as well as of measurements of the pial arteriolar diameters and the mean aBP. After the surgery was performed, the animals were stabilized on the ventilator for 10-20 min under the baseline conditions to allow the blood gases, pH, and mean aBP to settle within the normal range before the actual experiments were started. Between hypercapnia and hyperventilation experiments, a time interval of at least 10-15 min was needed for the stabilization of blood gases and mean aBP.
CSF was sampled from five experimental animals and six controls, with the technique described previously (15). Approximately 300-μL samples of CSF were taken from the space under the window by slowly infusing artificial CSF through the inlet port and allowing the CSF to drip freely from the outlet port into a collecting tube containing 5 μL of 200 mM EDTA. The samples were put on ice immediately and stored at −20°C before analysis. Concentrations of 6-keto-PGF1α (the hydrolysis product of prostacyclin) in the CSF samples were determined by RIA (14).
Statistical analysis.
Data are presented as medians (range) or means (SEM). Differences between the groups were calculated with nonparametric Mann-Whitney U test. Significance of changes during the experiments (“within the groups”) were assessed using nonparametric test for two related samples. The data were analyzed using SPSS for Windows, Release 9.0.1.
RESULTS
Arterial Blood Gases, pH, and Mean aBP During Experiments
Baseline arterial pH, PaCO2, PaO2, and mean aBP values for DEXA and control groups were within the normal range without any significant differences between the groups (Table 1).
Effects of hypercapnia and hyperventilation on the acid base status, PaO2, and mean aBP in DEXA and control groups are summarized in Table 1. Five-minute hypercapnia increased PaCO2 values significantly from baseline 1 levels with resultant declines in pH values both in the DEXA group and controls. There were no differences in PaCO2 levels observed at the end of the 5-min hypercapnia periods between the DEXA group and controls. No hypoxemic PaO2 values were observed, and the PaO2 values measured at the end of the hypercapnic experiments did not differ significantly from values recorded at baseline 1. The mean aBP values were differently influenced in the DEXA group versus controls. In DEXA animals, no significant change in mean aBP values was observed when baseline 1 values and measurements at the end of 5-min hypercapnia were compared, whereas control animals exhibited significant declines of mean aBP at the same time period.
Hyperventilation for 5 min produced significant hypocapnia and increased pH and PaO2 values from baseline 2 levels similarly within the DEXA group and controls (Table 1). Dexamethasone pretreatment did not influence mean aBP values during the hyperventilation experiments.
Effects of dexamethasone pretreatment on arteriolar diameter during hypercapnia and hyperventilation.
No differences were found in the baseline diameters of the small (60-70 μm) and large (90-110 μm) arterioles between the DEXA group and controls (Table 2). The modifying effects of dexamethasone pretreatment on arteriolar diameter during hyper- or hypocapnia are summarized in Figure 2. After 5-min hypercapnia, the absolute increase in arteriolar diameters in the DEXA group was significantly less than that observed in corresponding nontreated controls (p = 0.001 for both small and large arterioles). After 5-min hyperventilation, the absolute diminution of arteriolar diameters in the DEXA group was significantly more pronounced than in corresponding nontreated controls (p = 0.02 for small arterioles and p = 0.009 for large arterioles).
Effect of dexamethasone pretreatment on the concentrations 6-keto-PGF1α in CSF.
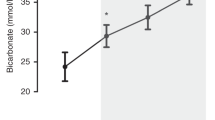
The baseline 1 levels of 6-keto-PGF1α in DEXA animals seemed to be moderately lower than the levels in control animals, but the difference was not significant. At the end of the hypercapnia experiments, the CSF samples taken from DEXA animals had significantly lower concentrations of 6-keto-PGF1α than the samples taken from controls (p = 0.004). At the end of the hyperventilation experiments, no differences in the concentrations of 6-keto-PGF1α in the CSF samples were found between DEXA and control animals (Table 3).
DISCUSSION
The main findings of this study in this animal model are that dexamethasone pretreatment 1) attenuates the pial arteriolar hyperemic response to hypercapnia, 2) prevents the normal elevation of 6-keto-PGF1α in the CSF samples during hypercapnia, and 3) enhances constrictive responses of pial arterioles to low PaCO2 induced by hyperventilation. Dexamethasone also prevented the hypercapnia-associated fall in mean aBP that was evident in the control animals. Although the number of observations is small, dexamethasone seems to have minimal, if any, acute direct cerebrovascular effects. After a single high (18 mg/kg i.v.) dose of dexamethasone, there were no changes in the resting diameters of pial arterioles.
The endothelium-derived prostanoids are important dilators of cerebral arterioles under both basal (3, 14) and pathologic conditions such as hypotension (16), hypoxia (10, 17), and hypercapnic challenge (9, 18). A key enzyme in prostanoid synthesis is cyclo-oxygenase, which is represented by two isoforms encoded by different genes, COX-1 and COX-2 (19). In newborn animals, COX-2 protein is constitutively expressed in microvessels, in vascular endothelium in the choroid plexus, and in cultured microvascular cells (19–22) and provides a major functional contribution to dilator prostanoid synthesis (23). Previously, pretreatment with dexamethasone had been shown to diminish hypercapnia-induced formation of prostanoids and attenuate the vasorelaxant responses to increased PaCO2 (13). In a different animal model (24), dexamethasone inhibited the dilation of cerebral arterioles, possibly by interfering with the expression of cyclo-oxygenase in leptomeningeal tissues. We found that multiple-dose 24-h pretreatment with dexamethasone significantly attenuated hyperemic cerebrovascular response to hypercapnia and caused a diminution in the hypercapnia-induced elevation of the prostacyclin metabolite 6-keto-PGF1α in CSF samples. Although the cerebrovascular effects of dexamethasone may require prostanoid participation, it seems unlikely that these effects could be attributed solely to the inhibition of cyclo-oxygenase. Substantial prostacyclin continues to be produced, and the role of prostacyclin in this respect can be permissive (18). Dexamethasone can also induce a group of phospholipase A2 inhibitory proteins, which in turn could limit the availability of an important prostaglandin precursor, arachidonic acid, by preventing its hydrolytic cleavage from phospholipids (25). When considering prostanoid participation, it is not possible to exclude the interference of several other compensatory mechanisms and mediators, e.g. other endothelium-derived relaxing factors, adenosine, ATP, glutamate, Ca++, and K+ (26). Nevertheless, it seems clear that the mechanisms of dexamethasone inhibition of hypercapnic vasodilation cannot be explained solely by effects on prostacyclin production.
Dexamethasone may directly or indirectly alter other processes involved in the regulation of cerebrovascular tone. Prostanoids, together with paracrine mediators nitric oxide (NO) and CO, are predominant vasorelaxants in the newborn cerebral microcirculation, and the interactions among these systems are likely (8, 27–29). The dilator actions of CO seem to involve prostacyclin and NO as permissive enablers (30), and the process is likely to occur via the activation of Ca2+-dependent potassium channels (8). Glucocorticoids have been shown to down-regulate the expression of calcium-dependent potassium channels in vascular smooth muscle (31) and thereby may interfere with the CO-induced vasorelaxant responses. If the down-regulated expression of this channel by glucocorticoids parallels the diminution in channel activity, then an attenuated relaxation response—with a resultant net increase in vascular tone-can be expected. The dexamethasone effects could be transmitted via several alternative pathways. Glucocorticoids might down-regulate the expression of endothelial NO synthase (32), inhibit the formation of a cofactor necessary for NO synthase (33), or even influence the permeability of blood-brain barrier (34) and by this way modify the transfer kinetics for other substances. The precise processes involved will require further investigation.
The present data show that, in a newborn animal model, pretreatment with dexamethasone significantly attenuates cerebral arteriolar vasorelaxant responses during hypercapnia, augments vasoconstriction during hyperventilation, and diminishes the fall in systemic aBP during hypercapnia. There are a few points that need consideration when the clinical relevance of these findings is contemplated. In this newborn animal model, as often in the “true” clinical practice, hypercapnia was associated with “respiratory” acidemia and hypotension, and hyperventilation with hypocapnia, alkalosis, and hyperoxemia. In these settings, we thus studied the modulating effects of dexamethasone pretreatment plus the combinations of the above factors on the cerebral arteriolar responses. Although the anesthetic procedure was similar throughout the experiments, we cannot exclude the possibility that these agents may have influenced pial arteriolar responses. Dexamethasone pretreatment doses in these experiments were higher than the doses given to sick neonates. The effects of smaller dexamethasone doses on the pial arteriolar responses should now be studied urgently, because data on dangerous adverse effects associated with postnatal use of dexamethasone are accumulating (35, 36). A recent follow-up study indicated that dexamethasone given shortly after birth in preterm infants with respiratory distress is associated with a significant increase in cerebral palsy and neurodevelopmental delay (37). Our current data suggest that by blunting the hyperemic cerebrovascular responses and augmenting the constrictor responses in the cerebral microvessels, dexamethasone treatment may potentiate the vasoconstrictor responses of pial arterioles and hence contribute to brain ischemia. While these and other short- and longterm cerebrovascular effects of dexamethasone are examined, caution should continue to be exercised when this drug is used in the neonatal period.
Abbreviations
- aBP:
-
arterial blood pressure
- CSF:
-
cerebrospinal fluid
- DEXA:
-
dexamethasone pretreated
- NO:
-
nitric oxide
- PaCO2:
-
partial arterial CO2 tension
- PaO2:
-
partial arterial O2 tension
REFERENCES
Crowley P 2000 Prophylactic corticosteroids for preterm birth. Cochrane Database Syst Rev 2: CD000065
Grover TR, Ackerman KG, Le Cras TD, Jobe AH, Abman SH 2000 Repetitive prenatal glucocorticoids increase lung endothelial nitric oxide synthase expression in ovine fetuses delivered at term. Pediatr Res 48: 75–83.
Weidenfeld J, Amir I, Shohami E 1993 Role of glucocorticoids in the regulation of brain prostaglandin biosynthesis under basal conditions and in response to endotoxin. Endocrinology 132: 941–945.
Hullin F, Raynal P, Ragab-Thomas JM, Fauvel J, Chap H 1989 Effect of dexamethasone on prostaglandin synthesis and on lipocortin status in human endothelial cells. Inhibition of prostaglandin I 2 synthesis occurring without alteration of arachidonic acid liberation and of lipocortin synthesis. J Biol Chem 264: 3506–3513.
Ito Y, Kozawa O, Tokuda H, Suzuki A, Watanabe Y, Kotoyori J, Oiso Y 1994 Glucocorticoid inhibits cAMP production induced by vasoactive agents in aortic smooth muscle cells A. therosclerosis 110: 69–76.
Rosenstock M, Katz S, Danon A 1997 Glucocorticoids regulate both phorbol ester and calcium ionophore-induced endothelial prostacyclin synthesis. Prostaglandins Leukot Essent Fatty Acids 56: 1–8.
Raju VS, McCoubrey WK Jr, Maines MD 1997 Regulation of heme oxygenase-2 by glucocorticoids in neonatal rat brain: characterization of a functional glucocorticoid response element. Biochim Biophys Acta 1351: 89–104.
Leffler CW, Nasjletti A, Yu C, Johnson RA, Fedinec AL, Walker N 1999 Carbon monoxide and cerebral microvascular tone in newborn pigs. Am J Physiol 276:H1641–H1646.
Parfenova H, Shibata M, Zuckerman S, Leffler CW 1994 CO2 and cerebral circulation in newborn pigs: cyclic nucleotides and prostanoids in vascular regulation. Am J Physiol 266:H1494–H1501.
Leffler CW, Parfenova H 1997 Cerebral arteriolar dilation to hypoxia: role of prostanoids. Am J Physiol 272:H418–H424.
Albuquerque ML, Lowery-Smith L, Hsu P, Parfenova H, Leffler CW 209 1995 Low CO2 stimulates inositol phosphate turnover and increased inositol 1,4,5-trisphosphate levels in piglet cerebral microvascular smooth muscle cells. Proc Soc Exp Biol Med 209: 14–19.
Albuquerque ML, Leffler CW 1998 pHo, pHi, and pCO2 in stimulation of IP3 and [Ca2+]c in piglet cerebrovascular smooth muscle. Proc Soc Exp Biol Med 219: 226–234.
Wagerle LC, DeGiulio PA, Mishra OP, Delivoria-Papadopoulos M 1991 Effect of dexamethasone on cerebral prostanoid formation and pial arteriolar reactivity to CO2 in newborn pigs. Am J Physiol 260:H1313–H1318.
Leffler CW, Busija DW 1985 Prostanoids in cortical subarachnoid cerebrospinal fluid and pial arterial diameter in newborn pigs. Circ Res 57: 689–694.
Pourcyrous M, Busija DW, Shibata M, Bada HS, Korones SB, Leffler CW 1999 Cerebrovascular responses to therapeutic dose of indomethacin in newborn pigs. Pediatr Res 45: 582–587.
Leffler CW, Busija DW 1987 Prostanoids and pial arteriolar diameter in hypotensive newborn pigs. Am J Physiol 252:H687–H691.
Leffler CW, Smith JS, Edrington JL, Zuckerman SL, Parfenova H 1997 Mechanisms of hypoxia-induced cerebrovascular dilation in the newborn pig. Am J Physiol 272:H1323–H1332.
Willis AP, Leffler CW 1999 NO and prostanoids: age dependence of hypercapnia and histamine-induced dilations of pig pial arterioles. Am J Physiol 277:H299–H307.
Parfenova H, Massie V, Leffler CW 2000 Developmental changes in endotheliumderived vasorelaxant factors in cerebral circulation. Am J Physiol 278:H780–H788.
Parfenova H, Eidson TH, Leffler CW 1997 Upregulation of COX-2 in cerebral microvascular endothelial cells by smooth muscle cell signals. Am J Physiol 273:C277–C288.
Parfenova H, Balabanova L, Leffler CW 1998 Posttranslational regulation of cyclooxygenase by tyrosine phosphorylation in cerebral endothelial cells. Am J Physiol 274:C72–C81.
Thrikawala N, Bari F, Beasley TC, Thore C, Busija DW 1998 Effects of ischemia on prostaglandin H synthase-2 expression in piglet choroid plexus. Prostaglandins Other Lipid Mediat 56: 77–87.
Peri KG, Hardy P, Li DY, Varma DR, Chemtob S 1995 Prostaglandin G/H synthase-2 is a major contributor of brain prostaglandins in the newborn. J Biol Chem 270: 24615–24620.
Brian JE Jr, Moore SA, Faraci FM 1998 Expression and vascular effects of cyclooxygenase-2 in brain. Stroke 29: 2600–2606.
Hirata F, Schiffman NE, Venkatasubramanian K, Salomon D, Axelrod J 1980 A phospholipase A2 inhibitory protein in rabbit neutrophils induced by glucocorticoids. Proc Natl Acad Sci U S A 77: 2533–2536.
Chemtob S, Beharry K, Barna T, Varma DR, Aranda JV 1991 Differences in the effects in the newborn piglet of various nonsteroidal antiinflammatory drugs on cerebral blood flow but not on cerebrovascular prostaglandins. Pediatr Res 30: 106–111.
Meilin S, Rogatsky GG, Thom SR, Zarchin N, Guggenheimer-Furman E, Mayevsky A 1996 Effects of carbon monoxide on the brain may be mediated by nitric oxide. J Appl Physiol 81: 1078–1083.
Durante W, Kroll MH, Christodoulides N, Peyton KJ, Schafer AI 1997 Nitric oxide induces heme oxygenase-1 gene expression and carbon monoxide production in vascular smooth muscle cells. Circ Res 80: 557–564.
Mancuso C, Pistritto G, Tringali G, Grossman AB, Preziosi P, Navarra P 1997 Evidence that carbon monoxide stimulates prostaglandin endoperoxide synthase activity in rat hypothalamic explants and in primary cultures of rat hypothalamic astrocytes. Brain Res Mol Brain Res 45: 294–300.
Leffler CW, Nasjletti A, Johnson RA, Fedinec AL 2001 Contributions of prostacyclin and nitric oxide to carbon monoxide-induced cerebrovascular dilatation in piglets. Am J Physiol 280:H1490–H1495.
Brem AS, Bina RB, Mehta S, Marshall J 1999 Glucocorticoids inhibit the expression of calcium-dependent potassium channels in vascular smooth muscle. Mol Genet Metab 67: 53–57.
Wallerath T, Witte K, Schafer SC, Schwarz PM, Prellwitz W, Wohlfart P, Kleinert H, Lehr HA, Lemmer B, Forstermann U 1999 Down-regulation of the expression of endothelial NO synthase is likely to contribute to glucocorticoid-mediated hypertension. Proc Natl Acad Sci U S A 96: 13357–13362.
Johns DG, Dorrance AM, Tramontini NL, Webb RC 2001 Glucocorticoids inhibit tetrahydrobiopterin-dependent endothelial function. Exp Biol Med 226: 27–31.
Stonestreet BS, Petersson KH, Sadowska GB, Pettigrew KD, Patlak CS 1999 Antenatal steroids decrease blood-brain barrier permeability in the ovine fetus. Am J Physiol 276:R283–R289.
Halliday HL, Ehrenkranz RA 2001 Moderately early (7-14 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants. Cochrane Database Syst Rev 1: CD001144
Halliday HL, Ehrenkranz RA 2001 Early postnatal (<96 hours) corticosteroids for preventing chronic lung disease in preterm infants. Cochrane Database Syst Rev 1: CD001146
Shinwell ES, Karplus M, Reich D, Weintraub Z, Blazer S, Bader D, Yurman S, Dolfin T, Kogan A, Dollberg S, Arbel E, Goldberg M, Gur I, Naor N, Sirota L, Mogilner S, Zaritsky A, Barak M, Gottfried E 2000 Early postnatal dexamethasone treatment and increased incidence of cerebral palsy. Arch Dis Child Fetal Neonatal Ed 83:F177–F181.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by NHLBI/NIH (C.W.L.) and by a research grant from University of Kuopio (K.H.).
Rights and permissions
About this article
Cite this article
Heinonen, K., Fedinec, A. & Leffler, C. Dexamethasone Pretreatment Attenuates Cerebral Vasodilative Responses to Hypercapnia and Augments Vasoconstrictive Responses to Hyperventilation in Newborn Pigs. Pediatr Res 53, 260–265 (2003). https://doi.org/10.1203/01.PDR.0000047524.30084.64
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000047524.30084.64